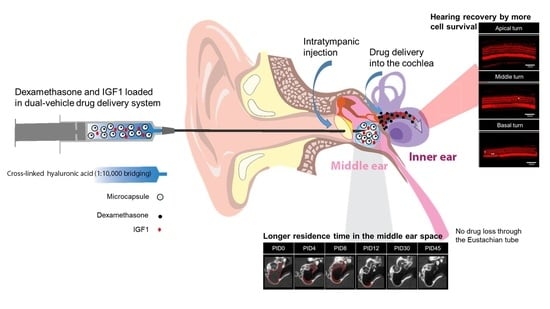
Effect and Biocompatibility of a Cross-Linked Hyaluronic Acid and Polylactide-co-glycolide Microcapsule Vehicle in Intratympanic Drug Delivery for Treating Acute Acoustic Trauma
Abstract
:1. Introduction
2. Results
2.1. Residence Time of the Drug/Vehicle as Evaluated by Micro CT
2.2. Visible Light Endoscopy
2.3. Real-Time Fluorescence Endoscopy with Indocyanine Green (ICG)
2.4. Histologic Findings of the TM and Middle Ear Mucosa
2.5. Audiometric Assessment Using the Auditory Brainstem Response (ABR)
2.6. Hair Cell Count
3. Discussion
4. Materials and Methods
4.1. Experimental Design and Animal Groups
4.2. Animal Model of Acute Acoustic Trauma
4.3. Preparation of Drug/Vehicle Formulations
4.4. IT Injection Procedure
4.5. Micro CT
4.6. Visible Light Endoscopy
4.7. Real-Time Fluorescence Endoscopy with ICG
4.8. Hearing Threshold Assessment Based on ABR
4.9. Inner Ear Hair Cell Count
4.10. Middle Ear Histology of the Drug/Vehicle after Contacting the Mucosa
4.11. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Animal Care and Use Committee Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilson, W.R.; Byl, F.M.; Laird, N. The Efficacy of Steroids in the Treatment of Idiopathic Sudden Hearing Loss: A Double-blind Clinical Study. Arch. Otolaryngol. Head Neck Surg. 1980, 106, 772–776. [Google Scholar] [CrossRef]
- Stachler, R.J.; Chandrasekhar, S.S.; Archer, S.M.; Rosenfeld, R.M.; Schwartz, S.R.; Barrs, D.M.; Brown, S.R.; Fife, T.D.; Ford, P.; Ganiats, T.G.; et al. Clinical practice guideline: Sudden hearing loss. Otolaryngol. Head Neck Surg. 2012, 146 (Suppl. 3), S1–S35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattox, D.E.; Simmons, F.B. Natural History of Sudden Sensorineural Hearing Loss. Ann. Otol. Rhinol. Laryngol. 1977, 86, 463–480. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Jolly, C.; Braun, S.; Janssen, T.; Scherer, E.; Steinhoff, J.; Ebenhoch, H.; Lohner, A.; Stark, T.; Kiefer, J. Effects of a dexamethasone-releasing implant on cochleae: A functional, morphological and pharmacokinetic study. Hear. Res. 2015, 327, 89–101. [Google Scholar] [CrossRef]
- Min, K.H.; Rhee, C.-K.; Jung, J.Y.; Suh, M.-W. Characteristics of Adverse Effects When Using High Dose Short Term Steroid Regimen. Korean J. Audiol. 2012, 16, 65–70. [Google Scholar] [CrossRef]
- Rivera, T.; Sanz, L.; Camarero, G.; Varela-Nieto, I. Drug delivery to the inner ear: Strategies and their therapeutic implications for sensorineural hearing loss. Curr. Drug Deliv. 2012, 9, 231–242. [Google Scholar] [CrossRef] [Green Version]
- Parnes, L.S.; Sun, A.-H.; Freeman, D.J. Corticosteroid Pharmacokinetics in the Inner Ear Fluids: An Animal Study Followed by Clinical Application. Laryngoscope 1999, 109, 1–17. [Google Scholar] [CrossRef]
- Chandrasekhar, S.S.; Rubinstein, R.Y.; Kwartler, J.A.; Gatz, M.; Connelly, P.E.; Huang, E.; Baredes, S. Dexamethasone pharmacokinetics in the inner ear: Comparison of route of administration and use of facilitating agents. Otolaryngol. Head Neck Surg. 2000, 122, 521–528. [Google Scholar] [PubMed] [Green Version]
