Internet-Supported Physical Exercise Training for Persons with Multiple Sclerosis—A Randomised, Controlled Study
Abstract
:1. Introduction
2. Results
2.1. Compliance
2.2. Health-Related Quality of Life and Fatigue
2.3. Muscle Strength
2.4. Aerobic Capacity and Lung Function
2.5. Physical Activity
3. Discussion
3.1. Health-Related Quality of Life
3.2. Fatigue
3.3. Muscle Strength
3.4. Aerobic Capacity and Lung Function
3.5. Physical Activity
3.6. Compliance
3.7. Limitations
4. Materials and Methods
4.1. Study Design
4.2. Subjects
4.3. Assessments
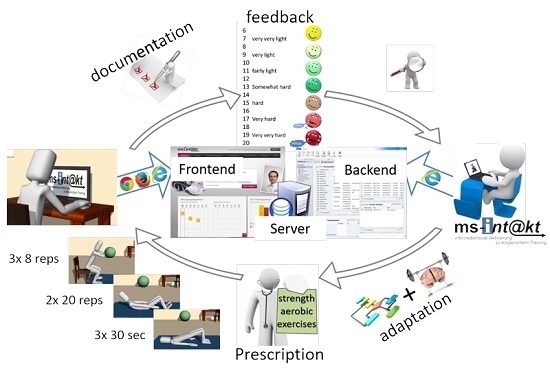
4.4. Intervention
4.5. Statistical Procedures
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Tallner, A.; Mäurer, M.; Pfeifer, K. Multiple Sklerose und körperliche Aktivität. Nervenarzt 2013, 84, 1238–1244. [Google Scholar] [CrossRef] [PubMed]
- Latimer-Cheung, A.E.; Pilutti, L.A.; Hicks, A.L.; Ginis, K.A.M.; Fenuta, A.M.; MacKibbon, K.A.; Motl, R.W. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: A systematic review to inform guideline development. Arch. Phys. Med. Rehabil. 2013, 94, 1800–1828. [Google Scholar] [CrossRef] [PubMed]
- Dalgas, U.; Stenager, E.; Ingemann-Hansen, T. Multiple sclerosis and physical exercise: Recommendations for the application of resistance-, endurance- and combined training. Mult. Scler. 2008, 14, 35–53. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, J.H. Getting beyond the plateau: Bridging the gap between rehabilitation and community-based exercise. PMR 2012, 4, 857–861. [Google Scholar] [CrossRef] [PubMed]
- Marcus, B.; Nigg, C.; Riebe, D.; Forsyth, L. Interactive communication strategies: Implications for population-based physical activity promotion. Am. J. Prev. Med. 2000, 19, 121–126. [Google Scholar] [CrossRef]
- Kuspinar, A.; Rodriguez, A.M.; Mayo, N.E. The effects of clinical interventions on health-related quality of life in multiple sclerosis: A meta-analysis. Mult. Scler. 2012, 18, 1686–1704. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.; Gosney, J. Effect of exercise training on quality of life in multiple sclerosis: A meta-analysis. Mult. Scler. 2008, 14, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.H.; Gold, S.M.; Witte, J.; Bartsch, K.; Lang, U.E.; Hellweg, R.; Reer, R.; Braumann, K.M.; Heesen, C. Impact of aerobic training on immune-endocrine parameters, neurotrophic factors, quality of life and coordinative function in multiple sclerosis. J. Neurol. Sci. 2004, 225, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Gillison, F.; Skevington, S.; Sato, A.; Standage, M.; Evangelidou, S. The effects of exercise interventions on quality of life in clinical and healthy populations: A meta-analysis. Soc. Sci. Med. 2009, 68, 1700–1710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andreasen, A.; Stenager, E.; Dalgas, U. The effect of exercise therapy on fatigue in multiple sclerosis. Mult. Scler. 2011, 17, 1041–1054. [Google Scholar] [CrossRef] [PubMed]
- Pilutti, L.A.; Greenlee, T.A.; Motl, R.W.; Nickrent, M.S.; Petruzzello, S.J. Effects of exercise training on fatigue in multiple sclerosis: A meta-analysis. Psychosom. Med. 2013, 75, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Platta, M.E.; Ensari, I.; Motl, R.W.; Pilutti, L.A. Effect of exercise training on fitness in multiple sclerosis: A meta-analysis. Arch. Phys. Med. Rehabil. 2016. [Google Scholar] [CrossRef] [PubMed]
- Langeskov-Christensen, M.; Heine, M.; Kwakkel, G.; Dalgas, U. Aerobic capacity in persons with multiple sclerosis: A systematic review and meta-analysis. Sports Med. 2015, 45, 905–923. [Google Scholar] [CrossRef] [PubMed]
- Gosselink, R.; Kovacs, L.; Decramer, M. Respiratory muscle involvement in multiple sclerosis. Eur. Respir. J. 1999, 13, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Mutluay, F.K.; Demir, R.; Ozyilmaz, S.; Caglar, A.T.; Altintas, A.; Gurses, H.N. Breathing-enhanced upper extremity exercises for patients with multiple sclerosis. Clin. Rehabil. 2007, 21, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Davies, C.; Spence, J.; Vandelanotte, C.; Caperchione, C.; Mummery, K. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- Dlugonski, D.; Motl, R.W.; Mohr, D.C.; Sandroff, B.M. Internet-delivered behavioral intervention to increase physical activity in persons with multiple sclerosis: Sustainability and secondary outcomes. Psychol. Health Med. 2012, 17, 636–651. [Google Scholar] [CrossRef] [PubMed]
