Intranasal Borna Disease Virus (BoDV-1) Infection: Insights into Initial Steps and Potential Contagiosity
Abstract
:1. Introduction
2. Results
2.1. Clinical Findings and Histopathology
2.2. Detection of BoDV-1-N, BoDV-N-1-Specific Genomic RNA (gRNA), and mRNA
2.3. Characterization and BoDV-1 Infection of the Culture of the OM
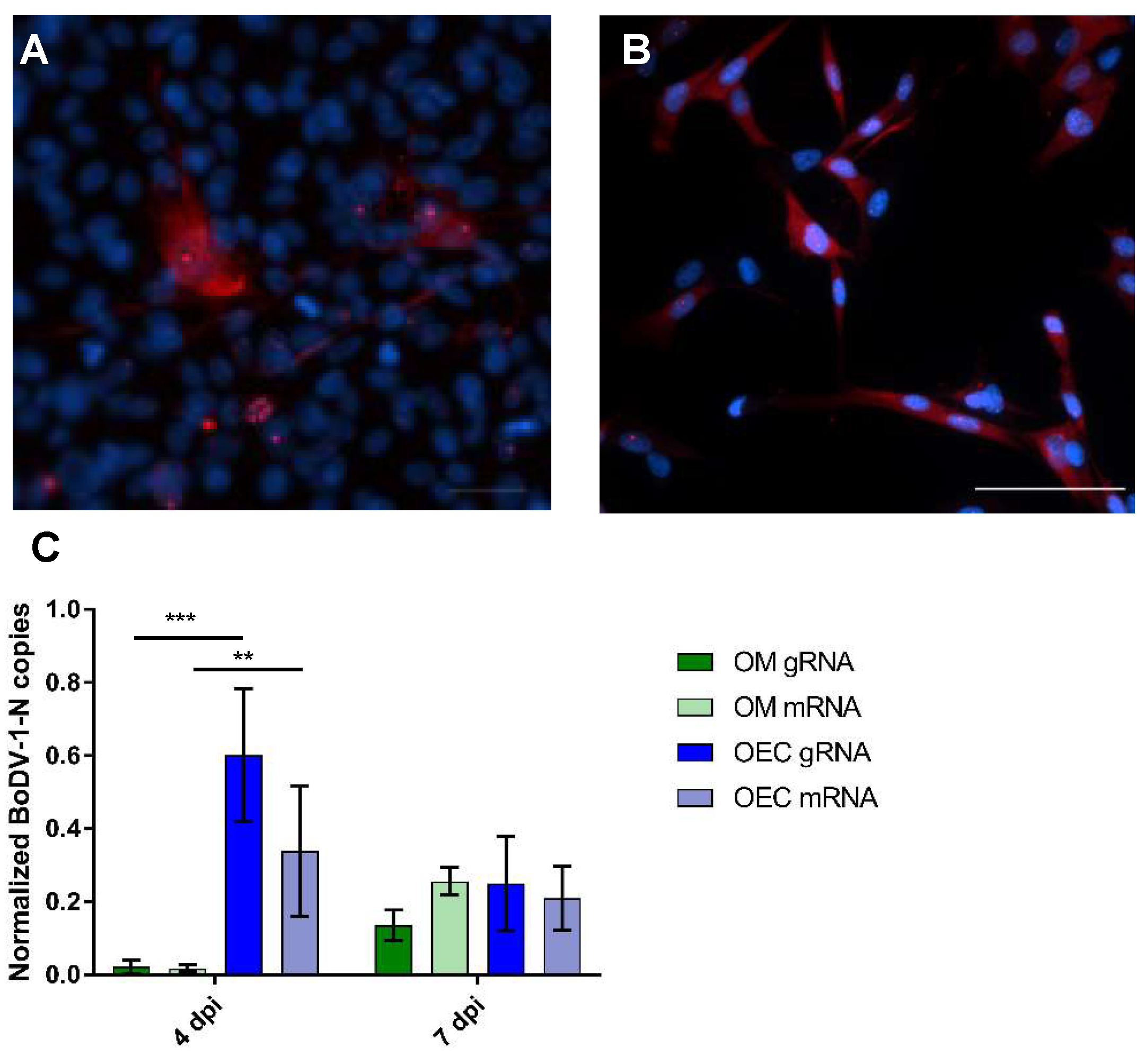
2.4. Comparative Analysis of BoDV-1 Infection in the Culture of the OM and in OECs
3. Discussion
3.1. Clinic and Histopathology
3.2. Characterization of Viral Spread
3.3. In Vitro Characterization of the Infection of the OM
3.4. BoDV-1-Infection of the Cell Cultures
3.5. Comparative BoDV-1-Infection of OM and OECs
4. Materials and Methods
4.1. Virus Stock Preparation
4.2. Intranasal Infection of Rats
4.3. Tissue Preparation and Histology
4.4. Immunohistochemistry
4.5. In Situ Hybridization (ISH)
4.6. Evaluation and Statistical Analysis of Viral Antigen and RNA Detection by Immunohistochemistry and In Situ Hybridization
4.7. Culture of the Rat Olfactory Mucosa
4.8. Cell Culture of Purified Adult Canine and Rat Olfactory Ensheathing Cells (OECs)
4.9. BoDV-1-Infection of the Cell Cultures
4.10. Immunofluorescence (IF) of the Cell Cultures
4.11. Characterization of the Culture of the OM
4.12. Quantitative Real Time RT-PCR to Determine Viral Replication (BoDV-1 gRNA) and Transcription (BoDV-1 mRNA)
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Briese, T.; Schneemann, A.; Lewis, A.J.; Park, Y.S.; Kim, S.; Ludwig, H.; Lipkin, W.I. Genomic organization of Borna disease virus. Proc. Natl. Acad. Sci. USA 1994, 91, 4362–4366. [Google Scholar] [CrossRef] [PubMed]
- Cubitt, B.; de la Torre, J.C. Borna disease virus (BDV), a nonsegmented RNA virus, replicates in the nuclei of infected cells where infectious BDV ribonucleoproteins are present. J. Virol. 1994, 68, 1371–1381. [Google Scholar] [PubMed]
- Cubitt, B.; Oldstone, C.; de la Torre, J.C. Sequence and genome organization of Borna disease virus. J. Virol. 1994, 68, 1382–1396. [Google Scholar] [PubMed]
- Richt, J.A.; Rott, R. Borna disease virus: A mystery as an emerging zoonotic pathogen. Vet. J. 2001, 161, 24–40. [Google Scholar] [CrossRef] [PubMed]
- Herden, C.; Briese, T.; Lipkin, W.I.; Richt, J.A. Bornaviridae. In Fields Virology; Knipe, D.M., Howley, P.M., Eds.; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2013; pp. 1124–1150. [Google Scholar]
- Weissenböck, H.; Bagó, Z.; Kolodziejek, J.; Hager, B.; Palmetzhofer, G.; Dürrwald, R.; Nowotny, N. Infections of horses and shrews with Bornaviruses in Upper Austria: A novel endemic area of Borna disease. Emerg. Microbes Infect. 2017, 6, e52. [Google Scholar] [CrossRef] [PubMed]
- Vahlenkamp, T.W.; Konrath, A.; Weber, M.; Muller, H. Persistence of Borna disease virus in naturally infected sheep. J. Virol. 2002, 76, 9735–9743. [Google Scholar] [CrossRef]
- Bonnaud, E.M.; Szelechowski, M.; Bétourné, A.; Foret, C.; Thouard, A.; Gonzalez-Dunia, D.; Malnou, C.E. Borna disease virus phosphoprotein modulates epigenetic signaling in neurons to control viral replication. J. Virol. 2015, 89, 5996–6008. [Google Scholar] [CrossRef] [PubMed]