- Bachmann, G.; Su, J.; Zumegen, C.; Wittekindt, C.; Michel, O. Permeability of the round window membrane for prednisolone-21-hydrogen succinate. Prednisolone content of the perilymph after local administration vs. systemic injection. HNO 2001, 49, 538–542. [Google Scholar] [CrossRef]
- Chandrasekhar, S.S. Intratympanic Dexamethasone for Sudden Sensorineural Hearing Loss: Clinical and Laboratory Evaluation. Otol. Neurotol. 2001, 22, 18–23. [Google Scholar] [CrossRef]
- Lee, J.H.; Hwang, Y.; Li, H.; Kim, H.; Suh, M.; Han, D.; Oh, S. In-depth proteome of perilymph in guinea pig model. Proteoms 2021, 21, e2000138. [Google Scholar] [CrossRef] [PubMed]
- Seggas, I.; Koltsidopoulos, P.; Bibas, A.; Tzonou, A.; Sismanis, A. Intratympanic steroid therapy for sudden hearing loss: A review of the literature. Otol. Neurotol. 2011, 32, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekhar, S.S.; Do, B.S.T.; Schwartz, S.R.; Bontempo, L.J.; Faucett, E.A.; Finestone, S.A.; Hollingsworth, D.B.; Kelley, D.M.; Kmucha, S.T.; Moonis, G.; et al. Clinical Practice Guideline: Sudden Hearing Loss (Update) Executive Summary. Otolaryngol. Neck Surg. 2019, 161, 195–210. [Google Scholar] [CrossRef] [Green Version]
- Salmon, W.D., Jr.; Daughaday, W.H. A hormonally controlled serum factor which stimulates sulfate incorporation by cartilage in vitro. J. Lab. Clin. Med. 1957, 49, 825–836. [Google Scholar]
- Rinderknecht, E.; Humbel, R.E. Polypeptides with nonsuppressible insulin-like and cell-growth promoting activities in human serum: Isolation, chemical characterization, and some biological properties of forms I and II. Proc. Natl. Acad. Sci. USA 1976, 73, 2365–2369. [Google Scholar] [CrossRef] [Green Version]
- Frago, L.M.; Cañón, S.; de la Rosa, E.J.; León, Y.; Varela-Nieto, I. Programmed cell death in the developing inner ear is balanced by nerve growth factor and insulin-like growth factor I. J. Cell Sci. 2003, 116, 475–486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iwai, K.; Nakagawa, T.; Endo, T.; Matsuoka, Y.; Kita, T.; Kim, T.-S.; Tabata, Y.; Ito, J. Cochlear Protection by Local Insulin-Like Growth Factor-1 Application Using Biodegradable Hydrogel. Laryngoscope 2006, 116, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.Y.; Nakagawa, T.; Okano, T.; Hori, R.; Ono, K.; Tabata, Y.; Lee, S.H.; Ito, J. Novel therapy for hearing loss: Delivery of insulin-like growth factor 1 to the cochlea using gelatin hydrogel. Otol. Neurotol. 2007, 28, 976–981. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, T.; Kumakawa, K.; Usami, S.-I.; Hato, N.; Tabuchi, K.; Takahashi, M.; Fujiwara, K.; Sasaki, A.; Komune, S.; Sakamoto, T.; et al. A randomized controlled clinical trial of topical insulin-like growth factor-1 therapy for sudden deafness refractory to systemic corticosteroid treatment. BMC Med. 2014, 12, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Yamahara, K.; Yamamoto, N.; Nakagawa, T.; Ito, J. Insulin-like growth factor 1: A novel treatment for the protection or regeneration of cochlear hair cells. Hear. Res. 2015, 330, 2–9. [Google Scholar] [CrossRef]
