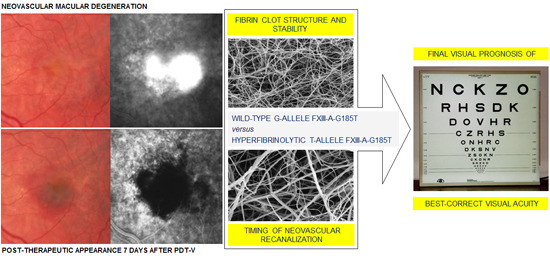
Effect of Factor XIII-A G185T Polymorphism on Visual Prognosis after Photodynamic Therapy for Neovascular Macular Degeneration
Abstract
:1. Introduction
2. Results
| Study Population (n = 412 Patients Affected by Subfoveal CNV) | |||||
|---|---|---|---|---|---|
| Baseline Characteristics | FXIII-A 185-T-Allele Carriers (n = 187) | FXIII-A 185-T-Allele Non-Carriers (n = 225) | p Value | ||
| Sex | |||||
| Male/Female–no. (%) | 86 (46.0)/101 (54.0) | 104 (46.2)/121 (53.8) | NS * | ||
| Mean age ± SD (range)–years | 64.514 ± 13.807 (34–86) | 64.802 ± 15.122 (33–88) | NS † | ||
| Mean BCVA ± SD (range)–logMAR | 0.604 ± 0.215 (0.2–1.0) | 0.594 ± 0.231 (0.1–1.0) | NS † | ||
| Mean CNV area ± SD (range)–micron2 | 2894.2 ± 2789.3 (232–10,065) | 2759.4 ± 2605.7 (244–10,125) | NS † | ||
| Type of neovascular lesion | |||||
| Classic or predominantly classic AMD-related CNV–no. (%) | 63 (33.7) | 76 (33.8) | NS * | ||
| Minimally classic or occult AMD-related CNV–no. (%) | 48 (25.7) | 57 (25.3) | NS * | ||
| Classic PM-related CNV–no. (%) | 76 (40.6) | 92 (40.9) | NS * | ||
| Study Population (n = 412 Patients Affected by Subfoveal CNV) | |||
|---|---|---|---|
| Outcome Measures | FXIII-A 185-T-Allele Carriers (n = 187) | FXIII-A 185-T-Allele Non-Carriers (n = 225) | p Value |
| Number of PDT-V | No. (%) | No. (%) | |
| 1–2 | 7 (3.7) | 31 (13.8) | |
| 3–4 | 38 (20.3) | 111 (49.3) | |
| 5–6 | 100 (53.5) | 68 (30.2) | |
| 7–8 | 42 (22.5) | 15 (6.7) | |
| Mean number of PDT-V ± SE | 5.51 ± 0.13 | 3.76 ± 0.12 | 0.01 * |
| Final BCVA (logMAR) | No. (%) | No. (%) | |
| 0.1–0.3 | 8 (4.3) | 39 (17.3) | |
| 0.4–0.6 | 45 (24.1) | 78 (34.7) | |
| 0.7–0.9 | 70 (37.4) | 70 (31.1) | |
| 1.0–1.3 | 64 (34.2) | 38 (16.9) | |
| Mean final BCVA ± SD | 0.81 ± 0.31 | 0.59 ± 0.33 | 0.01 † |
| BCVA change (logMAR) | No. (%) | No. (%) | |
| −0.4–−0.2 | 12 (6,4) | 20 (8.9) | |
| −0.1–0.0 | 32 (17.1) | 107 (47.5) | |
| 0.1–0.2 | 22 (11.8) | 45 (20.0) | |
| 0.3–0.7 | 121 (64.7) | 53 (23.6) | |
| Mean BCVA change ± SE | 0.22 ± 0.03 | 0.08 ± 0.02 | 0.01 * |
3. Discussion
4. Experimental Section
4.1. Study Patients
| Inclusion Criteria |
| diagnosis of AMD in Caucasian patients with more than 65 years or of PM in patients with less than 60 years; best-correct visual acuity better than 20/200 (Snellen equivalent); angiographic diagnosis of classic or predominantly classic CNV secondary to AMD, occult with no classic CNV secondary to AMD or classic CNV secondary to PM; active CNV under the geometric center of the foveal avascular zone (subfoveal); greatest linear dimension of the neovascular complex less than 5400 micron in patients with AMD- or PM-related classic CNV; greatest dimension of the neovascular complex equal or less than 4 Macular Photocoagulation Study disc areas in patients with AMD-related minimally classic or occult CNV. |
| Exclusion Criteria |
| history of any other CNV treatment before and/or during PDT-V protocol; presence of any other possible cause of CNV, such as angioid streaks, chorioretinal inflammatory diseases, hereditary retinal disorders, presumed ocular histoplasmosis syndrome, and/or severe ocular trauma; intraocular surgery and any laser-treatment of the eye during the 6 months before or the 3 months after PDT-V protocol; presence of any significant side effect, condition and/or event possibly influencing the outcome of each PDT-V application; active or chronic systemic diseases related to alterations of hemostatic balance; assumption of any medication known to affect the hemostatic balance, such as antiplatelet, antithrombotic and anticoagulant drugs. |
4.2. Data Collection
4.3. Statistical Analyses
