Anti-Inflammatory and Skin Barrier Repair Effects of Topical Application of Some Plant Oils
Abstract
:1. Introduction
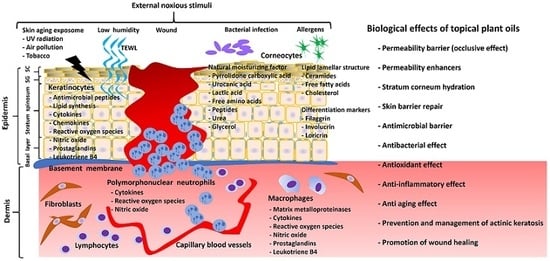
1.1. Stratum Corneum Structure and Function
1.2. Atopic Dermatitis and Barrier Function
1.3. Wound Healing
1.4. Skin Inflammation and Proliferation
1.5. Reactive Oxidative Stress, Skin Aging and Skin Cancer
2. The Constituents of Plant Oils
2.1. Phenolic Compounds
2.2. Triterpenes
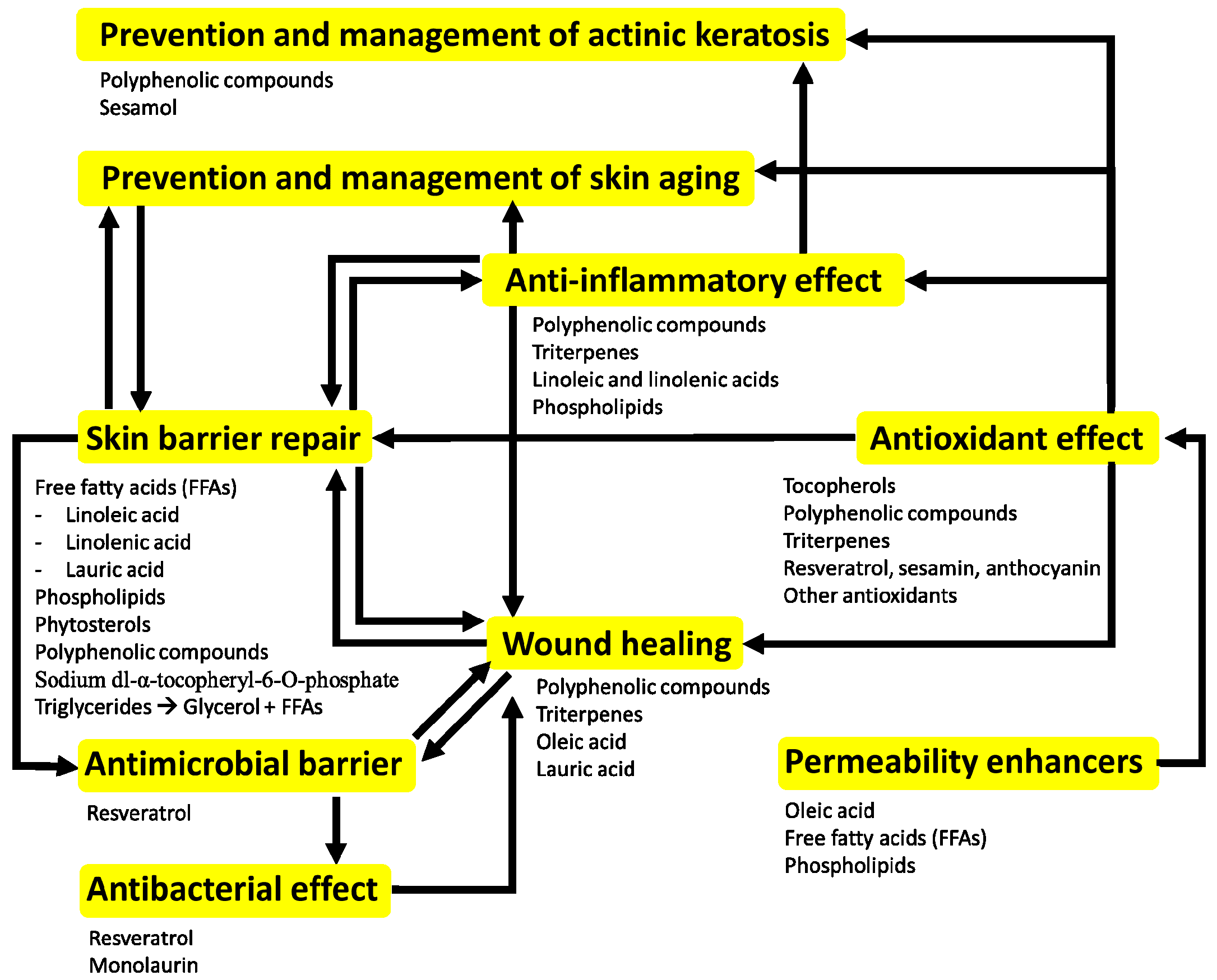
3. The Potential Beneficial Effects of Topical Application of Plant Oils on Skin
3.1. Olive Oil
3.2. Sunflower Seed Oil
3.3. Grape Seed Oil
3.4. Coconut Oil
3.5. Safflower Seed Oil
3.6. Argan Oil
3.7. Soybean Oil
3.8. Peanut Oil
3.9. Sesame Oil
3.10. Avocado Oil
3.11. Borage Oil
3.12. Jojoba Oil
3.13. Oat Oil
3.14. Pomegranate Seed Oil
3.15. Almond Oil
3.16. Bitter Apricot Oil
3.17. Rose Hip Oil
3.18. German Chamomile Oil
3.19. Shea Butter
4. Conclusions
Conflicts of Interest
Abbreviations
| 15-HETE AD | 15-hydroxyeicosatetraenoic acid Atopic dermatitis |
| CE | Cornified envelope |
| COX | Cyclooxygenase |
| FFA | Free Fatty Acid |
| LB | Lamellar body |
| MMP | Matrix metalloproteinase |
| NMF | Natural moisturizing factor |
| PMN | Polymorphonuclear neutrophils |
| PPAR PUFA | Peroxisome proliferator-activated receptor Polyunsaturated fatty acid |
| ROS | Reactive oxygen species |
| SC | Stratum corneum |
| SFA | Saturated Fatty Acid |
| SG | Stratum granulosum |
| TEWL | Transepidermal water loss |
| TNF-α | Tumor necrosis factor-alpha |
| UFA | Unsaturated Fatty Acid |
| UV | Ultraviolet |
| WH | Wound healing |
References
- Elias, P.M. Epidermal lipids, barrier function, and desquamation. J. Investig. Dermatol. 1983, (Suppl. 80), 44s–49s. [Google Scholar] [CrossRef]
- Kang, L.; Ho, P.C.; Chan, S.Y. Interactions between a skin penetration enhancer and the main components of human stratum corneum lipids. J. Therm. Anal. Calorim. 2006, 83, 27–30. [Google Scholar] [CrossRef]
- Ziboh, V.A.; Miller, C.C.; Cho, Y. Metabolism of polyunsaturated fatty acids by skin epidermal enzymes: Generation of antiinflammatory and antiproliferative metabolites. Am. J. Clin. Nutr. 2000, 71 (Suppl. 1), 361S–366S. [Google Scholar]
- Ansari, M.N.; Nicolaides, N.; Fu, H.C. Fatty acid composition of the living layer and stratum corneum lipids of human sole skin epidermis. Lipids 1970, 5, 838–845. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.G.; Bryce, R.P.; Horrobin, D.F. Essential fatty acids: Molecular and cellular basis of their anti-cancer action and clinical implications. Crit. Rev. Oncol. Hematol. 1998, 27, 179–209. [Google Scholar] [CrossRef]
- Sahle, F.F.; Gebre-Mariam, T.; Dobner, B.; Wohlrab, J.; Neubert, R.H. Skin diseases associated with the depletion of stratum corneum lipids and stratum corneum lipid substitution therapy. Skin Pharmacol. Physiol. 2015, 28, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Terashi, H.; Izumi, K.; Rhodes, L.M.; Marcelo, C.L. Human stratified squamous epithelia differ in cellular fatty acid composition. J. Dermatol. Sci. 2000, 24, 14–24. [Google Scholar] [CrossRef]
- Drake, D.R.; Brogden, K.A.; Dawson, D.V.; Wertz, P.W. Thematic review series: Skin lipids. Antimicrobial lipids at the skin surface. J. Lipid Res. 2008, 49, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.K.; Man, M.Q.; Santiago, J.L.; Park, K.; Roelandt, T.; Oda, Y.; Hupe, M.; Crumrine, D.; Lee, H.J.; Gschwandtner, M.; et al. Topical antihistamines display potent anti-inflammatory activity linked in part to enhanced permeability barrier function. J. Investig. Dermatol. 2013, 133, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Elias, P.M.; Wakefield, J.S. Mechanisms of abnormal lamellar body secretion and the dysfunctional skin barrier in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2014, 134, 781e1–791e1. [Google Scholar] [CrossRef] [PubMed]
- Patzelt, A.; Lademann, J.; Richter, H.; Darvin, M.E.; Schanzer, S.; Thiede, G.; Sterry, W.; Vergou, T.; Hauser, M. In vivo investigations on the penetration of various oils and their influence on the skin barrier. Skin Res. Technol. 2012, 18, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Elias, P.M.; Wakefield, J.S. Therapeutic implications of a barrier-based pathogenesis of atopic dermatitis. Clin. Rev. Allergy Immunol. 2011, 41, 282–295. [Google Scholar] [CrossRef] [PubMed]