- Dlugonski, D.; Motl, R.W.; McAuley, E. Increasing physical activity in multiple sclerosis: Replicating Internet intervention effects using objective and self-report outcomes. J. Rehabil. Res. Dev. 2011, 48, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.W.; Dlugonski, D.; Wojcicki, T.R.; McAuley, E.; Mohr, D.C. Internet intervention for increasing physical activity in persons with multiple. Mult. Scler. 2011, 17, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Ertekin, O.; Ozakbas, S.; Idiman, E.; Algun, Z.C. Quality of life, fatigue and balance improvements after home-based exercise program in multiple sclerosis patients. Arch. Neuropsychiatry 2012, 49, 33–38. [Google Scholar]
- Romberg, A.; Virtanen, A.; Ruutiainen, J. Long-term exercise improves functional impairment but not quality of life in multiple sclerosis. J. Neurol. 2005, 252, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Wonneberger, M. Long-term endurance exercise improves aerobic capacity in patients with relapsing-remitting multiple sclerosis: Impact of baseline fatigue. J. Neurol. Sci. 2014, 336, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Sosnoff, J.J.; Finlayson, M.; McAuley, E.; Morrison, S.; Motl, R.W. Home-based exercise program and fall-risk reduction in older adults with multiple sclerosis: Phase 1 randomized controlled trial. Clin. Rehabil. 2014, 28, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Learmonth, Y.C.; Marshall-Mckenna, R.; Paul, L.; Mattison, P.; Miller, L. A qualitative exploration of the impact of a 12-week group exercise class for those moderately affected with multiple sclerosis. Disabil. Rehabil. 2013, 35, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.A.; Lewis, L.K.; Ferrar, K.; Marshall, S.; de Bourdeaudhuij, I.; Vandelanotte, C. Are health behavior change interventions that use online social networks effective? A systematic review. J. Med. Internet Res. 2014, 16, e40. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.; Griffin, M. The use of gaming technology for rehabilitation in people with multiple sclerosis. Mult. Scler. 2015, 21, 355–371. [Google Scholar] [CrossRef] [PubMed]
- Stout, R.; Wirtz, P.; Carbonari, J.; Del Boca, F. Ensuring balanced distribution of prognostic factors in treatment outcome research. J. Stud. Alcohol 1994, S12, 70–75. [Google Scholar] [CrossRef]
- Streber, R.; Peters, S.; Pfeifer, K. Systematic review of correlates and determinants of physical activity in persons with multiple sclerosis. Arch. Phys. Med. Rehabil. 2016, 97, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Tallner, A.; Mäurer, M.; Pfeifer, K. Körperliche Aktivität bei Personen mit Multipler Sklerose in Deutschland. Neurol. Rehabil. 2013, 19, 236–243. [Google Scholar]
- Gold, S.M.; Heesen, C.; Schulz, H.; Guder, U.; Mönch, A.; Gbadamosi, J.; Buhmann, C.; Schulz, K.H. Disease specific quality of life instruments in multiple sclerosis: Validation of the Hamburg Quality of Life Questionnaire in Multiple Sclerosis (HAQUAMS). Mult. Scler. 2001, 7, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Flachenecker, P.; Müller, G.; König, H.; Meissner, H.; Toyka, K.V.; Rieckmann, P. “Fatigue” in multiple sclerosis. Development and and validation of the “Würzburger Fatigue Inventory for MS”. Nervenarzt 2006, 77, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Wagner, P.; Singer, R. Ein fragebogen zur erfassung der habituellen körperlichen aktivität verschiedener bevölkerungsgruppen. Sportwissenschaft 2003, 33, 383–397. [Google Scholar]
- Tallner, A. Körperliche Aktivität und körperliche Funktionsfähigkeit—Erfassung und Wechselwirkungen bei Personen mit Multipler Sklerose. Doctoral’s Thesis, Universität Erlangen-Nürnberg, Erlangen, Germany, 2012. [Google Scholar]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Kiselka, A.; Greisberger, A.; Heller, M. Perception of muscular effort in multiple sclerosis. NeuroRehabilitation 2013, 32, 415–423. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov (accessed on 28 September 2016).


