COVID-19 Vaccines: A Review of the Safety and Efficacy of Current Clinical Trials
Abstract
:1. Introduction
2. BiONTech (BNT162b1 and BNT162b2)
3. Moderna (mRNA1273)
4. ChadOx1 nCoV-19 (AZD1222)
5. Convidecia (Adenovirus Type-5 Vectored COVID-19 Vaccine)
6. Gam-COVID-Vac (Recombinant Adenovirus Type 26 and Recombinant Adenovirus Type 5 Vaccine)
7. Covovax (NVAX-CoV2373)
8. WIV04-Strain Inactivated SARS-CoV-2 Vaccine
9. BBIBP-CorV
10. Coronavac Vaccine
11. Ad26.COV2.S
12. Covaxin (BBV 152)
13. Challenges
14. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Weekly Epidemiology Update 23 February 2021. WHO Situation Report. 2021. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update---23-february-2021 (accessed on 25 March 2021).
- Bonam, S.R.; Kotla, N.G.; Bohara, R.A.; Rochev, Y.; Webster, T.J.; Bayry, J. Potential immuno-nanomedicine strategies to fight COVID-19 like pulmonary infections. Nano Today 2021, 36, 101051. [Google Scholar] [CrossRef] [PubMed]
- Pardi, N.; Hogan, M.J.; Weissman, D. Recent advances in mRNA vaccine technology. Curr. Opin. Immunol. 2020, 65, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, M.J.; Lyke, K.E.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Neuzil, K.; Raabe, V.; Bailey, R.; Swanson, K.A.; et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature 2020, 586, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Sahin, U.; Muik, A.; Derhovanessian, E.; Vogler, I.; Kranz, L.M.; Vormehr, M.; Baum, A.; Pascal, K.; Quandt, J.; Maurus, D.; et al. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T-cell responses. Nature 2020, 586, 594–599. [Google Scholar] [CrossRef]
- Sette, A.; Moutaftsi, M.; Moyron-Quiroz, J.; McCausland, M.M.; Davies, D.H.; Johnston, R.J.; Peters, B.; Benhnia, M.R.-E.-I.; Hoffmann, J.; Su, H.-P.; et al. Selective CD4+ T Cell Help for Antibody Responses to a Large Viral Pathogen: Deterministic Linkage of Specificities. Immunnology 2008, 28, 847–858. [Google Scholar] [CrossRef] [Green Version]
- Walsh, E.E.; Frenck, R.W.; Falsey, A.R.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Neuzil, K.; Mulligan, M.J.; Bailey, R.; et al. Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates. N. Engl. J. Med. 2020, 383, 2439–2450. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Jackson, L.A.; Anderson, E.J.; Rouphael, N.G. An mRNA Vaccine against SARS-CoV-2-Preliminary Report. N. Engl. J. Med. 2020, 383, 1920–1931. [Google Scholar] [CrossRef]
- Xia, S.; Duan, K.; Zhang, Y. Effect of an Inactivated Vaccine Against SARS-CoV-2 on Safety and Immuno-genicity Outcomes: Interim Analysis of 2 Randomized Clinical Trials. JAMA 2020, 324, 951–960. [Google Scholar] [CrossRef] [PubMed]
- Xia, S.; Zhang, Y.; Wang, Y. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: A randomised, double-blind, placebo-controlled, phase 1/2 trial. Lancet Infect. Dis. 2021, 21, 39–51. [Google Scholar] [CrossRef]
- Folegatti, P.M.; Ewer, K.J.; Aley, P.K. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: A preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet 2020, 396, 467–478. [Google Scholar] [CrossRef]
- Ramasamy, M.N.; Minassian, A.M.; Ewer, K.J.; Flaxman, A.L.; Folegatti, P.M.; Owens, D.R.; Voysey, M.; Aley, P.K.; Angus, B.; Babbage, G.; et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): A single-blind, randomised, controlled, phase 2/3 trial. Lancet 2020, 396, 1979–1993. [Google Scholar] [CrossRef]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Zhu, F.C.; Li, Y.H.; Guan, X.H. Safety, tolerability, and immunogenicity of a recombinant adenovi-rus type-5 vectored COVID-19 vaccine: A dose-escalation, open-label, non-randomised, first-in-human trial. Lancet 2020, 395, 1845–1854. [Google Scholar] [CrossRef]
- Zhu, F.-C.; Guan, X.-H.; Li, Y.-H.; Huang, J.-Y.; Jiang, T.; Hou, L.-H.; Li, J.-X.; Yang, B.-F.; Wang, L.; Wang, W.-J.; et al. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: A randomised, double-blind, placebo-controlled, phase 2 trial. Lancet 2020, 396, 479–488. [Google Scholar] [CrossRef]
- ClinicalTrials.Gov. Phase III Trial of A COVID-19 Vaccine of Adenovirus Vector in Adults 18 Years Old and Above. Available online: https://clinicaltrials.gov/ct2/show/NCT04526990 (accessed on 18 March 2021).
- Logunov, D.Y.; Dolzhikova, I.V.; Zubkova, O.V. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: Two open, non-randomised phase 1/2 studies from Russia. Lancet 2020, 396, 887–897. [Google Scholar] [CrossRef]
- Logunov, D.Y.; Dolzhikova, I.V.; Shcheblyakov, D.V. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: An interim analysis of a randomised con-trolled phase 3 trial in Russia. Lancet 2021, 397, 671–681. [Google Scholar] [CrossRef]
- Keech, C.; Albert, G.; Cho, I. Phase 1-2 Trial of a SARS-CoV-2 Recombinant Spike Protein Nano-particle Vaccine. N. Engl. J. Med. 2020, 383, 2320–2332. [Google Scholar] [CrossRef]
- Mahase, E. Covid-19: Novavax vaccine efficacy is 86% against UK variant and 60% against South African variant. BMJ 2021, 372, n296. [Google Scholar] [CrossRef]
- Taylor, N.P. Novavax COVID-19 vaccine 90% efficacious in phase 3, but protection plummets against one variant. 2021. Available online: https://www.fiercebiotech.com/biotech/novavax-covid-19-vaccine-90-efficacious-phase-3-but-protection-plummets-against-one-variant (accessed on 9 April 2021).
- Chakraborty, S.; Mallajosyula, V.; Tato, C.M.; Tan, G.S.; Wang, T.T. SARS-CoV-2 vaccines in advanced clinical trials: Where do we stand? Adv. Drug Deliv. Rev. 2021, 172, 314–338. [Google Scholar] [CrossRef]
- Zhang, Y.; Zeng, G.; Pan, H. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: A randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 2021, 21, 181–192. [Google Scholar] [CrossRef]
- Anadolu Agency. Decision Based on Results of Country’s Phase III Trials That Put Estimated Vaccine Efficacy at 65.3%, Says Official. Available online: https://www.astrazeneca.com/media-centre/press-releases/2021/azd1222-us-phase-iii-primary-analysis-confirms-safety-and-efficacy.html (accessed on 18 March 2021).
