Impact of Bone Fracture on Ischemic Stroke Recovery
Abstract
:1. Introduction
2. Bone Fracture Causes Hippocampal Inflammation and Cognitive Dysfunction
3. Bone Fracture Exacerbates Ischemic Stroke Injury
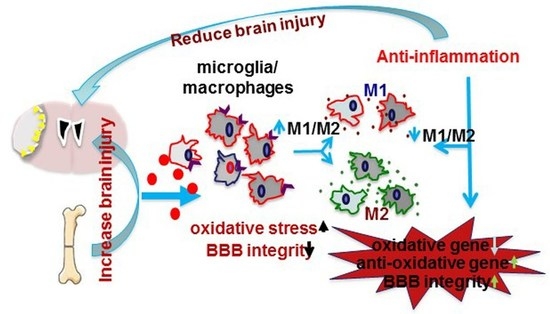
4. Inhibition of Inflammation Could Reduce the Negative Impact of Bone Fracture on Ischemic Stroke Recovery
5. Milestone Studies in Understanding Bone Fracture and Stroke Interplay
6. Clinical Implications
7. Future Directions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Kapral, M.K.; Fang, J.; Alibhai, S.M.; Cram, P.; Cheung, A.M.; Casaubon, L.K.; Prager, M.; Stamplecoski, M.; Rashkovan, B.; Austin, P.C. Risk of fractures after stroke: Results from the Ontario stroke registry. Neurology 2017, 88, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, E.S.; Fletcher, A.; Bloch, K.V.; Rodrigues, L.C. Risk factors for falls with severe fracture in elderly people living in a middle-income country: A. case control study. BMC Geriatr. 2008, 8, 21. [Google Scholar] [CrossRef] [PubMed]
- Myint, P.K.; Poole, K.E.; Warburton, E.A. Hip fractures after stroke and their prevention. QJM 2007, 100, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Huo, K.; Hashim, S.I.; Yong, K.L.; Su, H.; Qu, Q.M. Impact and risk factors of post-stroke bone fracture. World J. Exp. Med. 2016, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sennerby, U.; Melhus, H.; Gedeborg, R.; Byberg, L.; Garmo, H.; Ahlbom, A.; Pedersen, N.L.; Michaelsson, K. Cardiovascular diseases and risk of hip fracture. JAMA 2009, 302, 1666–1673. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.; Oden, A.; Johnell, O. Acute and long-term increase in fracture risk after hospitalization for stroke. Stroke 2001, 32, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Chung, S.D.; Xirasagar, S.; Jaw, F.S.; Lin, H.C. Increased risk of stroke in the year after a hip fracture: A population-based follow-up study. Stroke 2011, 42, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Lakshminarayan, K.; Schissel, C.; Anderson, D.C.; Vazquez, G.; Jacobs, D.R., Jr.; Ezzeddine, M.; Luepker, R.V.; Virnig, B.A. Five-year rehospitalization outcomes in a cohort of patients with acute ischemic stroke: Medicare linkage study. Stroke 2011, 42, 1556–1562. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, A.B.; Ehrenstein, V.; Szepligeti, S.K.; Sorensen, H.T. Hip fracture, comorbidity, and the risk of myocardial infarction and stroke: A Danish nationwide cohort study, 1995–2015. J. Bone Miner. Res. 2017, 32, 2339–2346. [Google Scholar] [CrossRef] [PubMed]
- Doyle, K.P.; Quach, L.N.; Sole, M.; Axtell, R.C.; Nguyen, T.V.; Soler-Llavina, G.J.; Jurado, S.; Han, J.; Steinman, L.; Longo, F.M.; et al. B-lymphocyte-mediated delayed cognitive impairment following stroke. J. Neurosci. 2015, 35, 2133–2145. [Google Scholar] [CrossRef] [PubMed]