- Hayashi, Y.; Yamamoto, N.; Nakagawa, T.; Ito, J. Insulin-like growth factor 1 inhibits hair cell apoptosis and promotes the cell cycle of supporting cells by activating different downstream cascades after pharmacological hair cell injury in neonatal mice. Mol. Cell. Neurosci. 2013, 56, 29–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, X.; Dellamary, L.; Fernandez, R.; Harrop, A.; Keithley, E.M.; Harris, J.P.; Ye, Q.; Lichter, J.; Lebel, C.; Piu, F. Dose-Dependent Sustained Release of Dexamethasone in Inner Ear Cochlear Fluids Using a Novel Local Delivery Approach. Audiol. Neurotol. 2009, 14, 393–401. [Google Scholar] [CrossRef]
- Park, M.; Hwang, Y.-J.; Noh, T.-S.; Woo, S.-W.; Park, J.-H.; Park, S.H.; Kim, M.S.; Suh, M.-W. Biocompatibility and Therapeutic Effect of 3 Intra-Tympanic Drug Delivery Vehicles in Acute Acoustic Trauma. Audiol. Neurotol. 2020, 25, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Ju, H.J.; Park, M.; Park, J.H.; Shin, G.R.; Choi, H.S.; Suh, M.-W.; Kim, M.S. In Vivo Imaging of Click-Crosslinked Hydrogel Depots Following Intratympanic Injection. Materials 2020, 13, 3070. [Google Scholar] [CrossRef]
- Hwang, Y.J.; Park, M.; Park, M.K.; Lee, J.H.; Oh, S.H.; Suh, M.W. High-Molecular-Weight Hyaluronic Acid Vehicle Can Deliver Gadolinium into the Cochlea at a Higher Concentration for a Longer Duration: A 9.4-T Magnetic Resonance Imaging Study. Front. Neurol. 2021, 12, 901. [Google Scholar]
- Sidell, D.; Ward, J.A.; Pordal, A.; Quimby, C.; Nassar, M.; Choo, D.I. Combination therapies using an intratympanic polymer gel delivery system in the guinea pig animal model: A safety study. Int. J. Pediatr. Otorhinolaryngol. 2016, 84, 132–136. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Long, W.; Liang, Z.; Wen, L.; Yang, F.; Chen, G. A novel vehicle for local protein delivery to the inner ear: Injectable and biodegradable thermosensitive hydrogel loaded with PLGA nanoparticles. Drug Dev. Ind. Pharm. 2017, 44, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Dormer, N.H.; Nelson-Brantley, J.; Staecker, H.; Berkland, C.J. Evaluation of a transtympanic delivery system in Mus musculus for extended release steroids. Eur. J. Pharm. Sci. 2019, 126, 3–10. [Google Scholar] [CrossRef] [PubMed]
- El Kechai, N.; Mamelle, E.; Nguyen, Y.; Huang, N.; Nicolas, V.; Chaminade, P.; Yen-Nicolaÿ, S.; Gueutin, C.; Granger, B.; Ferrary, E.; et al. Hyaluronic acid liposomal gel sustains delivery of a corticoid to the inner ear. J. Control. Release 2016, 226, 248–257. [Google Scholar] [CrossRef]
- Kim, B.S.; Oh, J.M.; Kim, K.S.; Seo, K.S.; Cho, J.S.; Khang, G.; Lee, H.B.; Park, K.; Kim, M.S. BSA-FITC-loaded microcapsules for in vivo delivery. Biomaterials 2009, 30, 902–909. [Google Scholar] [CrossRef]
- Salt, A.N.; Plontke, S.K. Principles of Local Drug Delivery to the Inner Ear. Audiol. Neurotol. 2009, 14, 350–360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fallacara, A.; Baldini, E.; Manfredini, S.; Vertuani, S. Hyaluronic Acid in the Third Millennium. Polymers 2018, 10, 701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Son, A.R.; Kim, D.Y.; Park, S.H.; Jang, J.Y.; Kim, K.; Kim, B.J.; Yin, X.Y.; Kim, J.H.; Min, B.H.; Han, D.K.; et al. Direct chemotherapeutic dual drug delivery through intra-articular injection for synergistic enhancement of rheumatoid arthritis treatment. Sci. Rep. 2015, 5, 14713. [Google Scholar] [CrossRef] [Green Version]
