Biomarkers for Refractory Lupus Nephritis: A Microarray Study of Kidney Tissue
Abstract
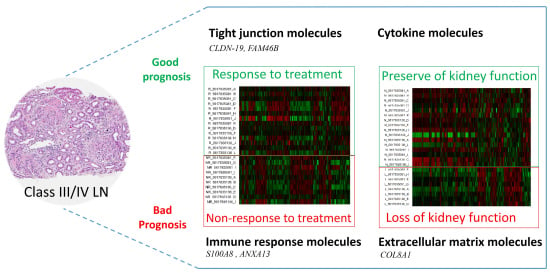
:1. Introduction
2. Results and Discussion
2.1. Patients and Samples
2.2. Intra-Renal Gene Expression in Lupus Nephritis (LN) Patients Who Did Not Respond to Treatment
| Characteristics | R a | NR b | p-Value |
|---|---|---|---|
| Number | 14 | 9 | n/a |
| Sex (F/M) | 13/1 | 9/0 | n/a |
| Age (years) | 32.31 ± 2.62 | 31.06 ± 2.70 | 0.88 |
| Clinical parameters | |||
| Serum creatinine (mg/dL) | 1.21 ± 0.32 | 1.56 ± 0.18 | 0.08 |
| Proteinuria (g/day) | 4.36 ± 0.80 | 4.33 ± 1.30 | 0.78 |
| Urinary erythrocyte count (per high-power field) | 92.86 ± 39.20 | 58.22 ± 31.82 | 0.37 |
| MDRD c GFR (mL/min) | 83.44 ± 11.63 | 51.18 ± 8.67 | 0.18 |
| Renal histology | |||
| Class III | 1 | 1 | n/a |
| Class IV | 13 | 8 | n/a |
| Activity index | 10.45 ± 0.86 | 11.63 ± 1.84 | 0.55 |
| Chronicity index | 1.55 ± 0.43 | 3.88 ± 0.83 | 0.03 |
| Steroid dose (mg/day) | 30.0 ± 8.66 | 21.60 ± 12.02 | 0.83 |
| Loss of renal function within 1 year d | 2 (14.29%) | 5 (55.55%) | 0.04 |
| Characteristics | R a | NR b | p-Value |
|---|---|---|---|
| Number | 22 | 22 | n/a |
| Sex (F/M) | 22/0 | 22/0 | n/a |
| Age (years) | 34.09 ± 1.98 | 32.04 ± 1.84 | 0.41 |
| Clinical parameters | |||
| Serum creatinine (mg/dL) | 1.15 ± 0.22 | 1.44 ± 0.29 | 0.29 |
| Proteinuria (g/day) | 3.39 ± 0.37 | 3.99 ± 0.75 | 0.93 |
| Urinary erythrocyte count (per high-power field) | 61.57 ± 26.26 | 35.27 ± 13.42 | 0.32 |
| MDRD c GFR (mL/min) | 85.60 ± 8.90 | 70.56 ± 8.62 | 0.30 |
| Renal histology | |||
| Class III | 3 | 5 | n/a |
| Class IV | 19 | 17 | n/a |
| Activity index | 9.38 ± 0.86 | 8.60 ± 1.21 | 0.40 |
| Chronicity index | 2.29 ± 0.51 | 3.15 ± 0.59 | 0.37 |
| Steroid dose (mg/day) | 25.59 ± 4.78 | 28.06 ± 6.50 | 0.70 |
| Loss of renal function d | 3 (13.64%) | 10 (31.82%) | 0.02 |

| Illumina IDs | Target ID | Fold Change | p-Value | Gene Function or Annotation |
|---|---|---|---|---|
| Upregulated genes | ||||
| ILMN_19368 a | ANAX13 | 2.22 | 0.0004 | annexin A13 |
| ILMN_627 a | ANAX13 | 2.46 | 0.0011 | annexin A13 |
| ILMN_3875 b | VCAM1 | 2.47 | 0.0022 | vascular cell adhesion molecule 1 |
| ILMN_26453 b | VCAM1 | 2.38 | 0.0026 | vascular cell adhesion molecule 1 |
| ILMN_8593 | CX3CR1 | 2.01 | 0.0051 | chemokine (C-X3-C motif) receptor 1 |
| ILMN_14011 | VNN1 | 2.38 | 0.0062 | vanin 1 |
| ILMN_13072 | S100A8 | 2.55 | 0.0095 | S100 calcium-binding protein A8 |
| Downregulated genes | ||||
| ILMN_6731 | CLDN19 | −2.23 | 0.0073 | claudin 19 |
| ILMN_13176 | DDIT4 | −2.27 | 0.0005 | DNA-damage-inducible transcript 4 |
| ILMN_9808 | FAM46B | −2.70 | 0.0015 | family with sequence similarity 46, member B |

2.3. Intra-Renal Gene Expression in LN Patients Who Had Loss of Kidney Function within 12 Months

| Illumina IDs | Target ID | Fold Change | p-Value | Gene Function or Annotation |
|---|---|---|---|---|
| Upregulated genes | ||||
| ILMN_19368 | ANAX13 | 1.82 | 0.03 | annexin A13 |
| ILMN_10408 | COL8A1 | 1.85 | 0.04 | collagen, type VIII, alpha 1 |
| Downregulated genes | ||||
| ILMN_1034 | SERPINA1 | −1.39 | 0.03 | serpin peptidase inhibitor, clade A, member 1 |
| ILMN_13176 | TRPV1 | −1.38 | 0.02 | transient receptor potential cation channel, subfamily V, member 6 |

2.4. Discussion
3. Experimental Section
3.1. Patients and Tissue Samples Collected
3.2. RNA Quality Control Assessment
3.3. Gene Expression Microarray
3.4. Microarray Data Analysis
3.5. Validation of the Candidate Biomarkers
3.6. Statistical Analysis of Real-Time PCR Validation
