A Wearable System to Objectify Assessment of Motor Tasks for Supporting Parkinson’s Disease Diagnosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
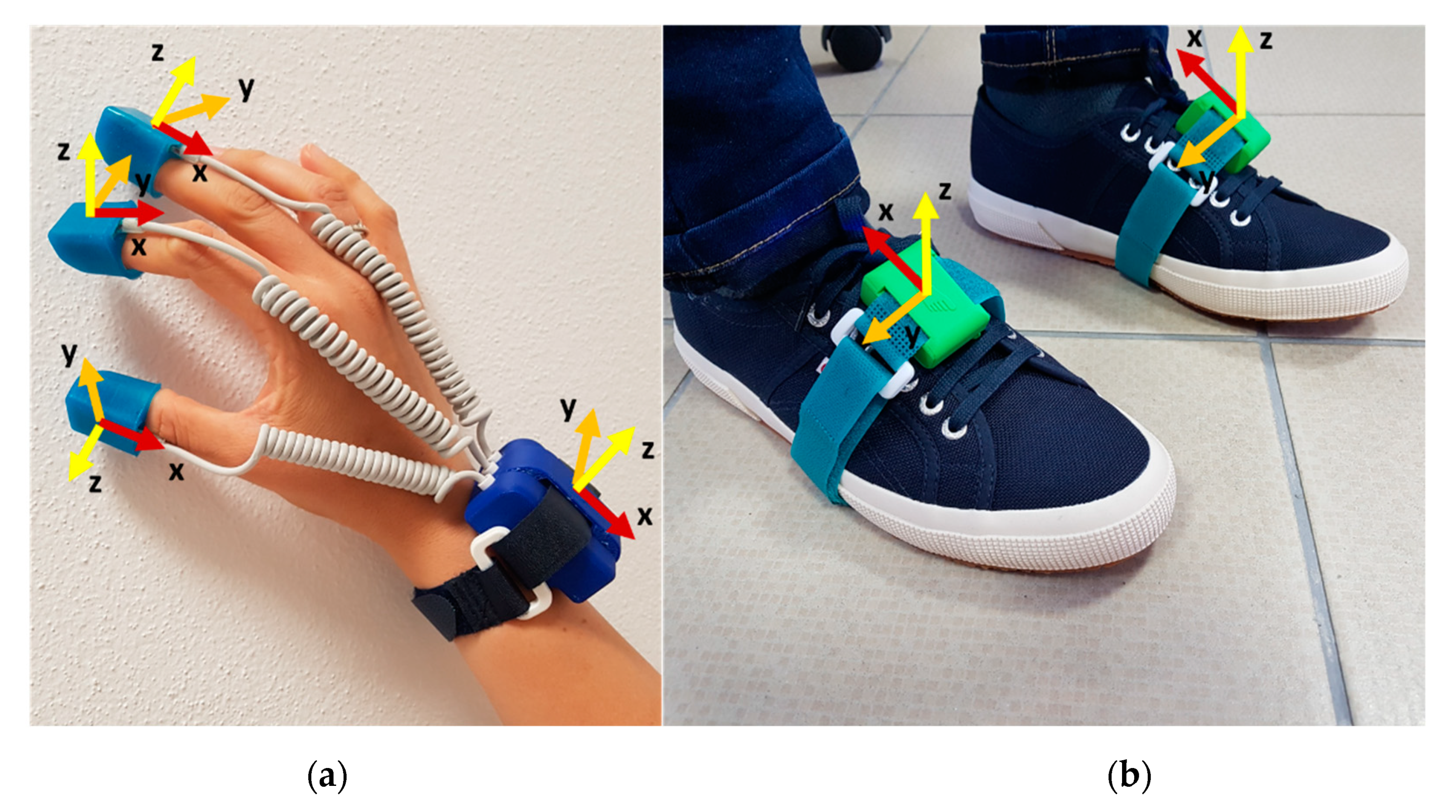
2.2. Instruments
2.3. Experimental Protocol
2.3.1. Upper Limb Tasks
- Thumb–Forefinger Tapping (THFF): the subject kept the hand fixed on the desk so that the plane between the thumb and forefinger joined was parallel to the table. In the starting position, the thumb and the forefinger were in contact, then the subject tapped the forefinger against the thumb as quickly and widely as possible (MDS-UPDRS 3.4—Finger tapping)
- Hand Opening/Closing (OPCL): the subject flexed the arm that was fixed on the table at the elbow, keeping the palm in front of him/herself. Starting from a fist position, the subject had to alternately open and close the hand, holding the forearm and the wrist fixed as quickly and widely as possible (MDS-UPDRS 3.5—Hand movements).
- Hand Pronation/Supination (PSUP): the subject put the arm outstretched in front of himself, with the wrist stable and the hand in prone position. The pronosupination movements had to be performed in parallel to the floor as quickly and widely as possible (MDS-UPDRS 3.6—Pronation-supination movements of hands).
- Hand Resting Tremor (HRST): the subject put the hand on the table in the prone position. This position has kept for the duration of the exercise, with the hand fully relaxed, without contrasting the potential tremor. Additionally, as a distracting task to get evidence on the potential tremor, they were asked to count backwards (MDS-UPDRS 3.17—Hand rest tremor amplitude).
- Hand Postural Tremor (POST): the subject put the arm outstretched in front of himself, with the wrist stable, the hand in the prone position and the fingers outstretched for all the time (MDS-UPDRS 3.15—Postural tremor of hands).
2.3.2. Lower Limb Tasks
- Toe Tapping Heel Pin (TTHP): the subject tapped the toe on the floor always keeping the heel in contact with the ground, as quickly and widely as possible (MDS-UPDRS 3.7—Toe Tapping).
- Leg Agility (HEHE): the subject tapped the heel on the floor always keeping the forefoot raised from the ground, as quickly and widely as possible (MDS-UPDRS 3.8—Leg agility).
- Heel Tapping Toe Pin (HTTP): the subject tapped the heel on the floor always keeping the toe in contact with the ground, as quickly and widely as possible.
- Heel-Toe Tapping (HETO): the subject tapped alternatively the heel and the toe on the floor, as quickly and widely as possible.
- Rotation (ROTA): the subject turned once in the clockwise direction for 360°, then the rotation has repeated in the anticlockwise direction (part of MDS-UPDRS 3.10—Gait).
2.3.3. Full Task
- Gait (GTAF + GTAH): the subject started the gait with the right foot, walking 15 m linearly until reached the finish line. The subject had to walk most naturally, at the preferred velocity. Both walking (GTAF) and arms swinging (GTAH) are simultaneously acquired and analysed (part of MDS-UPDRS 3.10—Gait).