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Resnikoff, S.; Pascolini, D.; Etya’ale, D.; Kocur, I.; Pararajasegaram, R.; Pokharel, G.P.; Mariotti, S.P. Global data on visual impairment in the year 2002. Bull. World Health Organ. 2004, 82, 844–851. [Google Scholar] [PubMed]
- Klein, R.; Peto, T.; Bird, A.; Vannewkirk, M.R. The epidemiology of age-related macular degeneration. Am. J. Ophthalmol. 2004, 137, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Ferris, F.L., III; Fine, S.L.; Hyman, L. Age-related macular degeneration and blindness due to neovascular maculopathy. Arch. Ophthalmol. 1984, 102, 1640–1642. [Google Scholar]
- Soubrane, G. Choroidal neovascularization in pathologic myopia: Recent developments in diagnosis and treatment. Surv. Ophthalmol. 2008, 53, 121–138. [Google Scholar] [CrossRef] [PubMed]
- Soubrane, G.; Cruess, A.; Lotery, A.; Pauleikhoff, D.; Monès, J.; Xu, X.; Zlateva, G.; Buggage, R.; Conlon, J.; Goss, T.F. Burden and health care resource utilization in neovascular age-related macular degeneration: Findings of a multicountry study. Arch. Ophthalmol. 2007, 125, 1249–1254. [Google Scholar] [CrossRef] [PubMed]
- Colquitt, J.L.; Jones, J.; Tan, S.C.; Takeda, A.; Clegg, A.J.; Price, A. Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: A systematic review and economic evaluation. Health Technol. Assess. 2008, 12, 1–222. [Google Scholar] [CrossRef]
- Cruess, A.F.; Zlateva, G.; Xu, X.; Soubrane, G.; Pauleikhoff, D.; Lotery, A.; Monès, J.; Buggage, R.; Schaefer, C.; Knight, T.; et al. Economic burden of bilateral neovascular age-related macular degeneration: Multi-country observational study. Pharmacoeconomics 2008, 26, 57–73. [Google Scholar] [PubMed]
- Das, A.; McGuire, P.G. Retinal and choroidal angiogenesis: Pathophysiology and strategies for inhibition. Prog. Retin. Eye Res. 2003, 22, 721–748. [Google Scholar] [CrossRef] [PubMed]
- Bressler, S.B. Introduction: Understanding the role of angiogenesis and antiangiogenic agents in age-related macular degeneration. Ophthalmology 2009, 116, S1–S7. [Google Scholar] [CrossRef] [PubMed]
- Chakravarthy, U.; Soubrane, G.; Bandello, F.; Chong, V.; Creuzot-Garcher, C.; Dimitrakos, S.A., II; Korobelnik, J.F.; Larsen, M.; Monés, J.; Pauleikhoff, D.; et al. Evolving European guidance on the medical management of neovascular age related macular degeneration. Br. J. Ophthalmol. 2006, 90, 1188–1196. [Google Scholar]
- Wormald, R.; Evans, J.; Smeeth, L.; Henshaw, K. Photodynamic therapy for neovascular age-related macular degeneration. Cochrane Database Syst. Rev. 2007, 3. [Google Scholar] [CrossRef]
- Vedula, S.S.; Krzystolik, M.G. Antiangiogenic therapy with anti-vascular endothelial growth factor modalities for neovascular age-related macular degeneration. Cochrane Database Syst. Rev. 2008, 2. [Google Scholar] [CrossRef]
- Cohen, S.Y. Anti-VEGF drugs as the 2009 first-line therapy for choroidal neovascularization in pathologic myopia. Retina 2009, 29, 1062–1066. [Google Scholar] [CrossRef] [PubMed]
- Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: One-year results of 2 randomized clinical trials—TAP Report No. 1. Arch. Ophthalmol. 1999, 117, 1329–1345. [Google Scholar]
- Verteporfin in Photodynamic Therapy (VIP) Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age related macular degeneration: 2 year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization—VIP Report No. 2. Am. J. Ophthalmol. 2001, 131, 541–560. [Google Scholar]
- Blinder, K.J.; Blumenkranz, M.S.; Bressler, N.M.; Bressler, S.B.; Donato, G.; Lewis, H.; Lim, J.I.; Menchini, U.; Miller, J.W.; Monès, J.M.; et al.; Verteporfin in Photodynamic Therapy (VIP) Study Group Verteporfin therapy of subfoveal choroidal neovascularization in pathologic myopia: 2-Year results of a randomized clinical trial—VIP Report No. 3. Ophthalmology 2003, 110, 667–673. [Google Scholar]
