1. Introduction
Depressive disorders are common psychiatric disorders characterized by inflammatory conditions, oxidative stress, overproduction of nitric oxide and imbalance of antioxidant [
1], whereas 121 million people affected by it [
2]. According to the World Health Organization (WHO) and Years Lived with Disability (YLDs) states that depression is a major cause of disability and fourth leading psychiatric disorders in the world [
2]. Depression may be probably comorbid with the other disorders for example obesity, anxiety, diabetes, Alzheimer’s disease, schizophrenia [
3]. Oxidative stress considered for the major cause of depressive disorders. Hence, it is an important therapeutic target for the treatment of depression and its associated psychiatric disorders [
3].
Oxidative stress (OS) is only the imbalance of oxidants and antioxidants, whereas it framed as a typical result of aerobic metabolism [
4]. Both enzymatic (superoxide dismutase, catalase, glutathione peroxidase) and nonenzymatic (Vitamin C, Vitamin E, flavonoids) techniques are engaged with the antioxidant defense and antioxidant efficacy of any particle or molecule relies upon the cooxidant [
4]. The oxidative stress is typically a complex process, which occurs due to the production of reactive nitrogen species (RNS) and reactive oxygen species (ROS) [
5,
6]. ROS is a continuous generation process of body metabolism, which helps in the management of different biologic and pathologic process, namely, immune system, lipid peroxidation, phagocytes activation [
7,
8]. Additionally, overproduction of ROS may cause oxidative damage by targeting the weak position of the components such as unsaturated fatty acids in membranes, thiol groups in proteins [
9,
10]. Several chronic health diseases are reported due to the overproduction of lipid peroxidation. According to several studies, free radical may cause several neuropsychiatric disorders and also mediate a neuronal dysfunction which led to schizophrenia with some other major depression [
11,
12,
13]. Oxidative stress has a significant influence in the advancement of chronic and degenerative health diseases, for example, malignant growth [
14], joint inflammation, aging, immune system issue, cardiovascular and neurodegenerative ailments [
15]. The human body has a few mechanisms to neutralize oxidative stress by antioxidants, which are either provided through natural foods or additionally supplements [
14,
16]. Vitamin C and E together act as antioxidant defense, whereas the combinations of vitamin E/C (400 IU: 500 mg) are effective against the schizophrenia [
17]. In addition, the N-acetyl-cysteine (NAC) twice per day (1 g) is useful for bipolar disorder [
18] and even in depression [
13]. Such investigations have likewise opened the potential roads of new treatment systems utilizing antioxidants as adjunctive treatment in the neuropsychiatric disorders and also naturally derived food substances have been used as a great potential over the last two decades and numerous biologic activities demonstrating promising aspect on anti-inflammatory, anti-apoptotic and modulatory effects [
19].
In anxiety disorders, benzodiazepines are gradually substituted by antidepressants, which are not only useful in depression, but also in anxiety disorders for acute and long-term treatment [
20]. Although, the tricyclic antidepressants and monoamine oxidase inhibitors are first generation antidepressant drugs, which poses toxicity in higher dose with several undesirable adverse effects and slow onset of action [
21,
22]. However, the new generation (second and third) antidepressant drugs (selective serotonin reuptake inhibitors and serotonin and norepinephrine reuptake inhibitors) are more targets selective. However, they also reported several major adverse effects, including gastrointestinal, CNS problems, seizure, insomnia, dry mouth and elevation of blood pressure [
22]. So, researchers are trying to explore new potential lead compounds from medicinal plants having several biologic properties, whereas early tests (in vivo and in vitro) was followed to evaluate the possible activity and toxicity level of the lead compounds [
21]. Three visual methodologies, including surface plasmon resonance, scintillation proximity assay and isothermal titration calorimetry are used to identify whether the compounds bind to the receptor. Later, the virtual screening, medicinal chemistry, combinatorial chemistry and computer-aided drug design (molecular docking, ADME/T) was followed to develop a new lead compound [
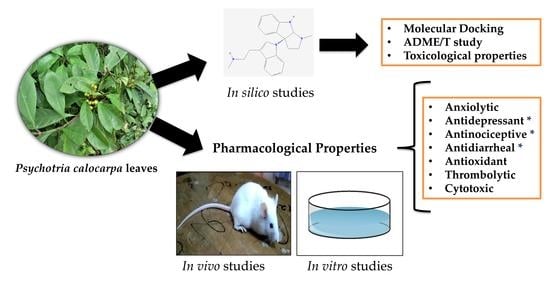
21]. Despite this long and time-consuming process, natural products are the topic of interest in the treatment of several diseases. Hence, our present study design for biologic properties of
Psychotria calocarpa using in vivo and in vitro assay with in silico study to explore a potential lead compound for chronic diseases.