2.4. Signal Processing
2.4.1. Pre-Processing
Movement Tasks
Tremor Tasks
2.4.2. Segmentation and Events Detection
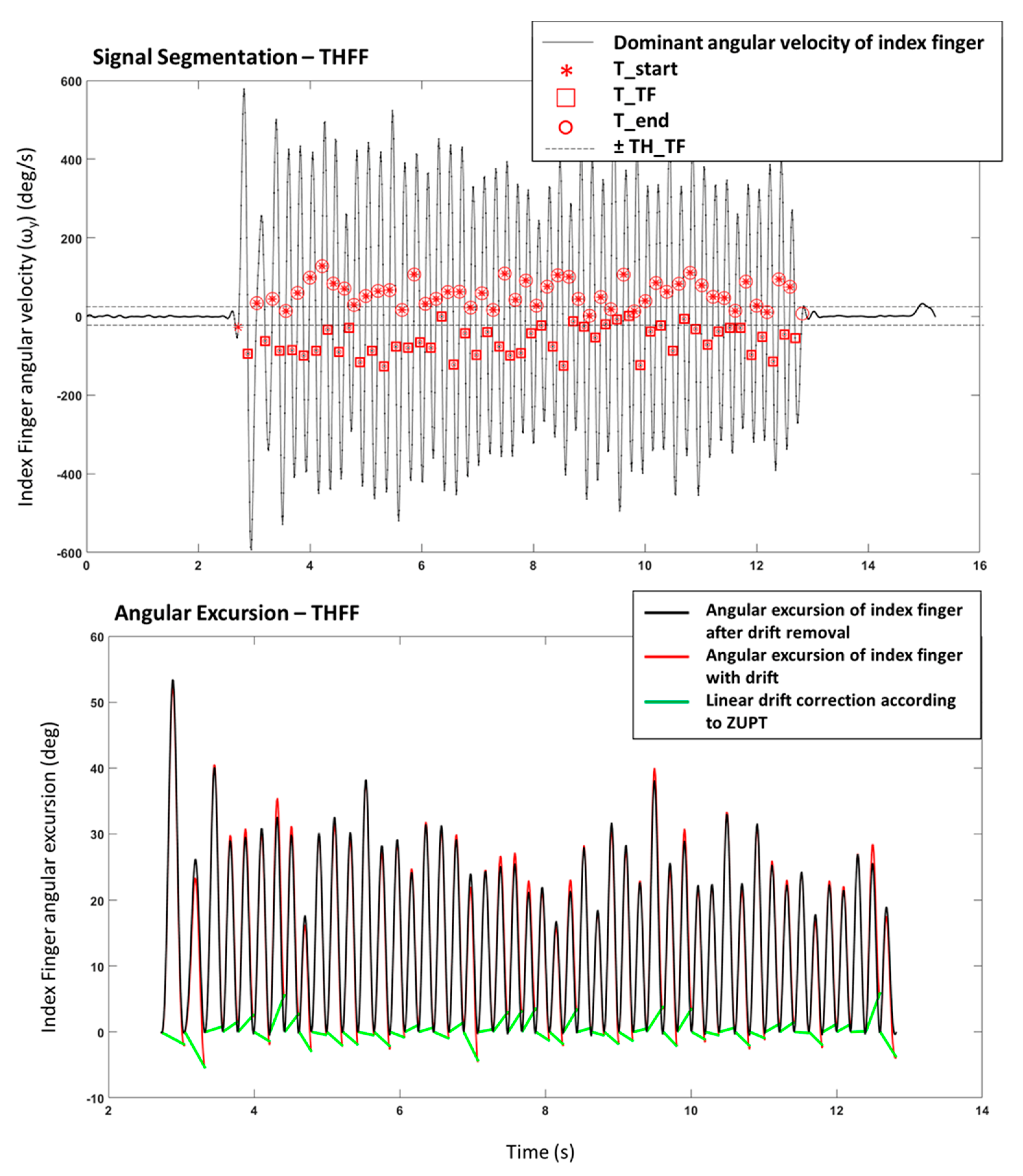
Movement Tasks
- THFF
- OPCL
- PSUP
- GTAH
- GTAF
- ROTA
- TTHP
- HTTP
- HETO
- HEHE
Tremor Tasks
2.4.3. Feature Extraction
Movement Tasks
- Number of movements:Taps = number of (Tend),
- Mean frequency:
- Mean of the maximum movement amplitude (i.e., the maximum angle reached by the toe in the TTHP, maximum angle reached by the heel during HTTP, the maximum angular distance between finger and thumb in THFF, the maximum opening of the hand in OPCL, maximum excursion in supination movement in PSUP, the maximum swing of the arm in GTAH) over all the task:where:with:
- Integral of the magnitude of the total acceleration vector (IAV), which is related to the estimated energy expenditure [36]:
- Variability in frequency overall movements:with:
- Variability in amplitude overall movements:
- Mean of opening (or supination, or frontward) velocity overall movements (for TTHF, OPCL, PSUP, GTAH only):
- Mean of closing (or pronation, or backward) velocity over all movements (for TTHF, OPCL, PSUP, GTAH only):
- Number of tapping movements:Taps = min[number(THS); number(TTO)],
- Mean frequency of the toe-tapping:
- Mean frequency of the heel tapping:
- Mean frequency of the heel-toe tapping:
- Mean of the maximum toe movement amplitude (i.e., the maximum angle from the ground reached by the toe) over all the taps:where:
- Mean of the maximum heel movement amplitude (i.e., the maximum angle from the ground reached by the heel) over all the taps:where:
- Variability in frequency overall movements as in Equation (7), where f is FreqHT.
- Variability in toe amplitude overall movements as in Equation (9), where Exc is ExcT.
- Variability in heel amplitude overall movements as in Equation (9), where Exc is ExcH.
- The IAV parameter was computed in the same manner of Equation (6).
- Gait Time to cover 15 meters:GT_Time = Tend(end) − Tstart(1).
- Number of strides during 15 meters walking:GT_Strd = number(Tend).
- Mean Gait Frequency:GT_Freq = GT_Strd/GT_Time
- Mean Stride Time:
- Mean Swing Time:
- Mean Stance Time:
- Mean Relative Stance:
- Mean of the maximum dorsiflexion angular excursion of the foot over all the strides:where:with:
- Rotation Time to cover 360 degrees:RO_Time = Tend(end) − Tstart(1).
- Number of strides during 15 meters walking:RO_Strd = number(Tend).
- Mean Gait Frequency:RO_Freq = RO_Strd/RO_Time
- Total Stance Time:
- Total Relative Stance:
Tremor Tasks
- Average power in PSD: it is the mean value of the power of the signal calculated through the PSD.
- Fundamental frequency: it is the frequency corresponding to the peak of the power.
