Preparation and Characterization of Resorbable Bacterial Cellulose Membranes Treated by Electron Beam Irradiation for Guided Bone Regeneration
Abstract
:1. Introduction
2. Results and Discussion
2.1. Characterization of EI-BCMs
2.1.1. Scanning Electron Microscopy
2.1.2. Mechanical Properties Analyses
2.1.3. Attenuated Total Reflection-Fourier Transform Infrared Spectroscopy (ATR-FTIR)
2.1.4. Thermogravimetric Analyses (TGAs)
2.1.5. In Vitro Degradation
2.2. In Vitro Cell Studies
2.2.1. Cell Proliferation Assay
2.2.2. Immunofluorescent Staining and FE-SEM Analyses of Cells on BCMs
2.3. In Vivo Animal Studies
2.3.1. Histologic Findings
2.3.2. Histometric Analyses
3. Materials and Methods
3.1. Preparation of Bacterial Cellulose Membranes (BCMs)
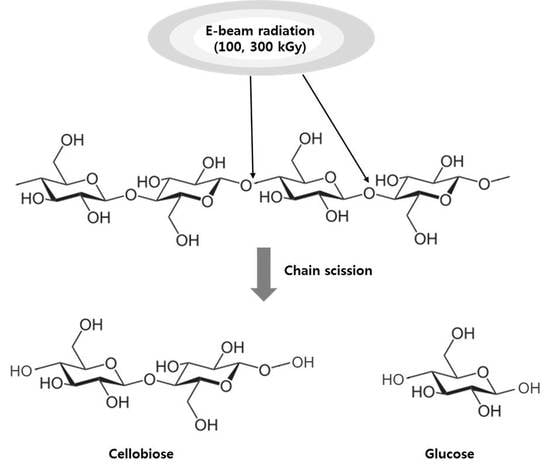
3.2. Fabrication of Electron Beam Irradiated BCMs (EI-BCMs)
3.3. Characterization of EI-BCMs
3.3.1. Scanning Electron Microscope (SEM) Image Analysis of BCMs
3.3.2. Mechanical Properties
3.3.3. Attenuated Total Reflection-Fourier Transform Infrared Spectroscopy (ATR-FTIR)
3.3.4. Thermogravimetric Analysis (TGA)
3.3.5. In Vitro Degradation of EI-BCMs
3.4. In Vitro Cell Studies
3.4.1. Cell Proliferation Assay
3.4.2. Immunofluorescent Staining
3.4.3. Field Emission-Scanning Electron Microscopy(FE-SEM) of Surface Cells
3.5. In Vivo Animal Studies
3.5.1. Experimental Animals
3.5.2. Surgical Procedures
3.5.3. Post-Operative Care and Sacrifice
3.5.4. Histometric Analysis
3.5.5. Statistical Analyses
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| BC | Bacterial cellulose |
| EI | Electron beam |
| EI-BCM | Electron beam irradiated BC membrane |
| NI-BCM | Unirradiated BC membrane |
| GBR | Guided bone regeneration |
| CM | Collagen membrane |
| SEM | Scanning electron microscopy |
| FE-SEM | Field emission-scanning electron microscope |
| ATR-FTIR | Attenuated total reflection-Fourier transform infrared spectroscopy analyses |
| TGA | Thermal gravimetric analyses |
| NBA | New bone area |
| PTFE | Polytetrafluoroethylene |
| PGA | Polyglycolic acid |
| PLA | Polylactic acid |
| 3D | Three dimension |
| PBS | Phosphate buffered saline |
| SBF | Simulated body fluid |
| HA/β-TCP | Hydroxyapatite/β-tricalcium phosphate |
| EDTA | Ethylenediaminetetraacetic acid |
References
- Gottlow, J.; Nyman, S.; Karring, T.; Lindhe, J. New attachment formation as the result of controlled tissue regeneration. J. Clin. Periodontol. 1984, 11, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Misch, C.M. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int. J. Oral Maxillofac. Implant 1997, 12, 767–776. [Google Scholar]
- Hämmerle, C.H.; Karring, T. Guided bone regeneration at oral implant sites. Periodontol 2000 1998, 17, 151–175. [Google Scholar] [CrossRef] [PubMed]