Psychotria calocarpa belongs to the Rubiaceae family, which is locally known as ranga bhutta (Tanchangya, Chittagong, Bangladesh) [
23]. Plants of the genus
Psychotria have been used in folk medicine for the treatment of constipation in Malaysia [
24]. The local Tanchangya community of Bangladesh used the plant in the treatment of hysteria. A compound named psychotriasine was isolated from the leaves of
P. calocarpa by NMR analysis [
25]. However, there is no scientific report on the biologic activity of
P. calocarpa leaves. Hence, the present study has been designed to evaluate the biologic properties, namely, the anxiolytic, locomotor, antidepressant, antinociceptive, antidiarrheal, antioxidant, thrombolytic and cytotoxic activities as well as the semiqualitative phytochemical analysis of the methanol extract of
P. calocarpa leaves. The objective of the study is to find a lead compound from
P. calocarpa in moderating neuropsychiatric disorders by suppressing the oxidative stress signaling. As the plant was reported to contain one compound by NMR analysis, we used the computational studies using molecular docking, absorption, distribution, metabolism, excretion and toxicity (ADME/T) and toxicological properties analysis of the compound to understand the selected activities.
3. Materials and Methods
3.1. Chemicals
Diazepam, fluoxetine, loperamide and diclofenac sodium were acquired from Square Pharmaceuticals, Ltd. (Dhaka, Bangladesh), while streptokinase and Vincristine sulfate (2 mg/vial) was purchased from Beacon Pharmaceuticals, Ltd. Bangladesh. Aluminum chloride, 1, 1-diphenyl2-picrylhydrazyl (DPPH), gallic acid and Folin–Ciocâlteu reagent (FCR) were procured from Sigma-Aldrich (Bangalore, India). Ascorbic acid and quercetin were procured from BDH Chemicals, Ltd. (Poole, UK). Absorbance was taken by UV-vis spectrophotometer (UVmini-1240, Shimadzu, Japan). The other chemicals were purchased in analytical grades from local trader through Taj Scientific, Ltd. (Chittagong, Bangladesh)
3.2. Animals
Swiss albino mice of either sex weighing about 25–35 g (six–seven weeks) were purchased from the Jahangirnagar University, Dhaka −1343, Bangladesh. The mice were familiarized with the standard conditions by maintaining in room temperature 25 ± 2 °C, relative humidity 55–60% with a 12 h light/dark cycle. The animals were provided with proper food pellets and water supply. The study was conducted under the Animal Research: Reporting of In Vivo Experiments (ARRIVE) Guidelines for in vivo study and the Institutional Animal Ethical Committee, Department of Pharmacy, International Islamic University Chittagong, Bangladesh approved the study protocol under the reference number Pharm/P&D/138/13-19 [
82].
3.3. Collection and Preparation of Methanol Extract
The leaves of P. calocarpa were collected from the Hajarikhil Hill tract, Chittagong, Bangladesh in the month of February 2019, which was identified by Professor Dr Shaikh Bokhtear Uddin, Department of Botany, University of Chittagong, Bangladesh. The leaves were collected in fresh condition from the shrubs (1–1.5 m). At first, the leaves were washed with water and later shaded dried at 55–60 °C for seven days. The dried leaves were ground into the coarse powder (1.18 mm) by a grinder (NOWAKE, Japan) and soaked the powder (500 g) in methanol (2 L) for 15 days with occasional shaking and stirring. The extraction process was done in a standard laboratory condition (27 ± 2 °C). After 15 days, the filtration was done using Whatman #1 filter paper and the final filtrate was evaporated in the water bath at 45 °C. Lastly, the obtained sticky semi-solid part of the methanol extract of P. calocarpa leaves (MEPC) was preserved in 4 °C.