4. Conclusions
Supplementary Information
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ginzler, E.M.; Dooley, M.A.; Aranow, C.; Kim, M.Y.; Buyon, J.; Merrill, J.T.; Petri, M.; Gilkeson, G.S.; Wallace, D.J.; Weisman, M.H.; et al. Mycophenolate mofetil or intravenous cyclophosphamide for lupus nephritis. N. Engl. J. Med. 2005, 353, 2219–2228. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.E.; Korbet, S.M.; Katz, R.S.; Schwartz, M.M.; Lewis, E.J.; Collaborative Study Group. Value of a complete or partial remission in severe lupus nephritis. Clin. J. Am. Soc. Nephrol. 2008, 3, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Mok, C.C. Prognostic factors in lupus nephritis. Lupus 2005, 14, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Hill, G.S.; Delahousse, M.; Nochy, D.; Remy, P.; Mignon, F.; Mery, J.P.; Bariety, J. Predictive power of the second renal biopsy in lupus nephritis: Significance of macrophages. Kidney Int. 2001, 59, 304–316. [Google Scholar] [CrossRef] [PubMed]
- Avihingsanon, Y.; Benjachat, T.; Tassanarong, A.; Sodsai, P.; Kittikovit, V.; Hirankarn, N. Decreased renal expression of vascular endothelial growth factor in lupus nephritis is associated with worse prognosis. Kidney Int. 2009, 75, 1340–1348. [Google Scholar] [CrossRef] [PubMed]
- Rovin, B.H.; Zhang, X. Biomarkers for lupus nephritis: The quest continues. Clin. J. Am. Soc. Nephrol. 2009, 4, 1858–1865. [Google Scholar] [CrossRef] [PubMed]
- Perez de Lema, G.; Maier, H.; Nieto, E.; Vielhauer, V.; Luckow, B.; Mampaso, F.; Schlondorff, D. Chemokine expression precedes inflammatory cell infiltration and chemokine receptor and cytokine expression during the initiation of murine lupus nephritis. J. Am. Soc. Nephrol. 2001, 12, 1369–1382. [Google Scholar] [PubMed]
- Enghard, P.; Humrich, J.Y.; Rudolph, B.; Rosenberger, S.; Biesen, R.; Kuhn, A.; Manz, R.; Hiepe, F.; Radbruch, A.; Burmester, G.R.; et al. CXCR3+CD4+ T cells are enriched in inflamed kidneys and urine and provide a new biomarker for acute nephritis flares in systemic lupus erythematosus patients. Arthritis Rheum. 2009, 60, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Mishra, J.; Ma, Q.; Prada, A.; Mitsnefes, M.; Zahedi, K.; Yang, J.; Barasch, J.; Devarajan, P. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J. Am. Soc. Nephrol. 2003, 14, 2534–2543. [Google Scholar] [CrossRef] [PubMed]
- Avihingsanon, Y.; Phumesin, P.; Benjachat, T.; Akkasilpa, S.; Kittikowit, V.; Praditpornsilpa, K.; Wongpiyabavorn, J.; Eiam-Ong, S.; Hemachudha, T.; Tungsanga, K.; et al. Measurement of urinary chemokine and growth factor messenger RNAs: A noninvasive monitoring in lupus nephritis. Kidney Int. 2006, 69, 747–753. [Google Scholar] [CrossRef] [PubMed]
- Enghard, P.; Rieder, C.; Kopetschke, K.; Klocke, J.R.; Undeutsch, R.; Biesen, R.; Dragun, D.; Gollasch, M.; Schneider, U.; Aupperle, K.; et al. Urinary CD4 T-cells identify SLE patients with proliferative lupus nephritis and can be used to monitor treatment response. Ann. Rheum. Dis. 2014, 73, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Zickert, A.; Amoudruz, P.; Sundstrom, Y.; Ronnelid, J.; Malmstrom, V.; Gunnarsson, I. IL-17 and IL-23 in lupus nephritis—Association to histopathology and response to treatment. BMC Immunol. 2015, 16, 7. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhang, F.; Ma, J.; Zhang, X.; Wu, L.; Qu, B.; Xia, S.; Chen, S.; Tang, Y.; Shen, N. Association of large intergenic noncoding RNA expression with disease activity and organ damage in systemic lupus erythematosus. Arthritis Res. Ther. 2015, 17, 131. [Google Scholar] [CrossRef] [PubMed]