- Hatano, Y.; Adachi, Y.; Elias, P.M.; Crumrine, D.; Sakai, T.; Kurahashi, R.; Katagiri, K.; Fujiwara, S. The Th2 cytokine, interleukin-4, abrogates the cohesion of normal stratum corneum in mice: Implications for pathogenesis of atopic dermatitis. Exp. Dermatol. 2013, 22, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Elias, P.M. Lipid abnormalities and lipid-based repair strategies in atopic dermatitis. Biochim. Biophys. Acta 2014, 1841, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Reinke, J.M.; Sorg, H. Wound repair and regeneration. Eur. Surg. Res. 2012, 49, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Robson, M.C.; Steed, D.L.; Franz, M.G. Wound healing: Biologic features and approaches to maximize healing trajectories. Curr. Probl. Surg. 2001, 38, 72–140. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Richmond, A. Chemokine Regulation of Neutrophil Infiltration of Skin Wounds. Adv. Wound Care 2015, 4, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Profyris, C.; Tziotzios, C.; Do Vale, I. Cutaneous scarring: Pathophysiology, molecular mechanisms, and scar reduction therapeutics Part I. The molecular basis of scar formation. J. Am. Acad. Dermatol. 2012, 66, 1–10, quiz 11-2. [Google Scholar] [CrossRef] [PubMed]
- Olczyk, P.; Mencner, L.; Komosinska-Vassev, K. The role of the extracellular matrix components in cutaneous wound healing. Biomed. Res. Int. 2014, 2014, 747584. [Google Scholar] [CrossRef] [PubMed]
- Goren, I.; Muller, E.; Schiefelbein, D.; Christen, U.; Pfeilschifter, J.; Muhl, H.; Frank, S. Systemic anti-TNFalpha treatment restores diabetes-impaired skin repair in ob/ob mice by inactivation of macrophages. J. Investig. Dermatol. 2007, 127, 2259–2267. [Google Scholar] [CrossRef] [PubMed]
- Schmuth, M.; Blunder, S.; Dubrac, S.; Gruber, R.; Moosbrugger-Martinz, V. Epidermal barrier in hereditary ichthyoses, atopic dermatitis, and psoriasis. J. Dtsch. Dermatol. Ges. 2015, 13, 1119–1123. [Google Scholar] [CrossRef] [PubMed]
- Fujii, M.; Shimazaki, Y.; Muto, Y.; Kohno, S.; Ohya, S.; Nabe, T. Dietary deficiencies of unsaturated fatty acids and starch cause atopic dermatitis-like pruritus in hairless mice. Exp. Dermatol. 2015, 24, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Ternowitz, T.; Fogh, K.; Kragballe, K. 15-Hydroxyeicosatetraenoic acid (15-HETE) specifically inhibits LTB4-induced chemotaxis of human neutrophils. Skin Pharmacol. 1988, 1, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Ziboh, V.A.; Cho, Y.; Mani, I.; Xi, S. Biological significance of essential fatty acids/prostanoids/lipoxygenase-derived monohydroxy fatty acids in the skin. Arch. Pharm. Res. 2002, 25, 747–758. [Google Scholar] [CrossRef] [PubMed]
- An, K.P.; Athar, M.; Tang, X.; Katiyar, S.K.; Russo, J.; Beech, J.; Aszterbaum, M.; Kopelovich, L.; Epstein, E.H., Jr.; Mukhtar, H.; et al. Cyclooxygenase-2 expression in murine and human nonmelanoma skin cancers: Implications for therapeutic approaches. Photochem. Photobiol. 2002, 76, 73–80. [Google Scholar] [CrossRef]
- Muller-Decker, K. Cyclooxygenase-dependent signaling is causally linked to non-melanoma skin carcinogenesis: Pharmacological, genetic, and clinical evidence. Cancer Metastasis Rev. 2011, 30, 343–361. [Google Scholar] [CrossRef] [PubMed]
- Vierkotter, A.; Krutmann, J. Environmental influences on skin aging and ethnic-specific manifestations. Dermatoendocrinology 2012, 4, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Fisher, G.J.; Kang, S.; Varani, J.; Bata-Csorgo, Z.; Wan, Y.; Datta, S.; Voorhees, J.J. Mechanisms of photoaging and chronological skin aging. Arch. Dermatol. 2002, 138, 1462–1470. [Google Scholar] [CrossRef] [PubMed]
- Marrot, L. Pollution and Sun Exposure: A Deleterious Synergy. Mechanisms and Opportunities for Skin Protection. Curr. Med. Chem. 2017. [Google Scholar] [CrossRef]
- Durai, P.C.; Thappa, D.M.; Kumari, R.; Malathi, M. Aging in elderly: Chronological versus photoaging. Indian J. Dermatol. 2012, 57, 343–352. [Google Scholar] [PubMed]
- Ma, W.; Wlaschek, M.; Tantcheva-Poor, I.; Schneider, L.A.; Naderi, L.; Razi-Wolf, Z.; Schuller, J.; Scharffetter-Kochanek, K. Chronological ageing and photoageing of the fibroblasts and the dermal connective tissue. Clin. Exp. Dermatol. 2001, 26, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Scharffetter-Kochanek, K.; Wlaschek, M.; Brenneisen, P.; Schauen, M.; Blaudschun, R.; Wenk, J. UV-induced reactive oxygen species in photocarcinogenesis and photoaging. Biol. Chem. 1997, 378, 1247–1257. [Google Scholar] [PubMed]
- Sample, A.; He, Y.Y. Mechanisms and prevention of UV-induced melanoma. Photodermatol. Photoimmunol. Photomed. 2017. [Google Scholar] [CrossRef] [PubMed]
- Silva, S.; Michniak-Kohn, B.; Leonardi, G.R. An overview about oxidation in clinical practice of skin aging. An. Bras. Dermatol. 2017, 92, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Nishigori, C. Cellular aspects of photocarcinogenesis. Photochem. Photobiol. Sci. 2006, 5, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Mack Correa, M.C.; Mao, G.; Saad, P.; Flach, C.R.; Mendelsohn, R.; Walters, R.M. Molecular interactions of plant oil components with stratum corneum lipids correlate with clinical measures of skin barrier function. Exp. Dermatol. 2014, 23, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Kuriyama, K.; Shimizu, T.; Horiguchi, T.; Watabe, M.; Abe, Y. Vitamin E ointment at high dose levels suppresses contact dermatitis in rats by stabilizing keratinocytes. Inflamm. Res. 2002, 51, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Parish, W.E.; Read, J.; Paterson, S.E. Changes in basal cell mitosis and transepidermal water loss in skin cultures treated with vitamins C and E. Exp. Dermatol. 2005, 14, 684–691. [Google Scholar] [CrossRef] [PubMed]
