Monoamine Oxidase B Expression Correlates with a Poor Prognosis in Colorectal Cancer Patients and Is Significantly Associated with Epithelial-to-Mesenchymal Transition-Related Gene Signatures
Abstract
:1. Introduction
2. Results
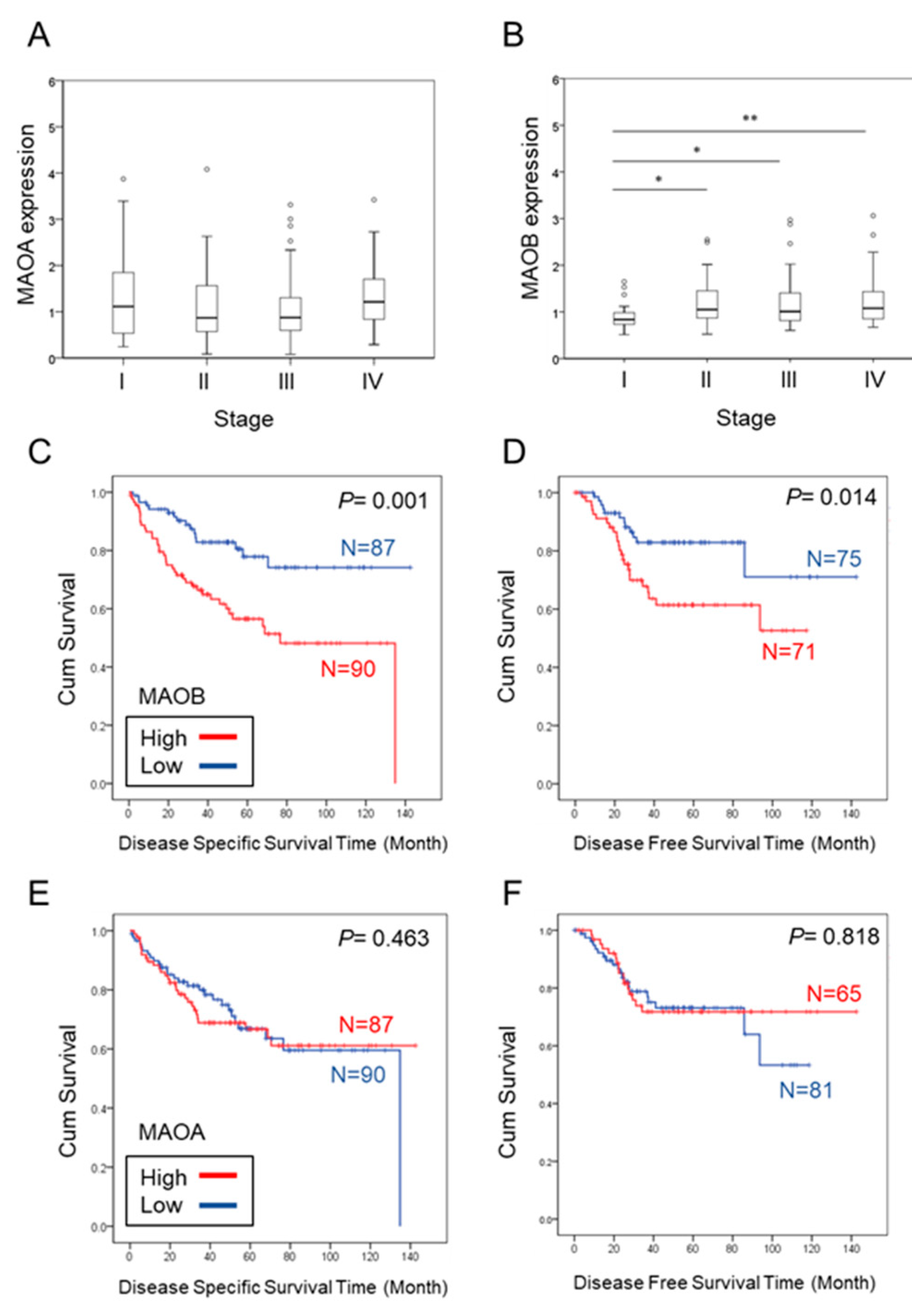
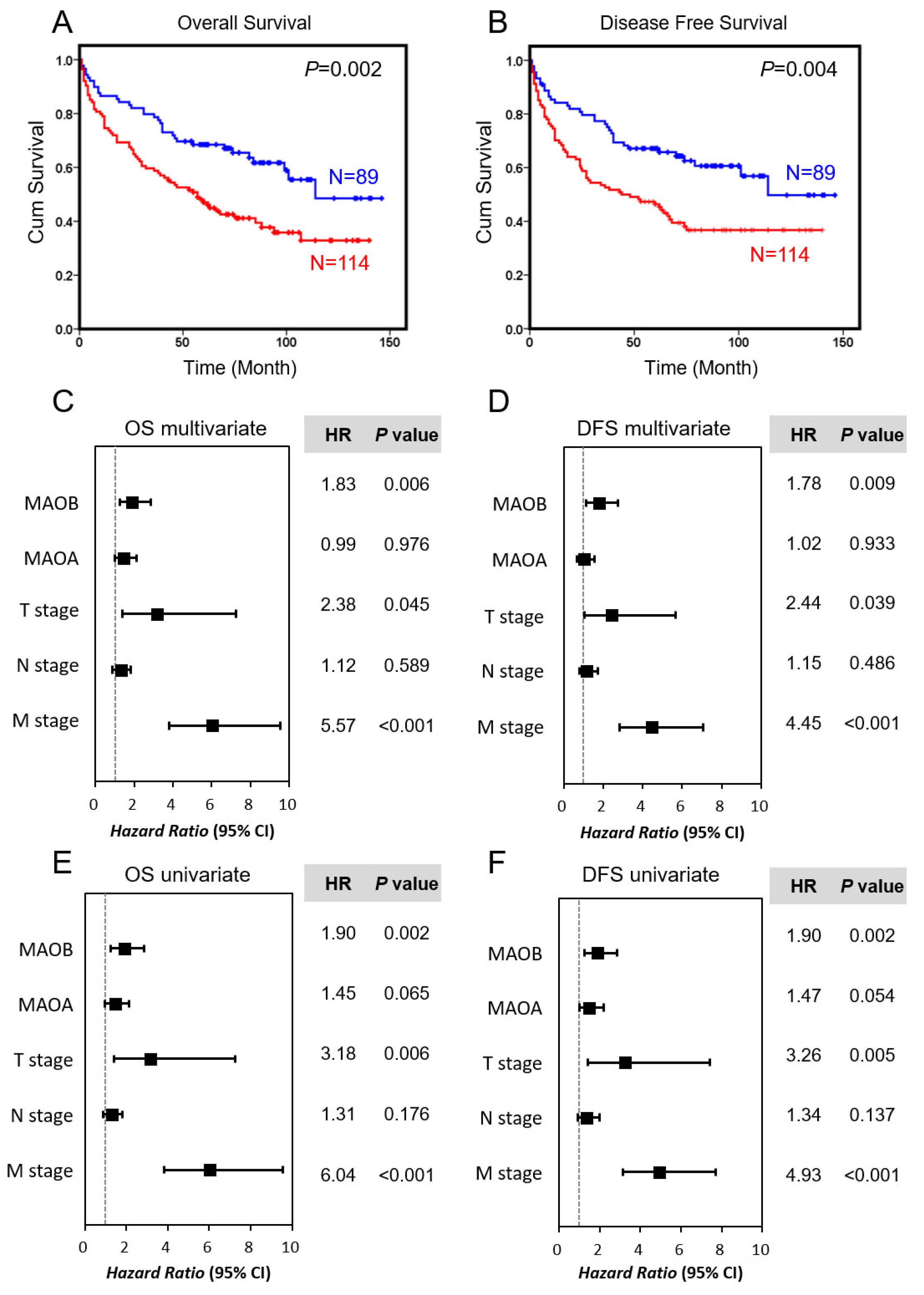
2.1. Higher Expression of MAOB, but Not MAOA, Correlated with a Poorer Prognosis in CRC Patients
2.2. Immunohistochemical (IHC) Analysis of MAOA and MAOB in CRC Tissues
2.3. Correlations between Expressions of MAOs and Clinicopathological Parameters of CRC Patients
2.4. Prognostic Value of MAO Expressions in a Taiwanese Colorectal Cancer Cohort
2.5. Correlation between MAOB Expression Levels and EMT-Related Markers
3. Discussion
4. Materials and Methods
4.1. Patients and Case Selection
4.2. Tissue Microarray (TMA) Construction and IHC Staining
4.3. In Silico Analysis
4.4. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CRC | Colorectal cancer |
| DFS | Disease-free survival |
| DSS | Disease-specific survival |
| EMT | Epithelial-to-mesenchymal transition |
| IHC | Immunohistochemical |
| MAO | Monoamine oxidase |
| OS | Overall survival |
| TCGA | The Cancer Genome Atlas |
| TMA | Tissue microarray |
References
- Siegel, R.; Naishadham, D.; Jemal, A. Cancer statistics, 2013. CA Cancer J. Clin. 2013, 63, 11–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, J.J.; Lau, J.Y.; Goh, K.L.; Leung, W.K. Increasing incidence of colorectal cancer in Asia: Implications for screening. Lancet Oncol. 2005, 6, 871–876. [Google Scholar] [CrossRef]
- Aghili, M.; Izadi, S.; Madani, H.; Mortazavi, H. Clinical and pathological evaluation of patients with early and late recurrence of colorectal cancer. Asia Pac. J. Clin. Oncol. 2010, 6, 35–41. [Google Scholar] [CrossRef]
- Jiang, T.; Tang, H.M.; Wu, Z.H.; Chen, J.; Lu, S.; Zhou, C.Z.; Yan, D.W.; Peng, Z.H. Cullin 4B is a novel prognostic marker that correlates with colon cancer progression and pathogenesis. Med. Oncol. 2013, 30, 534. [Google Scholar] [CrossRef] [PubMed]
- Yan, D.W.; Li, D.W.; Yang, Y.X.; Xia, J.; Wang, X.L.; Zhou, C.Z.; Fan, J.W.; Wen, Y.G.; Sun, H.C.; Wang, Q.; et al. Ubiquitin D is correlated with colon cancer progression and predicts recurrence for stage II-III disease after curative surgery. Br. J. Cancer 2010, 103, 961–969. [Google Scholar] [CrossRef] [Green Version]
