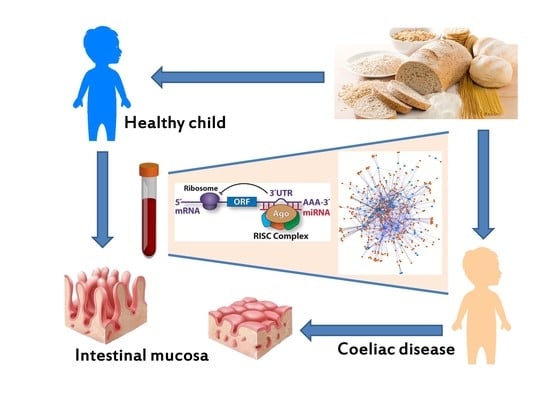
Intestinal and Circulating MicroRNAs in Coeliac Disease
Abstract
:1. Introduction
2. The Role of miRNAs in Intestinal Development and Homeostasis
3. Intestinal miRNAs of Patients with Coeliac Disease
4. Circulating miRNAs of Patients with Coeliac Disease
5. Post-Transcriptional Gene Expression Regulation by miRNAs in Coeliac Disease
6. Perspectives and Future Directions
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| 3′UTR | 3′ Untranslated Region |
| APCs | Antigen Presenting Cells |
| BMP2 | Bone Morphogenetic Protein 2 |
| CA | Patients with Iron-Deficiency Anaemia |
| CC | Patients with Classical Clinical Symptoms |
| CD | Coeliac Disease |
| DLL1 | Delta Like Canonical Notch Ligand1 |
| EMA | Anti-Endomysium IgA |
| ESPGHAN | European Society for Paediatric Gastroenterology Hepatology and Nutrition |
| FAS | Fas Cell Surface Death Receptor |
| GFD | Gluten Free Diet |
| HLA | Human Leukocyte Antigen |
| KLF4 | Kruppel-Like Factor 9 |
| LEF1 | Lymphoid Enhancer Binding Factor |
| MHC | Major Histocompatibility Complex |
| miRNA | MicroRNA |
| NTC | Patients on Gluten-Free Diet |
| NUMBL | NUMB like, Endocytic Adaptor Protein |
| pre-miRNA | Precursor miRNA |
| qRT-PCR | Quantitative Reverse Transcription-Polymerase Chain Reaction |
| RISC | RNA-Induced Silencing Complex |
| RUNX1 | Runt Related Transcription Factor 1 |
| STAT3 | Signal Transducer and Activator of Transcription 3 |
| tTG | Tissue Transglutaminase |
| TGM2 | Transglutaminase 2 |
| TJ | Tight Junctions |
References
- Meresse, B.; Ripoche, J.; Heyman, M.; Cerf-Bensussan, N. Celiac disease: From oral tolerance to intestinal inflammation, autoimmunity and lymphomagenesis. Mucosal Immunol. 2009, 2, 8–23. [Google Scholar] [CrossRef] [PubMed]
- Giordani, L.; del Pinto, T.; Vincentini, O.; Felli, C.; Silano, M.; Viora, M. Two wheat decapeptides prevent gliadin-dependent maturation of human dendritic cells. Exp. Cell Res. 2014, 321, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Sollid, L.M. Intraepithelial lymphocytes in celiac disease: License to kill revealed. Immunity 2004, 21, 303–304. [Google Scholar] [CrossRef] [PubMed]
- Schuppan, D.; Junker, Y.; Barisani, D. Celiac disease: From pathogenesis to novel therapies. Gastroenterology 2009, 137, 1912–1933. [Google Scholar] [CrossRef] [PubMed]
- Guandalini, S.; Assiri, A. Celiac disease: A review. JAMA Pediatr. 2014, 168, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Husby, S.; Koletzko, S.; Korponay-Szabo, I.R.; Mearin, M.L.; Phillips, A.; Shamir, R.; Troncone, R.; Giersiepen, K.; Branski, D.; Catassi, C.; et al. European society for pediatric gastroenterology, hepatology, and nutrition guidelines for the diagnosis of coeliac disease. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 136–160. [Google Scholar] [CrossRef] [PubMed]