- De Freitas Cuba, L.; Braga Filho, A.; Cherubini, K.; Salum, F.G.; Figueiredo, M.A. Topical application of Aloe vera and vitamin E on induced ulcers on the tongue of rats subjected to radiation: Clinical and histological evaluation. Support. Care Cancer 2016, 24, 2557–2564. [Google Scholar] [CrossRef] [PubMed]
- Kato, E.; Takahashi, N. Improvement by sodium dl-alpha-tocopheryl-6-O-phosphate treatment of moisture-retaining ability in stratum corneum through increased ceramide levels. Bioorg. Med. Chem. 2012, 20, 3837–3842. [Google Scholar] [CrossRef] [PubMed]
- Dreier, J.; Sorensen, J.A.; Brewer, J.R. Superresolution and Fluorescence Dynamics Evidence Reveal That Intact Liposomes Do Not Cross the Human Skin Barrier. PLoS ONE 2016, 11, e0146514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morifuji, M.; Oba, C.; Ichikawa, S.; Ito, K.; Kawahata, K.; Asami, Y.; Ikegami, S.; Itoh, H.; Sugawara, T. A novel mechanism for improvement of dry skin by dietary milk phospholipids: Effect on epidermal covalently bound ceramides and skin inflammation in hairless mice. J. Dermatol. Sci. 2015, 78, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Sato, J.; Denda, M.; Ashida, Y.; Koyama, J. Loss of water from the stratum corneum induces epidermal DNA synthesis in hairless mice. Arch. Dermatol. Res. 1998, 290, 634–637. [Google Scholar] [CrossRef] [PubMed]
- Lercker, G.; Rodriguez-Estrada, M.T. Chromatographic analysis of unsaponifiable compounds of olive oils and fat-containing foods. J. Chromatogr. A 2000, 881, 105–129. [Google Scholar] [CrossRef]
- Tanojo, H.; Boelsma, E.; Junginger, H.E.; Ponec, M.; Bodde, H.E. In vivo human skin barrier modulation by topical application of fatty acids. Skin Pharmacol. Appl. Skin Physiol. 1998, 11, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Elias, P.M.; Brown, B.E.; Ziboh, V.A. The permeability barrier in essential fatty acid deficiency: Evidence for a direct role for linoleic acid in barrier function. J. Investig. Dermatol. 1980, 74, 230–233. [Google Scholar] [CrossRef] [PubMed]
- Hansen, H.S.; Jensen, B. Essential function of linoleic acid esterified in acylglucosylceramide and acylceramide in maintaining the epidermal water permeability barrier. Evidence from feeding studies with oleate, linoleate, arachidonate, columbinate and alpha-linolenate. Biochim. Biophys. Acta 1985, 834, 357–363. [Google Scholar] [CrossRef]
- Jiang, S.J.; Zhou, X.J. Examination of the mechanism of oleic acid-induced percutaneous penetration enhancement: An ultrastructural study. Biol. Pharm. Bull. 2003, 26, 66–68. [Google Scholar] [CrossRef] [PubMed]
- Viljoen, J.M.; Cowley, A.; du Preez, J.; Gerber, M.; du Plessis, J. Penetration enhancing effects of selected natural oils utilized in topical dosage forms. Drug Dev. Ind. Pharm. 2015, 41, 2045–2054. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, C.R.; Souza, M.A.; Ferro, E.A.; Favoreto, S., Jr.; Pena, J.D. Influence of topical administration of n-3 and n-6 essential and n-9 nonessential fatty acids on the healing of cutaneous wounds. Wound Repair Regen. 2004, 12, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Torres, L.R.; Santana, F.C.; Torres-Leal, F.L.; Melo, I.L.; Yoshime, L.T.; Matos-Neto, E.M.; Seelaender, M.C.; Araujo, C.M.; Cogliati, B.; Mancini-Filho, J. Pequi (Caryocar brasiliense Camb.) almond oil attenuates carbon tetrachloride-induced acute hepatic injury in rats: Antioxidant and anti-inflammatory effects. Food Chem. Toxicol. 2016, 97, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Servili, M.; Esposto, S.; Fabiani, R.; Urbani, S.; Taticchi, A.; Mariucci, F.; Selvaggini, R.; Montedoro, G.F. Phenolic compounds in olive oil: Antioxidant, health and organoleptic activities according to their chemical structure. Inflammopharmacology 2009, 17, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Duba, K.S.; Fiori, L. Supercritical CO2 extraction of grape seed oil: Effect of process parameters on the extraction kinetics. J. Supercrit. Fluid 2015, 98, 33–43. [Google Scholar] [CrossRef]
- Rombaut, N.; Savoire, R.; Thomasset, B.; Belliard, T.; Castello, J.; Van Hecke, E.; Lanoiselle, J.L. Grape seed oil extraction: Interest of supercritical fluid extraction and gas-assisted mechanical extraction for enhancing polyphenol co-extraction in oil. C. R. Chim. 2014, 17, 284–292. [Google Scholar] [CrossRef]
- Agra, L.C.; Ferro, J.N.S.; Barbosa, F.T.; Barreto, E. Triterpenes with healing activity: A systematic review. J. Dermatol. Treat. 2015, 26, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Wardecki, T.; Werner, P.; Thomas, M.; Templin, M.F.; Schmidt, G.; Brandner, J.M.; Merfort, I. Influence of Birch Bark Triterpenes on Keratinocytes and Fibroblasts from Diabetic and Nondiabetic Donors. J. Nat. Prod. 2016, 79, 1112–1123. [Google Scholar] [CrossRef] [PubMed]