- Maximum peak in PSD: it is the maximum value in the PSD of the acceleration signal, and it represents the peak of the power (for HEHE only)
- Percentage power of the signal in frequency band [3.5–7.5] Hz, which is typically associated with Parkinsonian tremor.
- Percentage power of the signal in frequency band [8–12] Hz, which is typically associated with physiological tremor (for POST only).
- The estimated energy expenditure, as IAV parameter, was computed in the same manner of Equation (6).
2.5. Data Analysis
2.5.1. Feature Selection Process
2.5.2. Classification
Support Vector Machine
Random Forest
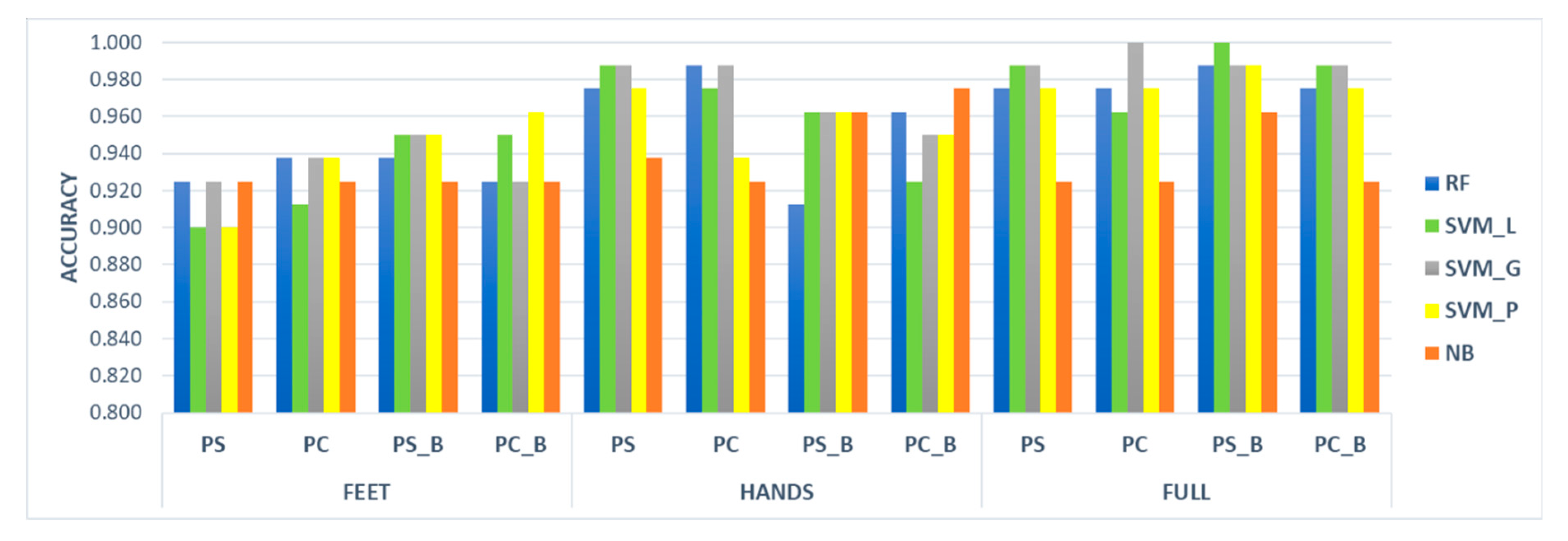
3. Results
3.1. Feature Selection
3.2. Classification Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Abbreviation | Description |
|---|---|
| PD | Parkinson’s Disease |
| HC | Healthy subjects of control |
| QoL | Quality of Life |
| MDS | Movement Disorder Society |
| UPDRS | Unified Parkinson’s Disease Rating Scale |
| HY | Hoehn & Yahr |
| TRL | Technological Readiness Level |
| IMU | Inertial Measurement Unit |
| ZUPT | Zero Velocity Update |
| THFF | Thumb Forefinger Tapping |
| OPCL | Hand Opening/Closing |
| PSUP | Hand Pronation/Supination |
| HRST | Hand Resting Tremor |
| POST | Hand Postural Tremor |
| TTHP | Toe Tapping Heel Pin |
| HEHE | Leg Agility |
| HTTP | Heel Tapping Toe Pin |
| HETO | Heel-Toe Tapping |
| ROTA | Rotation |
| GTAF | Gait |
| GTAH | Arms swing while walking |
| PS dataset | Dataset Post Significance |
| PS_B dataset | Dataset Post Significance with Bonferroni Correction |
| PC dataset | Dataset PS and Post Correlation |
| PC_B dataset | Dataset PS and Post Correlation with Bonferroni Correction |
| SVM | Support Vector Machine |
| SVM_P | Support Vector Machine with Polynomial kernel |
| SVM_L | Support Vector Machine with Linear kernel |
| SVM_G | Support Vector Machine with Gaussian kernel |
| RF | Random Forest |
| NB | Naïve Bayes |
| FEET | Condition including parameters from lower limbs only |
| HANDS | Condition including parameters from upper limbs only |
| FULL | Condition including all the measured parameters |
References
- Fahn, S. Clinical aspects of Parkinson disease. In Parkinson’s Disease: Molecular and Therapeutic Insights from Model Systems; Nass, R., Przedborski, S., Eds.; Elsevier Inc.: Amsterdam, the Netherlands, 2008; pp. 3–48. ISBN 9780123740281. [Google Scholar]
- Dorsey, E.R.; Elbaz, A.; Nichols, E.; Abd-Allah, F.; Abdelalim, A.; Adsuar, J.C.; Dahodwala, N. Global, regional, and national burden of Parkinson’s disease, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2018, 17, 939–953. [Google Scholar] [CrossRef] [Green Version]
- Godoi, B.B.; Amorim, G.D.; Quiroga, D.G.; Holanda, V.M.; Tournier, M.B. Parkinson’s disease and wearable devices, new perspectives for a public health issue: An integrative literature review. Rev. Assoc. Med. Bras. 2019, 65, 1413–1420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Titova, N.; Chauduri, R.K. Non-motor Parkinson’s disease: New concepts and personalised management. Med. J. Aust. 2018, 208, 404–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balzer-Geldsetzer, M.; Klotsche, J.; Reetz, K.; Spottke, A.; Storch, A.; Baudrexel, S.; Mollenhauer, B.; Berg, D.; Liepelt, I.; Kassubek, J.; et al. Quality of life in a German cohort of Parkinson’s patients assessed with three different measures. J. Neurol. 2018, 265, 2713–2722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mosley, P.E.; Moodie, R.; Dissanayaka, N. Caregiver burden in Parkinson disease: A critical review of recent literature. J. Geriatr. Psychiatry Neurol. 2017, 30, 235–252. [Google Scholar] [CrossRef]
- da Silva, S.L.O.; Quelhas, O.L.G.; Neto, J.V.; Leite, M.A.A. The cost of Parkinson’s disease: A systematic review. In Operations Management for Social Good; Leiras, A., Ed.; Springer Nature: Berlin, Germany, 2020; pp. 183–193. ISBN 9783030238155. [Google Scholar]