- Giersiepen, K.; Lelgemann, M.; Stuhldreher, N.; Ronfani, L.; Husby, S.; Koletzko, S.; Korponay-Szabo, I.R. ESPGHAN Working Group on Coeliac Disease Diagnosis. Accuracy of diagnostic antibody tests for coeliac disease in children: Summary of an evidence report. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Wienholds, E.; Plasterk, R.H. MicroRNA function in animal development. FEBS Lett. 2005, 579, 5911–5922. [Google Scholar] [CrossRef] [PubMed]
- Barbato, C.; Arisi, I.; Frizzo, M.E.; Brandi, R.; Da Sacco, L.; Masotti, A. Computational challenges in miRNA target predictions: To be or not to be a true target? J. Biomed. Biotechnol. 2009, 2009, 803069. [Google Scholar] [CrossRef] [PubMed]
- Bascunan-Gamboa, K.A.; Araya-Quezada, M.; Perez-Bravo, F. MicroRNAs: An epigenetic tool to study celiac disease. Rev. Esp. Enferm. Dig. 2014, 106, 325–333. [Google Scholar] [PubMed]
- Zhang, L.; Cheng, J.; Fan, X.M. MicroRNAs: New therapeutic targets for intestinal barrier dysfunction. World J. Gastroenterol. 2014, 20, 5818–5825. [Google Scholar] [CrossRef] [PubMed]
- McKenna, L.B.; Schug, J.; Vourekas, A.; McKenna, J.B.; Bramswig, N.C.; Friedman, J.R.; Kaestner, K.H. MicroRNAs control intestinal epithelial differentiation, architecture, and barrier function. Gastroenterology 2010, 139, 1654–1664. [Google Scholar] [CrossRef] [PubMed]
- Ye, D.; Guo, S.; Al-Sadi, R.; Ma, T.Y. MicroRNA regulation of intestinal epithelial tight junction permeability. Gastroenterology 2011, 141, 1323–1333. [Google Scholar] [CrossRef] [PubMed]
- Capuano, M.; Iaffaldano, L.; Tinto, N.; Montanaro, D.; Capobianco, V.; Izzo, V.; Tucci, F.; Troncone, G.; Greco, L.; Sacchetti, L. MicroRNA-449a overexpression, reduced NOTCH1 signals and scarce goblet cells characterize the small intestine of celiac patients. PLoS ONE 2011, 6, e29094. [Google Scholar] [CrossRef] [PubMed]
- Vaira, V.; Roncoroni, L.; Barisani, D.; Gaudioso, G.; Bosari, S.; Bulfamante, G.; Doneda, L.; Conte, D.; Tomba, C.; Bardella, M.T.; et al. MicroRNA profiles in coeliac patients distinguish different clinical phenotypes and are modulated by gliadin peptides in primary duodenal fibroblasts. Clin. Sci. 2014, 126, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Magni, S.; Buoli, C.G.; Elli, L.; Vanessi, S.; Ballarini, E.; Nicolini, G.; Rusconi, M.; Castoldi, M.; Meneveri, R.; Muckenthaler, M.U.; et al. miRNAs affect the expression of innate and adaptive immunity proteins in celiac disease. Am. J. Gastroenterol. 2014, 109, 1662–1674. [Google Scholar] [CrossRef] [PubMed]
- Buoli, C.G.; Panceri, R.; Dinelli, M.; Biondi, A.; Mancuso, C.; Meneveri, R.; Barisani, D. miRNA-regulated gene expression differs in celiac disease patients according to the age of presentation. Genes Nutr. 2015, 10, 32. [Google Scholar] [CrossRef] [PubMed]
- Comincini, S.; Manai, F.; Meazza, C.; Pagani, S.; Martinelli, C.; Pasqua, N.; Pelizzo, G.; Biggiogera, M.; Bozzola, M. Identification of autophagy-related genes and their regulatory miRNAs associated with celiac disease in children. Int. J. Mol. Sci. 2017, 18, 391. [Google Scholar] [CrossRef] [PubMed]