| Title | Intervention Group (n = 59) | Control Group (n = 67) | Total Sample (n = 126) | Difference Between Groups a |
|---|---|---|---|---|
| Number | ||||
| Female | 44 (75%) | 50 (75%) | 94 (75%) | NA |
| Male | 15 (25%) | 17 (25%) | 32 (25%) | NA |
| Type of Multiple Sclerosis | ||||
| relapsing-remitting | 52 (88%) | 57 (85%) | 109 (87%) | NA |
| secondary-progressive | 7 (12%) | 10 (15%) | 17 (13%) | NA |
| Age (Range 16–76) | 40.9 (10.4) | 40.7 (9.5) | 40.8 (9.9) | p = 0.895 |
| Duration of disease | 9.8 (9.2) | 9.2 (7.2) | 9.5 (8.2) | p = 0.651 |
| EDSS | 2.8 (0.8) | 2.7 (0.8) | 2.7 (0.8) | p = 0.529 |
| Outcome | Intervention Group | Control Group | ||||
|---|---|---|---|---|---|---|
| Baseline | Three-Month | Six-Month | Baseline | Three-Month | Six-Month | |
| HRQoL | 1.84 (0.42) | 1.85 (0.49) | 1.87 (0.49) | 1.79 (0.4) | 1.83 (0.42) | 1.78 (0.43) |
| Fatigue | 21.3 (12.9) | 19.05 (14.4) | 23.87 (15.0) | 23.5 (16.3) | 21.93 (15.3) | 20.56 (14.9) |
| Aerobic fitness (VO2peak) | 25.3 (6.1) | 25.66 (5.39) | 25.32 (6.63) | 25.2 (6.5) | 24.91 (6.29) | 25.51 (6.68) |
| Forced vital capacity (L) | 4.0 (0.9) | 4.18 (0.86) | 4.17 (0.77) | 4.18 (0.96) | 4.17 (0.99) | 4.22 (1.00) |
| Peak expiratory flow (L/sec) | 6.0 (1.53) | 6.41 (1.43) | 6.54 (1.56) | 6.78 (1.69) | 6.72 (1.59) | 6.94 (1.58) |
| Knee extension (Nm) | 287 (100) | 302.81 (93) | 311.1 (100) | 298 (118) | 292.98 (113) | 292.07 (111) |
| Knee flexion (Nm) | 156 (50) | 177.71 (59) | 181.45 (52) | 171 (65) | 175.3 (63) | 179.05 (62) |
| Trunk extension (Nm) | 169 (62) | 169.88 (59) | 181.66 (58) | 168 (67) | 169.26 (72) | 173.24 (69) |
| Trunk flexion (Nm) | 86 (32) | 91.41 (32) | 95.17 (31) | 85 (36) | 88.32 (38) | 91.07 (39) |
| Sport score | 2.3 (2.47) | 3.24 (2.73) | 3.36 (2.33) | 2.1 (2.43) | 1.9 (2.39) | 2.86 (2.89) |
| Outcome | Intervention Group (Time Effect) | Control Group (Time Effect) | Between Group Difference (Group × Time) | |||
|---|---|---|---|---|---|---|
| Mean Change [95% CI] | ES, p-Value | Mean Change [95% CI] | ES, p-Value | Difference of Mean Changes a [95% CI] | ES, p-Value | |
| HRQoL | ||||||
| Three-month | 0.02 [−0.06, 0.11] | 0.08, p = 0.58 | 0.03 [−0.04, 0.11] | 0.11, p =0.40 | −0.01 [−0.12, 0.10] | −0.01, p = 0.88 |
| Six-month | 0.04 [−0.06, 0.13] | 0.13, p = 0.45 | −0.05 [−0.14, 0.03] | −0.18, p = 0.25 | ||
| Fatigue | ||||||
| Three-month | −2.06 [−5.74, 1.62] | −0.16, p = 0.28 | −1.81 [−5.11, 1.49] | −0.14, p = 0.29 | −0.25 [−5.19, 4.69] | −0.01, p = 0.92 |
| Six-month | 5.3 [1.15, 9.46] | 0.42, p = 0.02 | −1.3 [−5.03, 2.43] | −0.1, p = 0.50 | ||
| Aerobic fitness (VO2peak) | ||||||
| Three-month | 0.13 [−0.83, 1.08] | 0.04, p = 0.80 | −0.33 [−1.19, 0.54] | −0.1, p = 0.46 | 0.45 [−0.84, 1.74] | 0.07, p = 0.49 |
| Six-month | −0.34 [−1.46, 0.78] | −0.11, p = 0.55 | 0.71 [−0.28, 1.71] | 0.23, p = 0.17 | ||