- Verteporfin Roundtable Participants. Guidelines for using verteporfin (Visudyne) in photodynamic therapy for choroidal neovascularization due to age-related macular degeneration and other causes: Update. Retina 2005, 25, 119–134. [Google Scholar]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; Kim, R.Y.; MARINA Study Group. Ranibizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar] [PubMed]
- Mitchell, P.; Korobelnik, J.F.; Lanzetta, P.; Holz, F.G.; Prünte, C.; Schmidt-Erfurth, U.; Tano, Y.; Wolf, S. Ranibizumab (Lucentis) in neovascular age-related macular degeneration: Evidence from clinical trials. Br. J. Ophthalmol. 2010, 94, 2–13. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.F.; Maguire, M.G.; Fine, S.L.; Ying, G.S.; Jaffe, G.J.; Grunwald, J.E.; Toth, C.; Redford, M.; Ferris, F.L., III; Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: Two-year results. Ophthalmology 2012, 119, 1388–1398. [Google Scholar] [PubMed]
- Heier, J.S.; Brown, D.M.; Chong, V.; Korobelnik, J.F.; Kaiser, P.K.; Nguyen, Q.D.; Kirchhof, B.; Ho, A.; Ogura, Y.; Yancopoulos, G.D.; et al.; VIEW 1 and VIEW 2 Study Groups Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 2012, 119, 2537–2548. [Google Scholar] [PubMed]
- Chakravarthy, U.; Harding, S.P.; Rogers, C.A.; Downes, S.M.; Lotery, A.J.; Culliford, L.A.; Reeves, B.C.; IVAN Study Investigators. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet 2013, 12, 1258–1267. [Google Scholar]
- Lazic, R.; Gabric, N. Verteporfin therapy and intravitreal bevacizumab combined and alone in choroidal neovascularization due to age-related macular degeneration. Ophthalmology 2007, 114, 1179–1185. [Google Scholar] [CrossRef] [PubMed]
- Antoszyk, A.N.; Tuomi, L.; Chung, C.Y.; Singh, A.; FOCUS Study Group. Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration (FOCUS): Year 2 results. Am. J. Ophthalmol. 2008, 145, 862–874. [Google Scholar] [PubMed]
- Navea, A.; Mataix, J.; Desco, M.C.; Garcia-Pous, M.; Palacios, E. One-year follow-up of combined customized therapy. Photodynamic therapy and bevacizumab for exudative age-related macular degeneration. Retina 2009, 29, 13–19. [Google Scholar] [PubMed]
- Kaiser, P.K.; Boyer, D.S.; Garcia, R.; Hao, Y.; Hughes, M.S.; Jabbour, N.M.; Kaiser, P.K.; Mieler, W.; Slakter, J.S.; Samuel, M.; et al. Verteporfin photodynamic therapy combined with intravitreal bevacizumab for neovascular age-related macular degeneration. Ophthalmology 2009, 116, 747–755. [Google Scholar] [PubMed]
- Desco, M.C.; Mataix, J.; Garcia-Pous, M.; Palacios-Pozo, E.; Navea, A. Combined therapy: Photodynamic therapy and bevacizumab to treat myopic neovascular membranes. One-year follow-up. Retina 2011, 31, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Bashshur, Z.F.; Schakal, A.R.; El-Mollayess, G.M.; Arafat, S.; Jaafar, D.; Salti, H.I. Ranibizumab monotherapy versus single-session verteporfin photodynamic therapy combined with as-needed ranibizumab treatment for the management of neovascular age-related macular degeneration. Retina 2011, 31, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, P.K.; Boyer, D.S.; Cruess, A.F.; Slakter, J.S.; Pilz, S.; Weisberger, A.; DENALI Study Group. Verteporfin plus ranibizumab for choroidal neovascularization in age-related macular degeneration: twelve-month results of the DENALI study. Ophthalmology 2012, 119, 1001–1010. [Google Scholar] [PubMed]