- Mercado, N.B.; Zahn, R.; Wegmann, F. Single-shot Ad26 vaccine protects against SARS-CoV-2 in rhesus macaques. Nature 2020, 586, 583–588. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Chandrashekar, A.; Zahn, R.; Wegmann, F.; Yu, J.; Mercado, N.B.; McMahan, K.; Martinot, A.J.; Piedra-Mora, C.; Beecy, S.; et al. Low-Dose Ad26.COV2.S Protection Against SARS-CoV-2 Challenge in Rhesus Macaques. bioRxiv 2021. [Google Scholar] [CrossRef]
- Stephenson, K.E.; Le Gars, M.; Sadoff, J.; de Groot, A.M.; Heerwegh, D.; Truyers, C.; Atyeo, C.; Loos, C.; Chandrashekar, A.; McMahan, K.; et al. Immunogenicity of the Ad26.COV2.S Vaccine for COVID-19. JAMA 2021. [Google Scholar] [CrossRef]
- Sadoff, J.; Le Gars, M.; Shukarev, G.; Heerwegh, D.; Truyers, C.; De Groot, A.M.; Stoop, J.; Tete, S.; Van Damme, W.; Leroux-Roels, I.; et al. Interim Results of a Phase 1–2a Trial of Ad26.COV2.S Covid-19 Vaccine. New Engl. J. Med. 2021. [Google Scholar] [CrossRef]
- Yadav, P.D.; Ella, R.; Kumar, S.; Patil, D.R.; Mohandas, S.; Shete, A.M.; Vadrevu, K.M.; Bhati, G.; Sapkal, G.; Kaushal, H.; et al. Immunogenicity and protective efficacy of inactivated SARS-CoV-2 vaccine candidate, BBV152 in rhesus macaques. Nat. Commun. 2021, 12, 1–11. [Google Scholar] [CrossRef]
- Ella, R.; Vadrevu, K.M.; Jogdand, H.; Prasad, S.; Reddy, S.; Sarangi, V.; Ganneru, B.; Sapkal, G.; Yadav, P.; Abraham, P.; et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBV152: A double-blind, randomised, phase 1 trial. Lancet Infect. Dis. 2021, 21, 637–646. [Google Scholar] [CrossRef]
- Ella, R.; Vadrevu, K.M.; Jogdand, H.; Prasad, S.; Reddy, S.; Sarangi, V.; Ganneru, B.; Sapkal, G.; Yadav, P.; Abraham, P.; et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBV152: Interim results from a double-blind, random-ised, multicentre, phase 2 trial, and 3-month follow-up of a double-blind, randomised phase 1 trial. Lancet Infect. Dis. 2021. [Google Scholar] [CrossRef]
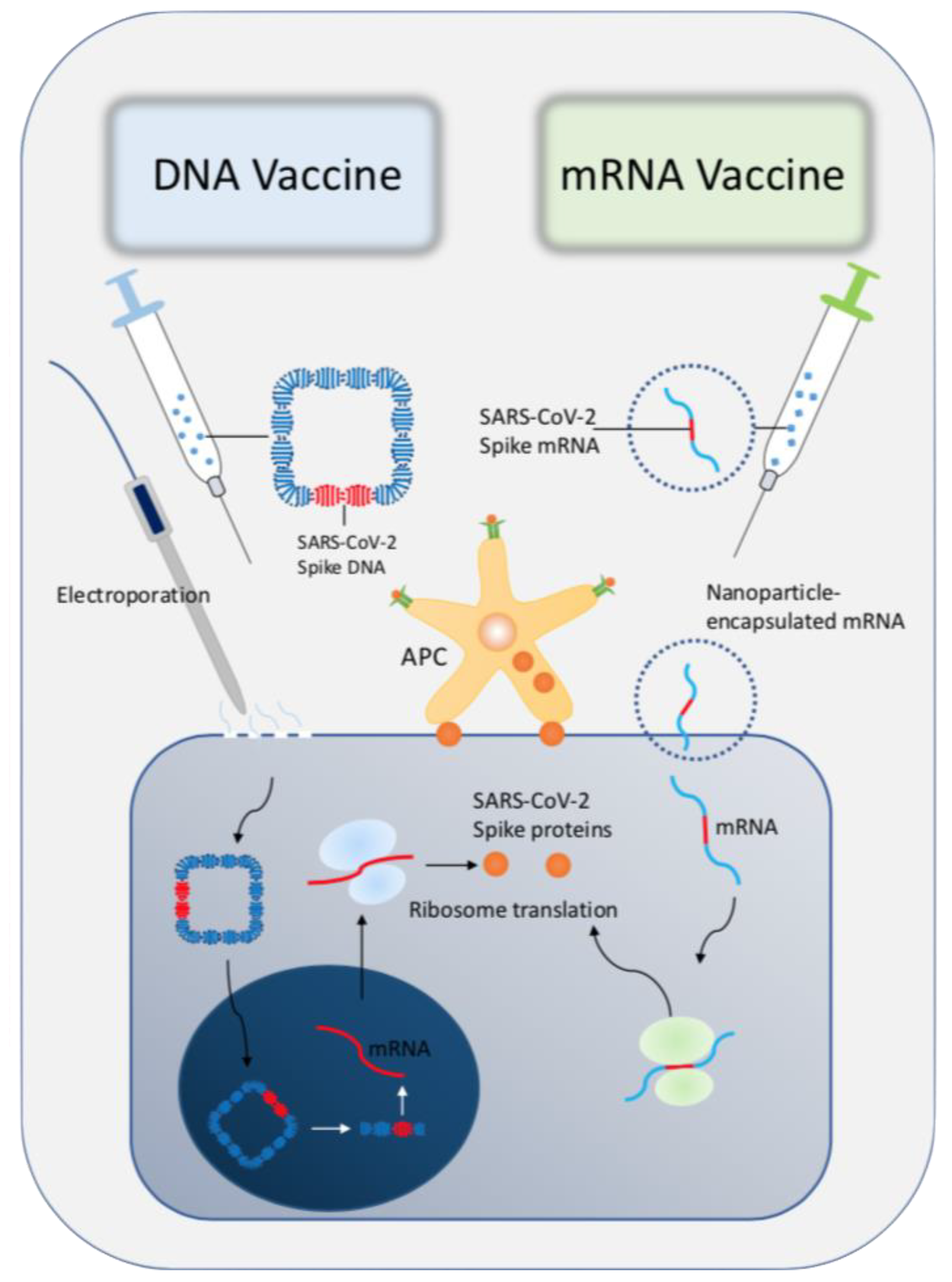
- Porter, K.R.; Raviprakash, K. DNA Vaccine Delivery and Improved Immunogenicity. Curr. Issues Mol. Biol. 2017, 22, 129–138. [Google Scholar] [CrossRef]
- Li, L.; Petrovsky, N. Molecular mechanisms for enhanced DNA vaccine immunogenicity. Expert Rev. Vaccines 2016, 15, 313–329. [Google Scholar] [CrossRef] [Green Version]
- Suschak, J.J.; Williams, J.A.; Schmaljohn, C.S. Advancements in DNA vaccine vectors, non-mechanical delivery methods, and molecular adjuvants to increase immunogenicity. Hum. Vaccines Immunother. 2017, 13, 2837–2848. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.A. A Comparison of Plasmid DNA and mRNA as Vaccine Technologies. Vaccines 2019, 7, 37. [Google Scholar] [CrossRef] [Green Version]
- Ritchie, H.; Beltekian, D.; Mathieu, E.; Hasell, J.; Macdonald, B.; Giattino, C.; Appel, C.; Roser, M.; Yunits, B.; van Woerden, E.; et al. Statistics and Research: Coronavirus (COVID-19) Vaccinations. 2021. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 22 March 2021).
- Liu, X.; Liu, C.; Liu, G.; Luo, W.; Xia, N. COVID-19: Progress in diagnostics, therapy and vaccination. Theranostics 2020, 10, 7821–7835. [Google Scholar] [CrossRef] [PubMed]
- Karpinski, T.M.; Ozarowski, M.; Seremak-Mrozikiewicz, A.; Wolski, H.; Wlodkowic, D. The 2020 race to-wards SARS-CoV-2 specific vaccines. Theranostics 2021, 11, 1690–1702. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Solidarity Vaccines Trial Expert Group. Draft Landscape and Tracker of COVID-19 Candidate Vaccines; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Madjid, M.; Safavi-Naeini, P.; Solomon, S.D.; Vardeny, O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020, 5, 831–840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smeeth, L.; Thomas, S.L.; Hall, A.J.; Hubbard, R.; Farrington, P.; Vallance, P. Risk of Myocardial Infarction and Stroke after Acute Infection or Vaccination. New Engl. J. Med. 2004, 351, 2611–2618. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwong, J.C.; Schwartz, K.L.; Campitelli, M.A. Acute Myocardial Infarction after Laboratory-Confirmed Influenza Infection. N. Engl. J. Med. 2018, 378, 345–353. [Google Scholar] [CrossRef]
- Soumya, R.S.; Unni, T.G.; Raghu, K.G. Impact of COVID-19 on the Cardiovascular System: A Review of Available Reports. Cardiovasc. Drugs Ther. 2020, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.J.; Rouphael, N.G.; Widge, A.T. Safety and Immunogenicity of SARS-CoV-2 mRNA-1273 Vaccine in Older Adults. N. Engl. J. Med. 2020, 383, 2427–2438. [Google Scholar] [CrossRef] [PubMed]
- Andreas Greinacher, T.T.; Theodore, E.; Warkentin, K.W.; Kyrle, P.; Eichinger., S. A Prothrombotic Thrombocytopenic Disorder Resembling Heparin-Induced Thrombocytopenia Following Coronavirus-19 Vaccination. N. Engl. J. Med. 2021. [Google Scholar] [CrossRef]
- Greinacher, A.; Thiele, T.; Warkentin, T.E.; Weisser, K.; Kyrle, P.A.; Eichinger, S. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination. N. Engl. J. Med. 2021. [Google Scholar] [CrossRef]
- Schultz, N.H.; Sørvoll, I.H.; Michelsen, A.E.; Munthe, L.A.; Lund-Johansen, F.; Ahlen, M.T.; Wiedmann, M.; Aamodt, A.-E.; Skattør, T.H.; Tjønnfjord, G.E.; et al. Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination. N. Engl. J. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Shayakhmetov, D.M.; Gaggar, A.; Ni, S.; Li, Z.-Y.; Lieber, A. Adenovirus Binding to Blood Factors Results in Liver Cell Infection and Hepatotoxicity. J. Virol. 2005, 79, 7478–7491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baker, A.H.; Mcvey, J.H.; Waddington, S.N.; Di Paolo, N.C.; Shayakhmetov, D.M. The Influence of Blood on In Vivo Adenovirus Bio-distribution and Transduction. Mol. Ther. 2007, 15, 1410–1416. [Google Scholar] [CrossRef] [PubMed]
- Summerford, C.; Samulski, R.J. Membrane-Associated Heparan Sulfate Proteoglycan Is a Receptor for Adeno-Associated Virus Type 2 Virions. J. Virol. 1998, 72, 1438–1445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- News Reuters. UPDATE 2-China’s Sinovac Defends COVID-19 Vaccine after Disappointing Brazil Data. Available online: https://www.reuters.com/article/health-coronavirus-malaysia-idCNL1N2JO0O9 (accessed on 18 March 2021).
