Non-Intensive Care Unit Acquired Pneumonia: A New Clinical Entity?
Abstract
:1. Search Strategy and Selection Criteria
2. Introduction
3. Epidemiology
4. Risk Factors for NIAP
5. Physiopathology
6. Causative Pathogens
7. Clinical Presentation and Diagnosis
8. Microbiological Evaluation
9. Biomarkers
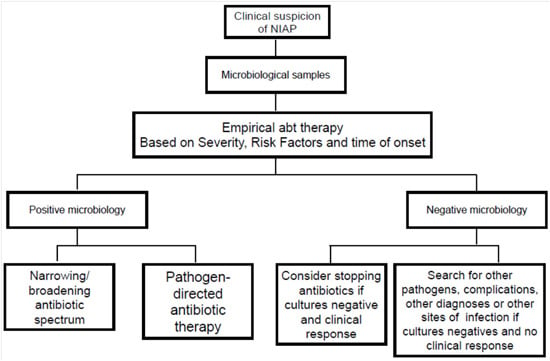
10. Treatment
10.1. De-Escalation and Withdrawal
10.2. Response to Treatment
10.3. Duration of Therapy
11. Prevention
12. Conclusions and Research Needs
Author Contributions
Conflicts of Interest
References
- Flanders, S.A.; Collard, H.R.; Saint, S. Nosocomial pneumonia: State of the science. Am. J. Infect. Control 2006, 34, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Ewig, S.; Lode, H.; Carlet, J.; European HAP working group. Defining, treating and preventing hospital acquired pneumonia. Intensive Care Med. 2009, 35, 9–29. [Google Scholar] [CrossRef] [PubMed]
- Craven, D.E.; Chroneou, A. Nosocomial pneumonia. In Principles and Practice of Infectious Diseases, 7th ed.; Madell, G.L., Benett, J.E., Dolin, R., Eds.; Elsevier Churchill Livingstone: Philadelphia, PA, USA, 2009; pp. 3717–3724. [Google Scholar]
- Leroy, O.; Soubrier, S. Hospital-acquired pneumonia: Risk factors, clinical features, management and antibiotic resistance. Curr. Opin. Pulm. Med. 2004, 10, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.P. Hospital-acquired pneumonia: Risk factors, microbiology, and treatment. Chest 2001, 119, 373S–384S. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am. J. Respir. Crit. Care Med. 2005, 171, 388–416. [Google Scholar]
- Woodhead, M.; Blasi, F.; Ewig, S.; Garau, J.; Huchon, G.; Ieven, M.; Ortqvist, A.; Schaberg, T.; Torres, A.; van der Heijden, G.; et al. Guidelines for the management of adult lower respiratory tract infections. Clin. Microbiol. Infect. 2011, 17, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, S.; di Pasquale, M.; Zanaboni, A.M.; Cosentini, R.; Brambilla, A.M.; Seghezzi, S.; Tarsia, P.; Mantero, M.; Blasi, F. Stratifying risk factors for multidrug-resistant pathogens in hospitalized patients coming from the community with pneumonia. Clin. Infect. Dis. 2012, 54, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, S.; Cilloniz, C.; Chalmers, J.D.; Zanaboni, A.M.; Cosentini, R.; Tarsia, P.; Pesci, A.; Blasi, F.; Torres, A. Multidrug-resistant pathogens in hospitalized patients coming from the community with pneumonia: A European perspective. Thorax 2013, 68, 997–999. [Google Scholar] [CrossRef] [PubMed]
- Sopena, N.; Heras, E.; Casas, I.; Bechini, J.; Guasch, I.; Pedro-Botet, M.L.; Roure, S.; Sabrià, M. Risk factors for hospital-acquired pneumonia outside the intensive care unit: A case-control study. Am. J. Infect. Control 2014, 42, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Sopena, N.; Sabrià, M. Neunos 2000 Study Group. Multicenter study of hospital-acquired pneumonia in non-ICU patients. Chest 2005, 127, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Everts, R.J.; Murdoch, D.R.; Chambers, S.T.; Town, G.I.; Withington, S.G.; Martin, I.R.; Frampton, C.; Chereshsky, A.Y.; Schousboe, M.I. Nosocomial pneumonia in adult general medical and surgical patients at Christchurch Hospital. N. Z. Med. J. 2000, 113, 221–224. [Google Scholar] [PubMed]
- Barreiro-Lopez, B.; Tricas, J.M.; Mauri, E.; Quintana, S.; Garau, J. Risk factors and prognostic factors of nosocomial pneumonia outside the intensive care units. Enfermedades Infecc. Med. Clin. 2005, 23, 519–525. (In Spanish) [Google Scholar]
- Weber, D.J.; Rutala, W.A.; Sickbert-Bennet, E.E.; Samsa, G.P.; Brown, V.; Niederman, M.S. Microbiology of ventilator-associated pneumonia compared with that of hospital-acquired pneumonia. Infect. Control Hosp. Epidemiol. 2007, 28, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Herer, B.; Fuhrman, C.; Gazevic, Z.; Cabrit, R.; Chouaïd, C. Management of nosocomial pneumonia on a medical ward: A comparative study of outcomes and costs of invasive procedures. Clin. Microbiol. Infect. 2009, 15, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Bonten, J.M.; Bergman, D.C. Nosocomial Pneumonia. In Hospital Epidemiology and Infection Control, 2nd ed.; Mayhall, C.G., Ed.; Williams and Wilkins: Philadelphia, PA, USA, 1999; pp. 211–238. [Google Scholar]