- Krebs, I.; Vécsei Marlovits, V.; Bodenstorfer, J.; Glittenberg, C.; Ansari Shahrezaei, S.; Ristl, R.; Binder, S. Comparison of Ranibizumab monotherapy versus combination of Ranibizumab with photodynamic therapy with neovascular age-related macular degeneration. Acta Ophthalmol. 2013, 91, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.M.; Prünte, C. Management of neovascular age-related macular degeneration. Prog. Retin. Eye Res. 2007, 26, 437–451. [Google Scholar] [CrossRef] [PubMed]
- Shah, G.K.; Sang, D.N.; Hughes, M.S. Verteporfin combination regimens in the treatment of neovascular age-related macular degeneration. Retina 2009, 29, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Kiss, C.; Sacu, S. The role of choroidal hypoperfusion associated with photodynamic therapy in neovascular age-related macular degeneration and the consequences for combination strategies. Prog. Retin. Eye Res. 2009, 28, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Amoaku, W.M.; Chakravarthy, U.; Gale, R.; Gavin, M.; Ghanchi, F.; Gibson, J.; Harding, S.; Johnston, R.L.; Kelly, S.; Lotery, A.; et al. Defining response to anti-VEGF therapies in neovascular AMD. Eye 2015, 29, 721–731. [Google Scholar] [PubMed]
- Schmidt-Erfurth, U.; Hasan, T. Mechanisms of action of photodynamic therapy with verteporfin for the treatment of age-related macular degeneration. Surv. Ophthalmol. 2000, 45, 195–214. [Google Scholar] [CrossRef]
- Schlotzer-Schrehardt, U.; Viestenz, A.; Naumann, G.O.; Laqua, H.; Michels, S.; Schmidt-Erfurth, U. Dose-related structural effects of photodynamic therapy on choroidal and retinal structures of human eyes. Graefes Arch. Clin. Exp. Ophthalmol. 2002, 240, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Michels, S.; Barbazetto, I.; Laqua, H. Photodynamic effects on choroidal neovascularization and physiological choroid. Investig. Ophthalmol. Vis. Sci. 2002, 43, 830–841. [Google Scholar]
- Michels, S.; Schmidt-Erfurth, U. Sequence of early vascular events after photodynamic therapy. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2147–2154. [Google Scholar] [CrossRef]
- Schmidt-Erfurth, U.; Niemeyer, M.; Geitzenauer, W.; Michels, S. Time course and morphology of vascular effects associated with photodynamic therapy. Ophthalmology 2005, 112, 2061–2069. [Google Scholar] [CrossRef] [PubMed]
- Blinder, K.J.; Bradley, S.; Bressler, N.M.; Bressler, S.B.; Donati, G.; Hao, Y.; Ma, C.; Menchini, U.; Miller, J.; Potter, M.J.; et al. Effect of lesion size, visual acuity, and lesion composition on visual acuity change with and without verteporfin therapy for choroidal neovascularization secondary to age-related macular degeneration: TAP and VIP report 1. Am. J. Ophthalmol. 2003, 136, 407–418. [Google Scholar]
- Axer-Siegel, R.; Ehrlich, R.; Yassur, Y.; Rosenblatt, I.; Kramer, M.; Priel, E.; Benjamini, Y.; Weinberger, D. Photodynamic therapy for age-related macular degeneration in a clinical setting: Visual results and angiographic patterns. Am. J. Ophthalmol. 2004, 137, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Arias, L.; Pujol, O.; Berniell, J.; Rubio, M.; Roca, G.; Castillo, L.; Acebes, E. Impact of lesion size on photodynamic therapy with verteporfin of predominantly classic lesions in age related macular degeneration. Br. J. Ophthalmol. 2005, 89, 312–315. [Google Scholar] [CrossRef] [PubMed]
- Ergun, E.; Heinzl, H.; Stur, M. Prognostic factors influencing visual outcome of photodynamic therapy for subfoveal choroidal neovascularization in pathologic myopia. Am. J. Ophthalmol. 2004, 138, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Axer-Siegel, R.; Ehrlich, R.; Weinberger, D.; Rosenblatt, I.; Shani, L.; Yassur, Y.; Priel, E.; Kramer, M. Photodynamic therapy of subfoveal choroidal neovascularization in high myopia in a clinical setting: Visual outcome in relation to age at treatment. Am. J. Ophthalmol. 2004, 138, 602–607. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.M.; Lai, T.Y.; Tano, Y.; Liu, D.T.; Li, K.K.; Lam, D.S. Photodynamic therapy in macular diseases of Asian populations: When East meets West. Jpn. J. Ophthalmol. 2006, 50, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Yang, N.; Fan, C.M.; Ho, C.K. Review of first year result of photodynamic therapy on age-related macular degeneration in Chinese population. Eye 2006, 20, 523–526. [Google Scholar] [CrossRef] [PubMed]