- Tavsan, S. Sinovac’s COVID-19 Shot is 83% Effective, Not 91%, Turkey Says. Nikkei Asia. Available online: https://asia.nikkei.com/Spotlight/Coronavirus/COVID-vaccines/Sinovac-s-COVID-19-shot-is-83-effective-not-91-Turkey-says (accessed on 9 April 2021).
- Nupus, H. Indonesia Approves China’s CoronaVac for Emergency Use. 2020. Available online: https://www.aa.com.tr/en/asia-pacific/indonesia-approves-china-s-coronavac-for-emergency-use/2105881 (accessed on 9 April 2021).
- U.S. Food and Drug Administration. FDA Briefing Document. In Proceedings of the Vaccines and Related Biological Products Advisory Committee Meeting, 11 December 2020; Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3747047 (accessed on 25 March 2021).
- Janssen Ad26.COV2.S. In Proceedings of the Vaccine for the Prevention of COVID-19. 26 February 2021. Available online: https://www.fda.gov/advisory-committees/advisory-committee-calendar/vaccines-and-related-biological-products-advisory-committee-february-26-2021-meeting-announcement (accessed on 25 March 2021).
- Buss, L.F.; Prete, C.A.; Abrahim, C.M.M. Three-quarters attack rate of SARS-CoV-2 in the Brazilian Amazon during a largely unmitigated epidemic. Science 2021, 371, 288–292. [Google Scholar] [CrossRef]
- Callaway, E. Could new COVID variants undermine vaccines? Labs scramble to find out. Nat. Cell Biol. 2021, 589, 177–178. [Google Scholar] [CrossRef]
- Zhou, D.; Chan, J.F.; Zhou, B. Robust SARS-CoV-2 infection in nasal turbinates after treatment with systemic neutralizing antibodies. Cell Host Microbe. 2021, 29, 551–563. [Google Scholar] [CrossRef]
- Clerkin, K.J.; Fried, J.A.; Raikhelkar, J.; Sayer, G.; Griffin, J.M.; Masoumi, A.; Jain, S.S.; Burkhoff, D.; Kumaraiah, D.; Rabbani, L.; et al. COVID-19 and Cardiovascular Disease. Circulation 2020, 141, 1648–1655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, J.S.Y.; Tambyah, P.A.; Sia, C.-H. A Call for Vaccine Against COVID-19: Implications for Cardiovascular Morbidity and Healthcare Utilization. Cardiovasc. Drugs Ther. 2020, 34, 585–587. [Google Scholar] [CrossRef]
- World Health Organization. Module 2: Types of Vaccine and Adverse Reactions. Available online: https://vaccine-safety-training.org/live-attenuated-vaccines.html (accessed on 23 March 2021).
- Guo, W.; Li, M.; Dong, Y.; Zhou, H.; Zhang, Z.; Tian, C.; Qin, R.; Wang, H.; Shen, Y.; Du, K.; et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes/Metab. Res. Rev. 2020, 36, e3319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katulanda, P.; Dissanayake, H.A.; Ranathunga, I.; Ratnasamy, V.; Wijewickrama, P.S.A.; Yogendranathan, N.; Gamage, K.K.K.; De Silva, N.L.; Sumanatilleke, M.; Somasundaram, N.P.; et al. Prevention and management of COVID-19 among patients with diabetes: An appraisal of the literature. Diabetology 2020, 63, 1440–1452. [Google Scholar] [CrossRef]
- Chen, C.; Yan, J.T.; Zhou, N.; Zhao, J.P.; Wang, D.W. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua Xin Xue Guan Bing Za Zhi 2020, 48, E008. [Google Scholar]
- Anderson, R.M.; Vegvari, C.; Truscott, J.; Collyer, B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet 2020, 396, 1614–1616. [Google Scholar] [CrossRef]
| Title [Reference] | Clinical Phase | Population Characteristics of the Latest Trial | Doses | Technology | Immunogenicity | Safety Profile |
|---|---|---|---|---|---|---|
| BNT162b1 [4,5,6] | 1–2 | 45 adults in 3 groups: 10 μg, 30 μg, 100 μg 12 vaccines: 3 placebo in each group | 2 injections, 21 days apart | Lipid nanoparticle nucleoside-modified mRNA vaccine, encoding the spike glycoprotein of SARS-CoV-2 | Dose-dependent antibody response | No serious adverse events |
| BNT162b2 [7,8] | 1–3 | 43,448 volunteers aged 16 or older in total: (1:1 ratio) 21,720 received vaccines 21,728 received placebo | 2 injections of 30 μg doses for phase 3, 21 days apart | Lipid nanoparticle nucleoside-modified mRNA vaccine, encoding the spike glycoprotein of SARS-CoV-2 | Similar dose-dependent response as BNT162b | No serious adverse events |
| mRNA-1273 [9,10,11] | 1–3 | 30,420 adults in total: (1:1 ratio) 15,210 received vaccines 15,210 received placebo | 2 injections of 100 μg doses, 28 days apart | Lipid nanoparticle capsule of four lipids, encoding the S-2P antigen. | 100% seroconversion rates by day 15 | Similar grade 3 adverse events in the placebo group (1.3%) and the vaccine group (1.5%) |
| ChAdOx1 nCoV-19 [12,13,14] | 1–3 | 23,848 adults randomised 1:1 ratio to receive ChAdOx1 nCoV-19 or placebo | 2 injections of 3.5–6.5 × 1010 viral particles per mL, 28 days apart | Chimpanzee adenovirus-vectored vaccine with SARS-CoV-2 spike glycoprotein | Median titre of booster-dose group is more than 5 times higher than the single-dose group. | - 13 serious adverse events - None considered related to the vaccine |
| Ad5-vectored COVID-19 [15,16,17] | 1 & 2 | 508 adults randomised 2:1:1 to receive vaccine at the dosage of 1 × 1011, 5 × 1010, or placebo | 1 injection | Replication defective Ad5-vectored vaccine expressing the spike glycoprotein of SARS-CoV-2 | Higher antibody GMT in high-dose group, compared with medium and low-dose groups. | - 25 grade 3 or above adverse events - All resolved within 3 to 4 days without medications |
| rAd26-S and rAd5-S [18,19] | 1–3 | 21,977 adults in total: 16,501 received vaccines 5476 received placebo | 2 injections of 1011 viral particles in 0.5 mL vaccine, 21 days apart | Replication of Ad5-vectored and Ad-26 vectored vaccine expressing the gene for SARS-CoV-2 full-length glycoprotein S | 100% seroconversion rate | No serious adverse events |
| NVX-CoV2373 [20,21,22] | 1–3 | 30,000 adults in total: Randomised in 2:1 ratio to receive vaccine and saline placebo | 2 injections of 5 mg protein with 50 mcg matrix-M adjuvant, 21 days apart. | Nanoparticle of trimeric full-length SARS-CoV-2 spike glycoproteins and Matrix-M1 adjuvant | IgG GMT and neutralization responses exceeding convalescent serum | No serious adverse events |