- Kistler, A.L.; Gancz, A.; Clubb, S.; Skewes-Cox, P.; Fischer, K.; Sorber, K.; Chiu, C.Y.; Lublin, A.; Mechani, S.; Farnoushi, Y.; et al. Recovery of divergent avian bornaviruses from cases of proventricular dilatation disease: Identification of a candidate etiologic agent. Virol. J. 2008, 5, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Honkavuori, K.S.; Shivaprasad, H.L.; Williams, B.L.; Quan, P.L.; Hornig, M.; Street, C.; Palacios, G.; Hutchison, S.K.; Franca, M.; Egholm, M.; et al. Novel borna virus in psittacine birds with proventricular dilatation disease. Emerg. Infect. Dis. 2008, 14, 1883–1886. [Google Scholar] [CrossRef]
- Hoffmann, B.; Tappe, D.; Hoper, D.; Herden, C.; Boldt, A.; Mawrin, C.; Niederstrasser, O.; Muller, T.; Jenckel, M.; van der Grinten, E.; et al. A Variegated Squirrel Bornavirus Associated with Fatal Human Encephalitis. N. Engl. J. Med. 2015, 373, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, J.H.; Durrwald, R.; Bao, Y.; Briese, T.; Carbone, K.; Clawson, A.N.; de Risi, J.L.; Garten, W.; Jahrling, P.B.; Kolodziejek, J.; et al. Taxonomic reorganization of the family Bornaviridae. Arch. Virol. 2015, 160, 621–632. [Google Scholar] [CrossRef] [PubMed]
- Tappe, D.; Schlottau, K.; Cadar, D.; Hoffmann, B.; Balke, L.; Bewig, B.; Hoffmann, D.; Eisermann, P.; Fickenscher, H.; Krumbholz, A.; et al. Occupation-Associated Fatal Limbic Encephalitis Caused by Variegated Squirrel Bornavirus 1, Germany, 2013. Emerg. Infect. Dis. 2018, 24, 978–987. [Google Scholar] [CrossRef] [PubMed]
- Schlottau, K.; Forth, L.; Angstwurm, K.; Höper, D.; Zecher, D.; Liesche, F.; Hoffmann, B.; Kegel, V.; Seehofer, D.; Platen, S.; et al. Fatal Encephalitic Borna Disease Virus 1 in Solid-Organ Transplant Recipients. N. Engl. J. Med. 2018, 379, 1377–1379. [Google Scholar] [CrossRef]
- Morales, J.A.; Herzog, S.; Kompter, C.; Frese, K.; Rott, R. Axonal transport of Borna disease virus along olfactory pathways in spontaneously and experimentally infected rats. Med. Microbiol. Immunol. 1988, 177, 51–68. [Google Scholar] [CrossRef] [PubMed]
- Winkler, W.G.; Fashinell, T.R.; Leffingwell, L.; Howard, P.; Conomy, P. Airborne rabies transmission in a laboratory worker. JAMA 1973, 226, 1219–1221. [Google Scholar] [CrossRef]
- van Riel, D.; Verdijk, R.; Kuiken, T. The olfactory nerve: A shortcut for influenza and other viral diseases into the central nervous system. J. Pathol. 2015, 235, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Mori, I. Transolfactory neuroinvasion by viruses threatens the human brain. Acta Virol. 2015, 59, 338–349. [Google Scholar] [CrossRef] [PubMed]
- Detje, C.N.; Lienenklaus, S.; Chhatbar, C.; Spanier, J.; Prajeeth, C.K.; Soldner, C.; Tovey, M.G.; Schlüter, D.; Weiss, S.; Stangel, M.; et al. Upon intranasal vesicular stomatitis virus infection, astrocytes in the olfactory bulb are important interferon Beta producers that protect from lethal encephalitis. J. Virol. 2015, 89, 2731–2738. [Google Scholar] [CrossRef]