- Verteporfin in Photodynamic Therapy (VIP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in pathologic myopia with verteporfin: 1-year results of a randomized clinical trial—VIP report No. 1. Ophthalmology 2001, 108, 841–852. [Google Scholar]
- Lam, D.S.; Chan, W.M.; Liu, D.T.; Fan, D.S.; Lai, W.W.; Chong, K.K. Photodynamic therapy with verteporfin for subfoveal choroidal neovascularisation of pathologic myopia in Chinese eyes: A prospective series of 1 and 2 year follow up. Br. J. Ophthalmol. 2004, 88, 1315–1319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayashi, K.; Ohno-Matsui, K.; Teramukai, S.; Shimada, N.; Moriyama, M.; Hara, W.; Yoshida, T.; Tokoro, T.; Mochizuki, M. Photodynamic therapy with verteporfin for choroidal neovascularization of pathologic myopia in Japanese patients: Comparison with nontreated controls. Am. J. Ophthalmol. 2008, 145, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Costagliola, C.; Gemmati, D.; D’Angelo, S.; Perri, P.; Scapoli, G.L.; Catozzi, L.; Federici, F.; Sebastiani, A.; Incorvaia, C. Predictive role of coagulation-balance gene polymorphisms in the efficacy of photodynamic therapy with verteporfin for classic choroidal neovascularization secondary to age-related macular degeneration. Pharmacogenet. Genom. 2007, 17, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Costagliola, C.; Gemmati, D.; D’Angelo, S.; Perri, P.; Campa, C.; Catozzi, L.; Federici, F.; Sebastiani, A.; Incorvaia, C. Coagulation-balance genetic predictors for efficacy of photodynamic therapy in occult choroidal neovascularization secondary to age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2008, 49, 3100–3106. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Gemmati, D.; Costagliola, C.; Semeraro, F.; D’Angelo, S.; Perri, P.; Sebastiani, A.; Incorvaia, C. Impact of coagulation-balance gene predictors on efficacy of photodynamic therapy for choroidal neovascularization in pathologic myopia. Ophthalmology 2010, 117, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Gemmati, D.; Costagliola, C.; Sebastiani, A.; Incorvaia, C. Predictive role of gene polymorphisms affecting thrombin-generation pathway in variable efficacy of photodynamic therapy for neovascular age-related macular degeneration. Recent. Pat. DNA Gene Seq. 2009, 3, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Gemmati, D.; Costagliola, C.; Sebastiani, A.; Incorvaia, C. Predictive role of C677T MTHFR polymorphism in variable efficacy of photodynamic therapy for neovascular age-related macular degeneration. Pharmacogenomics 2009, 10, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Costagliola, C.; Incorvaia, C.; Sebastiani, A.; Gemmati, D. Pharmacogenetic aspects in therapeutic management of subfoveal choroidal neovascularisation: Role of factor XIII-A 185 T-allele. Curr. Drug Targets 2011, 12, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Gemmati, D.; Costagliola, C.; Semeraro, F.; Perri, P.; D’Angelo, S.; Romano, M.R.; de Nadai, K.; Sebastiani, A.; Incorvaia, C. Genetic predictors of response to photodynamic therapy. Mol. Diagn. Ther. 2011, 15, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Gemmati, D.; Serino, M.L.; Ongaro, A.; Tognazzo, S.; Moratelli, S.; Resca, R.; Moretti, M.; Scapoli, G.L. A common mutation in the gene for coagulation factor XIII-A (VAL34Leu): A risk factor for primary intracerebral hemorrhage is protective against atherothrombotic diseases. Am. J. Hematol. 2001, 67, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Bressler, N.M.; TAP Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: Two-year results of 2 randomized clinical trials—TAP report No. 2. Arch. Ophthalmol. 2001, 119, 198–207. [Google Scholar] [PubMed]