- Alcorta, D.A.; Barnes, D.A.; Dooley, M.A.; Sullivan, P.; Jonas, B.; Liu, Y.; Lionaki, S.; Reddy, C.B.; Chin, H.; Dempsey, A.A.; et al. Leukocyte gene expression signatures in antineutrophil cytoplasmic autoantibody and lupus glomerulonephritis. Kidney Int. 2007, 72, 853–864. [Google Scholar] [CrossRef] [PubMed]
- Olsen, N.J.; Moore, J.H.; Aune, T.M. Gene expression signatures for autoimmune disease in peripheral blood mononuclear cells. Arthritis Res. Ther. 2004, 6, 120–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avihingsanon, Y.; Hirankarn, N. Major lupus organ involvement: Severe lupus nephritis. Lupus 2010, 19, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Loser, K.; Vogl, T.; Voskort, M.; Lueken, A.; Kupas, V.; Nacken, W.; Klenner, L.; Kuhn, A.; Foell, D.; Sorokin, L.; et al. The Toll-like receptor 4 ligands Mrp8 and Mrp14 are crucial in the development of autoreactive CD8+ T cells. Nat. Med. 2010, 16, 713–717. [Google Scholar] [CrossRef] [PubMed]
- Frosch, M.; Vogl, T.; Waldherr, R.; Sorg, C.; Sunderkotter, C.; Roth, J. Expression of MRP8 and MRP14 by macrophages is a marker for severe forms of glomerulonephritis. J. Leukoc. Biol. 2004, 75, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Tantivitayakul, P.; Benjachat, T.; Somparn, P.; Leelahavanichkul, A.; Kittikovit, V.; Hirankarn, N.; Pisitkun, T.; Avihingsanon, Y. Elevated Expressions of Myeloid-Related Proteins-8 and -14 are Danger Biomarkers for Lupus Nephritis. Lupus under Review. 2015. [Google Scholar]
- Hou, J.; Goodenough, D.A. Claudin-16 and claudin-19 function in the thick ascending limb. Curr. Opin. Nephrol. Hypertens. 2010, 19, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Angelow, S.; El-Husseini, R.; Kanzawa, S.A.; Yu, A.S. Renal localization and function of the tight junction protein, claudin-19. Am. J. Physiol. Ren. Physiol. 2007, 293, F166–F177. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Rajagopal, M.; Yu, A.S. Claudins and the kidney. Annu. Rev. Physiol. 2013, 75, 479–501. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Renigunta, A.; Gomes, A.S.; Hou, M.; Paul, D.L.; Waldegger, S.; Goodenough, D.A. Claudin-16 and claudin-19 interaction is required for their assembly into tight junctions and for renal reabsorption of magnesium. Proc. Natl. Acad. Sci. USA 2009, 106, 15350–15355. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.P.; Tong, M.K.; Leung, P.P.; Chan, V.W.; Leung, S.; Tam, P.C.; Chan, K.W.; Lee, K.F.; Yeung, W.S.; Luk, J.M. Kidney claudin-19: Localization in distal tubules and collecting ducts and dysregulation in polycystic renal disease. FEBS Lett. 2006, 580, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Peterson, K.S.; Huang, J.F.; Zhu, J.; D'Agati, V.; Liu, X.; Miller, N.; Erlander, M.G.; Jackson, M.R.; Winchester, R.J. Characterization of heterogeneity in the molecular pathogenesis of lupus nephritis from transcriptional profiles of laser-captured glomeruli. J. Clin. Investig. 2004, 113, 1722–1733. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Sui, W.; Lan, H.; Yan, Q.; Huang, H.; Huang, Y. Comprehensive analysis of microRNA expression patterns in renal biopsies of lupus nephritis patients. Rheumatol. Int. 2009, 29, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Kwan, B.C.; Lai, F.M.; Tam, L.S.; Li, E.K.; Chow, K.M.; Wang, G.; Li, P.K.; Szeto, C.C. Glomerular and tubulointerstitial miR-638, miR-198 and miR-146a expression in lupus nephritis. Nephrology 2012, 17, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Hauser, P.V.; Perco, P.; Muhlberger, I.; Pippin, J.; Blonski, M.; Mayer, B.; Alpers, C.E.; Oberbauer, R.; Shankland, S.J. Microarray and bioinformatics analysis of gene expression in experimental membranous nephropathy. Nephron Exp. Nephrol. 2009, 112, e43–e58. [Google Scholar] [CrossRef] [PubMed]