- Alves Martins, B.A.; de Bulhoes, G.F.; Cavalcanti, I.N.; Martins, M.M.; de Oliveira, P.G.; Martins, A.M.A. Biomarkers in Colorectal Cancer: The Role of Translational Proteomics Research. Front. Oncol. 2019, 9, 1284. [Google Scholar] [CrossRef]
- Hauptman, N.; Glavac, D. Colorectal Cancer Blood-Based Biomarkers. Gastroenterol. Res. Pract. 2017, 2017, 2195361. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez-Pons, M.; Cruz-Correa, M. Colorectal Cancer Biomarkers: Where Are We Now? Biomed. Res. Int. 2015, 2015, 149014. [Google Scholar] [CrossRef] [Green Version]
- Boland, C.R.; Thibodeau, S.N.; Hamilton, S.R.; Sidransky, D.; Eshleman, J.R.; Burt, R.W.; Meltzer, S.J.; Rodriguez-Bigas, M.A.; Fodde, R.; Ranzani, G.N.; et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: Development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998, 58, 5248–5257. [Google Scholar]
- Sinicrope, F.A.; Sargent, D.J. Clinical implications of microsatellite instability in sporadic colon cancers. Curr. Opin. Oncol. 2009, 21, 369–373. [Google Scholar] [CrossRef]
- Huang, L.; Frampton, G.; Rao, A.; Zhang, K.S.; Chen, W.; Lai, J.M.; Yin, X.Y.; Walker, K.; Culbreath, B.; Leyva-Illades, D.; et al. Monoamine oxidase A expression is suppressed in human cholangiocarcinoma via coordinated epigenetic and IL-6-driven events. Lab. Investig. 2012, 92, 1451–1460. [Google Scholar] [CrossRef] [PubMed]
- Rybaczyk, L.A.; Bashaw, M.J.; Pathak, D.R.; Huang, K. An indicator of cancer: Downregulation of monoamine oxidase-A in multiple organs and species. BMC Genom. 2008, 9, 134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mikula, M.; Rubel, T.; Karczmarski, J.; Goryca, K.; Dadlez, M.; Ostrowski, J. Integrating proteomic and transcriptomic high-throughput surveys for search of new biomarkers of colon tumors. Funct. Integr. Genom. 2010, 11, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.B.; Shao, C.; Li, X.; Li, Q.; Hu, P.; Shi, C.; Li, Y.; Chen, Y.T.; Yin, F.; Liao, C.P.; et al. Monoamine oxidase A mediates prostate tumorigenesis and cancer metastasis. J. Clin. Investig. 2014, 124, 2891–2908. [Google Scholar] [CrossRef] [Green Version]