- Zahra, W.; Rai, S.N.; Birla, H.; Singh, S.S.; Dilnashin, H.; Rathore, A.S.; Singh, S.P. The global economic impact of neurodegenerative diseases: Opportunities and challenges. In Bioeconomy for Sustainable Development; Keswani, C., Ed.; Springer Nature: Singapore, 2020; pp. 333–345. ISBN 9789811394300. [Google Scholar]
- Rees, R.N.; Acharya, A.P.; Schrag, A.; Noyce, A.J. An early diagnosis is not the same as a timely diagnosis of Parkinson’s disease. F1000Research 2018, 7, 1106. [Google Scholar] [CrossRef]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- Heinzel, S.; Berg, D.; Gasser, T.; Chen, H.; Yao, C. Update of the MDS research criteria for prodromal Parkinson’s disease. Mov. Disord. 2019, 34, 1464–1470. [Google Scholar] [CrossRef]
- Marsili, L.; Rizzo, G.; Colosimo, C. Diagnostic criteria for Parkinson’s disease: From James Parkinson to the concept of prodromal disease. Front. Neurol. 2018, 9, 156. [Google Scholar] [CrossRef]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.; Dodel, R.; et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef]
- El-Gohary, M.; Pearson, S.; McNames, J.; Mancini, M.; Horak, F.; Mellone, S.; Chiari, L. Continuous monitoring of turning in patients with movement disability. Sensors 2014, 14, 356–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, K.; Xiong, W.-X.; Liu, F.-T.; Sun, Y.-M.; Luo, S.; Ding, Z.-T.; Wu, J.-J.; Wang, J. Objective and quantitative assessment of motor function in Parkinson’s disease—From the perspective of practical applications. Ann. Transl. Med. 2016, 4, 90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rovini, E.; Maremmani, C.; Cavallo, F. How wearable sensors can support Parkinson’s disease diagnosis and treatment: A systematic review. Front. Neurosci. 2017, 11, 555. [Google Scholar] [CrossRef] [PubMed]
- Kubota, K.J.; Chen, J.A.; Little, M.A. Machine learning for large-scale wearable sensor data in Parkinson’s disease: Concepts, promises, pitfalls, and futures. Mov. Disord. 2016, 31, 1314–1326. [Google Scholar] [CrossRef]
- Jiménez Ruiz, A.R.; Seco Granja, F.; Prieto Honorato, J.C.; Guevara Rosas, J.I. Accurate pedestrian indoor navigation by tightly coupling foot-mounted IMU and RFID measurements. IEEE Trans. Instrum. Meas. 2012, 61, 178–189. [Google Scholar] [CrossRef] [Green Version]
- Moschetti, A.; Fiorini, L.; Esposito, D.; Dario, P.; Cavallo, F. Recognition of daily gestures with wearable inertial rings and bracelets. Sensors 2016, 16, 1341. [Google Scholar] [CrossRef] [Green Version]
- Garza-Rodríguez, A.; Sánchez-Fernández, L.P.; Sánchez-Pérez, L.A.; Ornelas-Vences, C.; Ehrenberg-Inzunza, M. Pronation and supination analysis based on biomechanical signals from Parkinson’s disease patients. Artif. Intell. Med. 2018, 84, 7–22. [Google Scholar] [CrossRef]
- Bobić, V.N.; Djurić-Jovičić, M.; Dragašević, N.; Popović, M.B.; Kostić, V.S.; Kvaščev, G. An expert system for quantification of bradykinesia based on wearable inertial sensors.pdf. Sensors 2019, 19, 2644. [Google Scholar] [CrossRef] [Green Version]
- Djurić-Jovičić, M.; Jovičić, N.S.; Roby-Brami, A.; Popović, M.B.; Kostić, V.S.; Djordjević, A.R. Quantification of finger-tapping angle based on wearable sensors. Sensors 2017, 17, 203. [Google Scholar] [CrossRef]
- Van Den Noort, J.; Verhagen, R.; Van Dijk, K.; Veltink, P.; Vos, M.; de Bie, R.M.A.; Bour, L.J.; Heida, C.T. Quantification of hand motor symptoms in Parkinson’s disease: A proof-of-principle study using inertial and force sensors. Ann. Biomed. Eng. 2017, 45, 2423–2436. [Google Scholar] [CrossRef]
- Technology Readiness Level. Available online: https://ec.europa.eu/research/participants/data/ref/h2020/wp/2014_2015/annexes/h2020-wp1415-annex-g-trl_en.pdf (accessed on 27 February 2020).