- Shankar, V.; Kao, M.; Hamir, A.N.; Sheng, H.; Koprowski, H.; Dietzschold, B. Kinetics of virus spread and changes in levels of several cytokine mRNAs in the brain after intranasal infection of rats with Borna disease virus. J. Virol. 1992, 66, 992–998. [Google Scholar]
- Carbone, K.M.; Duchala, C.S.; Griffin, J.W.; Kincaid, A.L.; Narayan, O. Pathogenesis of Borna disease in rats: Evidence that intra-axonal spread is the major route for virus dissemination and the determinant for disease incubation. J. Virol. 1987, 61, 3431–3440. [Google Scholar]
- Lennartz, F.; Bayer, K.; Czerwonka, N.; Lu, Y.; Kehr, K.; Hirz, M.; Steinmetzer, T.; Garten, W.; Herden, C. Surface glycoprotein of Borna Disease virus mediates virus spread from cell to cell. Cell Microbiol. 2015. [Google Scholar] [CrossRef] [PubMed]
- Porombka, D.; Baumgartner, W.; Herden, C. A rapid method for gene expression analysis of Borna disease virus in neurons and astrocytes using laser microdissection and real-time RT-PCR. J. Virol. Methods 2008, 148, 58–65. [Google Scholar] [CrossRef]
- Bourg, M.; Herzog, S.; Encarnacao, J.A.; Nobach, D.; Lange-Herbst, H.; Eickmann, M.; Herden, C. Bicolored white-toothed shrews as reservoir for borna disease virus, Bavaria, Germany. Emerg. Infect. Dis. 2013, 19, 2064–2066. [Google Scholar] [CrossRef]
- Nobach, D.; Bourg, M.; Herzog, S.; Lange-Herbst, H.; Encarnacao, J.A.; Eickmann, M.; Herden, C. Shedding of Infectious Borna Disease Virus-1 in Living Bicolored White-Toothed Shrews. PLoS ONE 2015, 10, e0137018. [Google Scholar] [CrossRef]
- Schlottau, K.; Jenckel, M.; van den Brand, J.; Fast, C.; Herden, C.; Höper, D.; Homeier-Bachmann, T.; Thielebein, J.; Mensing, N.; Diender, B.; et al. Variegated Squirrel Bornavirus 1 in Squirrels, Germany and the Netherlands. Emerg. Infect. Dis. 2017, 23, 477–481. [Google Scholar] [CrossRef] [Green Version]
- Higginson, J.R.; Barnett, S.C. The culture of olfactory ensheathing cells (OECs)—A distinct glial cell type. Exp. Neurol. 2011, 229, 2–9. [Google Scholar] [CrossRef]
- Pourkhodadad, S.; Oryan, S.H.; Kaka, G.; Sadraie, S.H. Neuroprotective Effects of Combined Treatment with Minocycline and Olfactory Ensheathing Cells Transplantation against Inflammation and Oxidative Stress after Spinal Cord Injury. Cell J. 2019, 21, 220–228. [Google Scholar] [CrossRef]
- Harberts, E.; Yao, K.; Wohler, J.E.; Maric, D.; Ohayon, J.; Henkin, R.; Jacobson, S. Human herpesvirus-6 entry into the central nervous system through the olfactory pathway. Proc. Natl. Acad. Sci. USA 2011, 108, 13734–13739. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Li, D.; Raisman, G. Interaction of olfactory ensheathing cells with astrocytes may be the key to repair of tract injuries in the spinal cord: The ‘pathway hypothesis’. J. Neurocytol. 2005, 34, 343–351. [Google Scholar] [CrossRef]
- Salinas, S.; Schiavo, G.; Kremer, E.J. A hitchhiker’s guide to the nervous system: The complex journey of viruses and toxins. Nat. Rev. Microbiol. 2010, 8, 645–655. [Google Scholar] [CrossRef]