- Maranz, S.; Wiesman, Z. Influence of climate on the tocopherol content of shea butter. J. Agric. Food Chem. 2004, 52, 2934–2937. [Google Scholar] [CrossRef] [PubMed]
- Nasopoulou, C.; Karantonis, H.C.; Detopoulou, M.; Demopoulos, C.A.; Zabetakis, I. Exploiting the anti-inflammatory properties of olive (Olea europaea) in the sustainable production of functional food and neutraceuticals. Phytochem. Rev. 2014, 13, 445–458. [Google Scholar] [CrossRef]
- Donato-Trancoso, A.; Monte-Alto-Costa, A.; Romana-Souza, B. Olive oil-induced reduction of oxidative damage and inflammation promotes wound healing of pressure ulcers in mice. J. Dermatol. Sci. 2016, 83, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Zahmatkesh, M.; Manesh, M.J.; Babashahabi, R. Effect of Olea ointment and Acetate Mafenide on burn wounds—A randomized clinical trial. Iran. J. Nurs. Midwifery Res. 2015, 20, 599–603. [Google Scholar] [PubMed]
- Budiyanto, A.; Ahmed, N.U.; Wu, A.; Bito, T.; Nikaido, O.; Osawa, T.; Ueda, M.; Ichihashi, M. Protective effect of topically applied olive oil against photocarcinogenesis following UVB exposure of mice. Carcinogenesis 2000, 21, 2085–2090. [Google Scholar] [CrossRef] [PubMed]
- Danby, S.G.; AlEnezi, T.; Sultan, A.; Lavender, T.; Chittock, J.; Brown, K.; Cork, M.J. Effect of olive and sunflower seed oil on the adult skin barrier: Implications for neonatal skin care. Pediatr. Dermatol. 2013, 30, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Cooke, A.; Cork, M.J.; Victor, S.; Campbell, M.; Danby, S.; Chittock, J.; Lavender, T. Olive Oil, Sunflower Oil or no Oil for Baby Dry Skin or Massage: A Pilot, Assessor-blinded, Randomized Controlled Trial (the Oil in Baby SkincaRE [OBSeRvE] Study). Acta Derm. Venereol. 2016, 96, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Norlen, L. Is Oil a Balsam for Baby Skin? Acta Derm. Venereol. 2016, 96, 291. [Google Scholar] [CrossRef] [PubMed]
- Korac, R.R.; Khambholja, K.M. Potential of herbs in skin protection from ultraviolet radiation. Pharmacogn. Rev. 2011, 5, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Kapadia, G.J.; Azuine, M.A.; Tokuda, H.; Takasaki, M.; Mukainaka, T.; Konoshima, T.; Nishino, H. Chemopreventive effect of resveratrol, sesamol, sesame oil and sunflower oil in the Epstein-Barr virus early antigen activation assay and the mouse skin two-stage carcinogenesis. Pharmacol. Res. 2002, 45, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Shivananda Nayak, B.; Dan Ramdath, D.; Marshall, J.R.; Isitor, G.; Xue, S.; Shi, J. Wound-healing properties of the oils of Vitis vinifera and Vaccinium macrocarpon. Phytother. Res. 2011, 25, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Khanna, S.; Venojarvi, M.; Roy, S.; Sharma, N.; Trikha, P.; Bagchi, D.; Bagchi, M.; Sen, C.K. Dermal wound healing properties of redox-active grape seed proanthocyanidins. Free Radic. Biol. Med. 2002, 33, 1089–1096. [Google Scholar] [CrossRef]
- Chan, M.M. Antimicrobial effect of resveratrol on dermatophytes and bacterial pathogens of the skin. Biochem. Pharmacol. 2002, 63, 99–104. [Google Scholar] [CrossRef]
- Park, K.; Elias, P.M.; Hupe, M.; Borkowski, A.W.; Gallo, R.L.; Shin, K.O.; Lee, Y.M.; Holleran, W.M.; Uchida, Y. Resveratrol stimulates sphingosine-1-phosphate signaling of cathelicidin production. J. Investig. Dermatol. 2013, 133, 1942–1949. [Google Scholar] [CrossRef] [PubMed]
- Davidov-Pardo, G.; McClements, D.J. Nutraceutical delivery systems: Resveratrol encapsulation in grape seed oil nanoemulsions formed by spontaneous emulsification. Food Chem. 2015, 167, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Shinagawa, F.B.; de Santana, F.C.; Torres, L.R.O.; Mancini-Filho, J. Grape seed oil: A potential functional food? Food Sci. Technol. 2015, 35, 399–406. [Google Scholar] [CrossRef]
- Evangelista, M.T.; Abad-Casintahan, F.; Lopez-Villafuerte, L. The effect of topical virgin coconut oil on SCORAD index, transepidermal water loss, and skin capacitance in mild to moderate pediatric atopic dermatitis: A randomized, double-blind, clinical trial. Int. J. Dermatol. 2014, 53, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Nevin, K.G.; Rajamohan, T. Effect of topical application of virgin coconut oil on skin components and antioxidant status during dermal wound healing in young rats. Skin Pharmacol. Physiol. 2010, 23, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Jang, J.E.; Kim, J.; Lee, Y.I.; Lee, D.W.; Song, S.Y.; Lee, J.H. Enhanced barrier functions and anti-inflammatory effect of cultured coconut extract on human skin. Food Chem. Toxicol. 2017, 106 (Pt A), 367–375. [Google Scholar] [CrossRef] [PubMed]
- Preuss, H.G.; Echard, B.; Enig, M.; Brook, I.; Elliott, T.B. Minimum inhibitory concentrations of herbal essential oils and monolaurin for gram-positive and gram-negative bacteria. Mol. Cell. Biochem. 2005, 272, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Oyi, A.R.; Onaolapo, J.; Obi, R.C. Formulation and Antimicrobial Studies of Coconut (Cocos nucifera Linne) Oil. Res. J. Appl. Sci. Eng. Technol. 2010, 2, 133–137. [Google Scholar]