- Seitz, D.P.; Adunuri, N.; Gill, S.S.; Rochon, P.A. Prevalence of dementia and cognitive impairment among older adults with hip fractures. J. Am. Med. Dir. Assoc. 2011, 12, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Sathiyakumar, V.; Avilucea, F.R.; Whiting, P.S.; Jahangir, A.A.; Mir, H.R.; Obremskey, W.T.; Sethi, M.K. Risk factors for adverse cardiac events in hip fracture patients: An analysis of NSQIP data. Int. Orthop. 2016, 40, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Van Staa, T.P.; Dennison, E.M.; Leufkens, H.G.; Cooper, C. Epidemiology of fractures in England and wales. Bone 2001, 29, 517–522. [Google Scholar] [CrossRef]
- Semenkovich, C.F. Insulin resistance and a long, strange trip. N. Engl. J. Med. 2016, 374, 1378–1379. [Google Scholar] [CrossRef] [PubMed]
- Kernan, W.N.; Viscoli, C.M.; Furie, K.L.; Young, L.H.; Inzucchi, S.E.; Gorman, M.; Guarino, P.D.; Lovejoy, A.M.; Peduzzi, P.N.; Conwit, R.; et al. Pioglitazone after ischemic stroke or transient ischemic attack. N. Engl. J. Med. 2016, 374, 1321–1331. [Google Scholar] [CrossRef] [PubMed]
- Jauch, E.C.; Saver, J.L.; Adams, H.P., Jr.; Bruno, A.; Connors, J.J.; Demaerschalk, B.M.; Khatri, P.; McMullan, P.W., Jr.; Qureshi, A.I.; Rosenfield, K.; et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American heart association/American stroke association. Stroke 2013, 44, 870–947. [Google Scholar] [CrossRef] [PubMed]
- Vidal, S.M.; Chaudhry, F.S.; Schneck, M. Management of acute ischemic stroke. Hosp. Pract. (1995) 2013, 41, 108–122. [Google Scholar] [CrossRef] [PubMed]
- Pena, I.D.; Borlongan, C.; Shen, G.; Davis, W. Strategies to extend thrombolytic time window for ischemic stroke treatment: An unmet clinical need. J. Stroke 2017, 19, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, T.; Kamiya, T.; Deguchi, K.; Inaba, T.; Zhang, H.; Shang, J.; Miyazaki, K.; Ohtsuka, A.; Katayama, Y.; Abe, K. Dissociation and protection of the neurovascular unit after thrombolysis and reperfusion in ischemic rat brain. J. Cereb. Blood Flow Metab. 2009, 29, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Dela Pena, I.C.; Yoo, A.; Tajiri, N.; Acosta, S.A.; Ji, X.; Kaneko, Y.; Borlongan, C.V. Granulocyte colony-stimulating factor attenuates delayed tpa-induced hemorrhagic transformation in ischemic stroke rats by enhancing angiogenesis and vasculogenesis. J. Cereb. Blood Flow Metab. 2015, 35, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Jadhav, A.P.; Desai, S.M.; Kenmuir, C.L.; Rocha, M.; Starr, M.T.; Molyneaux, B.J.; Gross, B.A.; Jankowitz, B.T.; Jovin, T.G. Eligibility for endovascular trial enrollment in the 6- to 24-hour time window: Analysis of a single comprehensive stroke center. Stroke 2018, 49, 1015–1017. [Google Scholar] [CrossRef] [PubMed]
- Diamandis, T.; Borlongan, C.V. One, two, three steps toward cell therapy for stroke. Stroke 2015, 46, 588–591. [Google Scholar] [CrossRef] [PubMed]
- Hankey, G.J. Secondary stroke prevention. Lancet Neurol. 2014, 13, 178–194. [Google Scholar] [CrossRef]
- Palan, J.; Odutola, A.; White, S.P. Is clopidogrel stopped prior to hip fracture surgery—A survey of current practice in the United Kingdom. Injury 2007, 38, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Tatemichi, T.K.; Paik, M.; Bagiella, E.; Desmond, D.W.; Pirro, M.; Hanzawa, L.K. Dementia after stroke is a predictor of long-term survival. Stroke 1994, 25, 1915–1919. [Google Scholar] [CrossRef] [PubMed]