- Azab, M.; Boyer, D.S.; Bressler, N.M.; Bressler, S.B.; Cihelkova, I.; Hao, Y.; Immonen, I.; Lim, J.I.; Menchini, U.; Naor, J.; et al. Verteporfin therapy of subfoveal minimally classic choroidal neovascularization in age-related macular degeneration: 2-Year results of a randomized clinical trial. Arch. Ophthalmol. 2005, 123, 448–457. [Google Scholar] [PubMed]
- Campa, C.; Costagliola, C.; Incorvaia, C.; Sheridan, C.; Semeraro, F.; De Nadai, K.; Sebastiani, A.; Parmeggiani, F. Inflammatory mediators and angiogenic factors in choroidal neovascularization: pathogenetic interactions and therapeutic implications. Mediators Inflamm. 2010, 2010. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Romano, M.R.; Costagliola, C.; Semeraro, F.; Incorvaia, C.; D’Angelo, S.; Perri, P.; de Palma, P.; de Nadai, K.; Sebastiani, A. Mechanism of inflammation in age-related macular degeneration. Mediators Inflamm. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Sorrentino, F.S.; Romano, M.R.; Costagliola, C.; Semeraro, F.; Incorvaia, C.; D’Angelo, S.; Perri, P.; de Nadai, K.; Bonomo Roversi, E.; et al. Mechanism of inflammation in age-related macular degeneration: An up-to-date on genetic landmarks. Mediators Inflamm. 2013, 2013. [Google Scholar] [CrossRef]
- Gallenga, C.E.; Parmeggiani, F.; Costagliola, C.; Sebastiani, A.; Gallenga, P.E. Inflammaging: Should this term be suitable for age related macular degeneration too? Inflamm. Res. 2014, 63, 105–107. [Google Scholar] [CrossRef] [PubMed]
- Incorvaia, C.; Campa, C.; Parmeggiani, F.; Menzione, M.; D’Angelo, S.; Della Corte, M.; Rinaldi, M.; Romano, M.; Dell’Omo, R.; Costagliola, C. 12-month retrospective study and review of photodynamic therapy with verteporfin for subfoveal choroidal neovascularization in age-related macular degeneration. Retina 2008, 29, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Costagliola, C.; Campa, C.; Incorvaia, C.; Parmeggiani, F.; Menzione, M.; Della Corte, M.; Rinaldi, M.; Romano, M.; Semeraro, F. Verteporfin photodynamic therapy for subfoveal choroidal neovascularization in pathologic myopia: A 12-month retrospective review. Eur. J. Ophthalmol. 2008, 18, 955–959. [Google Scholar] [PubMed]
- Ichinose, A. Physiopathology and regulation of factor XIII. Thromb. Haemost. 2001, 86, 57–65. [Google Scholar] [PubMed]
- Bereczky, Z.; Katona, E.; Muszbek, L. Fibrin stabilization (factor XIII), fibrin structure and thrombosis. Pathophysiol. Haemost. Thromb. 2003, 33, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Mosesson, M.W. Fibrinogen and fibrin structure and functions. J. Thromb. Haemost. 2005, 3, 1894–1904. [Google Scholar] [CrossRef] [PubMed]
- Jámbor, C.; Reul, V.; Schnider, T.W.; Degiacomi, P.; Metzner, H.; Korte, W.C. In vitro inhibition of factor XIII retards clot formation, reduces clot firmness, and increases fibrinolytic effects in whole blood. Anesth. Analg. 2009, 109, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Anwar, R.; Gallivan, L.; Edmonds, S.D.; Markham, A.F. Genotype/phenotype correlations for coagulation factor XIII: Specific normal polymorphisms are associated with high or low factor XIII specific activity. Blood 1999, 93, 897–905. [Google Scholar] [PubMed]