- Esquenazi, D.; Wigg, M.D.; Miranda, M.M.; Rodrigues, H.M.; Tostes, J.B.; Rozental, S.; da Silva, A.J.; Alviano, C.S. Antimicrobial and antiviral activities of polyphenolics from Cocos nucifera Linn. (Palmae) husk fiber extract. Res. Microbiol. 2002, 153, 647–652. [Google Scholar] [CrossRef]
- Chen, C.Y.; Peng, W.H.; Tsai, K.D.; Hsu, S.L. Luteolin suppresses inflammation-associated gene expression by blocking NF-kappaB and AP-1 activation pathway in mouse alveolar macrophages. Life Sci. 2007, 81, 1602–1614. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Lazaro, M. Distribution and biological activities of the flavonoid luteolin. Mini Rev. Med. Chem. 2009, 9, 31–59. [Google Scholar] [CrossRef] [PubMed]
- Boucetta, K.Q.; Charrouf, Z.; Aguenaou, H.; Derouiche, A.; Bensouda, Y. The effect of dietary and/or cosmetic argan oil on postmenopausal skin elasticity. Clin. Interv. Aging 2015, 10, 339–349. [Google Scholar] [PubMed]
- Manca, M.L.; Matricardi, P.; Cencetti, C.; Peris, J.E.; Melis, V.; Carbone, C.; Escribano, E.; Zaru, M.; Fadda, A.M.; Manconi, M. Combination of argan oil and phospholipids for the development of an effective liposome-like formulation able to improve skin hydration and allantoin dermal delivery. Int. J. Pharm. 2016, 505, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Jordan, M.; Nayel, A.; Brownlow, B.; Elbayoumi, T. Development and evaluation of tocopherol-rich argan oil-based nanoemulsions as vehicles possessing anticancer activity. J. Biomed. Nanotechnol. 2012, 8, 944–956. [Google Scholar] [CrossRef] [PubMed]
- Avsar, U.; Halici, Z.; Akpinar, E.; Yayla, M.; Avsar, U.; Harun, U.; Harun, U.; Hasan Tarik, A.; Bayraktutan, Z. The Effects of Argan Oil in Second-degree Burn Wound Healing in Rats. Ostomy Wound Manag. 2016, 62, 26–34. [Google Scholar]
- Jhan, J.K.; Chung, Y.C.; Chen, G.H.; Chang, C.H.; Lu, Y.C.; Hsu, C.K. Anthocyanin contents in the seed coat of black soya bean and their anti-human tyrosinase activity and antioxidative activity. Int. J. Cosmet. Sci. 2016, 38, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.N.; Han, S.N.; Ha, T.J.; Kim, H.K. Black soybean anthocyanins attenuate inflammatory responses by suppressing reactive oxygen species production and mitogen activated protein kinases signaling in lipopolysaccharide-stimulated macrophages. Nutr. Res. Pract. 2017, 11, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Bonina, F.; Puglia, C.; Avogadro, M.; Baranelli, E.; Cravotto, G. The topical protective effect of soybean-germ oil against UVB-induced cutaneous erythema: An in vivo evaluation. Arch. Pharm. 2005, 338, 598–601. [Google Scholar] [CrossRef] [PubMed]
- Zhai, H.; Ramirez, R.G.; Maibach, H.I. Hydrating effects of a corticoid oil formulation and its vehicle on human skin. Skin Pharmacol Appl Skin Physiol 2003, 16, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Lasne, C.; Nguyen-Ba, G.; Oueslatti, R.; Chouroulinkov, I. Inhibition of chemically-induced skin carcinogenesis in mice by peanut oil preparations. Bull Cancer 1991, 78, 237–247. [Google Scholar] [PubMed]
- Chiang, J.P.; Hsu, D.Z.; Tsai, J.C.; Sheu, H.M.; Liu, M.Y. Effects of topical sesame oil on oxidative stress in rats. Altern. Ther. Health Med. 2005, 11, 40–45. [Google Scholar] [PubMed]
- Nasiri, M.; Farsi, Z. Effect of light pressure stroking massage with sesame (Sesamum indicum L.) oil on alleviating acute traumatic limbs pain: A triple-blind controlled trial in emergency department. Complement. Ther. Med. 2017, 32, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Hsu, D.Z.; Chen, S.J.; Chu, P.Y.; Liu, M.Y. Therapeutic effects of sesame oil on monosodium urate crystal-induced acute inflammatory response in rats. Springerplus 2013, 2, 659. [Google Scholar] [CrossRef] [PubMed]
- Bigdeli Shamloo, M.B.; Nasiri, M.; Dabirian, A.; Bakhtiyari, A.; Mojab, F.; Alavi Majd, H. The Effects of Topical Sesame (Sesamum indicum) Oil on Pain Severity and Amount of Received Non-Steroid Anti-Inflammatory Drugs in Patients with Upper or Lower Extremities Trauma. Anesthesiol. Pain Med. 2015, 5, e25085. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, A.P.; Franco Ede, S.; Rodrigues Barreto, R.; Cordeiro, D.P.; de Melo, R.G.; de Aquino, C.M.; E Silva, A.A.; de Medeiros, P.L.; da Silva, T.G.; Goes, A.J.; et al. Effect of semisolid formulation of persea americana mill (avocado) oil on wound healing in rats. Evid. Based Complement. Alternat. Med. 2013, 2013, 472382. [Google Scholar] [CrossRef] [PubMed]