- Baldassarre, A.; Felli, C.; Prantera, G.; Masotti, A. Circulating microRNAs and bioinformatics tools to discover novel diagnostic biomarkers of pediatric diseases. Genes 2017. under review. [Google Scholar]
- Chen, X.; Liang, H.; Zhang, J.; Zen, K.; Zhang, C.Y. Secreted microRNAs: A new form of intercellular communication. Trends Cell Biol. 2012, 22, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Salido-Guadarrama, I.; Romero-Cordoba, S.; Peralta-Zaragoza, O.; Hidalgo-Miranda, A.; Rodriguez-Dorantes, M. MicroRNAs transported by exosomes in body fluids as mediators of intercellular communication in cancer. OncoTargets Ther. 2014, 7, 1327–1338. [Google Scholar]
- Bell, E.; Taylor, M.A. Functional roles for exosomal microRNAs in the tumour microenvironment. Comput. Struct. Biotechnol. J. 2016, 15, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.P.; Burge, C.B.; Bartel, D.P. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell 2005, 120, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Enright, A.J.; John, B.; Gaul, U.; Tuschl, T.; Sander, C.; Marks, D.S. MicroRNA targets in Drosophila. Genome Biol. 2003, 5, R1. [Google Scholar] [CrossRef] [PubMed]
- Lagana, A.; Forte, S.; Giudice, A.; Arena, M.R.; Puglisi, P.L.; Giugno, R.; Pulvirenti, A.; Shasha, D.; Ferro, A. miRò: A miRNA knowledge base. Database 2009, 2009, bap008. [Google Scholar] [CrossRef] [PubMed]
- Kertesz, M.; Iovino, N.; Unnerstall, U.; Gaul, U.; Segal, E. The role of site accessibility in microRNA target recognition. Nat. Genet. 2007, 39, 1278–1284. [Google Scholar] [CrossRef] [PubMed]
- Dweep, H.; Sticht, C.; Pandey, P.; Gretz, N. miRWalk—Database: Prediction of possible miRNA binding sites by “walking”" the genes of three genomes. J. Biomed. Inform. 2011, 44, 839–847. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lu, M.; Qiu, C.; Cui, Q. TransmiR: A transcription factor-microRNA regulation database. Nucleic Acids Res. 2010, 38, D119–D122. [Google Scholar] [CrossRef] [PubMed]
- Xiao, F.; Zuo, Z.; Cai, G.; Kang, S.; Gao, X.; Li, T. miRecords: An integrated resource for microRNA-target interactions. Nucleic Acids Res. 2009, 37, D105–D110. [Google Scholar] [CrossRef] [PubMed]
- Huang da, W.; Sherman, B.T.; Lempicki, R.A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2009, 4, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.W.; Sherman, B.T.; Tan, Q.; Kir, J.; Liu, D.; Bryant, D.; Guo, Y.; Stephens, R.; Baseler, M.W.; Lane, H.C.; et al. DAVID Bioinformatics Resources: Expanded annotation database and novel algorithms to better extract biology from large gene lists. Nucleic Acids Res. 2007, 35, W169–W175. [Google Scholar] [CrossRef] [PubMed]
- Barone, M.V.; Zanzi, D.; Maglio, M.; Nanayakkara, M.; Santagata, S.; Lania, G.; Miele, E.; Ribecco, M.T.; Maurano, F.; Auricchio, R.; et al. Gliadin-mediated proliferation and innate immune activation in celiac disease are due to alterations in vesicular trafficking. PLoS ONE 2011, 6, e17039. [Google Scholar] [CrossRef] [PubMed]