| WIV-04 strain inactivated vaccine [10] | 1–2 | 96 adults randomised 1:1:1:1 to receive low-dose, medium-dose, high-dose and aluminium hydroxide, respectively | Phase 1: 3 injections on day 0, 28 and 56 | Isolated from WIV-04 strain and cultivated in a Verco cell line, followed by serial inactivation | 100% seroconversion rates in phase 1 trial and 85.7% in the phase 2 | Mild injection site pain and fever (23.4%) |
| Phase 2: 2 injections on day 0 and 14, or day 0 and 21 | ||||||
| BBIBP-CorV [11,23] | 1–2 | 192 adults: 18–59 years (96 adults) ≥60 years (96 adults). 24 receiving vaccine of 2 μg, 4 μg or 8 μg on day 0 and 28; and 24 receiving placebo. | Phase 1: 2 injections separated 28 days | HB02-strain in Verco cell line, with serial inactivation | - Higher seroconversion with higher dosage (8 μg) by day 14, - Higher neutralizing antibody GMT in younger adults | One grade 3 adverse event: self-limiting fever (>38.5 °C) |
| Phase 2: Single-dose | ||||||
| Coronavac [24] | 1–3 | 13,000 adults randomised to receive vaccine or placebo (randomisation ratio not provided) | 2 injections, 28 days apart | Inactivated vaccine from Vero cell line with SARS-CoV-2 (CN02 strain) | -High seroconversion rates: 83% in the 3 μg group, 79% in the 6 μg group, and 4% in the placebo group | One case of serious hypersensitivity with urticaria, recovered 3 months after medical treatment. |
| Ad26.COV2.S [25,26,27,28,29] | 1–3 | 40,000 adults randomised to receive vaccination or placebo (randomisation ratio not provided) | 1 injection of 5 × 1010 virus particles | replication-incompetent adenovirus serotype 26 (Ad26) vector encoding full-length SARS-CoV-2 spike protein | 100% seroconversion day 57 | Comparable serious adverse events in vaccination group and placebo group. |
| BBV152 [30,31,32] | 1–2 | 380 participants (aged 12–65 years) randomised by 1:1 ratio to receive vaccines of either 3 μg or 6 μg. | 2 intramuscular injections on day 0 and day 28 | whole-virion inactivated SARS-CoV-2 vaccine formulated with a toll-like receptor 7/8 agonist molecule (IMDG) adsorbed to alum (Algel) | 92.9% (95% CI 88.2–96.2) seroconversion rate in the 3 μg group, and 98.3% (95% CI 95.1–99.6) in the 6 μg group. | Comparable local and systemic adverse event profile in the 3 μg (9.47%) and 6 μg (11.0%) groups. No reported serious adverse events. |
| Title [Reference] | Protective Efficacy | Antigen-Specific IgG GMT Level | Neutralizing Antibody Responses | Cellular Responses |
|---|---|---|---|---|
| BNT162b1 [4,5,6] | Similar to BNT162b2 (actual figure not stated) | - 10 μg: 4813 U/mL - 30 μg: 27,873 U/mL - Increase dosage to 100 μg did not increase the IgG GMC. - Lower antigen-binding IgG in participants ≥65 years of age | Higher GMT compared to convalescent serum panel - 10 μg: 1.8-fold - 30 μg: 2.8-fold | -Functional CD4+ and CD8+ responses in all participants, predominantly Th1 helper responses. - The mean fraction of RBD-specific T cells was higher than convalescent plasma. |
| BNT162b2 [7,8] | 94.6% (95% CI 89.9–97.3) | - 10 μg: 5782 U/mL - 20 μg: 12,464 U/mL - 30 μg: 9136 U/mL - Lower antigen-binding IgG for ≥65 years of age | Higher GMT compared to convalescent serum panel 18–55 years: 1.7–4.6 times ≥65 years: 1.1–2.2 times | Not assessed |
| mRNA1273 [9,10,11] | 94.1% (95% CI 89.3–96.8; p < 0.001) | - 25 μg: 299,751 U/mL - 100 μg: 782,719 U/mL - 250 μg: 1,192,154 U/mL | Neutralizing PRNT80 generally at or above the value of convalescent serum | - The 25 μg, 100 μg groups elicited CD4+ T cell responses to Th1 cytokines. - Minimal Th2 response |
| ChadOx1 nCoV-19 [12,13,14] | Overall: 70.4% (95% CI 54.8–80.6) 2-standard dose: 62.1% (95% CI 41.0–75.7) Low dose + standard dose: 90.0% (95% CI 67.4–97.0) | - Antigen-specific antibody peaked at day 28 with 157 GMEU - Antigen specific IgG on day 28 decreased with increasing age: 18–55 years: 6439 U/mL; 56–69 years: 4553 U/mL; and ≥70 years: 3565 U/mL | 91% and 100% participants achieved PRNT80 responses in one-dose and booster-dose groups, respectively. | - The median SFCs PBPMC in the standard-dose groups: 18–55 years: 1187; 56–69 years: 797 ≥70 years: 977 No significant increase of PBPMC after the booster vaccination (p = 0.46 from paired Student’s t test of day 28 vs. day 42) |
| Ad5-vectored COVID-19 [15,16,17] | Not available at the time of writing | - High-dose: 1445.8 (95% CI 935.5–2234.5); - Medium-dose: 806 (95% CI 528.2–1229.9) - Low-dose: 615.8 (95% CI 405.4–935.5) - Seroconversions of 97%, 94% and 100% in the low-dose, medium-dose and high-dose groups, respectively. | - High-dose: 34.0 (95% CI 22.6–50.1); - Medium-dose: 16.2 (95% CI 10.4–25.2); - Low-dose: 14.5 (95% CI 9.6–12.8)) - 4-fold increase of anti-RBD IgG in 50%, 50% and 75% in the high-dose, medium-dose and low-dose groups, respectively. | - The mean SFCs PMPMC: Low-dose: 20.8 (95%CI 12.7–34.0); Medium-dose: 40.8 (95% CI 27.6–60.3) and High-dose: 58.0 (95% CI 39.1–85.9) T-cell responses in the high-dose group significantly higher than the low-dose group (p < 0.001) |
| rAd26-S and rAd5-S [18,19] | 91.6% (95% CI 85.6–95.2) | SARS-CoV-2 S1 subunit-specific IgG GMT was 53,006 with Gam-COVID-Vac and 51,200 with Gam-COVID-Vac-Lyo | 100% neutralizing antibody with GMT 49.25 and 45.95 by using Gam-COVID-Vac and 51,200 with Gam-COVID-Vac-Lyo, respectively. | - 100% increased formation of CD4+ and CD8+ cells, and increased IFN-γ - Median cell proliferation: In frozen formulation: CD4+: + 2.5% CD8+: +1.3% In lyophilised formulation: CD4+: +1.3% CD8+: +1.1% |
| NVX-CoV2373 [20,21,22] | 89.3% (95% CI 75.2–95.4) against B.1.1.7 UK variant, 49.4% (95% CI 6.1–72.8) against B.1.351 South Africa variant. | - GMEU increase by 8 (15,319 units in “5 μg + M1” and 20,429 units in “25 μg + M1”). - GMEU level higher than in convalescent serum after second dose | GMFRs 5 times greater with adjuvant (5.2 times in “5 μg + M1” and 6.3 times in “25 μg + M1”). Second dose with adjuvant resulted in GMT levels 4 times greater than those in symptomatic infections. | Stimulated Th1 phenotype response with increased IFN-γ, IL-2 and TNF- α. Minimal Th2 responses as measured by IL-5 and IL-13 cytokines. |