- Nayak, B.S.; Raju, S.S.; Chalapathi Rao, A.V. Wound healing activity of Persea Americana (avocado) fruit: A preclinical study on rats. J. Wound Care 2008, 17, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Lamaud, E.; Huc, A.; Wepierre, J. Effects of avocado and soya bean lipidic non-saponifiables on the components of skin connective tissue after topical application in the hairless rat: Biophysical and biomechanical determination. Int. J. Cosmet. Sci. 1982, 4, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Kanehara, S.; Ohtani, T.; Uede, K.; Furukawa, F. Clinical effects of undershirts coated with borage oil on children with atopic dermatitis: A double-blind, placebo-controlled clinical trial. J. Dermatol. 2007, 34, 811–815. [Google Scholar] [CrossRef] [PubMed]
- Meier, L.; Stange, R.; Michalsen, A.; Uehleke, B. Clay jojoba oil facial mask for lesioned skin and mild acne—Results of a prospective, observational pilot study. Forsch Komplementmed 2012, 19, 75–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranzato, E.; Martinotti, S.; Burlando, B. Wound healing properties of jojoba liquid wax: An in vitro study. J. Ethnopharmacol. 2011, 134, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Nebus, J.; Nystrand, G.; Fowler, J.; Wallo, W. A daily oat-based skin care regimen for atopic skin. J. Am. Acad. Dermatol. 2009, 60, Ab67. [Google Scholar]
- Reynertson, K.A.; Garay, M.; Nebus, J.; Chon, S.; Kaur, S.; Mahmood, K.; Kizoulis, M.; Southall, M.D. Anti-inflammatory activities of colloidal oatmeal (Avena sativa) contribute to the effectiveness of oats in treatment of itch associated with dry, irritated skin. J. Drugs Dermatol. 2015, 14, 43–48. [Google Scholar] [PubMed]
- Sur, R.; Nigam, A.; Grote, D.; Liebel, F.; Southall, M.D. Avenanthramides, polyphenols from oats, exhibit anti-inflammatory and anti-itch activity. Arch. Dermatol. Res. 2008, 300, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Chon, S.H.; Tannahill, R.; Yao, X.; Southall, M.D.; Pappas, A. Keratinocyte differentiation and upregulation of ceramide synthesis induced by an oat lipid extract via the activation of PPAR pathways. Exp. Dermatol. 2015, 24, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Hora, J.J.; Maydew, E.R.; Lansky, E.P.; Dwivedi, C. Chemopreventive effects of pomegranate seed oil on skin tumor development in CD1 mice. J. Med. Food 2003, 6, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Timur Tashan, S.; Kafkasli, A. The effect of bitter almond oil and massaging on striae gravidarum in primiparaous women. J. Clin. Nurs. 2012, 21, 1570–1576. [Google Scholar] [CrossRef] [PubMed]
- Hajhashemi, M.; Rafieian, M.; Rouhi Boroujeni, H.A.; Miraj, S.; Memarian, S.; Keivani, A.; Haghollahi, F. The effect of Aloe vera gel and sweet almond oil on striae gravidarum in nulliparous women. J. Matern. Fetal Neonatal Med. 2017, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Sultana, Y.; Kohli, K.; Athar, M.; Khar, R.K.; Aqil, M. Effect of pre-treatment of almond oil on ultraviolet B-induced cutaneous photoaging in mice. J. Cosmet. Dermatol. 2007, 6, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Yang, W.; Li, Z.; Jia, W.; Li, J.; Zhang, P.; Xiao, T. Bitter apricot essential oil induces apoptosis of human HaCaT keratinocytes. Int. Immunopharmacol. 2016, 34, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Chrubasik, C.; Roufogalis, B.D.; Muller-Ladner, U.; Chrubasik, S. A systematic review on the Rosa canina effect and efficacy profiles. Phytother. Res. 2008, 22, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Shabykin, G.P.; Godorazhi, A.I. A polyvitamin preparation of fat-soluble vitamins (carotolin) and rose hip oil in the treatment of certain dermatoses. Vestnik Dermatol. Venerol. 1967, 41, 71–73. [Google Scholar]
- Lee, S.H.; Heo, Y.; Kim, Y.C. Effect of German chamomile oil application on alleviating atopic dermatitis-like immune alterations in mice. J. Vet. Sci. 2010, 11, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Verma, N.; Chakrabarti, R.; Das, R.H.; Gautam, H.K. Anti-inflammatory effects of shea butter through inhibition of iNOS, COX-2, and cytokines via the Nf-kappaB pathway in LPS-activated J774 macrophage cells. J. Complement. Integr. Med. 2012, 9. Article 4. [Google Scholar] [CrossRef] [PubMed]
- Hon, K.L.; Tsang, Y.C.; Pong, N.H.; Lee, V.W.; Luk, N.M.; Chow, C.M.; Leung, T.F. Patient acceptability, efficacy, and skin biophysiology of a cream and cleanser containing lipid complex with shea butter extract versus a ceramide product for eczema. Hong Kong Med. J. 2015, 21, 417–425. [Google Scholar] [PubMed]
- Edraki, M.; Akbarzadeh, A.; Hosseinzadeh, M.; Tanideh, N.; Salehi, A.; Koohi-Hosseinabadi, O. Healing effect of sea buckthorn, olive oil, and their mixture on full-thickness burn wounds. Adv. Skin Wound Care 2014, 27, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Salvini, S.; Sera, F.; Caruso, D.; Giovannelli, L.; Visioli, F.; Saieva, C.; Masala, G.; Ceroti, M.; Giovacchini, V.; Pitozzi, V.; et al. Daily consumption of a high-phenol extra-virgin olive oil reduces oxidative DNA damage in postmenopausal women. Br. J. Nutr. 2006, 95, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Fabiani, R.; De Bartolomeo, A.; Rosignoli, P.; Servili, M.; Montedoro, G.F.; Morozzi, G. Cancer chemoprevention by hydroxytyrosol isolated from virgin olive oil through G1 cell cycle arrest and apoptosis. Eur. J. Cancer Prev. 2002, 11, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Darmstadt, G.L.; Mao-Qiang, M.; Chi, E.; Saha, S.K.; Ziboh, V.A.; Black, R.E.; Santosham, M.; Elias, P.M. Impact of topical oils on the skin barrier: Possible implications for neonatal health in developing countries. Acta Paediatr. 2002, 91, 546–554. [Google Scholar] [CrossRef] [PubMed]