- Lo Coco, D.; Lopez, G.; Corrao, S. Cognitive impairment and stroke in elderly patients. Vasc. Health Risk Manag. 2016, 12, 105–116. [Google Scholar] [PubMed]
- Marengoni, A.; Corrao, S.; Nobili, A.; Tettamanti, M.; Pasina, L.; Salerno, F.; Iorio, A.; Marcucci, M.; Bonometti, F.; Mannucci, P.M. In-hospital death according to dementia diagnosis in acutely ill elderly patients: The reposi study. Int. J. Geriatr. Psychiatry 2011, 26, 930–936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marengoni, A.; Nobili, A.; Romano, V.; Tettamanti, M.; Pasina, L.; Djade, S.; Corrao, S.; Salerno, F.; Iorio, A.; Marcucci, M.; et al. Adverse clinical events and mortality during hospitalization and 3 months after discharge in cognitively impaired elderly patients. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Nadler, J.W.; Browndyke, J.; Terrando, N.; Ponnusamy, V.; Cohen, H.J.; Whitson, H.E.; Mathew, J.P. Postoperative cognitive dysfunction: Minding the gaps in our knowledge of a common postoperative complication in the elderly. Anesthesiol. Clin. 2015, 33, 517–550. [Google Scholar] [CrossRef] [PubMed]
- Moller, J.T.; Cluitmans, P.; Rasmussen, L.S.; Houx, P.; Rasmussen, H.; Canet, J.; Rabbitt, P.; Jolles, J.; Larsen, K.; Hanning, C.D.; et al. Long-term postoperative cognitive dysfunction in the elderly ispocd1 study. Ispocd investigators. International study of post-operative cognitive dysfunction. Lancet 1998, 351, 857–861. [Google Scholar] [CrossRef]
- Mathew, R.O.; Hsu, W.H.; Young, Y. Effect of comorbidity on functional recovery after hip fracture in the elderly. Am. J. Phys. Med. Rehabil. 2013, 92, 686–696. [Google Scholar] [CrossRef] [PubMed]
- Kannus, P.; Parkkari, J.; Sievanen, H.; Heinonen, A.; Vuori, I.; Jarvinen, M. Epidemiology of hip fractures. Bone 1996, 18, 57–63. [Google Scholar] [CrossRef]
- Cauley, J.A. Osteoporosis: Fracture epidemiology update 2016. Curr. Opin. Rheumatol. 2017, 29, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Gruber-Baldini, A.L.; Zimmerman, S.; Morrison, R.S.; Grattan, L.M.; Hebel, J.R.; Dolan, M.M.; Hawkes, W.; Magaziner, J. Cognitive impairment in hip fracture patients: Timing of detection and longitudinal follow-up. J. Am. Geriatr. Soc. 2003, 51, 1227–1236. [Google Scholar] [CrossRef] [PubMed]
- Monk, T.G.; Weldon, B.C.; Garvan, C.W.; Dede, D.E.; van der Aa, M.T.; Heilman, K.M.; Gravenstein, J.S. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology 2008, 108, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Tzimas, P.; Petrou, A.; Laou, E.; Milionis, H.; Mikhailidis, D.P.; Papadopoulos, G. Impact of metabolic syndrome in surgical patients: Should we bother? Br. J. Anaesth. 2015, 115, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.S.; Gooch, J.L.; Garcia, P.S. Postoperative cognitive dysfunction, Alzheimer's disease, and anesthesia. Int. J. Neurosci. 2014, 124, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Degos, V.; Koch, L.G.; Britton, S.L.; Zhu, Y.; Vacas, S.; Terrando, N.; Nelson, J.; Su, X.; Maze, M. Surgery results in exaggerated and persistent cognitive decline in a rat model of the metabolic syndrome. Anesthesiology 2013, 118, 1098–1105. [Google Scholar] [CrossRef] [PubMed]