3.4. Semiqualitative Phytochemical Screening
The semiqualitative phytochemical analysis of the methanol extract of
P. calocarpa leaves was carried out by the standard methodology for testing the alkaloid, glycosides, tannins, saponins, resins, carbohydrate, flavonoid, phenols, terpenoids, quinones and proteins [
83,
84,
85], which briefly presented in the
Supplementary Section.
3.5. Experimental Design
In this study, five Swiss albino mice of either sex were used in each group (control, standard and MEPC). The MEPC group was administrated 200 and 400 mg/kg accordance with their body weight (BW), whereas the control group was administrated 1% Tween-80 in water (10 mL/kg, BW). Diazepam (1 mg/kg, BW, IP) was used for the anxiolytic (elevated plus maze test, hole–board test and light and dark test) and locomotor activity (open field test), while fluoxetine (10 mg/kg, BW, IP) was used for antidepressant activity (forced swim test and tail suspension test). Diclofenac sodium (10 mg/kg BW, IP) and loperamide (5 mg/kg BW, IP) were used for testing the antinociceptive (acetic acid-induced writhing test and formalin-induced licking test) and antidiarrheal activity (castor oil-induced diarrhea and intestinal motility test), respectively.
3.6. Anxiolytic Activity
3.6.1. Elevated Plus Maze (EPM) Test
The elevated plus maze (EPM) test was used to examine the anxiolytic activity of plant extract MEPC in mice [
86]. The apparatus assembled by two open arms (5 × 10 cm
2) and two closed arms (5 × 10 × 15 cm
3), which was elevated from the floor in the height of 40 cm. The experiment of each group was followed, as described in
Section 3.5. Thirty minutes after the treatment, each treated mice was placed in the middle point of the EPM apparatus facing towards the closed arms and recorded for 5 min. The percentage of entries and time spent was calculated by the following equation.
3.6.2. Hole-Board Test (HBT)
The anxiolytic activity was assessed by the hole–board test, which consists of 16 evenly distributed holes 3 cm in diameter in a wooden space (40 × 40 × 25 cm
3). The apparatus elevated from the floor at the height of 25 cm. The dosing of each group was followed, as described in
Section 3.5. After thirty minutes of the treatment, each treated mice individually was placed in the center of the board. The animals were allowed to move freely and the movement recorded for 5 min [
87].
3.6.3. Light and Dark Box Test (LDT)
The anxiolytic activity of MEPC was evaluated by the light and dark test, which comprised of the four-sided box (46 × 27 × 30 cm
3). The box divided by 18 × 27 cm
2 into a small area and 27 × 27 cm
2 into a large area with a door, which positioned in the center of the dividing wall. The dosing of each group was followed, as described in
Section 3.5. Thirty minutes after the administration, each treated mice was placed individually in the dark compartment and recorded the time spent in the compartment for 5 min [
88].
3.7. Locomotor Activity
Open Field Test (OFT)
The locomotor activity of MEPC was assessed by the open field test according to the previously described method of Gupta et al. (1971) [
89]. A four-sided box with a measurement of 60 × 60 × 60 cm
3 with 25 equal squares (5 × 5 cm
2), which alternatively highlighted in black and white. The dosing of each group was followed, as described in
Section 3.5. Immediately after the treatment, each mouse was individually placed in the apparatus for 3 min at 0, 30, 60, 90 and 120 min intervals, where the number of squares moved was recorded.
3.8. Antidepressant Activity
3.8.1. Forced Swim Test (FST)
The antidepressant activity of MEPC and standard drug fluoxetine was evaluated by forced swimming test by previously described protocol [
90]. The FST assessed in a transparent glass beaker (25 × 15 × 25 cm
3) which occupied with water (25 ± 1 °C) up to 15 cm. The dosing of each group was followed, as mentioned in
Section 3.5. Thirty minutes after the administration, each mouse was individually placed in the apparatus for forced swimming. The study conducted for 6 min, where the first 2 min was used for initial adjustment and the last 4 min was considered as the immobility time.
where, A = immobile time in the control group; B = immobile time in the test group.
3.8.2. Tail Suspension Test (TST)
The antidepressant activity of MEPC and standard drug fluoxetine was evaluated by forced swimming test by the previously described method of Steru et al. 1985 [
91]. The treatment of each group was followed, as mentioned in
Section 3.5. After the administration, each mice group was individually hanged by the end of the tail (approximately 1 cm) using tape. The study conducted for 6 min, where the first 2 min was used for initial adjustment and the last 4 min was considered as the immobility time.
where, A = immobile time in the control group; B = immobile time in the test group.