- Aghanavesi, S.; Westin, J.; Bergquist, F.; Nyholm, D.; Askmark, H.; Sten Magnus, A.; Radu, C. A multiple motion sensors index for motor state quantification in Parkinson’s disease. Comput. Methods Progr. Biomed. 2020, 189, 105309. [Google Scholar] [CrossRef] [PubMed]
- Rovini, E.; Moschetti, A.; Fiorini, L.; Esposito, D.; Maremmani, C.; Cavallo, F. Wearable sensors for prodromal motor assessment of Parkinson’s disease using supervised learning. In Proceedings of the 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Berlin, Germany, 23–27 July 2019; pp. 4318–4321. [Google Scholar]
- Di Lazzaro, G.; Ricci, M.; Al-Wardat, M.; Schirinzi, T.; Scalise, S.; Giannini, F.; Mercuri, N.B.; Saggio, G.; Pisani, A. Technology-based objective measures detect subclinical axial signs in untreated, de novo Parkinson’s disease. J. Parkinsons Dis. 2020, 10, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Maremmani, C.; Cavallo, F.; Purcaro, C.; Rossi, G.; Salvadori, S.; Rovini, E.; Esposito, D.; Pieroni, A.; Ramat, S.; Vanni, P.; et al. Combining olfactory test and motion analysis sensors in Parkinson’s disease preclinical diagnosis: A pilot study. Acta Neurol. Scand. 2018, 137, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, F.; Maremmani, C.; Esposito, D.; Rovini, E.; Dario, P.; Carrozza, M.C. Method and Related Apparatus for Monitoring Biomechanical Performances of Human Limbs; WO/2014/108883; PCT/IB2014/058265; World Intellectual Property Organization, International Bureau: Geneva, Switzerland, 2014. [Google Scholar]
- Cavallo, F.; Moschetti, A.; Esposito, D.; Maremmani, C.; Rovini, E. Upper limb motor pre-clinical assessment in Parkinson’s disease using machine learning. Parkinsonism Relat. Disord. 2019, 63, 111–116. [Google Scholar] [CrossRef] [Green Version]
- Rovini, E.; Maremmani, C.; Moschetti, A.; Esposito, D.; Cavallo, F. Comparative motor pre-clinical assessment in Parkinson’s disease using supervised machine learning approaches. Ann. Biomed. Eng. 2018, 46, 2057–2068. [Google Scholar] [CrossRef]
- Kim, J.-W.; Kwon, Y.; Kim, Y.-M.; Chung, H.-Y.; Eom, G.-M.; Jun, J.-H.; Lee, J.-W.; Koh, S.-B.; Park, B.K.; Kwon, D.-K. Analysis of lower limb bradykinesia in Parkinson’s disease patients. Geriatr. Gerontol. Int. 2012, 12, 257–264. [Google Scholar] [CrossRef]
- Rigas, G.; Tzallas, A.T.; Tsipouras, M.G.; Bougia, P.; Tripoliti, E.E.; Baga, D.; Fotiadis, D.I.; Tsouli, S.G.; Konitsiotis, S. Assessment of tremor activity in the Parkinson’s disease using a set of wearable sensors. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 478–487. [Google Scholar] [CrossRef]
- Sabatini, A.M.; Martelloni, C.; Scapellato, S.; Cavallo, F. Assessment of walking features from foot inertial sensing. IEEE Trans. Biomed. Eng. 2005, 52, 486–494. [Google Scholar] [CrossRef] [Green Version]
- Ulamis, F.; Luy, M.; Cam, E.; Uzun, I. Effects of zero velocity update on total displacement for indoor inertial positioning systems. Int. J. Intell. Syst. Appl. Eng. 2017, 2, 59–63. [Google Scholar] [CrossRef] [Green Version]
- Cavallo, F.; Megali, G.; Sinigaglia, S.; Tonet, O.; Dario, P. A biomechanical analysis of surgeon’s gesture in a laparoscopic virtual scenario. Stud. Health Technol. Inf. 2006, 119, 79–84. [Google Scholar]
- Burges, C.J.C. A tutorial on support vector machines for pattern recognition. Data Min. Knowl. Discov. 1998, 2, 121–167. [Google Scholar] [CrossRef]
- Breiman, L. Random forest. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Maroco, J.; Silva, D.; Rodrigues, A.; Guerreiro, M.; Santana, I.; de Mendonça, A. Data mining methods in the prediction of dementia: A real-data comparison of the accuracy, sensitivity and specificity of linear discriminant analysis, logistic regression, neural networks, support vector machines, classification trees and random forests. BMC Res. Notes 2011, 4, 299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, K. YAN-PRTools. Available online: https://it.mathworks.com/matlabcentral/fileexchange/56723-yan-prtools (accessed on 23 March 2020).
- Zhang, H. The optimality of naive bayes. In Proceedings of the 17th International Florida Artificial Intelligence Research Society Conference, Sarasota, FL, USA, 19–22 May 2004; Volume 1, pp. 1–6. [Google Scholar]
- Oshiro, T.M.; Perez, P.S.; Baranauskas, J.A. How many trees in a random forest? In Proceedings of the International Workshop on Machine Learning and Data Mining in Pattern Recognition, Berlin, Germany, 13–20 July 2012; pp. 154–168. [Google Scholar]