- Kalinke, U.; Bechmann, I.; Detje, C.N. Host strategies against virus entry via the olfactory system. Virulence 2011, 2, 367–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGavern, D.B.; Kang, S.S. Illuminating viral infections in the nervous system. Nat. Rev. Immunol. 2011, 11, 318–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heckmann, J.; Enderlein, D.; Piepenbring, A.K.; Herzog, S.; Heffels-Redmann, U.; Malberg, S.; Herden, C.; Lierz, M. Investigation of Different Infection Routes of Parrot Bornavirus in Cockatiels. Avian Dis. 2017, 61, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Narayan, O.; Herzog, S.; Frese, K.; Scheefers, H.; Rott, R. Behavioral disease in rats caused by immunopathological responses to persistent borna virus in the brain. Science 1983, 220, 1401–1403. [Google Scholar] [CrossRef]
- Werner-Keišs, N.; Garten, W.; Richt, J.A.; Porombka, D.; Algermissen, D.; Herzog, S.; Baumgartner, W.; Herden, C. Restricted expression of Borna disease virus glycoprotein in brains of experimentally infected Lewis rats. Neuropathol. Appl. Neurobiol. 2008, 34, 590–602. [Google Scholar] [CrossRef] [PubMed]
- Herden, C.; Herzog, S.; Richt, J.A.; Nesseler, A.; Christ, M.; Failing, K.; Frese, K. Distribution of Borna disease virus in the brain of rats infected with an obesity-inducing virus strain. Brain Pathol. 2000, 10, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Charlier, C.M.; Debaisieux, S.; Foret, C.; Thouard, A.; Schiavo, G.; Gonzalez-Dunia, D.; Malnou, C.E. Neuronal retrograde transport of Borna disease virus occurs in signalling endosomes. J. Gen. Virol. 2016, 97, 3215–3224. [Google Scholar] [CrossRef]
- Mori, I.; Nishiyama, Y.; Yokochi, T.; Kimura, Y. Olfactory transmission of neurotropic viruses. J. Neurovirol. 2005, 11, 129–137. [Google Scholar] [CrossRef]
- Leung, J.Y.; Chapman, J.A.; Harris, J.A.; Hale, D.; Chung, R.S.; West, A.K.; Chuah, M.I. Olfactory ensheathing cells are attracted to, and can endocytose, bacteria. Cell. Mol. Life Sci. 2008, 65, 2732–2739. [Google Scholar] [CrossRef] [Green Version]
- Harris, J.A.; West, A.K.; Chuah, M.I. Olfactory ensheathing cells: Nitric oxide production and innate immunity. Glia 2009, 57, 1848–1857. [Google Scholar] [CrossRef]
- Macedo-Ramos, H.; Ruiz-Mendoza, S.; Mariante, R.M.; Guimarães, E.V.; Quadros-de-Souza, L.C.; Paiva, M.M.; Ferreira, E.O.; Pinto, T.C.; Teixeira, L.M.; Allodi, S.; et al. Streptococcus pneumoniae resists intracellular killing by olfactory ensheathing cells but not by microglia. Sci. Rep. 2016, 6, 36813. [Google Scholar] [CrossRef] [Green Version]
- de la Torre, J.C. Molecular biology of Borna disease virus and persistence. Front. Biosci. 2002, 7, d569–d579. [Google Scholar] [CrossRef]
- Tomonaga, K.; Kobayashi, T.; Ikuta, K. Molecular and cellular biology of Borna disease virus infection. Microbes Infect. 2002, 4, 491–500. [Google Scholar] [CrossRef]