| WIV-04 strain inactivated vaccine [10] | Not available at the time of writing. | - Low-dose: 415 (95% CI 288–597); - Medium-dose: 349 (95% CI 258–472); - High-dose: 311 (95% CI 229–422) | Neutralizing antibody levels increased significantly 14 days after the second dose, and the third dose | Not assessed |
| BBIBP-CorV [11,23] | Not available at the time of writing. | In the 4 μg trial by 14 days after the second dose, the GMTs were: - 279.2 (95% CI 192.6–404.7) against 35C; - 234.8 (95% CI 122.2–450.8) against 56Y; - 181.0 (95% CI 105.9–309.5) against 834Y; - 304.4 (95% CI 202.1–485.6) against HN97; - 117.4 (95% CI 61.1–225.4) against F13; - 193.3 (95% CI 141.4–264.0) against HB01; - 210.7 (95% CI 120.3–369.1) against BJ01, - 146.8 (95% CI 93.8–230.0) against CQ01; - 218.5 (95% CI 125.3–380.8) against QD01; - 394.8 (95% CI 256.5–607.6) against passage 7 virus. | -In age group 18–59 years, neutralizing antibody GMT were: 2 μg: 22.6 (95% CI 18.9–27.0); 4 μg: 29.3 (95% CI 23.8–36.0); 8 μg: 36.7 (95% CI 29.8–45.2) -In the age group ≥60 years, neutralizing antibody GMT were: 2 μg: 13.4 (95% CI 9.4–19.0); 4 μg: 18.9 (95% CI 13.4–26.6); 8 μg: 23.7 (95% CI 19.0–29.6) | Not assessed |
| Coronavac [24] | Brazil: symptomatic prevention: 50.4% - mild cases prevention: 78% Severe cases prevention: 100% Turkey: 83.5% (confidence interval not reported) Indonesia: 65.3%. (confidence interval not reported) | 3 μg: 27.6 (95% CI 22.7–33.5) 6 μg: 34.5 (95% CI 28.5–41.8) Placebo: 2.3 (95% CI 2.0–2.5) | 3 μg: 5.6 (95% CI 3.6–8.7); 6 μg: 7.7 (95% CI 5.2–11.5); Placebo: 2.0 (95% CI 2.0–2.0) | The average IFN-γ positive spot-forming cells per 100,000 cells were: 3 μg group: 7.4 (95% CI 3.9–11.1); 6 μg group: 3.9 (95% CI 1.0–6.7); Placebo: 1.5 (95% CI 0.2–2.9) |
| Ad26.COV2.S [25,26,27,28,29] | Overall: 66.9% (95% CI 59.0–73.4) ≥60 years old 76.3% (95% CI, 61.6–86.0) | - Ranged from 2432 U/mL to 5729 U/mL. - The booster immunization on day 57 increased binding antibody titres 2.56-fold (range 1.58–3.04). | - The GMT of neutralizing antibody ranged from 242 to 449. - The booster immunization on day 57 increased neutralizing antibody titres by a mean of 4.62-fold (range: 3.56–5.68). | Stronger CD4+ cells response recorded in younger adults: 18–55 years:76 to 83% ≥65 years: 60 to 67% |
| BBV152 [30,31,32] | Not reported | - 3 μg: 100.9 (95% CI 74.1–137.4) - 6 μg: 197.0 (95% CI 155.6–249.4) (p = 0.0041) | The neutralizing IgG GMTs at day 56 were 10,413.9 (95% CI 9142.4–11,862.2) in the 3 μg group; and 9541.6 (95% CI 8245.9–11,041.0) in the 6 μg group at day 56. | Strongly biased to a Th1 cell response at day 42. Th2 response were detected at minimal level. |
| Number | Vaccine Platform | Type of Candidate VACCINE | Usage | Developer | Clinical Status | Phase Trials Registration No. |
|---|---|---|---|---|---|---|
| 1 | Inactivated virus | CoronaVac; SARS-CoV-2 vaccine (inactivated) | 2 doses (day 0 + 14) Intramuscular | Sinovac Research and Development Co., Ltd. | Phase 4 | Phase ½: NCT04383574 NCT04352608 NCT04551547 |
| Phase 3: NCT04456595 NCT04508075 NCT04582344 NCT04617483 NCT04651790 NCT04800133 | ||||||
| Phase 4: NCT04756830 NCT04747821 NCT04775069 NCT04789356 NCT04754698 NCT04801888 | ||||||
| 2 | Inactivated virus | Inactivated SARS-CoV-2 vaccine (Vero cell) | 2 doses (day 0 + 21) Intramuscular | Sinopharm + China National Biotec Group Co + Wuhan Institute of Biological Products | Phase 3 | Phase ½: ChiCTR2000031809 |
| Phase 3: ChiCTR2000034780 ChiCTR2000039000 NCT04510207 NCT04612972 | ||||||
| 3 | Inactivated virus | Inactivated SARS-CoV-2 vaccine (Vero cell), vaccine name BBIBP-CorV | 2 doses (day 0 + 21) Intramuscular | Sinopharm + China National Biotec Group Co + Beijing Institute of Biological Products | Phase 3 | Phase 1/2: ChiCTR2000032459 |
| Phase 3: NCT04560881 NCT04510207 | ||||||
| 4 | Viral vector (Non-replicating) | ChAdOx1-S—(AZD1222) (Covishield) | 2 doses (day 0 + 28) Intramuscular | AstraZeneca + University of Oxford | Phase 4 | Phase 1: PACTR202005681895696 |
| Phase 1/2: PACTR202006922165132 NCT04568031 NCT04444674 NCT04324606 NCT04684446 ISRCTN15638344 NCT04760730 | ||||||
| Phase 2 NCT04686773 ISRCTN69254139 | ||||||
| Phase 3: ISRCTN89951424 NCT04516746 NCT04540393 NCT04536051 EUCTR2020–005226-28-DE NCT04800133 | ||||||
| Phase 4: NCT04760132 NCT04775069 | ||||||
| 5 | Viral vector (Non-replicating) | Recombinant novel coronavirus vaccine (Adenovirus type 5 vector) | 1 dose Day 0 Intramuscular | CanSino Biological Inc./Beijing Institute of Biotechnology | Phase 3 | Phase 1: ChiCTR2000030906 NCT04313127 NCT04568811 NCT04552366 |
| Phase 1/2: NCT04398147 | ||||||
| Phase 2: ChiCTR2000031781 NCT04566770 NCT04341389 | ||||||
| Phase 3: NCT04526990 NCT04540419 | ||||||
| 6 | Viral vector (Non-replicating) | Gam-COVID-Vac Adeno-based (rAd26-S + rAd5-S) | 2 doses (day 0 + 21) Intramuscular | Gamaleya Research Institute; Health Ministry of the Russian Federation | Phase 3 | Phase 1/2: NCT04436471 NCT04437875 NCT04713488 NCT04760730 |
| Phase 2: NCT04587219 | ||||||
| Phase 2/3: NCT04640233 | ||||||
| Phase 3: NCT04530396 NCT04564716 NCT04642339 NCT04656613 NCT04741061 | ||||||
| 7 | Viral vector (Non-replicating) | Ad26.COV2.S | 1–2 doses Day 0 or Day 0+ Day 56 Intramuscular | Janssen Pharmaceutical | Phase 3 | Phase 1: NCT04509947 |
| Phase 1/2: NCT04436276 | ||||||
| Phase 2: EUCTR2020-002584-63-DE NCT04535453 NCT04765384 | ||||||
| Phase 3: NCT04505722 NCT04614948 | ||||||
| 8 | Protein subunit | SARS-CoV-2 rS/Matrix M1-Adjuvant (Full length recombinant SARS CoV-2 glycoprotein nanoparticle vaccine adjuvanted with Matrix M) | 2 doses (day 0 + 21) Intramuscular | Novavax | Phase 3 | Phase 1/2: NCT04368988 |
| Phase 2: NCT04533399 | ||||||
| Phase 3: NCT04611802 EUCTR2020-004123-16-GB NCT04583995 | ||||||
| 9 | RNA based vaccine | mRNA -1273 mRNA-1283 | 2 doses (day 0 + 28) Intramuscular | Moderna + National Institute of Allergy and Infectious Diseases (NIAID) | Phase 4 | Phase 1: NCT04283461 NCT04813796 |
| Phase 1/2: NCT04677660 NCT04712110 | ||||||
| Phase 2: NCT04405076 NCT04761822 | ||||||
| Phase 2/3: NCT04649151 NCT04796896 | ||||||
| Phase 3: NCT04470427 NCT04811664 NCT04805125 NCT04806113 | ||||||