- Salazar, F.; Donate, M.; Boget, T.; Bogdanovich, A.; Basora, M.; Torres, F.; Fabregas, N. Intraoperative warming and post-operative cognitive dysfunction after total knee replacement. Acta Anaesthesiol. Scand. 2011, 55, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Samuelsson, B.; Hedstrom, M.I.; Ponzer, S.; Soderqvist, A.; Samnegard, E.; Thorngren, K.G.; Cederholm, T.; Saaf, M.; Dalen, N. Gender differences and cognitive aspects on functional outcome after hip fracture—A 2 years’ follow-up of 2134 patients. Age Ageing 2009, 38, 686–692. [Google Scholar] [CrossRef] [PubMed]
- Gruber-Baldini, A.L.; Hosseini, M.; Orwig, D.; Grattan, L.; Chiles Shaffer, N.; Hochberg, M.; Magaziner, J. Cognitive differences between men and women who fracture their hip and impact on six-month survival. J. Am. Geriatr. Soc. 2017, 65, e64–e69. [Google Scholar] [CrossRef] [PubMed]
- Cibelli, M.; Fidalgo, A.R.; Terrando, N.; Ma, D.; Monaco, C.; Feldmann, M.; Takata, M.; Lever, I.J.; Nanchahal, J.; Fanselow, M.S.; et al. Role of interleukin-1beta in postoperative cognitive dysfunction. Ann. Neurol. 2010, 68, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Terrando, N.; Monaco, C.; Ma, D.; Foxwell, B.M.; Feldmann, M.; Maze, M. Tumor necrosis factor-alpha triggers a cytokine cascade yielding postoperative cognitive decline. Proc. Natl. Acad. Sci. USA 2010, 107, 20518–20522. [Google Scholar] [CrossRef] [PubMed]
- Terrando, N.; Eriksson, L.I.; Ryu, J.K.; Yang, T.; Monaco, C.; Feldmann, M.; Jonsson Fagerlund, M.; Charo, I.F.; Akassoglou, K.; Maze, M. Resolving postoperative neuroinflammation and cognitive decline. Ann. Neurol. 2011, 70, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Xu, J.; Ma, D.; Zeng, Y.; Cibelli, M.; Maze, M. Postoperative impairment of cognitive function in rats: A possible role for cytokine-mediated inflammation in the hippocampus. Anesthesiology 2007, 106, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Degos, V.; Maze, M.; Vacas, S.; Hirsch, J.; Guo, Y.; Shen, F.; Jun, K.; van Rooijen, N.; Gressens, P.; Young, W.L.; et al. Bone fracture exacerbates murine ischemic cerebral injury. Anesthesiology 2013, 118, 1362–1372. [Google Scholar] [CrossRef] [PubMed]
- Han, Z.; Li, L.; Wang, L.; Degos, V.; Maze, M.; Su, H. Alpha-7 nicotinic acetylcholine receptor agonist treatment reduces neuroinflammation, oxidative stress and brain injury in mice with ischemic stroke and bone fracture. J. Neurochem. 2014, 131, 498–508. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Kang, S.; Zou, D.; Zhan, L.; Li, Z.; Zhu, W.; Su, H. Bone fracture pre-ischemic stroke exacerbates ischemic cerebral injury in mice. PLoS ONE 2016, 11, e0153835. [Google Scholar] [CrossRef] [PubMed]
- Kigerl, K.A.; Gensel, J.C.; Ankeny, D.P.; Alexander, J.K.; Donnelly, D.J.; Popovich, P.G. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J. Neurosci. 2009, 29, 13435–13444. [Google Scholar] [CrossRef] [PubMed]