- Laino, L.; Iezzi, G.; Piattelli, A.; Muzio, L.L.; Cicciù, M. Vertical ridge augmentation of the atrophic posterior mandible with sandwich technique: Bone block from the chin area versus corticocancellous bone block allograft—Clinical and histological prospective randomized controlled study. BioMed Res. Int. 2014, 2014, 982104. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Herford, A.S.; Cicciù, D.; Tandon, R.; Maiorana, C. Recombinant human bone morphogenetic protein-2 promote and stabilize hard and soft tissue healing for large mandibular new bone reconstruction defects. J. Craniofac. Surg. 2014, 3, 860–862. [Google Scholar] [CrossRef] [PubMed]
- Petrauskaite, O.; de Sousa Gomes, P.; Fernandes, M.H.; Juodzbalys, G.; Stumbras, A.; Maminskas, J.; Liesiene, J.; Cicciù, M. Biomimetic mineralization on a microporous cellulose-based matrix for bone regeneration. BioMed Res. Int. 2013, 2013, 452750. [Google Scholar] [CrossRef] [PubMed]
- Herford, A.S.; Tandon, R.; Stevens, T.W.; Stoffella, E.; Cicciu, M. Immediate distraction osteogenesis: The sandwich technique in combination with rhBMP-2 for anterior maxillary and mandibular defects. J. Craniofac. Surg. 2013, 4, 1383–1387. [Google Scholar] [CrossRef] [PubMed]
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Rispoli, L.; Fontana, F.; Beretta, M.; Poggio, C.E.; Maiorana, C. Surgery Guidelines for Barrier Membranes in Gudied Bone Regeneration (GBR). J. Otolaryngol. Rhinol. 2015, 1, 1–8. [Google Scholar] [CrossRef]
- Kasaj, A.; Reichert, C.; Götz, H.; Röhrig, B.; Smeets, R.; Willershausen, B. In vitro evaluation of various bioabsorbable and nonresorbable barrier membranes for guided tissue regeneration. Head Face Med. 2008, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Her, S.; Kang, T.; Fien, M.J. Titanium mesh as an alternative to a membrane for ridge augmentation. J. Oral Maxillofac. Surg. 2012, 70, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Gentile, P.; Chiono, V.; Tonda-Turo, C.; Ferreira, A.M.; Ciardelli, G. Polymeric membranes for guided bone regeneration. Biotechnol. J. 2011, 6, 1187–1197. [Google Scholar] [CrossRef] [PubMed]
- Gentile, P.; Frongia, M.E.; Cardellach, M.; Miller, C.A.; Stafford, G.P.; Leggett, G.J.; Hatton, P.V. Functionalised nanoscale coatings using layer-by-layer assembly for imparting antibacterial properties to polylactide-co-glycolide surfaces. Acta Biomater. 2015, 21, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Von Arx, T.; Buser, D. Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: A clinical study with 42 patients. Clin. Oral Implants Res. 2006, 17, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Rakhmatia, U.D.; Ayukawa, Y.; Furuhashi, A.; Koyano, K. Current barrier membranes: Ti mesh and other membranes for guided bone regeneration in dental applications. J. Prosthodont. Res. 2013, 57, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Piattelli, A.; Scarano, A.; Corigliano, M.; Piattelli, M. Comparison of bone regeneration with the use of mineralized and demineralized freeze-dried bone allografts: A histological and histochemical study in man. Biomaterials 1996, 17, 1127–1131. [Google Scholar] [CrossRef]
- Kellomäki, M.; Niiranen, H.; Puumanen, K.; Ashammakhi, N.; Waris, T.; Törmälä, P. Bioabsorbable scaffolds for guided bone regeneration and generation. Biomaterials 2000, 21, 2495–2505. [Google Scholar] [CrossRef]