- Juuti-Uusitalo, K.; Maki, M.; Kainulainen, H.; Isola, J.; Kaukinen, K. Gluten affects epithelial differentiation-associated genes in small intestinal mucosa of coeliac patients. Clin. Exp. Immunol. 2007, 150, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Gregorieff, A.; Clevers, H. Wnt signaling in the intestinal epithelium: From endoderm to cancer. Genes Dev. 2005, 19, 877–890. [Google Scholar] [CrossRef] [PubMed]
- Fevr, T.; Robine, S.; Louvard, D.; Huelsken, J. Wnt/β-catenin is essential for intestinal homeostasis and maintenance of intestinal stem cells. Mol. Cell. Biol. 2007, 27, 7551–7559. [Google Scholar] [CrossRef] [PubMed]
- Moss, S.F.; Attia, L.; Scholes, J.V.; Walters, J.R.; Holt, P.R. Increased small intestinal apoptosis in coeliac disease. Gut 1996, 39, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Maiuri, L.; Ciacci, C.; Raia, V.; Vacca, L.; Ricciardelli, I.; Raimondi, F.; Auricchio, S.; Quaratino, S.; Londei, M. FAS engagement drives apoptosis of enterocytes of coeliac patients. Gut 2001, 48, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, S.C.; Barbara, G.; Buurman, W.; Ockhuizen, T.; Schulzke, J.D.; Serino, M.; Tilg, H.; Watson, A.; Wells, J.M. Intestinal permeability—A new target for disease prevention and therapy. BMC Gastroenterol. 2014, 14, 189. [Google Scholar] [CrossRef] [PubMed]
- Clemente, M.G.; de Virgiliis, S.; Kang, J.S.; Macatagney, R.; Musu, M.P.; di Pierro, M.R.; Drago, S.; Congia, M.; Fasano, A. Early effects of gliadin on enterocyte intracellular signalling involved in intestinal barrier function. Gut 2003, 52, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Ekimler, S.; Sahin, K. Computational methods for MicroRNA target prediction. Genes 2014, 5, 671–683. [Google Scholar] [CrossRef] [PubMed]
- Zahm, A.M.; Thayu, M.; Hand, N.J.; Horner, A.; Leonard, M.B.; Friedman, J.R. Circulating microRNA is a biomarker of pediatric Crohn disease. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Masotti, A.; Baldassarre, A.; Fabrizi, M.; Olivero, G.; Loreti, M.C.; Giammaria, P.; Veronelli, P.; Graziani, M.P.; Manco, M. Oral glucose tolerance test unravels circulating miRNAs associated with insulin resistance in obese preschoolers. Pediatr. Obes. 2017, 12, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Masotti, A.; Baldassarre, A.; Guzzo, M.P.; Iannuccelli, C.; Barbato, C.; di Franco, M. Circulating microRNA profiles as liquid biopsies for the characterization and diagnosis of fibromyalgia syndrome. Mol. Neurobiol. 2016, 1–8. [Google Scholar] [CrossRef] [PubMed]


| Upregulated miRNAs | Downregulated miRNAs | Reference |
|---|---|---|
| Upregulated miRNAs in biopsies of CD patients (active and on gluten free-diet) | Downregulated miRNAs in biopsies of CD patients (active and on gluten free-diet) | [14] |
| miR-182, miR-196a, miR-330, miR-449a, miR-492, miR-500, miR-503, miR-504, miR-644 | miR-105, miR-124a, miR-135a, miR-189, miR-202, miR-219, miR-299-5p, miR-323, miR-379, miR-380-5p, miR-409-5p, miR-412, miR-512-3p, miR-566, miR-576, miR-600, miR-614, miR-616, miR-618, miR-631, miR-659 | |