| Phase 4: NCT04760132 NCT04792567 | ||||||
| 10 | RNA based vaccine | BNT162b2 | 2 doses (day 0 + 21) Intramuscular | Pfizer/BioNTech + Fosun Pharma | Phase 4 | Phase 1: NCT04523571 ChiCTR2000034825 NCT04816643 |
| Phase 1/2: NCT04588480 NCT04380701 NCT04537949 EUCTR2020-003267-26-DE | ||||||
| Phase 2: NCT04649021 NCT04761822 | ||||||
| Phase 2/3: NCT04754594 | ||||||
| Phase 3: NCT04368728 NCT04713553 NCT04800133 NCT04805125 NCT04816669 | ||||||
| Phase 4: NCT04760132 EUCTR2021-000412-28-BE EUCTR2021-000412-28-BE NCT04780659 NCT04775069 | ||||||
| 11 | Protein subunit | Recombinant SARS-CoV-2 vaccine (CHO Cell) | 2–3 doses Day 0 + 28 or Day 0 + 28 + 56 Intramuscular | Anhui Zhifei Longcom Biopharmaceutical + Institute of Microbiology, Chinese Academy of Sciences | Phase 3 | Phase 1: NCT04445194 ChiCTR2000035691 NCT04636333 |
| Phase 1/2: NCT04550351 NCT04813562 | ||||||
| Phase 2: NCT04466085 | ||||||
| Phase 3: NCT04646590 | ||||||
| 12 | RNA based vaccine | CVnCoV Vaccine | 2 doses Day 0 + Day 28 Intramuscular | CureVac AG | Phase 3 | Phase 1: NCT04449276 |
| Phase 2: NCT04515147 PER-054-20 | ||||||
| Phase 2/3: NCT04652102 | ||||||
| Phase 3: NCT04674189 | ||||||
| 13 | Inactivated virus | SARS-CoV-2 vaccine (Vero cells) | 2 doses Day 0 + Day 28 Intramuscular | Institute of Medical Biology + Chinese Academy of Medical Sciences | Phase 3 | Phase 1/2: NCT04470609 NCT04412538 |
| Phase 3: NCT04659239 | ||||||
| 14 | Inactivated virus | QazCovid-in®—COVID-19 inactivated vaccine | 2 doses Day 0 + Day 21 Intramuscular | Research Institute for Biological Safety Problems, Rep of Kazakhstan | Phase 3 | Phase ½: NCT04530357 |
| Phase 3: NCT04691908 | ||||||
| 15 | DNA based vaccine | INO-4800 + electroporation | 2 doses Day 0 + Day 28 Intradermal | Inovio Pharmaceuticals + International Vaccine Institute + Advaccine (Suzhou) Biopharmaceutical Co., Ltd. | Phase 2/3 | Phase 1: NCT04336410 ChiCTR2000038152 |
| Phase 1/2: NCT04447781 | ||||||
| Phase 2: ChiCTR2000040146 | ||||||
| Phase 2/3: NCT04642638 | ||||||
| 16 | DNA based vaccine | AG0301-COVID19 | 2 doses Day 0 + Day 14 Intramuscular | AnGes + Takara Bio + Osaka University | Phase 2/3 | Phase 1/2: NCT04463472 NCT04527081 jRCT2051200085 |
| Phase 2/3: NCT04655625 | ||||||
| 17 | DNA based vaccine | nCov vaccine | 3 doses Day 0 + Day 28 + Day 56 Intradermal | Zydus Cadila | Phase 3 | Phase 1/2: CTRI/2020/07/026352 CTRI/2021/03/032051 |
| Phase 3: CTRI/2020/07/026352 | ||||||
| 18 | DNA based vaccine | GX-19N | 2 doses Day 0 + Day 28 Intramuscular | Genexine Consortium | Phase ½ | Phase 1/2: NCT04445389 NCT04715997 |
| 19 | Inactivated virus | Whole-Virion Inactivated SARS-CoV-2 Vaccine (BBV152) | 2 doses Day 0 + Day 14 Intramuscular | Bharat Biotech International Limited | Phase 3 | Phase 1/2: NCT04471519 CTRI/2020/07/026300 CTRI/2020/09/027674 |
| Phase 3: NCT04641481; CTRI/2020/11/028976 | ||||||
| 20 | Protein subunit | KBP-COVID-19 (RBD-based) | 2 doses Day 0 + Day 21 Intramuscular | Kentucky Bioprocessing Inc. | Phase 1/2 | Phase 1/2: NCT04473690 |
| 21 | Protein subunit | VAT00002: SARS-CoV-2 S protein with adjuvant | 2 doses Day 0 + Day 21 Intramuscular | Sanofi Pasteur + GSK | Phase 3 | Phase 1/2: NCT04537208 |
| Phase 2: NCT04762680 | ||||||
| Phase 3: PACTR202011523101903 | ||||||
| 22 | RNA based vaccine | ARCT-021 | 2 doses Day 0 + Day 21 Intramuscular | Arcturus Therapeutics | Phase 2 | Phase 1/2: NCT04480957 |
| Phase 2: NCT04668339 NCT04728347 | ||||||
| 23 | Virus like particle | RBD SARS-CoV-2 HBsAg VLP vaccine | 2 doses Day 0 + Day 28 Intramuscular | Serum Institute of India + Accelagen Pty + SpyBiotech | Phase 1/2 | Phase 1/2: ACTRN12620000817943 ACTRN12620001308987 |
| 24 | Inactivated virus | Inactivated SARS-CoV-2 vaccine (Vero cell) | 2–3 doses Detailed schedule not specified Intramuscular | Beijing Minhai Biotechnology Co | Phase 2 | Phase 1: NCT04758273 |
| Phase 2: NCT04756323 | ||||||
| 25 | Viral vector (Non-replicating) | GRAd-COV2 (Replication defective Simian Adenovirus (GRAd) encoding S) | 1 dose Day 0 Intramuscular | ReiThera + Leukocare + Univercells | Phase 2/3 | Phase 1: NCT04528641 |
| Phase 2/3: NCT04791423 | ||||||
| 26 | Viral vector (Non-replicating) | VXA-CoV2-1 Ad5 adjuvanted Oral Vaccine platform | 2 doses Day 0 + Day 28 Intramuscular | Vaxart | Phase 1 | Phase 1: NCT04563702 |
| 27 | Viral vector (Non-replicating) | MVA-SARS-2-S | 2 doses Day 0 + Day 28 Intramuscular | University of Munich (Ludwig-Maximilians) | Phase 1 | Phase 1: NCT04569383 |
| 28 | Protein subunit | SCB-2019 + AS03 or CpG 1018 adjuvant plus Alum adjuvant (Native like Trimeric subunit Spike Protein vaccine) | 2 doses Day 0 + Day 21 Intramuscular | Clover Biopharmaceuticals Inc./GSK/Dynavax | Phase 2/3 | Phase 1: NCT04405908 |
| Phase 2/3: NCT04672395 | ||||||
| 29 | Protein subunit | COVAX-19® Recombinant spike protein + adjuvant | 2 doses Day 0 + Day 21 Intramuscular | Vaxine Pty Ltd. | Phase 1 | Phase 1: NCT04453852 |
| 30 | Protein subunit | MVC-COV1901 (S-2P protein + CpG 1018) | 2 doses Day 0 + Day 28 Intramuscular | Medigen Vaccine Biologics + Dynavax + National Institute of Allergy and Infectious Diseases (NIAID) | Phase 2 | Phase 1: NCT04487210 |
| Phase 2: NCT04695652 | ||||||
| 31 | Protein subunit | FINLAY-FR1 anti-SARS-CoV-2 Vaccine (RBD + adjuvant) | 2 doses Day 0 + Day 28 Intramuscular | Instituto Finlay de Vacunas | Phase 1/2 | Phase 1: RPCEC00000338 |
| Phase 1/2: RPCEC00000332 | ||||||
| 32 | Protein subunit | FINLAY-FR-2 anti-SARS-CoV-2 Vaccine (RBD chemically conjugated to tetanus toxoid plus adjuvant) | 2 doses Day 0 + Day 28 Intramuscular | Instituto Finlay de Vacunas | Phase 3 | Phase 1: RPCEC00000340 |
| Phase 2: RPCEC00000347 | ||||||
| Phase 3: RPCEC00000354 | ||||||
| 33 | Protein subunit | EpiVacCorona (EpiVacCorona vaccine based on peptide antigens for the prevention of COVID-19) | 2 doses Day 0 + Day 21 Intramuscular | Federal Budgetary Research Institution State Research Center of Virology and Biotechnology “Vector” | Phase 3 | Phase 1/2: NCT04527575 |
| Phase 3: NCT04780035 | ||||||