- Zitzmann, N.U.; Naef, R.; Schärer, P. Resorbable versus nonresorbable membranes in combination with bio-oss for guided bone regeneration. Int. J. Oral Maxillofac. Implants. 1997, 12, 844–852. [Google Scholar] [PubMed]
- Embuscado, M.E.; Marks, J.S.; BeMiller, J.N. Bacterial cellulose. II. Optimization of cellulose production by Acetobacterxylinum through response surface methodology. Food Hydrocoll. 1994, 8, 419–430. [Google Scholar] [CrossRef]
- Nishiyama, Y.; Sugiyama, J.; Chanzy, H.; Langan, P. Crystal structure and hydrogen bonding system in cellulose iα from synchrotron x-ray and neutron fiber diffraction. J. Am. Chem. Soc. 2003, 125, 14300–14306. [Google Scholar] [CrossRef] [PubMed]
- Svensson, A.; Nicklasson, E.; Harrah, T.; Panilaitis, B.; Kaplan, D.; Brittberg, M.; Gatenholm, P. Bacterial cellulose as a potential scaffold for tissue engineering of cartilage. Biomaterials 2005, 26, 419–431. [Google Scholar] [CrossRef] [PubMed]
- Gayathry, G.; Gopalaswamy, G. Production and characterisation of microbial cellulosic fibre from acetobacterxylinum. Indian J. Fibre Text. Res. 2014, 39, 93–96. [Google Scholar]
- Wu, Z.Y.; Liang, H.W.; Chen, L.F.; Hu, B.C.; Yu, S.H. Bacterial cellulose: A robust platform for design of three dimensional carbon-based functional nanomaterials. Acc. Chem. Res. 2015, 49, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Helenius, G.; Bäckdahl, H.; Bodin, A.; Nannmark, U.; Gatenholm, P.; Risberg, B. In vivo biocompatibility of bacterial cellulose. J. Biomed. Mater. Res. A 2006, 76, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Gao, C.; Han, M.; Liang, H.; Ren, K.; Wang, Y.; Luo, H. Preparation and characterization of bacterial cellulose/heparin hybrid nanofiber for potential vascular tissue engineering scaffolds. Polym. Adv. Technol. 2011, 22, 2643–2648. [Google Scholar] [CrossRef]
- Rajwade, J.M.; Paknikar, K.M.; Kumbhar, J.V. Applications of bacterial cellulose and its composites in biomedicine. Appl. Microbiol. Biotechnol. 2015, 99, 2491–2511. [Google Scholar] [CrossRef] [PubMed]
- Müller, F.A.; Müller, L.; Hofmann, I.; Greil, P.; Wenzel, M.M.; Staudenmaier, R. Cellulose-based scaffold materials for cartilage tissue engineering. Biomaterials 2006, 27, 3955–3963. [Google Scholar] [CrossRef] [PubMed]
- Dugan, J.M.; Gough, J.E.; Eichhorn, S.J. Bacterial cellulose scaffolds and cellulose nanowhiskers for tissue engineering. Nanomedicine 2013, 8, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.Z.; Huang, Y.; Yuan, C.D.; Raman, S.; Zhu, Y.; Jiang, H.J.; He, F.; Gao, C. Biomimetic synthesis of hydroxyapatite/bacterial cellulose nanocomposites for biomedical applications. Mater. Sci. Eng. C 2007, 27, 855–864. [Google Scholar] [CrossRef]
- Lee, S.H.; Lim, Y.M.; Jeong, S.I.; An, S.J.; Kang, S.S.; Jeong, C.M.; Huh, J.B. The effect of bacterial cellulose membrane compared with CM on guided bone regeneration. J. Adv. Prosthodont. 2015, 7, 484–495. [Google Scholar] [CrossRef] [PubMed]