- De Lange, M.; Andrew, T.; Snieder, H.; Ge, D.; Futers, T.S.; Standeven, K.; Spector, T.D.; Grant, P.J.; Ariëns, R.A. Joint linkage and association of six single-nucleotide polymorphisms in the factor XIII-A subunit gene point to V34L as the main functional locus. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 1914–1919. [Google Scholar] [CrossRef] [PubMed]
- Kohler, H.P.; Ariëns, R.A.; Whitaker, P.; Grant, P.J. A common coding polymorphism in the FXIII A-subunit gene (FXIIIVal34Leu) affects cross-linking activity. Thromb. Haemost. 1998, 80, 704–704. [Google Scholar] [PubMed]
- Ariëns, R.A.; Philippou, H.; Nagaswami, C.; Weisel, J.W.; Lane, D.A.; Grant, P.J. The factor XIII V34L polymorphism accelerates thrombin activation of factor XIII and affects cross-linked fibrin structure. Blood 2000, 96, 988–995. [Google Scholar] [PubMed]
- Maurer, M.C.; Trumbo, T.A.; Isetti, G.; Turner, B.T., Jr. Probing interactions between the coagulants thrombin, Factor XIII, and fibrin(ogen). Arch. Biochem. Biophys. 2006, 1(445), 36–45. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, V.; Kohler, H.P. Effect of factor XIII Val34Leu on α2-antiplasmin incorporation into fibrin. Thromb. Haemost. 2000, 84, 1128–1130. [Google Scholar]
- Ariëns, R.A.; Lai, T.S.; Weisel, J.W.; Greenberg, C.S.; Grant, P.J. Role of factor XIII in fibrin clot formation and effects of genetic polymorphisms. Blood 2002, 100, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Lim, B.C.; Ariëns, R.A.; Carter, A.M.; Weisel, J.W.; Grant, P.J. Genetic regulation of fibrin structure and function: Complex gene-environment interactions may modulate vascular risk. Lancet 2003, 361, 1424–1431. [Google Scholar] [CrossRef]
- Kobbervig, C.; Williams, E. FXIII polymorphisms, fibrin clot structure and thrombotic risk. Biophys. Chem. 2004, 112, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Komáromi, I.; Bagoly, Z.; Muszbek, L. Factor XIII: Novel structural and functional aspects. J. Thromb. Haemost. 2011, 9, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Durlu, Y.K. Retinal and choroidal alterations following photodynamic therapy. Adv. Exp. Med. Biol. 2003, 533, 115–122. [Google Scholar] [PubMed]
- Dewi, N.A.; Yuzawa, M.; Tochigi, K.; Kawamura, A.; Mori, R. Effects of photodynamic therapy on the choriocapillaris and retinal pigment epithelium in the irradiated area. Jpn. J. Ophthalmol. 2008, 52, 277–281. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parmeggiani, F.; Costagliola, C.; Semeraro, F.; Romano, M.R.; Rinaldi, M.; Gallenga, C.E.; Serino, M.L.; Incorvaia, C.; D’Angelo, S.; De Nadai, K.; et al. Effect of Factor XIII-A G185T Polymorphism on Visual Prognosis after Photodynamic Therapy for Neovascular Macular Degeneration. Int. J. Mol. Sci. 2015, 16, 19796-19811. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms160819796
Parmeggiani F, Costagliola C, Semeraro F, Romano MR, Rinaldi M, Gallenga CE, Serino ML, Incorvaia C, D’Angelo S, De Nadai K, et al. Effect of Factor XIII-A G185T Polymorphism on Visual Prognosis after Photodynamic Therapy for Neovascular Macular Degeneration. International Journal of Molecular Sciences. 2015; 16(8):19796-19811. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms160819796
Chicago/Turabian StyleParmeggiani, Francesco, Ciro Costagliola, Francesco Semeraro, Mario R Romano, Michele Rinaldi, Carla Enrica Gallenga, Maria Luisa Serino, Carlo Incorvaia, Sergio D’Angelo, Katia De Nadai, and et al. 2015. "Effect of Factor XIII-A G185T Polymorphism on Visual Prognosis after Photodynamic Therapy for Neovascular Macular Degeneration" International Journal of Molecular Sciences 16, no. 8: 19796-19811. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms160819796