- Hirai, Y.; Hirano, Y.; Matsuda, A.; Hiraoka, Y.; Honda, T.; Tomonaga, K. Borna Disease Virus Assembles Porous Cage-like Viral Factories in the Nucleus. J. Biol. Chem. 2016, 291, 25789–25798. [Google Scholar] [CrossRef]
- Liang, F. Olfactory receptor neuronal dendrites become mostly intra-sustentacularly enwrapped upon maturity. J. Anat. 2018, 232, 674–685. [Google Scholar] [CrossRef]
- Geib, T.; Sauder, C.; Venturelli, S.; Hassler, C.; Staeheli, P.; Schwemmle, M. Selective virus resistance conferred by expression of Borna disease virus nucleocapsid components. J. Virol. 2003, 77, 4283–4290. [Google Scholar] [CrossRef] [PubMed]
- Fujino, K.; Horie, M.; Honda, T.; Merriman, D.K.; Tomonaga, K. Inhibition of Borna disease virus replication by an endogenous bornavirus-like element in the ground squirrel genome. Proc. Natl. Acad. Sci. USA 2014, 111, 13175–13180. [Google Scholar] [CrossRef] [Green Version]
- Fujino, K.; Horie, M.; Honda, T.; Nakamura, S.; Matsumoto, Y.; Francischetti, I.M.; Tomonaga, K. Evolutionarily conserved interaction between the phosphoproteins and X proteins of bornaviruses from different vertebrate species. PLoS ONE 2012, 7, e51161. [Google Scholar] [CrossRef]
- Horie, M.; Honda, T.; Suzuki, Y.; Kobayashi, Y.; Daito, T.; Oshida, T.; Ikuta, K.; Jern, P.; Gojobori, T.; Coffin, J.M.; et al. Endogenous non-retroviral RNA virus elements in mammalian genomes. Nature 2010, 463, 84–87. [Google Scholar] [CrossRef] [Green Version]
- Horie, M.; Kobayashi, Y.; Suzuki, Y.; Tomonaga, K. Comprehensive analysis of endogenous bornavirus-like elements in eukaryote genomes. Philos. Trans. R Soc. Lond. B Biol. Sci. 2013, 368. [Google Scholar] [CrossRef]
- Belyi, V.A.; Levine, A.J.; Skalka, A.M. Unexpected inheritance: Multiple integrations of ancient bornavirus and ebolavirus/marburgvirus sequences in vertebrate genomes. PLoS Pathog. 2010, 6, e1001030. [Google Scholar] [CrossRef]
- Honda, T.; Tomonaga, K. Endogenous non-retroviral RNA virus elements evidence a novel type of antiviral immunity. Mob. Genet. Elem. 2016, 6, e1165785. [Google Scholar] [CrossRef] [Green Version]
- Lischka, F.W.; Efthymiou, A.; Zhou, Q.; Nieves, M.D.; McCormack, N.M.; Wilkerson, M.D.; Sukumar, G.; Dalgard, C.L.; Doughty, M.L. Neonatal mouse cortical but not isogenic human astrocyte feeder layers enhance the functional maturation of induced pluripotent stem cell-derived neurons in culture. Glia 2018, 66, 725–748. [Google Scholar] [CrossRef]
- Schutte, R.J.; Xie, Y.; Ng, N.N.; Figueroa, P.; Pham, A.T.; O’Dowd, D.K. Astrocyte-enriched feeder layers from cryopreserved cells support differentiation of spontaneously active networks of human iPSC-derived neurons. J. Neurosci. Methods 2018, 294, 91–101. [Google Scholar] [CrossRef]
- Richt, J.A.; Stitz, L. Borna disease virus-infected astrocytes function in vitro as antigen-presenting and target cells for virus-specific CD4-bearing lymphocytes. Arch. Virol. 1992, 124, 95–109. [Google Scholar] [CrossRef]