| 34 | Protein subunit | RBD (baculovirus production expressed in Sf9 cells) Recombinant SARS-CoV-2 vaccine (Sf9 Cell) | 2 doses Day 0 + Day 21 Intramuscular | West China Hospital + Sichuan University | Phase 2 | Phase 1: ChiCTR2000037518 NCT04530656 |
| Phase 2: ChiCTR2000039994 NCT04640402 NCT04718467 | ||||||
| 35 | Protein subunit | IMP CoVac-1 (SARS-CoV-2 HLA-DR peptides) | 1 dose Day 0 Subcutaneous | University Hospital Tuebingen | Phase 1 | NCT04546841 |
| 36 | Protein subunit | UB-612 (Multitope peptide based S1-RBD-protein based vaccine) | 2 doses Day 0 + Day 28 Intramuscular | COVAXX + United Biomedical Inc | Phase 2/3 | Phase 1: NCT04545749 |
| Phase 2: NCT04773067 | ||||||
| Phase 2/3: NCT04683224 | ||||||
| 37 | Viral vector (Replicating) | DelNS1-2019-nCoV-RBD-OPT1 (Intranasal flu-based-RBD) | 2 doses Day 0 + Day 28 Intranasal | University of Hong Kong, Xiamen University and Beijing Wantai Biological Pharmacy | Phase 2 | Phase 1: ChiCTR2000037782 NCT04809389 |
| Phase 2: ChiCTR2000039715 | ||||||
| 38 | RNA based vaccine | LNP-nCoVsaRNA | 2 doses Day 0 + Day 28 Intranasal | Imperial College London | Phase 1 | Phase 1: ISRCTN17072692 |
| 39 | RNA based vaccine | SARS-CoV-2 mRNA vaccine (ARCoV) | 2 doses Day 0 + Day 28 Intranasal | Academy of Military Science (AMS), Walvax Biotechnology and Suzhou Abogen Biosciences | Phase 2 | Phase 1: ChiCTR2000034112 ChiCTR2000039212 |
| Phase 2: ChiCTR2100041855 | ||||||
| 40 | Virus like particle | Coronavirus-Like Particle COVID-19 (CoVLP) | 2 doses Day 0 + Day 21 Intranasal | Medicago Inc. | Phase 2/3 | Phase 1: NCT04450004 |
| Phase 2: NCT04662697 | ||||||
| Phase 2/3: NCT04636697 | ||||||
| 41 | Viral vector (Replicating) + APC | Covid-19/aAPC vaccine. The Covid-19/aAPC vaccine is prepared by applying lentivirus modification with immune modulatory genes and the viral minigenes to the artificial antigen presenting cells (aAPCs). | 3 doses Day 0 + Day 14 + Day 28 Subcutaneous | Shenzhen Geno-Immune Medical Institute | Phase 1 | Phase 1: NCT04299724 |
| 42 | Viral vector (Non-replicating) + APC | LV-SMENP-DC vaccine. Dendritic cells are modified with lentivirus vectors expressing Covid-19 minigene SMENP and immune modulatory genes. CTLs are activated by LV-DC presenting Covid-19 specific antigens. | 1 dose Day 0 Subcutaneous | Shenzhen Geno-Immune Medical Institute | Phase 1/2 | Phase 1/2: NCT04276896 |
| 43 | Protein subunit | AdimrSC-2f (Recombinant RBD +/− Aluminium) | No detail | Adimmune Corporation | Phase 1 | Phase 1: NCT04522089 |
| 44 | DNA based vaccine | Covigenix VAX-001—DNA vaccines + proteo-lipid vehicle (PLV) formulation | 2 doses Day 0 + Day 14 Intramuscular | Entos Pharmaceuticals Inc. | Phase 1 | NCT04591184 |
| 45 | DNA based vaccine | CORVax—Spike (S) Protein Plasmid DNA Vaccine | 2 doses Day 0 + Day 14 Intradermal | Providence Health & Services | Phase 1 | Phase 1: NCT04627675 |
| 46 | RNA based vaccine | ChulaCov19 mRNA vaccine | 2 doses Day 0 + Day 21 Intramuscular | Chulalongkorn University | Phase 1 | Phase 1: NCT04566276 |
| 47 | DNA based vaccine | bacTRL-Spike oral DNA vaccine | 1 dose Day 0 Oral | Symvivo Corporation | Phase 1 | NCT04334980 |
| 48 | Viral Vector (Non-replicating) | Human Adenovirus type 5: hAd5 S + N vaccine (S-fusion + N-ETSD) E2b-deleted Adeno | 1–2 doses Day 0 + day 21 Subcutaneous or Oral | Immunity Bio.Inc | Phase 1 | Phase 1: NCT04591717 NCT04710303 |
| 49 | Viral vector (Non-replicating) | COH04S1 (MVA-SARS-2-S)—Modified vaccinia ankara (sMVA) platform + synthetic SARS-CoV-2 | 2 doses Day 0 + Day 28 Intramuscular | City of Hope Medical Center + National Cancer Institute | Phase 1 | Phase 1: NCT04639466 |
| 50 | Viral vector (Replicating) | rVSV-SARS-CoV-2-S Vaccine | 1 dose Day 0 Intramuscular | Israel Institute for Biological Research | Phase 1/2 | Phase 1/2: NCT04608305 |
| 51 | Viral vector (Replicating) + APC | Dendritic cell vaccine AV-COVID-19. A vaccine consisting of autologous dendritic cells loaded with antigens from SARS-CoV-2, with or without GM-CSF | 1 dose Day 0 Intramuscular | Aivita Biomedical, Inc. National Institute of Health Research and Development, Ministry of Health Republic of Indonesia | Phase 1/2 | Phase 1: NCT04690387 NCT04685603 |
| Phase 1/2: NCT04386252 | ||||||
| 52 | Live attenuated virus | COVI-VAC | 1–2 doses Day 0 or Day 0 + 28 Intranasal | Codagenix/Serum Institute of India | Phase 1 | Phase 1: NCT04619628 |
| 53 | Protein subunit | CIGB-669 (RBD + AgnHB) | 3 doses Day 0 + 14 + 28 or Day 0 + 28 + 56 Intranasal | Center for Genetic Engineering and Biotechnology (CIGB) | Phase 1/2 | Phase 1/2: RPCEC00000345 |
| 54 | Protein subunit | CIGB-66 (RBD + aluminium hydroxide) | 3 doses Day 0 + 14 + 28 or Day 0 + 28 + 56 Intranasal | Center for Genetic Engineering and Biotechnology (CIGB) | Phase 3 | Phase 1/2: RPCEC00000346 |
| Phase 3 RPCEC00000359 | ||||||
| 55 | Inactivated Virus | VLA2001 | 2 doses Day 0 + Day 21 Intramuscular | Valneva, National Institute for Health Research, United Kingdom | Phase 1/2 | Phase 1/2: NCT04671017 |
| 56 | Protein subunit | BECOV2 | 2 doses Day 0 + Day 28 Intramuscular | Biological E. Limited | Phase 1/2 | Phase 1/2: CTRI/2020/11/029032 |
| 57 | Viral vector (Replicating) | AdCLD-CoV19 (adenovirus vector) | 1 dose Day 0 Intramuscular | Cellid Co., Ltd. | Phase 1/2 | Phase 1/2: NCT04666012 |
| 58 | DNA based vaccine | GLS-5310 | 2 doses Day 0 + Day 56 or Day 0 + Day 84 Intradermal | GeneOne Life Science, Inc. | Phase 1/2 | Phase 1/2: NCT04673149 |
| 59 | Protein subunit | Recombinant Sars-CoV-2 Spike protein, Aluminum adjuvanted | 2 doses Day 0 + 21 Intramuscular | Nanogen Pharmaceutical Biotechnology | Phase 1/2 | Phase 1/2: NCT04683484 |
| 60 | Protein subunit | Recombinant protein vaccine S-268019 (using Baculovirus expression vector system) | 2 doses Day 0 + 21 Intramuscular | Shionogi | Phase 1/2 | Phase 1/2: jRCT2051200092 |
| 61 | Viral vector (Non-replicating) | AdCOVID, Adenovirus-based platform expresses the receptor-binding domain (RBD) of the Sars-Cov-2 spike protein | 1 doses Day 0 Intranasal | Altimmune, Inc. | Phase 1 | Phase 1: NCT04679909 |