- Dziedzic, T.; Pera, J.; Klimkowicz, A.; Turaj, W.; Slowik, A.; Rog, T.M.; Szczudlik, A. Serum albumin level and nosocomial pneumonia in stroke patients. Eur. J. Neurol. 2006, 13, 299–301. [Google Scholar] [CrossRef] [PubMed]
- Herzig, S.; Howell, M.; Ngo, L.; Marcantonio, E.R. Acid-suppressive medication use and the risk for hospital-acquired pneumonia. JAMA 2009, 301, 2120–2128. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.-L. Prevention of nosocomial bacterial pneumonia. Thorax 1999, 54, 544–549. [Google Scholar] [CrossRef] [PubMed]
- Rice, L. Evolution and clinical importance of extended-spectrum betalactamases. Chest 2001, 119, 391S–396S. [Google Scholar] [CrossRef] [PubMed]
- Loeb, M.B. Pneumonia in nursing homes and long-term care facilities. Semin. Respir. Crit. Care Med. 2005, 26, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Quagliarello, V.; Ginter, S.; Han, L.; van Ness, P.; Allore, H.; Tinetti, M. Modifiable risk factors for nursing home-acquired pneumonia. Clin. Infect. Dis. 2005, 40, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Fiore, A.E.; Butler, J.C.; Emori, T.G.; Gaynes, R.P. A survey of methods used to detect nosocomial legionellosis among participants in the National Nosocomial Infections Surveillance System. Infect. Control Hosp. Epidemiol. 1999, 20, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Denning, D.W. Invasive aspergillosis. Clin. Infect. Dis. 1998, 26, 781–805. [Google Scholar] [CrossRef] [PubMed]
- Grayston, J.T.; Diwan, W.K.; Cooney, M.; Wang, S.P. Community and hospital acquired pneumonia associated with Chlamydia TWAR infection demonstrated serologically. Arch. Intern. Med. 1989, 149, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Claessens, Y.E.; Debray, M.P.; Tubach, F.; Brun, A.L.; Rammaert, B.; Hausfater, P.; Naccache, J.M.; Ray, P.; Choquet, C.; Carette, M.F.; et al. Early chest computed tomography scan to assist diagnosis and guide treatment decision for suspected community-acquired pneumonia. Am. J. Respir. Crit. Care Med. 2015, 192, 974–982. [Google Scholar] [CrossRef] [PubMed]
- Fagon, J.Y.; Chastre, J.; Wolff, M.; Gervais, C.; Parer-Aubas, S.; Stéphan, F.; Similowski, T.; Mercat, A.; Diehl, J.L.; Sollet, J.P.; et al. Invasive and noninvasive strategies for management of suspected ventilator-associated pneumonia. A randomized trial. Ann. Intern. Med. 2000, 132, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Polzin, A.; Pletz, M.; Erbes, R.; Raffenberg, M.; Mauch, H.; Wagner, S.; Arndt, G.; Lode, H. Procalcitonin as a diagnostic tool in lower respiratory tract infections and tuberculosis. Eur. Respir. J. 2003, 21, 939–943. [Google Scholar] [CrossRef] [PubMed]
- Kollef, M.H.; Sherman, G.; Ward, S.; Fraser, V.J. Inadequate antimicrobial treatment of infections: A risk factor for hospital mortality among critically ill patients. Chest 1999, 115, 462–474. [Google Scholar] [CrossRef] [PubMed]
- Sabrià, M.; Sopena, N. “HAP in nonventilated patients”, nosocomial and ventilator-associated pneumonia. ERS Monogr. 2011, 53. [Google Scholar] [CrossRef]
- Nobre, V.; Harbarth, S.; Graf, J.D.; Rohner, P.; Pugin, J. Use of procalcitonin to shorten antibiotic treatment duration in septic patients: A randomized trial. Am. J. Respir. Crit. Care Med. 2008, 177, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, S.; Blasi, F.; Zanaboni, A.M.; Peyrani, P.; Tarsia, P.; Gaito, S.; Ramirez, J.A. Duration of antibiotic therapy in hospitalized patients with community-acquired pneumonia. Eur. Respir. J. 2010, 36, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, S.; Giuliani, F.; Ramirez, J.; Blasi, F. DURATION Study Group. How to choose the duration of antibiotic therapy in patients with pneumonia. Curr. Opin. Infect. Dis. 2015, 28, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Takano, Y.; Sakamoto, O.; Suga, M.; Muranaka, H.; Ando, M. Prognostic factors of nosocomial pneumonia in general wards: A prospective multivariate analysis in Japan. Respir. Med. 2002, 96, 16–23. [Google Scholar] [CrossRef]