- Choi, J.W.; Kim, Y.S.; Park, J.K.; Song, E.H.; Park, J.H.; Kim, M.S.; Shin, Y.S.; Kim, C.-H. Controlled Release of Hepatocyte Growth Factor from MPEG-b-(PCL-ran-PLLA) Diblock Copolymer for Improved Vocal Fold Regeneration. Macromol. Biosci. 2016, 17, 1600163. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.-J.; Son, J.; Jung, S.Y.; Yi, G.; Yoo, J.; Kim, D.-K.; Koo, H. Optimized phospholipid-based nanoparticles for inner ear drug delivery and therapy. Biomater. 2018, 171, 133–143. [Google Scholar] [CrossRef]
- Mamelle, E.; El Kechai, N.; Adenis, V.; Nguyen, Y.; Sterkers, O.; Agnely, F.; Bochot, A.; Edeline, J.M.; Ferrary, E. Assessment of the efficacy of a local steroid rescue treatment administered 2 days after a moderate noise-induced trauma in guinea pig. Acta Oto-Laryngol. 2018, 138, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Aslıer, N.G.Y.; Tağaç, A.A.; Durankaya, S.M.; Çalışır, M.; Ersoy, N.; Kırkım, G.; Yurdakoç, K.; Bağrıyanık, H.A.; Yılmaz, O.; Sütay, S.; et al. Dexamethasone-loaded chitosan-based genipin-cross-linked hydrogel for prevention of cisplatin induced ototoxicity in Guinea pig model. Int. J. Pediatr. Otorhinolaryngol. 2019, 122, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.-K.; Bahk, C.W.; Kim, S.H.; Ahn, J.-C.; Jung, J.Y.; Chung, P.-S.; Suh, M.-W. Effect of low-level laser treatment on cochlea hair-cell recovery after acute acoustic trauma. J. Biomed. Opt. 2012, 17, 68002. [Google Scholar] [CrossRef] [PubMed]






| Number of Hair Cells (/200 μm) | OHCs in Basal Turn | OHCs in Middle Turn | OHCs in Apical Turn | IHCs in All Three Turns |
|---|---|---|---|---|
| Group 1 (n = 9) | 73 ± 0.7 | 73.1 ± 0.7 | 73.7 ± 0.6 | 54.7 ± 0.8 |
| Group 2 (n = 8) | 72 ± 1.4 | 71.6 ± 0.8 | 73.6 ± 1.1 | 55.3 ± 0.9 |
| p value | 0.743 (ns) | 0.093 (ns) | 0.888 (ns) | 0.864 (ns) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, J.-A.; Kim, B.J.; Hwang, Y.-J.; Woo, S.-W.; Noh, T.-S.; Suh, M.-W. Effect and Biocompatibility of a Cross-Linked Hyaluronic Acid and Polylactide-co-glycolide Microcapsule Vehicle in Intratympanic Drug Delivery for Treating Acute Acoustic Trauma. Int. J. Mol. Sci. 2021, 22, 5720. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms22115720
Cho J-A, Kim BJ, Hwang Y-J, Woo S-W, Noh T-S, Suh M-W. Effect and Biocompatibility of a Cross-Linked Hyaluronic Acid and Polylactide-co-glycolide Microcapsule Vehicle in Intratympanic Drug Delivery for Treating Acute Acoustic Trauma. International Journal of Molecular Sciences. 2021; 22(11):5720. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms22115720
Chicago/Turabian StyleCho, Jung-Ah, Bong Jik Kim, Yu-Jung Hwang, Shin-Wook Woo, Tae-Soo Noh, and Myung-Whan Suh. 2021. "Effect and Biocompatibility of a Cross-Linked Hyaluronic Acid and Polylactide-co-glycolide Microcapsule Vehicle in Intratympanic Drug Delivery for Treating Acute Acoustic Trauma" International Journal of Molecular Sciences 22, no. 11: 5720. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms22115720