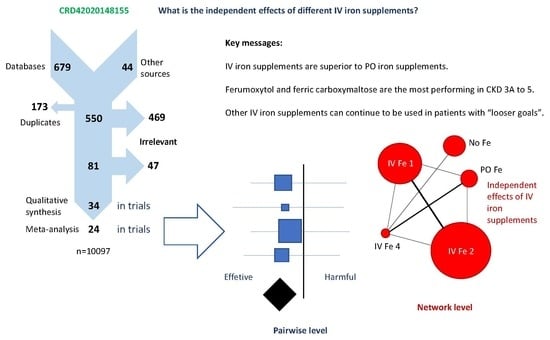
The Impact of Iron Supplementation for Treating Anemia in Patients with Chronic Kidney Disease: Results from Pairwise and Network Meta-Analyses of Randomized Controlled Trials
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kidney Disease: Improving Global Outcomes (KDIGO) Anemia Work Group. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int. Suppl. 2012, 2, 279–335. Available online: https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-Anemia-Guideline-English.pdf (accessed on 11 March 2020).
- Fishbane, S.; Spinowitz, B. Update on Anemia in ESRD and Earlier Stages of CKD: Core Curriculum 2018. Am. J. Kidney Dis. 2018, 71, 423–435. [Google Scholar] [CrossRef] [PubMed]
- Gafter-Gvili, A.; Schechter, A.; Rozen-Zvi, B. Iron Deficiency Anemia in Chronic Kidney Disease. Acta Haematol. 2019, 142, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Macdougall, I.C. Intravenous iron therapy in patients with chronic kidney disease: Recent evidence and future directions. Clin. Kidney J. 2017, 10, i16–i24. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Fishbane, S.; Bolton, W.K.; Winkelmayer, W.C.; Strauss, W.; Li, Z.; Pereira, B.J. Factors affecting response and tolerability to ferumoxytol in nondialysis chronic kidney disease patients. Clin. Nephrol. 2012, 78, 181–188. [Google Scholar] [CrossRef]
- Lu, M.; Cohen, M.H.; Rieves, D.; Pazdur, R. FDA report: Ferumoxytol for intravenous iron therapy in adult patients with chronic kidney disease. Am. J. Hematol. 2010, 85, 315–319. [Google Scholar] [CrossRef]
- Provenzano, R.; Schiller, B.; Rao, M.; Coyne, D.; Brenner, L.; Pereira, B.J. Ferumoxytol as an intravenous iron replacement therapy in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2009, 4, 386–393. [Google Scholar] [CrossRef] [Green Version]
- Bolton, W.K.; Fishbane, S.; Li, J.; Milich, L.; Brenner, R. 29: Increases in hemoglobin and the effect of ESA use in CKD patients treated with IV ferumoxytol [abstract]. Am. J. Kidney. Dis. 2009, 53, B29. [Google Scholar] [CrossRef]
- Spinowitz, B.S.; Kausz, A.T.; Baptista, J.; Noble, S.D.; Sothinathan, R.; Bernardo, M.V.; Brenner, L.; Pereira, B.J. Ferumoxytol for treating iron deficiency anemia in CKD. J. Am. Soc. Nephrol. 2008, 19, 1599–1605. [Google Scholar] [CrossRef] [Green Version]
- Coyne, D.W.; Kapoian, T.; Suki, W.; Singh, A.K.; Moran, J.E.; Dahl, N.V.; Rizkala, A.R. Ferric gluconate is highly efficacious in anemic hemodialysis patients with high serum ferritin and low transferrin saturation: Results of the Dialysis Patients’ Response to IV Iron with Elevated Ferritin (DRIVE) Study. J. Am. Soc. Nephrol. 2007, 18, 975–984. [Google Scholar] [CrossRef] [PubMed]
- Kapoian, T.; O’Mara, N.B.; Singh, A.K.; Moran, J.; Rizkala, A.R.; Geronemus, R.; Kopelman, R.C.; Dahl, N.V.; Coyne, D.W. Ferric gluconate reduces epoetin requirements in hemodialysis patients with elevated ferritin. J. Am. Soc. Nephrol. 2008, 19, 372–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strauss, W.E.; Dahl, N.V.; Li, Z.; Lau, G.; Allen, L.F. Ferumoxytol versus iron sucrose treatment: A post-hoc analysis of randomized controlled trials in patients with varying renal function and iron deficiency anemia. BMC Hematol. 2016, 16, 20. [Google Scholar] [CrossRef] [Green Version]
- Macdougall, I.C.; Strauss, W.E.; McLaughlin, J.; Li, Z.; Dellanna, F.; Hertel, J. A randomized comparison of ferumoxytol and iron sucrose for treating iron deficiency anemia in patients with CKD. Clin. J. Am. Soc. Nephrol. 2014, 9, 705–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hetzel, D.; Strauss, W.; Bernard, K.; Li, Z.; Urboniene, A.; Allen, L.F. A Phase III, randomized, open-label trial of ferumoxytol compared with iron sucrose for the treatment of iron deficiency anemia in patients with a history of unsatisfactory oral iron therapy. Am. J. Hematol. 2014, 89, 646–650. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Macdougall, I.C.; White, C.; Anker, S.D.; Bhandari, S.; Farrington, K.; Kalra, P.A.; McMurray, J.J.V.; Murray, H.; Tomson, C.R.V.; Wheeler, D.C.; et al. Intravenous iron in patients undergoing maintenance hemodialysis. N. Engl. J. Med. 2019, 380, 447–458. [Google Scholar] [CrossRef]