- Thompson, D.A.; Makary, M.A.; Dorman, T.; Pronovost, P.J. Clinical and economic outcomes of hospital acquired pneumonia in intra-abdominal surgery patients. Ann. Surg. 2006, 243, 547–552. [Google Scholar] [CrossRef]
- Tablan, O.C.; Anderson, L.J.; Besser, R.; Bridges, C.; Hajjeh, R.; CDC; Healthcare infection control practices advisory committee. Guidelines for preventing health-care associated pneumonia, 2003: Recommendations of the CDC and the healthcare infection control practices advisory committee. MMWR Recomm. Rep. 2004, 53, 1–36. [Google Scholar] [PubMed]
- Pittet, D.; Hugonnet, S.; Harbarth, S.; Mourouga, P.; Sauvan, V.; Touveneau, S.; Perneger, T.V. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene: Infection control programme. Lancet 2000, 356, 1307–1312. [Google Scholar] [CrossRef]
- Terpenning, M. Geriatric oral health and pneumonia risk. Clin. Infect. Dis. 2005, 40, 1807–1810. [Google Scholar] [CrossRef] [PubMed]
- Yoneyama, T.; Yoshida, M.; Ohrui, T.; Mukaiyama, H.; Okamoto, H.; Hoshiba, K.; Ihara, S.; Yanagisawa, S.; Ariumi, S.; Morita, T. Oral care reduces pneumonia in older patients in nursing homes. J. Am. Geriatr. Soc. 2002, 50, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Aliberti, S.; Ramirez, J.; Cosentini, R.; Valenti, V.; Voza, A.; Rossi, P.; Stolz, D.; Legnani, D.; Pesci, A.; Richeldi, L.; et al. Acute myocardial infarction vs. other cardiovascular events in community-acquired pneumonia. ERJ Open Res. 2015, 1. [Google Scholar] [CrossRef]
- Aliberti, S.; Ramirez, J.A. Cardiac diseases complicating community-acquired pneumonia. Curr. Opin. Infect. Dis. 2014, 27, 295–301. [Google Scholar] [CrossRef] [PubMed]





| Author | Year of Publication | Study | Study Setting | Number of pts Enrolled | Incidence/Prevalence of NIAP | Most Frequent Pathogens Isolated in NIAP |
|---|---|---|---|---|---|---|
| Sopena et al. [10] | 2014 | Incident case-control study | Spain, 600-bed tertiary hospital | 119 cases with NIAP and 238 controls | 2.45 cases/1000 hospital admissions | S. pneumoniae 13%, Enterobacteriaceae 8%, P. aeruginosa 3%, MRSA 3% |
| Herer et al. [15] | 2009 | Randomized control trial | France, 411-bed facility | 68 pts with NIAP | / | Staphylococcus aureus 25.4%, MSSA 25%, P. aeruginosa 19% |
| Weber et al. [14] | 2007 | Prospective, observational study | USA, a tertiary care academic hospital | 556 pts (588 episodes of pneumonia): VAP 309 pts (327 episodes) NIAP 247 pts (261 episodes) | / | Gram-positive cocci (42.59% [MSSA, 13.33%]; [MRSA, 20.37%]), P. aeruginosa 9% |
| Barreiro-Lopez et al. [13] | 2005 | Prospective case-control study | Spain | 67 pts with NIAP | 3.35 cases/1000 admissions | / |
| Sopena et al. [11] | 2005 | Multicenter, prospective, observational study | Spain, 12 teaching hospitals | 186 patients with NIAP | 3 ± 1.4 cases/1000 hospital admissions | S. pneumoniae, 9.7%, Enterobacteriaceae 5%, P. aeruginosa 4% |
| Everts et al. [12] | 2000 | Prospective observational study | New Zealand, university-affiliated hospital | 126 pts with NIAP | 6.1 cases/1000 admissions | Legionella spp., 13%, MSSA 3% |
| Penicillin-Resistant Pneumococci | Age > 65 years | Betalactam-Therapy (last 3 month) | Alcoholism | Immune Suppressive Illness | Multiple Comorbidities |
|---|---|---|---|---|---|
| Gram-negative bacilli | Chronic underlying disease | Multiple comorbidities | Residence in a NH | Recent antibiotic therapy | |
| P. aeruginosa and multi resistant Gram-negative bacilli | Wide spectrum antibiotics | Severe underlying disease | Prior broad spectrum abt therapy | Structural lung disease | Corticosteroid therapy |