- Maghsoudi, H.; Gabraely, N. Epidemiology and outcome of 121 cases of chemical burn in East Azarbaijan province, Iran. Injury 2008, 39, 1042–1046. [Google Scholar] [CrossRef] [PubMed]
- Mullany, L.C.; Darmstadt, G.L.; Khatry, S.K.; Tielsch, J.M. Traditional massage of newborns in Nepal: Implications for trials of improved practice. J. Trop. Pediatr. 2005, 51, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Agero, A.L.; Verallo-Rowell, V.M. A randomized double-blind controlled trial comparing extra virgin coconut oil with mineral oil as a moisturizer for mild to moderate xerosis. Dermatitis 2004, 15, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.R.; Zhao, M.B.; Tu, P.F. Simultaneous determination of four nucleosides in Carthamus tinctorius L. and Safflower injection using high-performance liquid chromatography. J. Chin. Pharmaceut. Sci. 2009, 18, 326–330. [Google Scholar]
- Solanki, K.; Matnani, M.; Kale, M.; Joshi, K.; Bavdekar, A.; Bhave, S.; Pandit, A. Transcutaneous absorption of topically massaged oil in neonates. Indian Pediatr. 2005, 42, 998–1005. [Google Scholar] [PubMed]
- Boucetta, K.Q.; Charrouf, Z.; Derouiche, A.; Rahali, Y.; Bensouda, Y. Skin hydration in postmenopausal women: Argan oil benefit with oral and/or topical use. Prz. Menopauzalny 2014, 13, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Puglia, C.; Bonina, F. In vivo spectrophotometric evaluation of skin barrier recovery after topical application of soybean phytosterols. J. Cosmet. Sci. 2008, 59, 217–224. [Google Scholar] [PubMed]
- Ring, J.; Mohrenschlager, M. Allergy to peanut oil—Clinically relevant? J. Eur. Acad. Dermatol. Venereol. 2007, 21, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Yunginger, J.W.; Calobrisi, S.D. Investigation of the allergenicity of a refined peanut oil-containing topical dermatologic agent in persons who are sensitive to peanuts. Cutis 2001, 68, 153–155. [Google Scholar] [PubMed]
- Dar, A.A.; Arumugam, N. Lignans of sesame: Purification methods, biological activities and biosynthesis—A review. Bioorg. Chem. 2013, 50, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, T.; Fukuda, Y.; Osawa, T.; Namiki, M. Oil and Minor Components of Sesame (Sesamum-indicum L.) Strains. J. Am. Oil Chem. Soc. 1990, 67, 508–511. [Google Scholar] [CrossRef]
- Wright, S. Essential fatty acids and the skin. Br. J. Dermatol. 1991, 125, 503–515. [Google Scholar] [CrossRef] [PubMed]
- Tollesson, A.; Frithz, A. Transepidermal water loss and water content in the stratum corneum in infantile seborrhoeic dermatitis. Acta Derm. Venereol. 1993, 73, 18–20. [Google Scholar] [PubMed]
- Wisniak, J. Jojoba oil and derivatives. Prog. Chem. Fats Other Lipids 1977, 15, 167–218. [Google Scholar] [CrossRef]
- Pazyar, N.; Yaghoobi, R.; Ghassemi, M.R.; Kazerouni, A.; Rafeie, E.; Jamshydian, N. Jojoba in dermatology: A succinct review. G. Ital. Dermatol. Venereol. 2013, 148, 687–691. [Google Scholar] [PubMed]
- Nasr, M.; Abdel-Hamid, S.; Moftah, N.H.; Fadel, M.; Alyoussef, A.A. Jojoba Oil Soft Colloidal Nanocarrier of a Synthetic Retinoid: Preparation, Characterization and Clinical Efficacy in Psoriatic Patients. Curr. Drug Deliv. 2017, 14, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Shahin, M.; Hady, S.A.; Hammad, M.; Mortada, N. Novel jojoba oil-based emulsion gel formulations for clotrimazole delivery. AAPS PharmSciTech 2011, 12, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Youngs, V.L. Oat Lipids. Cereal Chem. 1978, 55, 591–597. [Google Scholar]
- Amri, Z.; Lazreg-Aref, H.; Mekni, M.; El-Gharbi, S.; Dabbaghi, O.; Mechri, B.; Hammami, M. Oil Characterization and Lipids Class Composition of Pomegranate Seeds. Biomed. Res. Int. 2017, 2017, 2037341. [Google Scholar] [CrossRef] [PubMed]
- Bogdan, C.; Iurian, S.; Tomuta, I.; Moldovan, M. Improvement of skin condition in striae distensae: Development, characterization and clinical efficacy of a cosmetic product containing Punica granatum seed oil and Croton lechleri resin extract. Drug Des. Dev. Ther. 2017, 11, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Baccarin, T.; Lemos-Senna, E. Potential Application of Nanoemulsions for Skin Delivery of Pomegranate Peel Polyphenols. AAPS PharmSciTech 2017, 18, 3307–3314. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, L.M.; Sari, M.H.M.; Cervi, V.F.; Gehrcke, M.; Barbieri, A.V.; Zborowski, V.A.; Beck, R.C.R.; Nogueira, C.W.; Cruz, L. Pomegranate seed oil nanoemulsions improve the photostability and in vivo antinociceptive effect of a non-steroidal anti-inflammatory drug. Colloids Surf. B Biointerfaces 2016, 144, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Korgavkar, K.; Wang, F. Stretch marks during pregnancy: A review of topical prevention. Br. J. Dermatol. 2015, 172, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Ilyasoğlu, H. Characterization of Rosehip (Rosa canina L.) Seed and Seed Oil. Int. J. Food Prop. 2014, 17, 1591–1598. [Google Scholar] [CrossRef]