| 62 | Protein subunit | SARS-CoV-2-RBD-Fc fusion protein | Dosage and Schedule not specified Subcutaneous or intramuscular | University Medical Center Groningen + Akston Biosciences Inc. | Phase 1/2 | Phase 1/2: NCT04681092 |
| 63 | Inactivated Virus | ERUCOV-VAC, inactivated virus | 2 doses Day 0 + 21 Intramuscular | Erciyes University | Phase 2 | Phase 1: NCT04691947 |
| Phase 2: NCT04824391 | ||||||
| 64 | Protein subunit | COVAC-1 and COVAC-2 sub-unit vaccine (spike protein) + SWE adjuvant | 2 doses Day 0 + 28 Intramuscular | University of Saskatchewan | Phase 1/2 | Phase 1/2: NCT04702178 |
| 65 | Protein subunit | GBP510, a recombinant surface protein vaccine with adjuvant AS03 (aluminium hydroxide) | 2 doses Day 0 + 28 Intramuscular | SK Biosciences Co. Ltd. and CEPI | Phase 1/2 | Phase 1/2: NCT04742738 NCT04750343 |
| 66 | Protein subunit | Razi Cov Pars, recombinant spike protein | 3 doses Day 0 + 21 + 51 Intramuscular and intranasal | Razi Vaccine and Serum Research Institute | Phase 1 | Phase 1: IRCT20201214049709N1 |
| 67 | Inactivated Virus | COVID-19 inactivated vaccine | 2 doses Day 0 + 14 Intramuscular | Shifa Pharmed Industrial Co | Phase 2/3 | Phase 1: IRCT20201202049567N1 IRCT20201202049567N2 |
| 68 | Protein subunit | MF59 adjuvanted SARS-CoV-2 Sclamp vaccine | 2 doses Day 0 + 28 Intramuscular | The University of Queensland | Phase 1 | Phase 1: NCT04495933 |
| 69 | DNA based vaccine | COVIGEN | 2 doses Day 0 + 28 Intramuscular or intradermal | University of Sydney, Bionet Co., Ltd. Technovalia | Phase 1 | Phase 1: NCT04742842 |
| 70 | DNA based vaccine | COVID-eVax, a candidate plasmid DNA vaccine of the Spike protein | No detailed dosage schedule Intramuscular | Takis + Rottapharm Biotech | Phase 1/2 | Phase 1/2: NCT04788459 EUCTR2020-003734-20-IT |
| 71 | Viral vector (Non-replicating) | BBV154, Adenoviral vector COVID-19 vaccine | 1 dose Day 0 Intramuscular | Bharat Biotech International Limited | Phase 1 | Phase 1: NCT04751682 |
| 72 | RNA based vaccine | PTX-COVID19-B, mRNA vaccine | 2 doses Day 0 + 28 Intramuscular | Providence Therapeutics | Phase 1 | Phase 1: NCT04765436 |
| 73 | Viral vector (Replicating) | NDV-HXP-S, Newcastle disease virus (NDV) vector expressing the spike protein of SARS-CoV-2, with or without the adjuvant CpG 1018 | 2 doses Day 0 + 28 Intramuscular | Mahidol University; The Government Pharmaceutical Organization (GPO); Icahn School of Medicine at Mount Sinai | Phase 1/2 | Phase 1/2: NCT04764422 |
| 74 | RNA based vaccine | CoV2 SAM (LNP) vaccine. A self-amplifying mRNA (SAM) lipid nanoparticle (LNP) platform + Spike antigen | 2 doses Day 0 + 28 Intramuscular | GlaxoSmithKline | Phase 1 | Phase 1: NCT04758962 |
| 75 | Virus like particle | VBI-2902a. An enveloped virus-like particle (eVLP) of SARS-CoV-2 spike (S) glycoprotein and aluminum phosphate adjuvant. | 2 doses Day 0 + 28 Intramuscular | VBI Vaccines Inc. | Phase 1/2 | NCT04773665 |
| 76 | Protein subunit | SK SARS-CoV-2 recombinant surface antigen protein subunit (NBP2001) + adjuvanted with alum. | 2 doses Day 0 + 28 Intramuscular | SK Bioscience Co., Ltd. | Phase 1 | Phase 1: NCT04760743 |
| 77 | Viral vector (Non-replicating) | Chimpanzee Adenovirus serotype 68 (ChAd) and self-amplifying mRNA (SAM) vectors expressing spike alone, or spike plus additional SARS-CoV-2 T cell epitopes. | 2–3 doses Day 0 +14 + 28 or Day 0 + 28 + 56 or Day 0 + 112 Intramuscular | Gritstone Oncology | Phase 1 | Phase 1: NCT04776317 |
| 78 | RNA based vaccine | mRNA-1273.351. A lipid nanoparticle (LNP)-encapsulated mRNA-based vaccine that encodes for a full-length, prefusion stabilized S protein of the SARS-CoV-2 B.1.351 variant. | 3 doses Day 0 + 28 + 56 Intramuscular | Moderna + National Institute of Allergy and Infectious Diseases (NIAID) | Phase 1 | Phase 1: NCT04785144 |
| 79 | Protein subunit | SpFN (spike ferritin nanoparticle) uses spike proteins with a liposomal formulation QS21 (ALFQ) adjuvant. | 3 doses Day 0 + 28 + 120 Intramuscular | Walter Reed Army Institute of Research (WRAIR) | Phase 1 | Phase 1: NCT04784767 |
| 80 | Protein subunit | EuCorVac-19; A spike protein using the recombinant protein technology and with an adjuvant. | 2 doses Day 0 + 21 Intramuscular | POP Biotechnologies and EuBiologics Co.,Ltd | Phase 1/2 | Phase 1/2: NCT04783311 |
| 81 | Inactivated virus | Inactivated SARS-CoV-2 vaccine FAKHRAVAC (MIVAC) | 2 doses Day 0 + 21 Intramuscular | Organization of Defensive Innovation and Research | Phase 1 | Phase 1: IRCT20210206050259N1 |
| 82 | Live attenuated virus | MV-014-212, a live attenuated vaccine that expresses the spike (S) protein of SARS-CoV-2 | 2 doses Day 0 + 35 Intranasal | Meissa Vaccines, Inc. | Phase 1 | Phase 1: NCT04798001 |
| 83 | RNA based vaccine | MRT5500, an mRNA vaccine candidate | 2 doses Day 0 + 21 Intramuscular | Sanofi Pasteur and Translate Bio | Phase 1/2 | Phase 1/2: NCT04798027 |
| 84 | Virus like particle | SARS-CoV-2 VLP Vaccine | 1 doses Day 0 Subcutaneous | The Scientific and Technological Research Council of Turkey | Phase 1 | Phase 1: NCT04818281 |
| 85 | Protein subunit | ReCOV: Recombinant two-component spike and RBD protein COVID-19 vaccine (CHO cell). | 2 doses Day 0 + 21 Intramuscular | Jiangsu Rec-Biotechnology | Phase 1 | Phase 1: NCT04818801 |
| 86 | RNA based vaccine | DS-5670a, mRNA vaccine | 2 doses Day 0 + 21 Intramuscular | Daiichi Sankyo Co., Ltd. | Phase 1/2 | Phase 1/2: NCT04821674 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, Z.-P.; Yang, M.; Lai, C.-L. COVID-19 Vaccines: A Review of the Safety and Efficacy of Current Clinical Trials. Pharmaceuticals 2021, 14, 406. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14050406
Yan Z-P, Yang M, Lai C-L. COVID-19 Vaccines: A Review of the Safety and Efficacy of Current Clinical Trials. Pharmaceuticals. 2021; 14(5):406. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14050406
Chicago/Turabian StyleYan, Zhi-Peng, Ming Yang, and Ching-Lung Lai. 2021. "COVID-19 Vaccines: A Review of the Safety and Efficacy of Current Clinical Trials" Pharmaceuticals 14, no. 5: 406. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14050406