- Zaborowska, M.; Bodin, A.; Bäckdahl, H.; Popp, J.; Goldstein, A.; Gatenholm, P. Microporous bacterial cellulose as a potential scaffold for bone regeneration. Acta Biomater. 2010, 6, 2540–2547. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.M.; Xi, T.F.; Zheng, Y.F.; Zhou, L.; Wan, Y.Z. In vitro structural changes of nano-bacterial cellulose immersed in phosphate buffer solution. J. Biomim. Biomater. Tissue Eng. 2011, 10, 55–66. [Google Scholar] [CrossRef]
- Li, J.; Wan, Y.; Li, L.; Liang, H.; Wang, J. Preparation and characterization of 2,3-dialdehyde bacterial cellulose for potential biodegradable tissue engineering scaffolds. Mater. Sci. Eng. A 2009, 29, 1635–1642. [Google Scholar] [CrossRef]
- Czaja, W.K.; Kyryliouk, D.; DePaula, C.A.; Buechter, D.D. Oxidation of γ-irradiated microbial cellulose results in bioresorbable, highly conformable biomaterial. J. Appl. Polym. Sci. 2014, 131, 39995. [Google Scholar] [CrossRef]
- Hu, Y.; Catchmark, J.M. In vitro biodegradability and mechanical properties of bioabsorbable bacterial cellulose incorporating cellulases. Acta Biomater. 2011, 7, 2835–2845. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Hamid, S.; Zain, S. Conversion of lignocellulosic biomass to nanocellulose: Structure and chemical process. Sci. World J. 2014, 2014, 631013. [Google Scholar] [CrossRef] [PubMed]
- Darwis, D.; Khusniya, T.; Hardiningsih, L.; Nurlidar, F.; Winarno, H. In Vitro degradation behaviour of irradiated bacterial cellulose membrane. Atom Indones. 2013, 38, 78–82. [Google Scholar] [CrossRef]
- Chmielewski, A. Worldwide developments in the field of radiation processing of materials in the down of 21st century. Nukleonika 2006, 51, 3–9. [Google Scholar]
- Földváry, C.M.; Takács, E.; Wojnarovits, L. Effect of high-energy radiation and alkali treatment on the properties of cellulose. Radiat. Phys. Chem. 2003, 67, 505–508. [Google Scholar] [CrossRef]
- Petryayev, Y.P.; Boltromeyuk, V.; Kovalenko, N.; Shadyro, O. Mechanism of radiation-initiated degradation of cellulose and derivatives. Polym. Sci. USSR 1988, 30, 2208–2214. [Google Scholar] [CrossRef]
- Lee, S.H.; An, S.J.; Lim, Y.M.; Huh, J.B. The Efficacy of electron beam irradiated bacterial cellulose membranes as compared with collagen membranes on guided bone regeneration in peri-implant bone defects. Materials 2017, 10, 1018. [Google Scholar] [CrossRef] [PubMed]
- Khan, R.A.; Beck, S.; Dussault, D.; Salmieri, S.; Bouchard, J.; Lacroix, M. Mechanical and barrier properties of nanocrystalline cellulose reinforced poly (caprolactone) composites: Effect of gamma radiation. J. Appl. Polym. Sci. 2013, 129, 3038–3046. [Google Scholar] [CrossRef]
- Bartee, B.K.; Carr, J. Evaluation of a high-density polytetrafluoroethylene (n-PTFE) membrane as a barrier material to facilitate guided bone regeneration in the rat mandible. J. Oral Implantol. 1995, 21, 88–95. [Google Scholar] [PubMed]
- Fujihara, K.; Kotaki, M.; Ramakrishna, S. Guided bone regeneration membrane made of polycaprolactone/calcium carbonate composite nano-fibers. Biomaterials 2005, 26, 4139–4147. [Google Scholar] [CrossRef] [PubMed]