- Durafourt, B.A.; Moore, C.S.; Zammit, D.A.; Johnson, T.A.; Zaguia, F.; Guiot, M.C.; Bar-Or, A.; Antel, J.P. Comparison of polarization properties of human adult microglia and blood-derived macrophages. Glia 2012, 60, 717–727. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Li, P.; Guo, Y.; Wang, H.; Leak, R.K.; Chen, S.; Gao, Y.; Chen, J. Microglia/macrophage polarization dynamics reveal novel mechanism of injury expansion after focal cerebral ischemia. Stroke 2012, 43, 3063–3070. [Google Scholar] [CrossRef] [PubMed]
- Han, Z.; Shen, F.; He, Y.; Degos, V.; Camus, M.; Maze, M.; Young, W.L.; Su, H. Activation of alpha-7 nicotinic acetylcholine receptor reduces ischemic stroke injury through reduction of pro-inflammatory macrophages and oxidative stress. PLoS ONE 2014, 9, e105711. [Google Scholar]
- Klein, J.A.; Ackerman, S.L. Oxidative stress, cell cycle, and neurodegeneration. J. Clin. Investig. 2003, 111, 785–793. [Google Scholar] [CrossRef] [PubMed]
- Paravicini, T.M.; Sobey, C.G. Cerebral vascular effects of reactive oxygen species: Recent evidence for a role of nadph-oxidase. Clin. Exp. Pharmacol. Physiol. 2003, 30, 855–859. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wei, X.; Liu, K.; Zhang, X.; Yang, F.; Zhang, H.; He, Y.; Zhu, T.; Li, F.; Shi, W.; et al. NOX2 deficiency ameliorates cerebral injury through reduction of complexin II-mediated glutamate excitotoxicity in experimental stroke. Free Radic. Biol. Med. 2013, 65, 942–951. [Google Scholar] [CrossRef] [PubMed]
- Anrather, J.; Racchumi, G.; Iadecola, C. NF-kappaB regulates phagocytic NADPH oxidase by inducing the expression of gp91phox. J. Biol. Chem. 2006, 281, 5657–5667. [Google Scholar] [CrossRef] [PubMed]
- Palencia, G.; Garcia, E.; Osorio-Rico, L.; Trejo-Solis, C.; Escamilla-Ramirez, A.; Sotelo, J. Neuroprotective effect of thalidomide on MPTP-induced toxicity. Neurotoxicology 2015, 47, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Zou, D.; Luo, M.; Han, Z.; Zhan, L.; Zhu, W.; Kang, S.; Bao, C.; Li, Z.; Nelson, J.; Zhang, R.; et al. Activation of alpha-7 nicotinic acetylcholine receptor reduces brain edema in mice with ischemic stroke and bone fracture. Mol. Neurobiol. 2016, 34, 8278–8286. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.B.; Sig Choi, J.; Yu, Y.M.; Nam, K.; Piao, C.S.; Kim, S.W.; Lee, M.H.; Han, P.L.; Park, J.S.; Lee, J.K. Hmgb1, a novel cytokine-like mediator linking acute neuronal death and delayed neuroinflammation in the postischemic brain. J. Neurosci. 2006, 26, 6413–6421. [Google Scholar] [CrossRef] [PubMed]
- Vacas, S.; Degos, V.; Tracey, K.J.; Maze, M. High-mobility group box 1 protein initiates postoperative cognitive decline by engaging bone marrow-derived macrophages. Anesthesiology 2014, 120, 1160–1167. [Google Scholar] [CrossRef] [PubMed]
- Andersson, U.; Wang, H.; Palmblad, K.; Aveberger, A.C.; Bloom, O.; Erlandsson-Harris, H.; Janson, A.; Kokkola, R.; Zhang, M.; Yang, H.; et al. High mobility group 1 protein (hmg-1) stimulates proinflammatory cytokine synthesis in human monocytes. J. Exp. Med. 2000, 192, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Valdearcos, M.; Uchida, Y.; Lutrin, D.; Koliwad, S.K.; Maze, M. Microglia mediate postoperative hippocampal neuroinflammation and cognitive decline in mice. JCI Insight 2017, 2, e91229. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Takahashi, H.K.; Liu, K.; Wake, H.; Liu, R.; Maruo, T.; Date, I.; Yoshino, T.; Ohtsuka, A.; Mori, S.; et al. Anti-high mobility group box-1 monoclonal antibody protects the blood-brain barrier from ischemia-induced disruption in rats. Stroke 2011, 42, 1420–1428. [Google Scholar] [CrossRef] [PubMed]