- Wu, J.B.; Yin, L.; Shi, C.; Li, Q.; Duan, P.; Huang, J.M.; Liu, C.; Wang, F.; Lewis, M.; Wang, Y.; et al. MAOA-Dependent Activation of Shh-IL6-RANKL Signaling Network Promotes Prostate Cancer Metastasis by Engaging Tumor-Stromal Cell Interactions. Cancer Cell 2017, 31, 368–382. [Google Scholar] [CrossRef] [Green Version]
- Sharpe, M.A.; Baskin, D.S. Monoamine oxidase B levels are highly expressed in human gliomas and are correlated with the expression of HiF-1alpha and with transcription factors Sp1 and Sp3. Oncotarget 2016, 7, 3379–3393. [Google Scholar] [CrossRef] [Green Version]
- Chen, P.H.; Huang, B.; Shieh, T.Y.; Wang, Y.H.; Chen, Y.K.; Wu, J.H.; Huang, J.H.; Chen, C.C.; Lee, K.W. The influence of monoamine oxidase variants on the risk of betel quid-associated oral and pharyngeal cancer. Sci. World J. 2014, 2014, 183548. [Google Scholar] [CrossRef]
- Gentles, A.J.; Newman, A.M.; Liu, C.L.; Bratman, S.V.; Feng, W.; Kim, D.; Nair, V.S.; Xu, Y.; Khuong, A.; Hoang, C.D.; et al. The prognostic landscape of genes and infiltrating immune cells across human cancers. Nat. Med. 2015, 21, 938–945. [Google Scholar] [CrossRef]
- Aguirre-Gamboa, R.; Gomez-Rueda, H.; Martinez-Ledesma, E.; Martinez-Torteya, A.; Chacolla-Huaringa, R.; Rodriguez-Barrientos, A.; Tamez-Pena, J.G.; Trevino, V. SurvExpress: An online biomarker validation tool and database for cancer gene expression data using survival analysis. PLoS ONE 2013, 8, e74250. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Zhou, B.P. Epithelial-mesenchymal Transition—A Hallmark of Breast Cancer Metastasis. Cancer Hallm. 2013, 1, 38–49. [Google Scholar] [CrossRef] [Green Version]
- Mittal, V. Epithelial Mesenchymal Transition in Aggressive Lung Cancers. Adv. Exp. Med. Biol. 2016, 890, 37–56. [Google Scholar] [PubMed]
- Loboda, A.; Nebozhyn, M.V.; Watters, J.W.; Buser, C.A.; Shaw, P.M.; Huang, P.S.; Van’t Veer, L.; Tollenaar, R.A.; Jackson, D.B.; Agrawal, D.; et al. EMT is the dominant program in human colon cancer. BMC Med. Genom. 