- Moschetti, A.; Fiorini, L.; Esposito, D.; Dario, P.; Cavallo, F. Toward an unsupervised approach for daily gesture recognition in assisted living applications. IEEE Sens. J. 2017, 17, 8395–8403. [Google Scholar] [CrossRef]
- Dormann, C.F.; Elith, J.; Bacher, S.; Buchmann, C.; Carl, G.; Carré, G.; Marquéz, J.R.G.; Gruber, B.; Lafourcade, B.; Leitão, P.J.; et al. Collinearity: A review of methods to deal with it and a simulation study evaluating their performance. Ecography 2013, 36, 27–46. [Google Scholar] [CrossRef]
- Elith, J.H.; Graham, C.P.; Anderson, R.; Dudík, M.; Ferrier, S.; Guisan, A.J.; Hijmans, R.; Huettmann, F.R.; Leathwick, J.; Lehmann, A.; et al. Novel methods improve prediction of species’ distributions from occurrence data. Ecography 2006, 29, 129–151. [Google Scholar] [CrossRef] [Green Version]
- Rovini, E.; Esposito, D.; Fabbri, L.; Pancani, S.; Vannetti, F.; Cavallo, F. Vision optical-based evaluation of SensHand accuracy for Parkinson’s disease motor assessment. In Proceedings of the IEEE International Symposium on Measurements & Networking (M&N), Catania, Italy, 8–10 July 2019. [Google Scholar]
| Exercise | ||||||
|---|---|---|---|---|---|---|
| Parameter | TTHP | HTTP | HETO | HEHE | ROTA | GTAF |
| Number of movements | TT_Taps | HH_Taps | HT_Taps | RO_Strd | GT_Strd | |
| Frequency | TT_Freq | HH_Freq | HT_FreqT HT_FreqH HT_FreqHT | HE_Freq | RO_Freq | GT_Freq |
| Max. Amplitude | TT_Exc | HH_Exc | HT_ExcT HT_ExcH | GT_Ang | ||
| Frequency Variability | TT_CVfreq | HH_CVfreq | HT_CVfreq | |||
| Amplitude Variability | TT_CVexc | HH_CVexc | HT_CVexcT HT_CVexcH | |||
| Time | RO_Time | GT_Time | ||||
| Stride Time | GT_StrdT | |||||
| Swing Time | GT_SWT | |||||
| Stance Time | RO_STT | GT_STT | ||||
| Relative Stance | RO_RS | GT_RS | ||||
| Average Power | HE_Power | |||||
| Peak Power | HE_Peak | |||||
| IAV | TT_IAV | HH_IAV | HT_IAV | HE_IAV | ||
| Exercise | ||||||
|---|---|---|---|---|---|---|
| Parameter | THFF | OPCL | PSUP | HRST 1 | POST 1 | GTAH |
| Number of movements | TF_Taps | OC_Taps | PS_Taps | GT_Taps | ||
| Frequency | TF_Freq | OC_Freq | PS_Freq | RT_FreqA RT_FreqG | PT_FreqA PT_FreqG | GT_HFreq |
| Max. Amplitude | TF_Exc | OC_Exc | PS_Exc | GT_Exc | ||
| Opening Velocity | TF_ωo | OC_ωo | PS_ωs | GT_ωf | ||
| Closing Velocity | TF_ωc | OC_ωc | PS_ωp | GT_ωb | ||
| Frequency Variability | TF_CVfreq | OC_CVfreq | PS_CVfreq | GT_CVfreq | ||
| Amplitude Variability | TF_CVexc | OC_CVexc | PS_CVexc | GT_CVexc | ||
| Average Power | RT_PwrA RT_PwrG | PT_PwrA PT_PwrG | ||||
| % Power [3.5–7.5] Hz | RT_Perc1A RT_Perc1G | PT_Perc1A PT_Perc1G | ||||
| % Power [8–12] Hz | PT_Perc2A PT_Perc2G | |||||
| IAV | TF_IAV | OC_IAV | PS_IAV | RT_IAV | PT_IAV | GT_IAV |
| Left | Right | Significance | ||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | HC Median (IQR) | PD Median (IQR) | HC Median (IQR) | PD Median (IQR) | PS | PS_B | PC | PC_B |
| TT_Taps | 33.0 (11.2) | 29.0 (9.0) | 38.5 (9.2) | 31.0 (9.0) | X | X | X | X |
| TT_Freq | 3.29 (1.17) | 2.89 (0.92) | 3.93 (0.95) | 3.11 (0.98) | X | X | ||
| TT_Exc | 10.4 (5.3) | 7.7 (5.8) | 7.2 (5.4) | 7.6 (5.4) | ||||
| TT_CVfreq | 41.3 (25.4) | 48.3 (23.6) | 39.8 (18.1) | 38.7 (22.8) | ||||
| TT_Cvexc | 60.3 (35.1) | 70.1 (27.4) | 65.0 (23.5) | 64.1 (27.4) | ||||
| TT_IAV | 108.6 (4.2) | 99.0 (17.7) | 111.5 (4.5) | 101.2 (20.7) | X | X | X | X |
| HH_Taps | 38.0 (7.2) | 31.7 (8.2) | 40.0 (8.0) | 32.2 (10.2) | X | X | X | X |
| HH_Freq | 3.79 (0.74) | 3.16 (0.94) | 4.02 (0.79) | 3.22 (1.06) | X | X | ||
| HH_Exc | 10.3 (6.6) | 5.3 (8.8) | 8.8 (6.3) | 6.2 (5.8) | X | X | ||
| HH_Cvfreq | 53.0 (13.0) | 56.8 (20.6) | 54.8 (18.3) | 54.5 (27.1) | ||||
| HH_Cvexc | 80.6 (15.7) | 85.7 (21.0)) | 84.4 (18.9) | 82.6 (26.4) | ||||
| HH_IAV | 110.6 (4.1) | 106.3 (8.9) | 112.2 (3.9) | 106.6 (9.3) | X | X | X | X |
| HT_Taps | 14.5 (3.5) | 13.7 (3.2) | 15.7 (4.0) | 13.5 (3.5) | X | X | X | X |
| HT_FreqT | 1.50 (0.37) | 1.43 (0.32) | 1.64 (0.46) | 1.40 (0.36) | X | X | ||
| HT_FreqH | 1.51 (0.37) | 1.44 (0.31) | 1.64 (0.46) | 1.41 (0.36) | X | X | ||
| HT_FreqHT | 3.17 (0.70) | 2.97 (0.76) | 3.35 (0.81) | 2.76 (0.93) | X | X | ||
| HT_ExcT | 36.6 (7.7) | 21.4 (13.7) | 32.0 (10.9) | 20.1 (9.7) | X | X | X | X |
| HT_ExcH | 36.3 (8.3) | 22.4 (12.6) | 31.7 (11.4) | 20.6 (9.3) | X | X | ||
| HT_Cvfreq | 40.8 (30.2) | 61.5 (26.9) | 41.3 (31.6) | 53.1 (31.1) | X | X | X | X |
| HT_CvexcT | 52.6 (48.2) | 71.9 (38.4) | 49.2 (44.8) | 44.8 (39.9) | X | X | ||
| HT_CvexcH | 55.6 (45.8) | 70.3 (41.5) | 56.0 (50.0) | 66.5 (32.9) | X | |||
| HT_IAV | 101.4 (4.9) | 96.1 (14.7) | 103.6 (3.9) | 96.2 (14.0) | X | X | X | X |
| HE_Power | 81.9 (32.4) | 6.1 (16.6) | 82.8 (37.5) | 7.2 (12.5) | X | X | X | X |