- Carbone, K.M.; Rubin, S.A.; Sierra-Honigmann, A.M.; Lederman, H.M. Characterization of a glial cell line persistently infected with borna disease virus (BDV): Influence of neurotrophic factors on BDV protein and RNA expression. J. Virol. 1993, 67, 1453–1460. [Google Scholar]
- Grill, R.J.; Pixley, S.K. In vitro generation of adult rat olfactory sensory neurons and regulation of maturation by coculture with CNS tissues. J. Neurosci. 1997, 17, 3120–3127. [Google Scholar] [CrossRef]
- Brauchi, S.; Cea, C.; Farias, J.G.; Bacigalupo, J.; Reyes, J.G. Apoptosis induced by prolonged exposure to odorants in cultured cells from rat olfactory epithelium. Brain Res. 2006, 1103, 114–122. [Google Scholar] [CrossRef]
- Vargas, G.; Lucero, M.T. A method for maintaining odor-responsive adult rat olfactory receptor neurons in short-term culture. Chem. Senses 1999, 24, 211–216. [Google Scholar] [CrossRef]
- Vargas, G.; Lucero, M.T. Dopamine modulates inwardly rectifying hyperpolarization-activated current (Ih) in cultured rat olfactory receptor neurons. J. Neurophysiol. 1999, 81, 149–158. [Google Scholar] [CrossRef]
- Pixley, S.K. CNS glial cells support in vitro survival, division, and differentiation of dissociated olfactory neuronal progenitor cells. Neuron 1992, 8, 1191–1204. [Google Scholar] [CrossRef]
- Chen, H.; Dadsetan, S.; Fomina, A.F.; Gong, Q. Expressing exogenous functional odorant receptors in cultured olfactory sensory neurons. Neural Dev. 2008, 3, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herzog, S.; Rott, R. Replication of Borna disease virus in cell cultures. Med. Microbiol. Immunol. 1980, 168, 153–158. [Google Scholar] [CrossRef]
- Ahlemeyer, B.; Kehr, K.; Richter, E.; Hirz, M.; Baumgart-Vogt, E.; Herden, C. Phenotype, differentiation, and function differ in rat and mouse neocortical astrocytes cultured under the same conditions. J. Neurosci. Methods 2013, 212, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Porombka, D.; Herzog, S.; Baumgartner, W.; Herden, C. Preservation of RNA and destruction of infectivity in microdissected brain tissues of Lewis rats infected with the Borna disease virus. J. Virol. Methods 2006, 135, 247–253. [Google Scholar] [CrossRef]
- Porombka, D.; Baumgartner, W.; Eickmann, M.; Herden, C. Implications for a regulated replication of Borna disease virus in brains of experimentally infected Lewis rats. Virus Genes 2008, 36, 415–420. [Google Scholar] [CrossRef]
- Weissenböck, H.; Nowotny, N.; Caplazi, P.; Kolodziejek, J.; Ehrensperger, F. Borna disease in a dog with lethal meningoencephalitis. J. Clin. Microbiol. 1998, 36, 2127–2130. [Google Scholar] [PubMed]
- Okamoto, M.; Kagawa, Y.; Kamitani, W.; Hagiwara, K.; Kirisawa, R.; Iwai, H.; Ikuta, K.; Taniyama, H. Borna disease in a dog in Japan. J. Comp. Pathol. 2002, 126, 312–317. [Google Scholar] [CrossRef]
- Bajramovic, J.J.; Munter, S.; Syan, S.; Nehrbass, U.; Brahic, M.; Gonzalez-Dunia, D. Borna Disease Virus Glycoprotein Is Required for Viral Dissemination in Neurons. J. Virol. 2003, 77, 12222–12231. [Google Scholar] [CrossRef] [Green Version]