2011, 4, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Califf, R.M. Biomarker definitions and their applications. Exp. Biol. Med. 2018, 243, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Chauvin, A.; Boisvert, F.M. Clinical Proteomics in Colorectal Cancer, a Promising Tool for Improving Personalised Medicine. Proteomes 2018, 6, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oldenhuis, C.N.; Oosting, S.F.; Gietema, J.A.; de Vries, E.G. Prognostic versus predictive value of biomarkers in oncology. Eur. J. Cancer 2008, 44, 946–953. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, M.S. Biotransformation of xenobiotics by amine oxidases. Fundam. Clin. Pharmacol. 2001, 15, 75–84. [Google Scholar] [CrossRef]
- Edmondson, D.E. Hydrogen peroxide produced by mitochondrial monoamine oxidase catalysis: Biological implications. Curr. Pharm. Des. 2014, 20, 155–160. [Google Scholar] [CrossRef]
- Reuter, S.; Gupta, S.C.; Chaturvedi, M.M.; Aggarwal, B.B. Oxidative stress, inflammation, and cancer: How are they linked? Free Radic. Biol. Med. 2010, 49, 1603–1616. [Google Scholar] [CrossRef] [Green Version]
- Siddiqui, A.; Mallajosyula, J.K.; Rane, A.; Andersen, J.K. Ability to delay neuropathological events associated with astrocytic MAO-B increase in a Parkinsonian mouse model: Implications for early intervention on disease progression. Neurobiol. Dis. 2010, 40, 444–448. [Google Scholar] [CrossRef] [Green Version]
- Dabrowska, M.; Skoneczny, M.; Rode, W. Functional gene expression profile underlying methotrexate-induced senescence in human colon cancer cells. Tumour Biol. 2011, 32, 965–976. [Google Scholar] [CrossRef] [Green Version]
- Dienstmann, R.; Mason, M.J.; Sinicrope, F.A.; Phipps, A.I.; Tejpar, S.; Nesbakken, A.; Danielsen, S.A.; Sveen, A.; Buchanan, D.D.; Clendenning, M.; et al. Prediction of overall survival in stage II and III colon cancer beyond TNM system: a retrospective, pooled biomarker study. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2017, 28, 1023–1031. [Google Scholar] [CrossRef] [PubMed]