| HE_Peak | 111.1 (80.1)) | 127.8 (92.5) | 13.2 (28.4) | 13.3 (23.6) | X | X | ||
| HE_Freq | 3.86 (0.69) | 3.59 (0.83) | 4.30 (0.93) | 3.83 (0.76) | X | X | X | X |
| HE_IAV | 140.5 (26.4) | 104.5 (11.8) | 141.4 (25.8) | 102.6 (11.2) | X | X | ||
| GT_Time | 11.2 (1.9) | 13.4 (2.2) | 11.9 (2.1) | 13.7 (3.1) | X | X | X | X |
| GT_Strd | 11.0 (1.8) | 12.5 (2.3) | 11.0 (1.8) | 12.8 (3.0) | X | X | X | X |
| GT_Freq | 0.95 (0.09) | 0.94 (0.06) | 0.96 (0.10) | 0.94 (0.11) | ||||
| GT_StrdT | 1.07 (0.11) | 1.09 (0.07) | 1.06 (0.11) | 1.08 (0.13) | ||||
| GT_SWT | 0.33 (0.03) | 0.32 (0.03) | 0.32 (0.03) | 0.33 (0.03) | ||||
| GT_STT | 0.74 (0.09) | 0.76 (0.07) | 0.75 (0.09) | 0.77 (0.10) | ||||
| GT_RS | 69.1 (1.7) | 69.7 (1.9) | 70.4 (2.4) | 70.2 (2.1) | X | X | ||
| GT_Ang | 92.1 (9.8) | 75.1 (14.0) | 76.9 (11.0) | 68.9 (13.4) | X | X | X | X |
| RO_Time | 2.5 (0.6) | 2.3 (1.0) | 3.7 (1.7) | 3.7 (1.7) | X | X | X | X |
| RO_Strd | 3.0 (1.0) | 3.0 (0.5) | 4.5 (1.2) | 4.5 (1.5) | X | X | X | X |
| RO_Freq | 1.39 (0.29) | 1.34 (0.40) | 1.20 (0.33) | 1.25 (0.35) | X | X | ||
| RO_STT | 1.07 (0.48) | 1.01 (0.67) | 1.65 (1.23) | 1.76 (1.30) | X | X | ||
| RO_RS | 44.1 (11.3) | 44.4 (13.6) | 48.6 (14.5) | 48.7 (11.9) | X | |||
| Left | Right | Significance | ||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | HC Median (IQR) | PD Median (IQR) | HC Median (IQR) | PD Median (IQR) | PS | PS_B | PC | PC_B |
| PS_Taps | 23.0 (7.5) | 16.0 (10.7) | 23.8 (9.8) | 15.5 (9.0) | X | X | X | X |
| PS_Freq | 2.36 (0.75) | 1.62 (1.07) | 2.37 (1.09) | 1.50 (0.95) | X | X | ||
| PS_Exc | 157.1 (39.7) | 107.1 (44.5) | 149.6 (36.8) | 122.8 (41.9) | X | X | X | X |
| PS_ωp | 641.5 (139.9) | 349.5 (193.2) | 647.4 (163.5) | 334.2 (218.7) | X | X | ||
| PS_ωs | 715.2 (233.2) | 338.5 (206.8) | 695.1 (215.5) | 324.9 (196.9) | X | X | X | X |
| PS_CVfreq | 24.5 (16.3) | 24.3 (22.1) | 23.2 (12.9) | 21.7 (17.9) | ||||
| PS_CVexc | 24.2 (31.4) | 27.1 (37.0) | 22.1 (15.8) | 29.6 (26.7) | ||||
| PS_IAV | 155.8 (55.5) | 109.7 (11.0) | 150.6 (53.4) | 107.5 (16.5) | X | X | ||
| OC_Taps | 34.0 (6.8) | 21.5 (15.5) | 36.0 (9.8) | 21.5 (13.3) | X | X | X | X |
| OC_Freq | 3.39 (0.68) | 2.10 (1.50) | 3.58 (1.00) | 2.14 (1.32) | X | X | ||
| OC_Exc | 104.3 (44.1) | 116.4 (77.5) | 89.7 (50.7) | 103.3 (73.3) | ||||
| OC_ωo | 597.3 (211.6) | 458.5 (326.9) | 554.5 (215.6) | 433.3 (268.0) | X | |||
| OC_ωc | 706.5 (249.9) | 435.5 (420.0) | 637.8 (257.1) | 464.8 (361.9) | X | X | X | X |
| OC_CVfreq | 23.4 (12.3) | 30.1 (28.4) | 25.4 (14.0) | 26.1 (24.9) | X | X | ||
| OC_CVexc | 44.8 (26.4) | 50.6 (34.2) | 56.6 (23.3) | 41.7 (35.9) | ||||
| OC_IAV | 258.5 (81.8) | 144.7 (97.8) | 241.7 (66.7) | 136.2 (90.3) | X | X | X | X |
| TF_Taps | 44.3 (11.5) | 29.3 (16.5) | 46.5 (12.0) | 31.5 (17.5) | X | X | X | X |
| TF_Freq | 4.45 (1.20) | 2.94 (1.71) | 4.69 (1.21) | 3.17 (1.76) | X | X | ||
| TF_Exc | 23.6 (21.5) | 24.5 (25.9) | 15.9 (17.9) | 20.9 (26.6) | ||||
| TF_ωo | 169.6 (119.6) | 110.9 (104.3) | 117.0 (104.1) | 109.1 (114.6) | ||||
| TF_ωc | 201.8 (138.2) | 119.5 (135.8) | 144.4 (123.2) | 127.3 (132.7) | X | X | ||
| TF_CVfreq | 26.3 (19.1) | 41.3 (37.9) | 24.8 (22.5) | 49.1 (35.3) | X | X | X | X |
| TF_CVexc | 73.9 (23.7) | 75.0 (42.9) | 82.1 (21.7) | 83.7 (32.4) | ||||
| TF_IAV | 147.7 (31.7) | 114.0 (39.7) | 129.3 (27.6) | 112.3 (26.6) | X | X | X | X |
| GT_Taps | 12.8 (1.5) | 13.0 (2.5) | 12.5 (1.8) | 13.8 (3.5) | X | X | X | X |
| GT_HFreq | 0.96 (0.12) | 0.97 (0.13) | 0.96 (0.10) | 0.97 (0.18) | ||||
| GT_Exc | 73.7 (38.1) | 41.4 (42.0) | 74.3 (35.7) | 38.8 (29.6) | X | X | ||
| GT_ωf | 77.8 (40.6) | 45.8 (44.2) | 64.3 (39.6) | 31.0 (30.7) | X | X | ||
| GT_ωb | 55.4 (24.9) | 49.6 (27.0) | 43.4 (31.9) | 58.9 (27.4) | X | X | ||
| GT_CVfreq | 13.3 (8.8) | 21.7 (50.4) | 11.8 (16.7) | 29.3 (46.0) | X | X | ||
| GT_CVexc | 41.3 (21.7) | 24.1 (26.3) | 38.1 (19.7) | 18.3 (17.3) | X | X | X | X |
| GT_IAV | 135.7 (25.3) | 142.4 (16.9) | 127.0 (15.1) | 143.5 (29.3) | X | X | X | X |
| RT_PwrA | 0.0013 (0.0005) | 0.0018 (0.0009) | 0.0017 (0.0005) | 0.0019 (0.0009) | X | X | ||
| RT_FreqA | 6.42 (3.78) | 6.57 (3.98) | 6.84 (4.17) | 5.79 (3.22) | ||||
| RT_Perc1A | 29.3 (4.8) | 31.0 (4.0) | 29.4 (6.5) | 31.3 (7.4) | X | X | ||
| RT_IAV | 97.7 (2.2) | 103.3 (8.7) | 98.7 (3.8) | 103.6 (5.3) | X | X | ||
| RT_PwrG | 0.052 (0.604) | 0.675 (0.459) | 0.048 (0.572) | 0.749 (1.084) | X | X | X | X |
| RT_FreqG | 5.42 (2.61) | 4.93 (2.12) | 5.23 (3.13) | 5.28 (2.62) | ||||
| RT_Perc1G | 32.6 (8.2) | 38.2 (14.1) | 32.5 (7.0) | 37.1 (18.1) | X | X | ||