| Upregulated in GFD patients | Downregulated in GFD patients | [15] |
| miR-422a, miR-551a, miR-1285-3p, miR-3681-5p | N.A. | |
| Upregulated in CD patients | Downregulated in CD patients | |
| miR-24-2-5p, miR-2113, miR-4300, miR-551b-5p, miR-519d, miR-642b-3p, miR-523-3p, miR-491-3p | miR-215, miR-451a, miR-192-5p, miR-31-5p, miR-194-5p, miR-338-3p | |
| Upregulated in CD patients with anaemia | Downregulated in CD patients with anaemia | |
| miR-491-3p, miR-337-3p, miR-2355-3p, miR-3148, miR-24-2-5p , miR-920, miR-638, miR-146b-3p, miR-1304-5p, miR-498, miR-490-3p, miR-1285-3p, miR-3183, miR-1290, miR-1299, miR-1270, miR-3663-5p, miR-618, miR-3135a, miR-4268, miR-4300, miR-4324, miR-300, miR-519d, miR-422a, miR-302a-3p, miR-3654, miR-3611, miR-4329, miR-3681-5p, miR-551b-5p, miR-4303, miR-642a-5p/miR-642b-5p, miR-550b-3p, miR-593-3p, miR-146a-5p, miR-1273e, miR-432-5p | miR-215, miR-31-5p, miR-193a-5p, miR-194-5p, miR-192-5p, miR-451a, miR-192-3p, miR-138-1-3p, miR-30b-5p, miR-664-5p | |
| Upregulated miRNAs in human biopsies of CD patients | Downregulated miRNAs in human biopsies of CD patients | [16] |
| N.A. | miR-192-5p, miR-194-5p, miR-197, miR-31-5p, miR-338-3p | |
| Upregulated miRNAs in human biopsies of CD patients | Downregulated miRNAs in human biopsies of CD patients | [17] |
| miR-21-5p, miR-21-3p, miR-486-5p | miR-192-5p, miR-31-5p, miR-338-3p |
| Gene Symbol | Gene Name |
|---|---|
| ABL1 | ABL proto-oncogene 1, non-receptor tyrosine kinase |
| AKT2 | AKT serine/threonine kinase 2 |
| APC2 | APC2, Wnt signaling pathway regulator |
| APPL1 | adaptor protein, phosphotyrosine interacting with PH domain and leucine zipper 1 |
| ARHGAP5 | Rho GTPase activating protein 5 |
| BCR | BCR, RhoGEF and GTPase activating protein |
| CBL | Cbl proto-oncogene |
| CCND1 | cyclin D1 |
| CCND2 | cyclin D2 |
| CEBPα | CCAAT/enhancer binding protein α |
| COL4α4 | collagen type IV α 4 chain |
| CREBBP | CREB binding protein |
| CRK | CRK proto-oncogene, adaptor protein |
| CSF1R | colony stimulating factor 1 receptor |
| DIAPH1 | diaphanous related formin 1 |
| E2F3 | E2F transcription factor 3 |
| ETS1 | ETS proto-oncogene 1, transcription factor |
| FGF2 | fibroblast growth factor 2 |
| FGF23 | fibroblast growth factor 23 |
| FGFR1 | fibroblast growth factor receptor 1 |
| FLNB | filamin B |
| FZD4 | frizzled class receptor 4 |
| HDAC2 | histone deacetylase 2 |
| INSR | insulin receptor |
| ITGβ8 | integrin subunit β 8 |
| KITLG | KIT ligand |
| KRAS | KRAS proto-oncogene, GTPase |
| LAMγ1 | laminin subunit γ 1 |
| MAPK1 | mitogen-activated protein kinase 1 |
| MET | MET proto-oncogene, receptor tyrosine kinase |
| MITF | melanogenesis associated transcription factor |
| NKX3-1 | NK3 homeobox 1 |
| PAX8 | paired box 8 |
| PDGFRα | platelet derived growth factor receptor α |