- Moccia, F.; Tolone, S.; Allaria, A.; Napolitano, V.; Rosa, D.; Ilaria, F.; Ottavia, M.; Cesaro, E.; Docimo, L.; Fei, L. Lymph Node Ratio Versus TNM System As Prognostic Factor in Colorectal Cancer Staging. a Single Center Experience. Open Med. 2019, 14, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.J.; Deane, N.G.; Wu, F.; Merchant, N.B.; Zhang, B.; Jiang, A.; Lu, P.; Johnson, J.C.; Schmidt, C.; Bailey, C.E.; et al. Experimentally derived metastasis gene expression profile predicts recurrence and death in patients with colon cancer. Gastroenterology 2010, 138, 958–968. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Clinicopathological Feature | n | MAOA Expression, n (%) | p | MAOB Expression, n (%) | p-Value | ||
|---|---|---|---|---|---|---|---|
| 203 | Low | High | Low | High | |||
| 126 (62.1) | 77 (37.9) | 89 (43.8) | 114 (56.2) | ||||
| Age (years) | |||||||
| <65 | 64 | 44 (68.8) | 20 (31.2) | 0.2401 | 34 (53.1) | 30 (46.9) | 0.0979 |
| ≥65 | 139 | 82 (59.0) | 57 (41.0) | 55 (40.0) | 84 (60.0) | ||
| Gender | |||||||
| Male | 117 | 66 (56.4) | 51 (43.6) | 0.0732 | 45 (38.5) | 72 (61.5) | 0.0973 |
| Female | 86 | 60 (69.8) | 26 (30.2) | 44 (51.2) | 42 (48.8) | ||
| Tumor location | |||||||
| Right colon | 35 | 20 (57.1) | 15 (42.9) | 0.7988 | 10 (28.6) | 25 (71.4) | 0.2519 |
| Transverse colon | 25 | 17 (68.0) | 8 (32.0) | 12 (48.0) | 13 (52.0) | ||
| Descending colon | 16 | 9 (56.3) | 7 (43.7) | 7 (43.8) | 9 (56.2) | ||
| Rectosigmoid colon | 127 | 80 (63.0) | 47 (37.0) | 60 (47.2) | 67 (52.8) | ||
| T stage | |||||||
| T1+T2 | 27 | 17 (63.0) | 10 (37.0) | 0.9203 | 14 (51.9) | 13 (48.1) | 0.4884 |
| T3+T4 | 176 | 109 (61.9) | 67 (38.1) | 75 (42.6) | 101 (57.4) | ||
| N stage | |||||||
| N0 | 97 | 64 (66.0) | 33 (34.0) | 0.0633 | 48 (49.5) | 49 (50.5) | 0.1594 |
| N1+N2 | 106 | 62 (58.5) | 44 (51.5) | 41 (38.7) | 65 (61.3) | ||
| M stage | |||||||
| M0 | 172 | 112 (65.1) | 60 (34.9) | 0.0564 | 78 (45.3) | 94 (54.7) | 0.4096 |
| M1 | 31 | 14 (45.2) | 17 (54.8) | 11 (35.5) | 20 (64.5) | ||
| TNM stage | |||||||
| Stage I | 21 | 15 (71.4) | 6 (28.6) | 0.1089 | 12 (57.1) | 9 (42.9) | 0.1208 |
| Stage II | 65 | 45 (69.2) | 20 (30.8) | 34 (52.3) | 31 (47.7) | ||
| Stage III | 86 | 52 (60.5) | 34 (39.5) | 32 (37.2) | 54 (62.8) | ||
| Stage IV | 31 | 14 (45.2) | 17 (54.8) | 11 (35.5) | 20 (64.5) | ||
| Grade | |||||||
| Grade 1 | 4 | 3 (75.0) | 1 (25.0) | 0.6883 | 3 (75.0) | 1 (25.0) | 0.3743 |
| Grade 2 | 181 | 112 (61.9) | 69 (38.1) | 76 (42.0) | 105 (58.0) | ||