- Hirschberger, J. Herstellung und Charakterisierung Monoklonaler Antikörper Gegen T-Lymphozyten des Huhnes; Veterinary Medicine Dissertation: Giessen, Germany, 1987. [Google Scholar]
- Gaedke, K.; Zurbriggen, A.; Baumgartner, W. In vivo and in vitro detection of canine distemper virus nucleoprotein gene with digoxigenin-labelled RNA, double-stranded DNA probes and oligonucleotides by in situ hybridization. Zentralbl. Veterinarmed. B 1997, 44, 329–340. [Google Scholar] [CrossRef]
- Zurbriggen, A.; Muller, C.; Vandevelde, M. In situ hybridization of virulent canine distemper virus in brain tissue, using digoxigenin-labeled probes. Am. J. Vet. Res. 1993, 54, 1457–1461. [Google Scholar] [PubMed]
- Ahlemeyer, B.; Baumgart-Vogt, E. Optimized protocols for the simultaneous preparation of primary neuronal cultures of the neocortex, hippocampus and cerebellum from individual newborn (P0.5) C57Bl/6J mice. J. Neurosci. Methods 2005, 149, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Roloff, F.; Ziege, S.; Baumgärtner, W.; Wewetzer, K.; Bicker, G. Schwann cell-free adult canine olfactory ensheathing cell preparations from olfactory bulb and mucosa display differential migratory and neurite growth-promoting properties in vitro. BMC Neurosci. 2013, 14, 141. [Google Scholar] [CrossRef] [PubMed]
- Ziege, S.; Baumgartner, W.; Wewetzer, K. Toward defining the regenerative potential of olfactory mucosa: Establishment of Schwann cell-free adult canine olfactory ensheathing cell preparations suitable for transplantation. Cell Transpl. 2013, 22, 355–367. [Google Scholar] [CrossRef]
- Sonigra, R.J.; Kandiah, S.S.; Wigley, C.B. Spontaneous immortalisation of ensheathing cells from adult rat olfactory nerve. Glia 1996, 16, 247–256. [Google Scholar] [CrossRef]
- Chomczynski, P.; Sacchi, N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal. Biochem. 1987, 162, 156–159. [Google Scholar] [CrossRef]
- Schaudien, D.; Baumgartner, W.; Herden, C. High preservation of DNA standards diluted in 50% glycerol. Diagn. Mol. Pathol. 2007, 16, 153–157. [Google Scholar] [CrossRef]





© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kupke, A.; Becker, S.; Wewetzer, K.; Ahlemeyer, B.; Eickmann, M.; Herden, C. Intranasal Borna Disease Virus (BoDV-1) Infection: Insights into Initial Steps and Potential Contagiosity. Int. J. Mol. Sci. 2019, 20, 1318. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms20061318
Kupke A, Becker S, Wewetzer K, Ahlemeyer B, Eickmann M, Herden C. Intranasal Borna Disease Virus (BoDV-1) Infection: Insights into Initial Steps and Potential Contagiosity. International Journal of Molecular Sciences. 2019; 20(6):1318. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms20061318
Chicago/Turabian StyleKupke, Alexandra, Sabrina Becker, Konstantin Wewetzer, Barbara Ahlemeyer, Markus Eickmann, and Christiane Herden. 2019. "Intranasal Borna Disease Virus (BoDV-1) Infection: Insights into Initial Steps and Potential Contagiosity" International Journal of Molecular Sciences 20, no. 6: 1318. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms20061318