3.9. Antinociceptive Activity
3.9.1. Acetic Acid-Induced Writhing Inhibition Test
The acetic acid-induced writhing test was used for the evaluation of the antinociceptive activity of MEPC by the previously described method [
92]. The treatment followed the process, as mentioned in
Section 3.5. Thirty minutes after the administration, 0.7% acetic acid (
v/v) was injected in the intraperitoneal route of mice. The total writhing by each mouse was recorded for 15 min. Following equation was used to evaluate the percentage of inhibition:
where, A = mean number of writhing by control group; B = mean number of writhing by test group.
3.9.2. Formalin-Induced Licking Test
The antinociceptive activity of MEPC was assessed by the formalin-induced licking test, as described by Okokon et al. 2010 [
93]. The treatment followed the process, as mentioned in
Section 3.5. After 30 min of the treatment, 20 μL of formalin solution (2.5% v/v) was injected into the sub-plantar region (hind paw) of the mice. The licking times were recorded as early phase (0–5 min) and late phase (15–30 min). Following equation was used to evaluate the percentage of inhibition:
where, A = mean licking time by control group; B = mean licking time by test group.
3.10. Antidiarrheal Activity
3.10.1. Castor Oil-Induced Diarrhea
The antidiarrheal activity was evaluated by castor oil-induced diarrhea test following the previously described method [
94]. Each mouse was fasted for 24 h before starting the experiment and treatment followed the process as mentioned in
Section 3.5. After one hour, 0.5 mL castor oil-induced orally and placed each mouse individually in a separate cage with blotting paper. The total number of feces counted for 4 h and replaced the blotting paper in every one hour after. The following equation was followed for the calculation of percentage inhibition of defecation:
where, A = average feces number of the control group; B = average feces number of the test group.
3.10.2. Intestinal Motility by Charcoal Marker
The Intestinal motility by the charcoal marker for the antidiarrheal study of MEPC was evaluated by Mascolo et al. 1994 [
95]. Each mouse was fasted for 24 h before starting the experiment and treatment followed the process as mentioned in
Section 3.5. After one hour, each mouse received 1 mL charcoal solution (10% charcoal in 5% gum acacia). One hour after charcoal administration, each mouse was sacrificed and measured the distance traveled by the charcoal marker and total length of the intestine. The following equation was followed for the calculation of the percentage of inhibition and peristalsis index:
where, A = Distance travel by the control (cm); B = Distance travel by the test groups (cm)
3.11. Antioxidant Activity
3.11.1. DPPH Free Radical-Scavenging Assay
The antioxidant activity of MEPC was evaluated by DPPH free radical-scavenging assay as described by Braca et al. 2001 [
96]. In this experiment, a serially diluted concentration (15.625–500 µg/mL) was followed for the MEPC and standard antioxidant ascorbic acid. Three milliliters of 0.004% DPPH solution (4 mg DPPH in 100 mL of 95% methanol) was mixed with serially diluted concentration (0.1 mL) and allowed to incubate for 30 min at room temperature (25 °C) in the dark condition. The absorbance was read at 517 nm. Additionally, the study followed in triplicate manner.
3.11.2. Total Phenol Content (TPC)
The semi-quantitative phytochemical analysis of total phenol content (TPC) of the MEPC was assessed by Reza et al. 2018 [
97]. Here, 2.5 mL of 10% Folin–Ciocâlteu reagent and 2.5 mL of Na
2CO
3 (20%), respectively was added to the 500-μg/mL extract and the solution was filled up to 10 mL by distilled water (D.W.). The solution was allowed to incubate for 20 min at 25 °C and the absorbance was read at 765 nm. Additionally, the study followed in triplicate manner. The TPC of the MEPC measured from the calibration curve of gallic acid solution (standard), whereas the TPC was expressed in milligrams of gallic acid equivalents (GAE) per gram of extracts (mg GAE/g extract).