- Maranz, S.; Kpikpi, W.; Wiesman, Z.; Sauveur, A.D.; Chapagain, B. Nutritional values and indigenous preferences for shea fruits (Vitellaria paradoxa CF Gaertn. f.) in African agroforestry parklands. Econ. Bot. 2004, 58, 588–600. [Google Scholar] [CrossRef]
| Plant Oils | Skin Barrier Repair | Anti-Bacterial Effect | Anti-Inflammatory Effect | Antioxidant Effect | Wound Healing | Skin Aging | Skin Cancer | References |
|---|---|---|---|---|---|---|---|---|
| Olive oil | No | ? | Yes | Yes | Yes | Possible effect | Yes | Cardoso CR et al., 2004 [50] Nasopoulou C et al., 2014 [58] Donato-Trancoso A et al., 2016 [59] Zahmatkesh M et al., 2015 [60] Budiyanto A et al., 2000 [61] Danby SG et al., 2013 [62] Cooke A et al., 2016 [63] Norlen L et al., 2016 [64] Korac RR et al., 2011 [65] |
| Sunflower seed oil | Yes | ? | Yes | ? | Possible effect | ? | Yes | Cardoso et al., 2004 [50] Danby SG et al., 2013 [62] Cooke A et al., 2016 [63] Norlen L et al., 2016 [64] Kapadia GJ et al., 2002 [66] |
| Grape seed oil | ? | Yes | Possible effect | Yes | Yes | Possible effect | Possible effect | Kapadia GJ et al., 2002 [66] Shivananda Nayak B et al., 2011 [67] Khanna S et al., 2002 [68] Chan MM et al., 2002 [69] Park K et al., 2013 [70] Davidov-Pardo G et al., 2015 [71] Shinagawa FB et al., 2015 [72] |
| Coconut oil | Yes | Yes | Yes | Yes | Yes | Yes | ? | Evangelista MT et al., 2014 [73] Nevin KG et al., 2010 [74] Kim S et al., 2017 [75] Korac RR et al., 2011 [65] Preuss HG et al., 2005 [76] Oyi AR et al., 2010 [77] Esquenazi D et al., 2002 [78] |
| Safflower seed oil | ? | ? | Yes | ? | ? | ? | ? | Chen CY et al., 2007 [79] Lopez-Lazaro M, 2009 [80] |
| Argan oil | Yes | ? | Yes | ? | Yes | ? | Possible effect | Boucetta KQ et al., 2015 [81] Manca ML et al., 2016 [82] Jordan M et al., 2012 [83] Avsar U et al., 2016 [84] |
| Soybean oil | Yes | Yes | Yes | Yes | ? | ? | ? | Patzelt A et al., 2012 [11] Jhan JK et al., 2016 [85] Kim JN et al., 2017 [86] Bonina F et al., 2005 [87] |
| Peanut oil | Yes | ? | ? | ? | ? | Yes | Yes | Korac RR et al., 2011 [65] Zhai H et al., 2003 [88] Lasne C et al., 1991 [89] |
| Sesame oil | Possible effect | ? | Yes | Yes | ? | Yes | Yes | Kapadia GJ et al., 2002 [66] Korac RR et al., 2011 [65] Chiang JP et al., 2005 [90] Nasiri M et al., 2017 [91] Hsu DZ et al., 2013 [92] Bigdeli Shamloo et al., 2015 [93] |
| Avocado oil | ? | ? | Possible effect | ? | Yes | ? | ? | Patzelt A et al., 2012 [11] De Oliveira AP et al., 2013 [94] Nayak BS et al., 2008 [95] Lamaud E et al., 1982 [96] |
| Borage oil | Yes | ? | Possible effect | ? | ? | ? | ? | Kanehara S et al., 2007 [97] |
| Jojoba oil | Yes | Possible effect | Yes | Yes | Yes | Yes | ? | Meier L et al., 2012 [98] Ranzato E et al., 2011 [99] |
| Oat oil | Yes | Possible effect | Yes | Yes | ? | ? | ? | Nebus J et al., 2009 [100] Reynertson KA et al., 2015 [101] Sur R et al., 2008 [102] Chon SH et al., 2015 [103] |
| Pomegranate seed oil | ? | ? | ? | Yes | ? | Possible effect | Possible effect | Hora J et al., 2003 [104] |
| Almond oil | Possible effect | ? | ? | ? | ? | Yes | ? | Timur Tashan S et al., 2012 [105] Hajhashemi M et al., 2017 [106] Sultana Y et al., 2007 [107] |
| Bitter apricot oil | ? | ? | ? | ? | ? | ? | Possible effect | Li K et al., 2016 [108] |
| Rose hip oil | Possible effect | ? | Yes | Yes | ? | Yes | ? | Chrubasik C et al., 2008 [109] Shabykin GP et al., 1967 [110] |
| German chamomile oil | Possible effect | ? | Yes | ? | ? | ? | ? | Lee SH et al., 2010 [111] |
| Shea butter | Possible effect | ? | Yes | Yes | ? | ? | ? | Verma N et al., 2012 [112] Hon KL et al., 2015 [113] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, T.-K.; Zhong, L.; Santiago, J.L. Anti-Inflammatory and Skin Barrier Repair Effects of Topical Application of Some Plant Oils. Int. J. Mol. Sci. 2018, 19, 70. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms19010070
Lin T-K, Zhong L, Santiago JL. Anti-Inflammatory and Skin Barrier Repair Effects of Topical Application of Some Plant Oils. International Journal of Molecular Sciences. 2018; 19(1):70. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms19010070
Chicago/Turabian StyleLin, Tzu-Kai, Lily Zhong, and Juan Luis Santiago. 2018. "Anti-Inflammatory and Skin Barrier Repair Effects of Topical Application of Some Plant Oils" International Journal of Molecular Sciences 19, no. 1: 70. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms19010070