| PT_PwrA | 0.017 (0.015) | 0.022 (0.031) | 0.015 (0.012) | 0.019 (0.026) | ||||
| PT_FreqA | 7.59 (4.03) | 7.62 (2.40) | 8.30 (1.88) | 7.40 (2.25) | X | X | ||
| PT_Perc1A | 17.3 (8.5) | 30.7 (16.0) | 22.7 (10.8) | 28.9 (19.0) | X | X | X | X |
| PT_Perc2A | 36.4 (11.8) | 30.6 (11.5) | 35.0 (11.9) | 28.6 (17.7) | X | X | ||
| PT_PwrG | 1.39 (0.29) | 1.34 (0.40) | 1.20 (0.33) | 1.25 (0.35) | X | X | ||
| PT_FreqG | 5.59 (5.18) | 5.84 (3.23) | 7.15 (3.76) | 5.76 (3.44) | ||||
| PT_IAV | 100.1 (2.6) | 103.4 (7.2) | 99.6 (3.4) | 101.6 (9.1) | X | X | X | X |
| PT_Perc1G | 25.0 (11.7) | 33.7 (20.5) | 22.3 (7.3) | 31.7 (20.5) | X | X | X | X |
| PT_Perc2G | 27.0 (10.5) | 22.7 (15.1) | 30.5 (15.2) | 23.8 (20.8) | X | X | ||
| PS | PC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| FEET | RF | SVM_L | SVM_G | SVM_P | NB | RF | SVM_L | SVM_G | SVM_P | NB |
| Recall | 0.900 | 0.900 | 0.850 | 0.900 | 0.850 | 0.925 | 0.925 | 0.950 | 0.900 | 0.850 |
| Specificity | 0.950 | 0.900 | 1.000 | 0.900 | 1.000 | 0.950 | 0.900 | 0.925 | 0.975 | 1.000 |
| Accuracy | 0.925 | 0.900 | 0.925 | 0.900 | 0.925 | 0.938 | 0.913 | 0.938 | 0.938 | 0.925 |
| Precision | 0.947 | 0.900 | 1.000 | 0.900 | 1.000 | 0.949 | 0.902 | 0.927 | 0.973 | 1.000 |
| F_measure | 0.923 | 0.900 | 0.919 | 0.900 | 0.930 | 0.937 | 0.914 | 0.938 | 0.939 | 0.930 |
| HANDS | ||||||||||
| Recall | 0.975 | 0.975 | 0.975 | 0.975 | 0.975 | 0.975 | 0.975 | 1.000 | 0.950 | 0.950 |
| Specificity | 0.975 | 1.000 | 1.000 | 0.975 | 0.900 | 1.000 | 0.975 | 0.975 | 0.925 | 0.900 |
| Accuracy | 0.975 | 0.988 | 0.988 | 0.975 | 0.938 | 0.988 | 0.975 | 0.988 | 0.938 | 0.925 |
| Precision | 0.975 | 0.988 | 1.000 | 0.975 | 0.907 | 1.000 | 0.975 | 0.976 | 0.927 | 0.905 |
| F_measure | 0.975 | 0.987 | 0.987 | 0.975 | 0.939 | 0.987 | 0.975 | 0.988 | 0.938 | 0.926 |
| FULL | ||||||||||
| Recall | 0.975 | 0.975 | 0.975 | 0.950 | 0.900 | 0.950 | 0.925 | 1.000 | 0.950 | 0.925 |
| Specificity | 1.000 | 1.000 | 1.000 | 1.000 | 0.950 | 1.000 | 1.000 | 1.000 | 1.000 | 0.925 |
| Accuracy | 0.975 | 0.988 | 0.988 | 0.975 | 0.925 | 0.975 | 0.963 | 1.000 | 0.975 | 0.925 |
| Precision | 1.000 | 1.000 | 1.000 | 1.000 | 0.947 | 1.000 | 1.000 | 1.000 | 1.000 | 0.925 |
| F_measure | 0.976 | 0.987 | 0.987 | 0.976 | 0.926 | 0.976 | 0.961 | 1.000 | 0.976 | 0.925 |
| PS_B | PC_B | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| FEET | RF | SVM_L | SVM_G | SVM_P | NB | RF | SVM_L | SVM_G | SVM_P | NB |
| Recall | 0.925 | 0.900 | 0.900 | 0.975 | 0.850 | 0.900 | 0.950 | 0.900 | 0.950 | 0.850 |
| Specificity | 0.950 | 1.000 | 1.000 | 0.925 | 1.000 | 0.950 | 0.950 | 0.950 | 0.975 | 1.000 |
| Accuracy | 0.938 | 0.950 | 0.950 | 0.950 | 0.925 | 0.925 | 0.950 | 0.925 | 0.963 | 0.925 |
| Precision | 0.949 | 1.000 | 1.000 | 0.929 | 1.000 | 0.947 | 0.950 | 0.947 | 0.974 | 1.000 |
| F_measure | 0.937 | 0.947 | 0.947 | 0.951 | 0.930 | 0.923 | 0.950 | 0.923 | 0.963 | 0.930 |
| HANDS | ||||||||||
| Recall | 0.850 | 0.950 | 0.950 | 0.925 | 0.950 | 0.925 | 0.900 | 0.925 | 0.900 | 0.975 |
| Specificity | 0.975 | 0.975 | 0.975 | 1.000 | 0.975 | 1.000 | 0.950 | 0.975 | 1.000 | 0.975 |
| Accuracy | 0.913 | 0.963 | 0.963 | 0.963 | 0.963 | 0.963 | 0.925 | 0.950 | 0.950 | 0.975 |
| Precision | 0.971 | 0.963 | 0.974 | 1.000 | 0.974 | 1.000 | 0.926 | 0.974 | 1.000 | 0.975 |
| F_measure | 0.907 | 0.962 | 0.962 | 0.964 | 0.963 | 0.961 | 0.923 | 0.949 | 0.952 | 0.975 |
| FULL | ||||||||||
| Recall | 0.950 | 1.000 | 0.975 | 0.975 | 0.950 | 0.950 | 0.975 | 0.975 | 0.950 | 0.925 |
| Specificity | 0.975 | 1.000 | 1.000 | 1.000 | 0.975 | 1.000 | 1.000 | 1.000 | 1.000 | 0.925 |
| Accuracy | 0.988 | 1.000 | 0.988 | 0.988 | 0.963 | 0.975 | 0.988 | 0.988 | 0.975 | 0.925 |
| Precision | 0.974 | 1.000 | 1.000 | 0.974 | 0.974 | 1.000 | 1.000 | 1.000 | 1.000 | 0.925 |
| F_measure | 0.988 | 1.000 | 0.987 | 0.988 | 0.963 | 0.976 | 0.987 | 0.987 | 0.976 | 0.925 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rovini, E.; Maremmani, C.; Cavallo, F. A Wearable System to Objectify Assessment of Motor Tasks for Supporting Parkinson’s Disease Diagnosis. Sensors 2020, 20, 2630. https://0-doi-org.brum.beds.ac.uk/10.3390/s20092630
Rovini E, Maremmani C, Cavallo F. A Wearable System to Objectify Assessment of Motor Tasks for Supporting Parkinson’s Disease Diagnosis. Sensors. 2020; 20(9):2630. https://0-doi-org.brum.beds.ac.uk/10.3390/s20092630
Chicago/Turabian StyleRovini, Erika, Carlo Maremmani, and Filippo Cavallo. 2020. "A Wearable System to Objectify Assessment of Motor Tasks for Supporting Parkinson’s Disease Diagnosis" Sensors 20, no. 9: 2630. https://0-doi-org.brum.beds.ac.uk/10.3390/s20092630