| Legionella | Hospital potable water | Previous nosocomial Legionellosis | ‒ | ‒ | ‒ |
| Anaerobes | Gengivitis or periodontal disease | Swallowing disorders | Depressed consciousness | Orotracheal manipulation | ‒ |
| MRSA | Intravascular devices | Nasal carriage | High prevalence | ‒ | ‒ |
| Aspergillus | Corticosteroid therapy | Neutropenia | Transplantation | ‒ | ‒ |
| Beta-lactams * + aminoglycoside Or quinolone | SEVERE NIAP NIAP WITH RISK FACTORS FOR P. aeruginosa Gram negative bacilli |
| Antipseudomonal cephalosporin Or Fluoroquinolones | LATE ONSET NIAP <5 days |
| Beta-lactam/beta-lactamase inhibitor Or Third generation non-pseudomonal cephalosporin: Or Fluoroquinolones | EARLY ONSET NIAP <5 days |
| Levofloxacin Or azitromycin | LEGIONELLA SPP: |
| Carbapenems Or b-lactam/b-lactamase inhibitor | ANAEROBES |
| Vancomycin Or Linezolid | MRSA (Methicillin resistant S. aureus) |
| Amphotericyn B desoxicolate Or amphotericyn liposomal Or Voriconazol | ASPERGILLUS SPP. |
| NIAP | VAP/NVICUAP | |
|---|---|---|
| Diagnosis | New infiltrate on CXR after 48 h of hospital admission +: fever, dyspnea, cough and purulent expectoration, leukocytosis or leukopenia | New or worsening infiltrates on CXR after 48 h after initiation of invasive mechianical ventilation/admission to ICU admission + fever worsening of PaO2/FiO2 purulent tracheal secretions leukocytosis or leukopenia |
| Stratification | Severe NIAP NIAP with risk factors Early onset NIAP Late onset NIAP | Ventilated patient/spontaneously breathing patient Late vs. early onset Presence of risk factors |
| Microbiological tests | Blood cultures Urinary Antigens Sputum Tracheal aspirate | Blood cultures PBS BAL BAS |
| Etiology | S. pneumoniae Enterobacteriaceae P. aeruginosa S. aureus Legionella pn. | Early onset: S. aureus, S. pneumoniae, H. influenzae, non-drug resistant GNEB Late onset: MRSA, drug resistant GNEB, P. aeruginosa, A. baumannii |
| Empirical therapy | Severe NIAP: b-lactams with an aminoglycoside or fluoroquinolone Early onset NIAP: b-lactam/b-lactamase inhibitor or third generation non-pseudomonal cephalosporin, or fluoroquinolones Late onset NIAP: Antipseudomonal cephalosporin Fluoroquinolones NIAP with risk factors: specific for each organism | Early onset: aminopenicillin plus b-lactamase-inhibitor Or third generation cephalosporin Or quinolones Late onset: antipseudomonal penicillin Or antipseudomonal cephalosporin Or carbapenems Plus quinolone if MRSA suspected Vancomycin Or Linezolid Antimicrobial treatment of pneumonia with risk factors, any onset: specific for each organism |
| Prevention | Interventions to modify individual risk factors, such as malnutrition, anemia, and risk of aspiration Hand hygiene Isolation of MDR patients | Avoid intubation Semi-recumbent position to decrease aspiration of oropharyngeal secretions Oral hygiene with chlorhexidine Probiotics Specialized endotracheal tubes (subglottic secretion drainage; silvercoated) |
| In-hospital mortality | One third of cases | 20% to 70%, depending on the characteristics of the patient and the microorganism involved |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Pasquale, M.; Aliberti, S.; Mantero, M.; Bianchini, S.; Blasi, F. Non-Intensive Care Unit Acquired Pneumonia: A New Clinical Entity? Int. J. Mol. Sci. 2016, 17, 287. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17030287
Di Pasquale M, Aliberti S, Mantero M, Bianchini S, Blasi F. Non-Intensive Care Unit Acquired Pneumonia: A New Clinical Entity? International Journal of Molecular Sciences. 2016; 17(3):287. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17030287
Chicago/Turabian StyleDi Pasquale, Marta, Stefano Aliberti, Marco Mantero, Sonia Bianchini, and Francesco Blasi. 2016. "Non-Intensive Care Unit Acquired Pneumonia: A New Clinical Entity?" International Journal of Molecular Sciences 17, no. 3: 287. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17030287