- Boutin, H.; LeFeuvre, R.A.; Horai, R.; Asano, M.; Iwakura, Y.; Rothwell, N.J. Role of il-1alpha and il-1beta in ischemic brain damage. J. Neurosci. 2001, 21, 5528–5534. [Google Scholar] [CrossRef] [PubMed]
- Murta, V.; Farias, M.I.; Pitossi, F.J.; Ferrari, C.C. Chronic systemic il-1beta exacerbates central neuroinflammation independently of the blood-brain barrier integrity. J. Neuroimmunol. 2015, 278, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Argaw, A.T.; Zhang, Y.; Snyder, B.J.; Zhao, M.L.; Kopp, N.; Lee, S.C.; Raine, C.S.; Brosnan, C.F.; John, G.R. Il-1beta regulates blood-brain barrier permeability via reactivation of the hypoxia-angiogenesis program. J. Immunol. 2006, 177, 5574–5584. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Jin, S.; Sonobe, Y.; Cheng, Y.; Horiuchi, H.; Parajuli, B.; Kawanokuchi, J.; Mizuno, T.; Takeuchi, H.; Suzumura, A. Interleukin-1beta induces blood-brain barrier disruption by downregulating sonic hedgehog in astrocytes. PLoS ONE 2014, 9, e110024. [Google Scholar]
- Chen, X.; Sadowska, G.B.; Zhang, J.; Kim, J.E.; Cummings, E.E.; Bodge, C.A.; Lim, Y.P.; Makeyev, O.; Besio, W.G.; Gaitanis, J.; et al. Neutralizing anti-interleukin-1beta antibodies modulate fetal blood-brain barrier function after ischemia. Neurobiol. Dis. 2015, 73, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Rachal Pugh, C.; Fleshner, M.; Watkins, L.R.; Maier, S.F.; Rudy, J.W. The immune system and memory consolidation: A role for the cytokine il-1beta. Neurosci. Biobehav. Rev. 2001, 25, 29–41. [Google Scholar] [CrossRef]
- Murray, C.L.; Obiang, P.; Bannerman, D.; Cunningham, C. Endogenous il-1 in cognitive function and anxiety: A study in IL-1RI−/− mice. PLoS ONE 2013, 8, e78385. [Google Scholar] [CrossRef] [PubMed]
- Pavlov, V.A.; Parrish, W.R.; Rosas-Ballina, M.; Ochani, M.; Puerta, M.; Ochani, K.; Chavan, S.; Al-Abed, Y.; Tracey, K.J. Brain acetylcholinesterase activity controls systemic cytokine levels through the cholinergic anti-inflammatory pathway. Brain Behav. Immun. 2009, 23, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Borovikova, L.V.; Ivanova, S.; Zhang, M.; Yang, H.; Botchkina, G.I.; Watkins, L.R.; Wang, H.; Abumrad, N.; Eaton, J.W.; Tracey, K.J. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 2000, 405, 458–462. [Google Scholar] [CrossRef] [PubMed]
- Bernik, T.R.; Friedman, S.G.; Ochani, M.; DiRaimo, R.; Susarla, S.; Czura, C.J.; Tracey, K.J. Cholinergic antiinflammatory pathway inhibition of tumor necrosis factor during ischemia reperfusion. J. Vasc. Surg. 2002, 36, 1231–1236. [Google Scholar] [CrossRef] [PubMed]