| Forced vital capacity (L) | ||||||
| Three-month | −0.03 [−0.12, 0.05] | −0.11, p = 0.46 | −0.02 [−0.1, 0.06] | −0.06, p = 0.657 | −0.01 [−0.13, 0.1] | −0.02, p = 0.81 |
| Six-month | −0.01 [−0.11, 0.09] | −0.03, p = 0.84 | 0.05 [−0.04, 0.14] | 0.19, p = 0.25 | ||
| Peak expiratory flow (L/sec) | ||||||
| Three-month | 0.36 [0.07, 0.65] | 0.35, p = 0.02 | −0.06 [−0.33, 0.21] | −0.06, p = 0.65 | 0.42 [0.03, 0.82] | 0.2, p = 0.04 |
| Six-month | 0.12 [−0.22, 0.46] | 0.12, p = 0.49 | 0.23 [-0.08, 0.53] | 0.23, p = 0.16 | ||
| Knee extension (Nm) | ||||||
| Three-month | 20.52 [7.56, 33.48] | 0.46, p = 0.003 | −1.39 [−12.91, 10.13] | −0.03, p=0.81 | 21.91 [4.57, 39.24] | 0.24, p = 0.02 |
| Six-month | 5.11 [−9.96, 20.18] | 0.11, p = 0.51 | 0.04 [−13.29, 13.38] | 0.0, p = 0.99 | ||
| Knee flexion (Nm) | ||||||
| Three-month | 19.61 [12.03, 27.19] | 0.76, p = 0.00 | 3.62 [−3.11, 10.35] | 0.14, p = 0.30 | 16 [5.86, 26.13] | 0.3, p = 0.003 |
| Six-month | 2.34 [−6.39, 11.07] | 0.09, p = 0.60 | 4.17 [−3.55, 11.89] | 0.16, p = 0.30 | ||
| Trunk extension (Nm) | ||||||
| Three-month | −1.11 [−9.53, 7.31] | −0.04, p = 0.80 | 0.02 [−7.54, 7.57] | 0, p = 0.99 | −1.13 [−12.44, 10.18] | −0.02, p = 0.85 |
| Six-month | 10.21 [0.56, 19.86] | 0.36, p = 0.05 | 4.46 [−4.1, 13.02] | 0.16, p = 0.31 | ||
| Trunk flexion (Nm) | ||||||
| Three-month | 6.29 [2.65, 9.93] | 0.5, p = 0.001 | 3.95 [0.69, 7.21] | 0.31, p = 0.02 | 2.34 [−2.55, 7.22] | 0.09, p = 0.35 |
| Six-month | 3.2 [−1.01, 7.41] | 0.26, p = 0.15 | 2.93 [-0.8, 6.66] | 0.24, p = 0.13 | ||
| Sport score | ||||||
| Three-month | 0.91 [0.44, 1.37] | 0.55, p = 0.00 | −0.19 [−0.61, 0.24] | −0.11, p = 0.393 | 1.09 [0.46, 1.73] | 0.33, p = 0.001 |
| Six-month | 0.12 [−0.41, 0.66] | 0.08, p = 0.65 | 0.96 [0.47, 1.45] | 0.59, p = 0.00 | ||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tallner, A.; Streber, R.; Hentschke, C.; Morgott, M.; Geidl, W.; Mäurer, M.; Pfeifer, K. Internet-Supported Physical Exercise Training for Persons with Multiple Sclerosis—A Randomised, Controlled Study. Int. J. Mol. Sci. 2016, 17, 1667. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17101667
Tallner A, Streber R, Hentschke C, Morgott M, Geidl W, Mäurer M, Pfeifer K. Internet-Supported Physical Exercise Training for Persons with Multiple Sclerosis—A Randomised, Controlled Study. International Journal of Molecular Sciences. 2016; 17(10):1667. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17101667
Chicago/Turabian StyleTallner, Alexander, René Streber, Christian Hentschke, Marc Morgott, Wolfgang Geidl, Mathias Mäurer, and Klaus Pfeifer. 2016. "Internet-Supported Physical Exercise Training for Persons with Multiple Sclerosis—A Randomised, Controlled Study" International Journal of Molecular Sciences 17, no. 10: 1667. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17101667