3.11.3. Total Flavonoid Content (TFC)
The total flavonoid content (TFC) of the MEPC was assessed, according to Reza et al. 2018 [
97]. Here, 500 μg/mL extract mixed with methanol (1.5 mL), 10% AlCl
3 (0.1 mL), 1 M CH
3COOK (0.1 mL) and distilled water (2.8 mL), respectively. Then, the solution was allowed to incubate for 30 min at 25 °C and the absorbance was taken at 415 nm. Additionally, the study followed in triplicate manner. The TFC of the MEPC measured from the calibration curve of quercetin solution (standard), whereas the TFC was expressed in milligrams of quercetin equivalents (QE) per gram of extracts (mg QE/g extract).
3.12. Thrombolytic Activity
The thrombolytic activity of MEPC leaves was evaluated by human blood clot lysis activity as described by Prasad et al. 2006 [
98]. In total ten male- female 20–25 years (
n = 10) healthy volunteer (non-smokers, no history of medication in last two week) were used for this study and 3 mL of blood withdrawn from the venous and 0.5 mL per Eppendorf distributed. The Eppendorf was previously weight. Then, the Eppendorf with blood was incubated for 45 min at 37 °C to form the clot. After forming a clot, the obtained serum in the clot was absolutely removed and again reweighed each Eppendorf. Briefly, 100 μL of MEPC extract (10 mg/mL) added to each Eppendorf. Similar protocols were followed for the standard drug streptokinase (100 μL) and control distilled water (100 μL). All the Eppendorf was allowed to incubate for 90 min at 37 °C and observed clot lysis. Again, the released fluid after incubation was removed and reweighed [
68].
3.13. Brine Shrimp Lethality Bioassay
The brine shrimp lethality bioassay was used to evaluate the cytotoxic activity of MEPC as depicted by Meyer et al., 1982 [
99]. The cytotoxicity of MEPC evaluated using simple organism
Artemia salina. Here, 2.5 g brine shrimp cyst added in the artificial seawater (3.8% NaCl solution/L,
w/v) in a beaker (1 L) by maintaining the temperature at 25 ± 1 °C and pH (8.0) with proper light intensity (60 W). The distance between light and brine shrimp beaker was 9 cm. The shrimp eggs hatched for 48 h for maturing the shrimp. In this experiment, a serially diluted concentration (15.625–1000 µg/mL) was followed for the MEPC, while 3.13–100 μg/mL was used for vincristine sulfate. Finally, all test tubes containing 5 mL freshly prepared artificial seawater, where 10 nauplii transferred carefully. Additionally, the study followed in triplicate manner. After 24 h, all test tubes inspected by an amplifying glass and the number of living nauplii in each test tube was observed and recorded [
68].
where, N
0 = the number of nauplii taken; N
1 = the number of nauplii dead.
3.14. In Silico Study
3.14.1. Molecular Docking Analysis
The isolated compounds from the leaves of
P. calocarpa by NMR analysis [
25] was subjected for molecular docking study by following the protocol of Sastry et al. 2013, which briefly explained in Tareq, 2019 [
100,
101]. The 3D structure of receptors/enzymes were retrieved from the Protein Data Bank (
https://www.rcsb.org/structure): potassium channel KCSA-FAB receptor (PDB ID: 4UUJ), structure of the ts3 human serotonin transporter receptor (PDB ID: 5I6X), cyclooxygenase-1 (PDB ID: 2OYE), cyclooxygenase-2 (PDB ID: 3HS5), 5-HT3 receptor (PDB: 5AIN), M3 muscarinic acetylcholine receptor (PDB: 4U14), urate oxidase (PDB: 1R4U), human tissue plasminogen activator (PDB: 1A5H) and human estrogen receptor (PDB: 3ERT) [
102]. Molecular docking study was analyzed by Schrödinger Mestro (v11.1).
3.14.2. ADME/T and Toxicological Properties Analysis
The absorption, distribution, metabolism, excretion and toxicity (ADME/T) analysis of psychotriasine was analyzed by the Lipinski’s rules [
80] and Veber’s rules [
81], whereas the toxicological properties assessed by admetSAR (Online tool). The ADME/T analysis was assessed by SwissADME (
http://www.swissadme.ch/) and QikProp (Schrödinger v11.1) [
103].
3.15. Statistical Analysis
Values represented as mean ± S.E.M (standard error mean). * p < 0.01 and ** p < 0.001 considered as significantly different from the control; one-way ANOVA (Dunnett’s test) was carried out using GraphPad Prism version 8.4., whereas two-way ANOVA with repeated measures was followed for the open filed test.