- Bhandari, S.; Kalra, P.A.; Kothari, J.; Ambühl, P.M.; Christensen, J.H.; Essaian, A.M.; Thomsen, L.L.; Macdougall, I.C.; Coyne, D.W. A randomized, open-label trial of iron isomaltoside 1000 (Monofer®) compared with iron sucrose (Venofer®) as maintenance therapy in haemodialysis patients. Nephrol. Dial. Transplant. 2015, 30, 1577–1589. [Google Scholar] [CrossRef] [Green Version]
- Singh, H.; Reed, J.; Noble, S.; Cangiano, J.L.; Van Wyck, D.B. Effect of intravenous iron sucrose in peritoneal dialysis patients who receive erythropoiesis-stimulating agents for anemia: A randomized, controlled trial. Clin. J. Am. Soc. Nephrol. 2006, 1, 475–482. [Google Scholar] [CrossRef]
- Onken, J.E.; Bregman, D.B.; Harrington, R.A.; Morris, D.; Buerkert, J.; Hamerski, D.; Iftikhar, H.; Mangoo-Karim, R.; Martin, E.R.; Martinez, C.O.; et al. Ferric carboxymaltose in patients with iron-deficiency anemia and impaired renal function: The REPAIR-IDA trial. Nephrol. Dial. Transplant. 2014, 29, 833–842. [Google Scholar] [CrossRef] [Green Version]
- Van Wyck, D.B.; Roppolo, M.; Martinez, C.O.; Mazey, R.M.; McMurray, S. A randomized, controlled trial comparing IV iron sucrose to oral iron in anemic patients with nondialysis-dependent CKD. Kidney Int. 2005, 68, 2846–2856. [Google Scholar] [CrossRef] [Green Version]
- Macdougall, I.C.; Bircher, A.J.; Eckardt, K.U.; Obrador, G.T.; Pollock, C.A.; Stenvinkel, P.; Swinkels, D.W.; Wanner, C.; Weiss, G.; Chertow, G.M. Iron management in chronic kidney disease: Conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int. 2016, 89, 28–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Lone, E.L.; Hodson, E.M.; Nistor, I.; Bolignano, D.; Webster, A.C.; Craig, J.C. Parenteral versus oral iron therapy for adults and children with chronic kidney disease. Cochrane Database Syst. Rev. 2019, 2, CD007857. [Google Scholar] [CrossRef] [PubMed]
- Shepshelovich, D.; Rozen-Zvi, B.; Avni, T.; Gafter, U.; Gafter-Gvili, A. Intravenous versus oral iron supplementation for the treatment of anemia in CKD: An updated systematic review and meta-analysis. Am. J. Kidney Dis. 2016, 68, 677–690. [Google Scholar] [CrossRef] [PubMed]
- Susantitaphong, P.; Alqahtani, F.; Jaber, B.L. Efficacy and safety of intravenous iron therapy for functional iron deficiency anemia in hemodialysis patients: A meta-analysis. Am. J. Nephrol. 2014, 39, 130–141. [Google Scholar] [CrossRef]
- Albaramki, J.; Hodson, E.M.; Craig, J.C.; Webster, A.C. Parenteral versus oral iron therapy for adults and children with chronic kidney disease. Cochrane Database Syst. Rev. 2012, 1, CD007857. [Google Scholar] [CrossRef]
- Rozen-Zvi, B.; Gafter-Gvili, A.; Paul, M.; Leibovici, L.; Shpilberg, O.; Gafter, U. Intravenous versus oral iron supplementation for the treatment of anemia in CKD: Systematic review and meta-analysis. Am. J. Kidney Dis. 2008, 52, 897–906. [Google Scholar] [CrossRef]
- Tagboto, S.; Cropper, L.; Turner, J.; Pugh-Clarke, K. The efficacy of a single dose of intravenous ferric carboxymaltose (Ferinject) on anaemia in a pre-dialysis population of chronic kidney disease patients. J. Ren. Care 2009, 35, 18–23. [Google Scholar] [CrossRef]
- Shao, Y.; Luo, W.; Xu, H.; Zhang, L.; Guo, Q. The efficacy of ferumoxytol for iron deficiency anemia: A meta-analysis of randomized controlled trials. Acta Haematol. 2019, 142, 125–131. [Google Scholar] [CrossRef]
- Rognoni, C.; Venturini, S.; Meregaglia, M.; Marmifero, M.; Tarricone, R. Efficacy and safety of ferric carboxymaltose and other formulations in iron-deficient patients: A systematic review and network meta-analysis of randomised controlled trials. Clin. Drug. Investig. 2016, 36, 177–194. [Google Scholar] [CrossRef] [Green Version]