- Hodgin, J.B.; Borczuk, A.C.; Nasr, S.H.; Markowitz, G.S.; Nair, V.; Martini, S.; Eichinger, F.; Vining, C.; Berthier, C.C.; Kretzler, M.; et al. A molecular profile of focal segmental glomerulosclerosis from formalin-fixed, paraffin-embedded tissue. Am. J. Pathol. 2010, 177, 1674–1686. [Google Scholar] [CrossRef] [PubMed]
- Schwab, K.; Witte, D.P.; Aronow, B.J.; Devarajan, P.; Potter, S.S.; Patterson, L.T. Microarray analysis of focal segmental glomerulosclerosis. Am. J. Nephrol. 2004, 24, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Shen, N.; Liang, D.; Tang, Y.; de Vries, N.; Tak, P.P. MicroRNAs—Novel regulators of systemic lupus erythematosus pathogenesis. Nat. Rev. Rheumatol. 2012, 8, 701–709. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Chuang, P.Y.; Liu, Z.H.; He, J.C. The primary glomerulonephritides: A systems biology approach. Nat. Rev. Nephrol. 2013, 9, 500–512. [Google Scholar] [CrossRef] [PubMed]
- De Spiegelaere, W.; Cornillie, P.; van Poucke, M.; Peelman, L.; Burvenich, C.; van den Broeck, W. Quantitative mRNA expression analysis in kidney glomeruli using microdissection techniques. Histol. Histopathol. 2011, 26, 267–275. [Google Scholar] [PubMed]
- Renal Disease Subcommittee of the American College of Rheumatology Ad Hoc Committee on Systemic Lupus Erythematosus Response Criteria. The American College of Rheumatology response criteria for proliferative and membranous renal disease in systemic lupus erythematosus clinical trials. Arthritis Rheum. 2006, 54, 421–432. [Google Scholar]
- Levey, A.S.; Inker, L.A.; Coresh, J. GFR estimation: From physiology to public health. Am. J. Kidney Dis. 2014, 63, 820–834. [Google Scholar] [CrossRef] [PubMed]
- Huang da, W.; Sherman, B.T.; Lempicki, R.A. Bioinformatics enrichment tools: Paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 2009, 37, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Mi, H.; Muruganujan, A.; Casagrande, J.T.; Thomas, P.D. Large-scale gene function analysis with the PANTHER classification system. Nat. Protoc. 2013, 8, 1551–1566. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benjachat, T.; Tongyoo, P.; Tantivitayakul, P.; Somparn, P.; Hirankarn, N.; Prom-On, S.; Pisitkun, P.; Leelahavanichkul, A.; Avihingsanon, Y.; Townamchai, N. Biomarkers for Refractory Lupus Nephritis: A Microarray Study of Kidney Tissue. Int. J. Mol. Sci. 2015, 16, 14276-14290. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms160614276
Benjachat T, Tongyoo P, Tantivitayakul P, Somparn P, Hirankarn N, Prom-On S, Pisitkun P, Leelahavanichkul A, Avihingsanon Y, Townamchai N. Biomarkers for Refractory Lupus Nephritis: A Microarray Study of Kidney Tissue. International Journal of Molecular Sciences. 2015; 16(6):14276-14290. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms160614276
Chicago/Turabian StyleBenjachat, Thitima, Pumipat Tongyoo, Pornpen Tantivitayakul, Poorichaya Somparn, Nattiya Hirankarn, Santitham Prom-On, Prapaporn Pisitkun, Asada Leelahavanichkul, Yingyos Avihingsanon, and Natavudh Townamchai. 2015. "Biomarkers for Refractory Lupus Nephritis: A Microarray Study of Kidney Tissue" International Journal of Molecular Sciences 16, no. 6: 14276-14290. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms160614276