- Bernik, T.R.; Friedman, S.G.; Ochani, M.; DiRaimo, R.; Ulloa, L.; Yang, H.; Sudan, S.; Czura, C.J.; Ivanova, S.M.; Tracey, K.J. Pharmacological stimulation of the cholinergic antiinflammatory pathway. J. Exp. Med. 2002, 195, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Yu, M.; Ochani, M.; Amella, C.A.; Tanovic, M.; Susarla, S.; Li, J.H.; Yang, H.; Ulloa, L.; Al-Abed, Y.; et al. Nicotinic acetylcholine receptor alpha7 subunit is an essential regulator of inflammation. Nature 2003, 421, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Cheyuo, C.; Wu, R.; Zhou, M.; Jacob, A.; Coppa, G.; Wang, P. Ghrelin suppresses inflammation and neuronal nitric oxide synthase in focal cerebral ischemia via the vagus nerve. Shock 2011, 35, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, D.; Ottani, A.; Mioni, C.; Bazzani, C.; Galantucci, M.; Minutoli, L.; Bitto, A.; Zaffe, D.; Botticelli, A.R.; Squadrito, F.; et al. Neuroprotection in focal cerebral ischemia owing to delayed treatment with melanocortins. Eur. J. Pharmacol. 2007, 570, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Shimohama, S.; Greenwald, D.L.; Shafron, D.H.; Akaika, A.; Maeda, T.; Kaneko, S.; Kimura, J.; Simpkins, C.E.; Day, A.L.; Meyer, E.M. Nicotinic alpha 7 receptors protect against glutamate neurotoxicity and neuronal ischemic damage. Brain Res. 1998, 779, 359–363. [Google Scholar] [CrossRef]
- Bertrand, N.; Ishii, H.; Beley, A.; Spatz, M. Biphasic striatal acetylcholine release during and after transient cerebral ischemia in gerbils. J. Cereb. Blood Flow Metab. 1993, 13, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, N.; Ishii, H.; Spatz, M. Cerebral ischemia in young and adult gerbils: Effects on cholinergic metabolism. Neurochem. Int. 1996, 28, 293–297. [Google Scholar] [CrossRef]
- Krafft, P.R.; Altay, O.; Rolland, W.B.; Duris, K.; Lekic, T.; Tang, J.; Zhang, J.H. Alpha7 nicotinic acetylcholine receptor agonism confers neuroprotection through gsk-3beta inhibition in a mouse model of intracerebral hemorrhage. Stroke 2012, 43, 844–850. [Google Scholar] [CrossRef] [PubMed]
- Duris, K.; Manaenko, A.; Suzuki, H.; Rolland, W.B.; Krafft, P.R.; Zhang, J.H. Alpha7 nicotinic acetylcholine receptor agonist pnu-282987 attenuates early brain injury in a perforation model of subarachnoid hemorrhage in rats. Stroke 2011, 42, 3530–3536. [Google Scholar] [CrossRef] [PubMed]
- Terrando, N.; Yang, T.; Ryu, J.K.; Newton, P.T.; Monaco, C.; Feldmann, M.; Ma, D.; Akassoglou, K.; Maze, M. Stimulation of the alpha7 nicotinic acetylcholine receptor protects against neuroinflammation after tibia fracture and endotoxemia in mice. Mol. Med. 2015, 20, 667–675. [Google Scholar] [PubMed]
- Lo, E.H. T time in the brain. Nat. Med. 2009, 15, 844–846. [Google Scholar] [CrossRef] [PubMed]
- Hayakawa, K.; Qiu, J.; Lo, E.H. Biphasic actions of hmgb1 signaling in inflammation and recovery after stroke. Ann. N. Y. Acad. Sci. 2010, 1207, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Petrovic-Djergovic, D.; Goonewardena, S.N.; Pinsky, D.J. Inflammatory disequilibrium in stroke. Circ. Res. 2016, 119, 142–158. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Mozaffarian, D.; Roger, V.L.; Benjamin, E.J.; Berry, J.D.; Borden, W.B.; Bravata, D.M.; Dai, S.; Ford, E.S.; Fox, C.S.; et al. Heart disease and stroke statistics—2013 update: A report from the American heart association. Circulation 2013, 127, e6–e245. [Google Scholar] [CrossRef] [PubMed]