- Moore, R.A.; Gaskell, H.; Rose, P.; Allan, J. Meta-analysis of efficacy and safety of intravenous ferric carboxymaltose (Ferinject) from clinical trial reports and published trial data. BMC Blood Disord. 2011, 11, 4. [Google Scholar] [CrossRef] [Green Version]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stewart, L.; Moher, D.; Shekelle, P. Why prospective registration of systematic reviews makes sense. Syst. Rev. 2012, 1, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirkham, J.J.; Altman, D.G.; Williamson, P.R. Bias due to changes in specified outcomes during the systematic review process. PLoS ONE 2010, 5, e9810. [Google Scholar] [CrossRef] [PubMed]
- Moher, D. The problem of duplicate systematic reviews. BMJ 2013, 347, f5040. [Google Scholar] [CrossRef] [PubMed]
- Terrin, N.; Schmid, C.H.; Lau, J. In an empirical evaluation of the funnel plot, researchers could not visually identify publication bias. J. Clin. Epidemiol. 2005, 58, 894–901. [Google Scholar] [CrossRef]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Schühlen, H. Pre-specified vs. post-hoc subgroup analyses: Are we wiser before or after a trial has been performed? Eur. Heart J. 2014, 35, 2055–2057. [Google Scholar] [CrossRef] [Green Version]
- Ioannidis, J.P. Why most discovered true associations are inflated. Epidemiology 2008, 19, 640–648. [Google Scholar] [CrossRef] [Green Version]
- Herrera-Gómez, F.; Chimeno, M.M.; Martín-García, D.; Lizaraso-Soto, F.; Maurtua-Briseño-Meiggs, Á.; Grande-Villoria, J.; Bustamante-Munguira, J.; Alamartine, E.; Vilardell, M.; Ochoa-Sangrador, C.; et al. Cholesterol-lowering treatment in chronic kidney disease: Multistage pairwise and network meta-analyses. Sci. Rep. 2019, 9, 8951. [Google Scholar] [CrossRef] [Green Version]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions—Version 5.1.0; The Cochrane Collaboration: London, UK, 2011; Available online: https://handbook-5-1.cochrane.org/ (accessed on 11 March 2020).
- Brown, S.; Hutton, B.; Clifford, T.; Coyle, D.; Grima, D.; Wells, G.; Cameron, C.A. Microsoft-Excel-based tool for running and critically appraising network meta-analyses: An overview and application of NetMetaXL. Syst. Rev. 2014, 3, 110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Systematic Reviews: Centre for Reviews and Dissemination’s (CRD) Guidance for Undertaking Reviews in Health Care; University of York: York, UK, 2008; Available online: https://york.ac.uk/media/crd/Systematic_Reviews.pdf (accessed on 11 March 2020).




| Iron Supplements † | SUCRA ‡ CKD 3A-5/dialysis § |
|---|---|
| Ferumoxytol 1020 mg/mo | 0.926/0.673 |
| Ferric carboxymaltose 750–1500 mg/mo | 0.808/NA |
| Iron sucrose ≥400 mg/mo | 0.598/0.840 |
| Iron sucrose 100–300 mg/mo | 0.567/0.614 |
| Iron isomaltoside 500 mg/mo | NA/0.615 |
| Iron gluconate 1000–1500 mg/mo | 0.502/0.439 |
| Iron polymaltose 500 mg/mo | NA/0.293 |
| Ferric carboxymaltose >1500 mg/mo | 0.280/NA |
| Iron isomaltoside 1000 mg/mo | 0.248/NA |
| Iron P.O. | 0.091/0.176 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adler, M.; Herrera-Gómez, F.; Martín-García, D.; Gavid, M.; Álvarez, F.J.; Ochoa-Sangrador, C. The Impact of Iron Supplementation for Treating Anemia in Patients with Chronic Kidney Disease: Results from Pairwise and Network Meta-Analyses of Randomized Controlled Trials. Pharmaceuticals 2020, 13, 85. https://0-doi-org.brum.beds.ac.uk/10.3390/ph13050085
Adler M, Herrera-Gómez F, Martín-García D, Gavid M, Álvarez FJ, Ochoa-Sangrador C. The Impact of Iron Supplementation for Treating Anemia in Patients with Chronic Kidney Disease: Results from Pairwise and Network Meta-Analyses of Randomized Controlled Trials. Pharmaceuticals. 2020; 13(5):85. https://0-doi-org.brum.beds.ac.uk/10.3390/ph13050085
Chicago/Turabian StyleAdler, Marcel, Francisco Herrera-Gómez, Débora Martín-García, Marie Gavid, F. Javier Álvarez, and Carlos Ochoa-Sangrador. 2020. "The Impact of Iron Supplementation for Treating Anemia in Patients with Chronic Kidney Disease: Results from Pairwise and Network Meta-Analyses of Randomized Controlled Trials" Pharmaceuticals 13, no. 5: 85. https://0-doi-org.brum.beds.ac.uk/10.3390/ph13050085