| Grade 3 | 8 | 6 (75.0) | 2 (25.0) | 5 (62.5) | 3 (37.5) | ||
| NA | 10 | 5 (50.0) | 5 (50.0) | 5 (50.0) | 5 (50.0) | ||
| Adjuvant chemotherapy | |||||||
| No | 89 | 58 (65.2) | 31 (34.8) | 0.4213 | 40 (44.9) | 49 (55.1) | 0.7799 |
| Yes | 114 | 68 (59.6) | 46 (40.4) | 49 (43.0) | 65 (57.0) | ||
| Vascular invasion | |||||||
| No | 93 | 56 (60.2) | 37 (39.8) | 0.7184 | 42 (45.2) | 51 (54.8) | 0.8415 |
| Yes | 110 | 70 (63.6) | 40 (36.4) | 47 (42.7) | 63 (57.3) | ||
| Perineural invasion | |||||||
| No | 157 | 94 (60.0) | 63 (40.0) | 0.3078 | 70 (44.6) | 87 (55.4) | 0.8231 |
| Yes | 46 | 32 (69.6) | 14 (30.4) | 19 (41.3) | 27 (58.7) | ||
| Tumor histology | |||||||
| Non-mucinous | 189 | 118 (62.4) | 71 (37.6) | 0.9203 | 83 (43.9) | 106 (56.1) | 0.8415 |
| Mucinous | 14 | 8 (57.1) | 6 (32.9) | 6 (42.9) | 8 (57.1) | ||
| Recurrence | |||||||
| No | 95 | 63 (66.3) | 32 (33.7) | 0.3055 | 51 (53.7) | 44 (47.3) | 0.0121 |
| Yes | 108 | 63 (58.3) | 45 (41.7) | 38 (35.2) | 70 (64.8) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.-C.; Chien, M.-H.; Lai, T.-C.; Su, C.-Y.; Jan, Y.-H.; Hsiao, M.; Chen, C.-L. Monoamine Oxidase B Expression Correlates with a Poor Prognosis in Colorectal Cancer Patients and Is Significantly Associated with Epithelial-to-Mesenchymal Transition-Related Gene Signatures. Int. J. Mol. Sci. 2020, 21, 2813. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21082813
Yang Y-C, Chien M-H, Lai T-C, Su C-Y, Jan Y-H, Hsiao M, Chen C-L. Monoamine Oxidase B Expression Correlates with a Poor Prognosis in Colorectal Cancer Patients and Is Significantly Associated with Epithelial-to-Mesenchymal Transition-Related Gene Signatures. International Journal of Molecular Sciences. 2020; 21(8):2813. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21082813
Chicago/Turabian StyleYang, Yi-Chieh, Ming-Hsien Chien, Tsung-Ching Lai, Chia-Yi Su, Yi-Hua Jan, Michael Hsiao, and Chi-Long Chen. 2020. "Monoamine Oxidase B Expression Correlates with a Poor Prognosis in Colorectal Cancer Patients and Is Significantly Associated with Epithelial-to-Mesenchymal Transition-Related Gene Signatures" International Journal of Molecular Sciences 21, no. 8: 2813. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms21082813