- Melton, L.J., 3rd. Who has osteoporosis? A conflict between clinical and public health perspectives. J. Bone Miner. Res. 2000, 15, 2309–2314. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.H.; Lin, C.L.; Hsu, H.C.; Chung, W.S. Increased risk of stroke among hip fracture patients: A nationwide cohort study. Osteoporos. Int. 2015, 26, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Mandal, P.K.; Simplaceanu, V.; Fodale, V. Intravenous anesthetic diazepam does not induce amyloid-beta peptide oligomerization but diazepam co-administered with halothane oligomerizes amyloid-beta peptide: An NMR study. J. Alzheimers Dis. 2010, 20, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Perucho, J.; Rubio, I.; Casarejos, M.J.; Gomez, A.; Rodriguez-Navarro, J.A.; Solano, R.M.; De Yebenes, J.G.; Mena, M.A. Anesthesia with isoflurane increases amyloid pathology in mice models of Alzheimer’s disease. J. Alzheimers Dis. 2010, 19, 1245–1257. [Google Scholar] [CrossRef] [PubMed]
- Hedbeck, C.J.; Inngul, C.; Blomfeldt, R.; Ponzer, S.; Tornkvist, H.; Enocson, A. Internal fixation versus cemented hemiarthroplasty for displaced femoral neck fractures in patients with severe cognitive dysfunction: A randomized controlled trial. J. Orthop. Trauma 2013, 27, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.Z.; Yao, R.; Zhang, Z.; Xu, H.; Wang, L.W. Parecoxib prevents early postoperative cognitive dysfunction in elderly patients undergoing total knee arthroplasty: A double-blind, randomized clinical consort study. Medicine 2016, 95, e4082. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Sands, L.P.; Vaurio, L.; Mullen, E.A.; Leung, J.M. The effects of postoperative pain and its management on postoperative cognitive dysfunction. Am. J. Geriatr. Psychiatry 2007, 15, 50–59. [Google Scholar] [CrossRef] [PubMed]
| Year | Authors | Major Discovery |
|---|---|---|
| 2010 | Cibelli et al. | TNF-α an upstream mediator for hippocampal IL-1β following tibia fracture |
| 2010 | Terrando et al. | HMGB1 initiate inflammatory cascade post-bone fracture which causes cognitive dysfunction |
| 2013 | Degos et al. | HMGB1 antibody reduces cell death in a fracture-enhanced stroke |
| 2014 | Han et al. | α7 nAChR agonists diminishes microglia/macrophage infiltration of the peri-infarct region |
| 2014 | Vacas et al. | HMGB1 antibody decreased BBB permeability after fracture-enhanced stroke |
| 2016 | Zou et al. | PHA treatment attenuated brain edema and enhanced BBB integrity in fracture-enhanced stroke |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wei, M.; Lyu, H.; Huo, K.; Su, H. Impact of Bone Fracture on Ischemic Stroke Recovery. Int. J. Mol. Sci. 2018, 19, 1533. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms19051533
Wei M, Lyu H, Huo K, Su H. Impact of Bone Fracture on Ischemic Stroke Recovery. International Journal of Molecular Sciences. 2018; 19(5):1533. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms19051533
Chicago/Turabian StyleWei, Meng, Haiyian Lyu, Kang Huo, and Hua Su. 2018. "Impact of Bone Fracture on Ischemic Stroke Recovery" International Journal of Molecular Sciences 19, no. 5: 1533. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms19051533