| PDPK1 | 3-phosphoinositide dependent protein kinase 1 |
| PIAS3 | protein inhibitor of activated STAT 3 |
| PIP5K1γ | phosphatidylinositol-4-phosphate 5-kinase type 1 γ |
| PPP1Cβ | protein phosphatase 1 catalytic subunit β |
| PRKCα | protein kinase C α |
| PTCH1 | patched 1 |
| PTPRJ | protein tyrosine phosphatase, receptor type J |
| RALB | RAS like proto-oncogene B |
| RAP1B | RAP1B, member of RAS oncogene family |
| RXRα | retinoid X receptor α |
| SORBS1 | sorbin and SH3 domain containing 1 |
| STAT5B | signal transducer and activator of transcription 5B |
| STK4 | serine/threonine kinase 4 |
| TCF7 | transcription factor 7 (T-cell specific, HMG-box) |
| TGFβR1 | transforming growth factor β receptor 1 |
| TJP1 | tight junction protein 1 |
| TRAF1 | TNF receptor associated factor 1 |
| TRAF5 | TNF receptor associated factor 5 |
| VEGFA | vascular endothelial growth factor A |
| XIAP | X-linked inhibitor of apoptosis |
| PRKCβ1 | protein kinase C β |
| Pathways | Genes |
|---|---|
| Focal adhesion | PRKCA, COL4A4, XIAP, DIAPH1, MET, PPP1CB, FLNB, PRKCB, MAPK1, PDPK1, CCND1, ARHGAP5, ITGB8, CCND2, VEGFA, PDGFRA, RAP1B, LAMC1, CRK, AKT2 |
| PI3K-Akt signaling pathway | PRKCA, COL4A4, FGFR1, RXRA, MET, KITLG, FGF23, MAPK1, PDPK1, CCND1, KRAS, ITGB8, CCND2, VEGFA, PDGFRA, LAMC1, FGF2, INSR, AKT2, CSF1R |
| Adherens junction | PTPRJ, MAPK1, FGFR1, TJP1, TCF7, SORBS1, TGFBR1, CREBBP, MET, INSR |
| MAPK signaling pathway | PRKCA, FGFR1, TGFBR1, FGF23, FLNB, STK4, PRKCB, MAPK1, KRAS, PDGFRA, RAP1B, CRK, FGF2, AKT2 |
| ErbB signaling pathway | PRKCA, MAPK1, KRAS, STAT5B, CBL, ABL1, CRK, PRKCB, AKT2 |
| Regulation of actin cytoskeleton | MAPK1, FGFR1, KRAS, APC2, ITGB8, DIAPH1, PDGFRA, FGF23, PIP5K1C, CRK, FGF2, PPP1CB |
| Wnt signaling pathway | PRKCA, TCF7, CCND1, APC2, CCND2, CREBBP, FZD4, PRKCB |
| VEGF signaling pathway | PRKCA, MAPK1, KRAS, VEGFA, PRKCB, AKT2 |
| Gap junction | PRKCA, MAPK1, TJP1, KRAS, PDGFRA, PRKCB |
| Cell cycle | E2F3, CCND1, HDAC2, CCND2, CREBBP, ABL1 |
| Jak-STAT signaling pathway | CCND1, CCND2, PIAS3, STAT5B, CREBBP, AKT2 |
| T cell receptor signaling pathway | MAPK1, PDPK1, KRAS, CBL, AKT2 |
| Tight junction | PRKCA, TJP1, KRAS, PRKCB, AKT2 |
| TNF signaling pathway | TRAF1, MAPK1, TRAF5, AKT2 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Felli, C.; Baldassarre, A.; Masotti, A. Intestinal and Circulating MicroRNAs in Coeliac Disease. Int. J. Mol. Sci. 2017, 18, 1907. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms18091907
Felli C, Baldassarre A, Masotti A. Intestinal and Circulating MicroRNAs in Coeliac Disease. International Journal of Molecular Sciences. 2017; 18(9):1907. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms18091907
Chicago/Turabian StyleFelli, Cristina, Antonella Baldassarre, and Andrea Masotti. 2017. "Intestinal and Circulating MicroRNAs in Coeliac Disease" International Journal of Molecular Sciences 18, no. 9: 1907. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms18091907