- Hegazy, E.; Abdel-Rehim, H.; Diaa, D.; El-Barbary, A. Controlling of degradation effects in radiation processing of polymers. In Controlling of Degradation Effects in Radiation Processing of Polymers; IAEA: Vienna, Austria, May 2009; pp. 67–84. [Google Scholar]
- Ershov, B.G. Radiation-chemical degradation of cellulose and other polysaccharides. Russ. Chem. Rev. 1998, 67, 315–334. [Google Scholar] [CrossRef]
- Von Sonntag, C. Free-radical-induced chain scission and cross-linking of polymers in aqueous solution—An overview. Radiat. Phys. Chem. 2003, 67, 353–359. [Google Scholar] [CrossRef]
- Webb, P.A. An Introduction to the Physical Characterization of Materials by Mercury Intrusion Porosimetry with Emphasis on Reduction and Presentation of Experimental Data; Micromeritics Instrument Corp.: Norcross, GA, USA, 2001. [Google Scholar]
- Eo, M.Y.; Fan, H.; Cho, Y.J.; Kim, S.M.; Lee, S.K. Cellulose membrane as a biomaterial: From hydrolysis to depolymerization with eletron beam. Biomater. Res. 2016, 20, 16. [Google Scholar] [CrossRef] [PubMed]
- Matsuhashi, S.; Kume, T.; Hashimoto, S.; Awang, M.R. Effect of gamma irradiation on enzymatic digestion of oil palm empty fruit bunch. J. Sci. Food Agric. 1995, 69, 265–267. [Google Scholar] [CrossRef]
- Ahn, S.J.; Shin, Y.M.; Kim, S.E.; Jeong, S.I.; Jeong, J.O.; Park, J.S.; Kim, C.Y. Characterization of hydroxyapatite-coated bacterial cellulose scaffold for bone tissue engineering. Biotechnol. Bioprocess Eng. 2015, 20, 948–955. [Google Scholar] [CrossRef]
- Chu, P.K.; Chen, J.Y.; Wang, L.P.; Huang, N. Plasma-surface modification of biomaterials. Mater. Sci. Eng. R Rep. 2002, 36, 143–206. [Google Scholar] [CrossRef]
- Pertile, R.; Moreira, S.; Andrade, F.; Domingues, L.; Gama, M. Bacterial cellulose modified using recombinant proteins to improve neuronal and mesenchymal cell adhesion. Biotechnol. Prog. 2012, 28, 526–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrade, F.K.; Moreira, S.M.; Domingues, L.; Gama, F.M. Improving the affinity of fibroblasts for bacterial cellulose using carbohydrate—Binding modules fused to RGD. J. Biomed. Mater. Res. A 2010, 28, 526–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Oliveira Barud, H.G.; da Silva, R.R.; da Silva Barud, H.; Tercjak, A.; Gutierrez, J.; Lustri, W.R.; Wilton, R.L.; Ribeiro, S.J. A multipurpose natural and renewable polymer in medical applications: Bacterial cellulose. Carbohydr. Polym. 2016, 153, 406–420. [Google Scholar] [CrossRef] [PubMed]
- Mendes, P.N.; Rahal, S.C.; Pereira-Junior, O.C.M.; Fabris, V.E.; Lenharo, S.L.R.; de Lima-Neto, J.F.; da Cruz Landim-Alvarenga, F. In vivo and in vitro evaluation of an Acetobacter xylinum synthesized microbial cellulose membrane intended for guided tissue repair. Acta Vet. Scand. 2009, 51, 12. [Google Scholar] [CrossRef] [PubMed]
- Mello, L.R.; Feltrin, L.T.; Neto, P.T.F.; Ferraz, F.A.P. Duraplasty with biosynthetic cellulose: An experimental study. J. Neurosurg. 1997, 86, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Herford, A.S.; Cicciù, M.; Eftimie, L.F.; Miller, M.; Signorino, F.; Famà, F.; Cervino, G.; Giudice, G.L.; Bramanti, E.; Lauritano, F.; et al. rhBMP-2 applied as support of distraction osteogenesis: A split-mouth histological study over nonhuman primates mandibles. Int. J. Clin. Exp. Med. 2016, 9, 17187–17194. [Google Scholar]
- Czaja, W.K.; Young, D.J.; Kawecki, M.; Brown, R.M. The Future prospects of microbial cellulose in biomedical applications. Biomacromolecules 2007, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Oyane, A.; Kim, H.M.; Furuya, T.; Kokubo, T.; Miyazaki, T.; Nakamura, T. Preparation and assessment of revised simulated body fluids. J. Biomed. Mater. Res. Part A 2003, 65, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.Y.; Lü, L.X.; Shi, J.C.; Wang, H.F.; Xiao, Z.D.; Huang, N.P. Introducing RGD peptides on PHBV films through peg-containing cross-linkers to improve the biocompatibility. Biomacromolecules 2011, 12, 551–559. [Google Scholar] [CrossRef] [PubMed]















| Weeks | Group (Membrane) | Mean ± SD | Median | *** p |
|---|---|---|---|---|
| 4 | CM | 17.13 ± 9.65 | 15.51 | <0.001 |
| NI-BCM | 15.82 ± 2.94 | 16.46 | ||
| 100k EI-BCM | 26.48 ± 3.78 | 25.44 | ||
| 300k EI-BCM | 26.55 ± 4.56 | 25.92 | ||
| 8 | CM | 17.47 ± 5.09 | 17.07 | <0.001 |
| NI-BCM | 16.78 ± 5.27 | 16.88 | ||
| 100k EI-BCM | 30.79 ± 3.86 | 30.70 | ||
| 300k EI-BCM | 26.47 ± 6.77 | 23.45 |
| 1× PBS (Phosphate Buffered Saline) | 5× SBF (Simulated Body Fluid) | ||||
|---|---|---|---|---|---|
| 137.0 | mM | NaCl | 710.0 | mM | Na+ |
| 2.70 | mM | KCl | 25.0 | mM | K+ |
| 10 | mM | Na2HPO4·H2O | 12.5 | mM | Ca2+ |
| 2.00 | mM | KH2PO4 | 7.5 | mM | Mg2+ |
| 1.00 | mM | CaCl2 | 21.0 | mM | HCO3− |
| 0.50 | mM | MgCl2 | 740 | mM | Cl− |
| 5.0 | mM | HPO42− | |||
| 2.5 | mM | SO42− | |||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
An, S.-J.; Lee, S.-H.; Huh, J.-B.; Jeong, S.I.; Park, J.-S.; Gwon, H.-J.; Kang, E.-S.; Jeong, C.-M.; Lim, Y.-M. Preparation and Characterization of Resorbable Bacterial Cellulose Membranes Treated by Electron Beam Irradiation for Guided Bone Regeneration. Int. J. Mol. Sci. 2017, 18, 2236. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms18112236
An S-J, Lee S-H, Huh J-B, Jeong SI, Park J-S, Gwon H-J, Kang E-S, Jeong C-M, Lim Y-M. Preparation and Characterization of Resorbable Bacterial Cellulose Membranes Treated by Electron Beam Irradiation for Guided Bone Regeneration. International Journal of Molecular Sciences. 2017; 18(11):2236. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms18112236
Chicago/Turabian StyleAn, Sung-Jun, So-Hyoun Lee, Jung-Bo Huh, Sung In Jeong, Jong-Seok Park, Hui-Jeong Gwon, Eun-Sook Kang, Chang-Mo Jeong, and Youn-Mook Lim. 2017. "Preparation and Characterization of Resorbable Bacterial Cellulose Membranes Treated by Electron Beam Irradiation for Guided Bone Regeneration" International Journal of Molecular Sciences 18, no. 11: 2236. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms18112236