An Adenovirus Vector Expressing FMDV RNA Polymerase Combined with a Chimeric VLP Harboring a Neutralizing Epitope as a Prime Boost Strategy to Induce FMDV-Specific Humoral and Cellular Responses
Abstract
:1. Introduction
2. Results and Discussion
2.1. Generation of Recombinant Adenoviruses Expressing the FMDV 3D RNA Polymerase
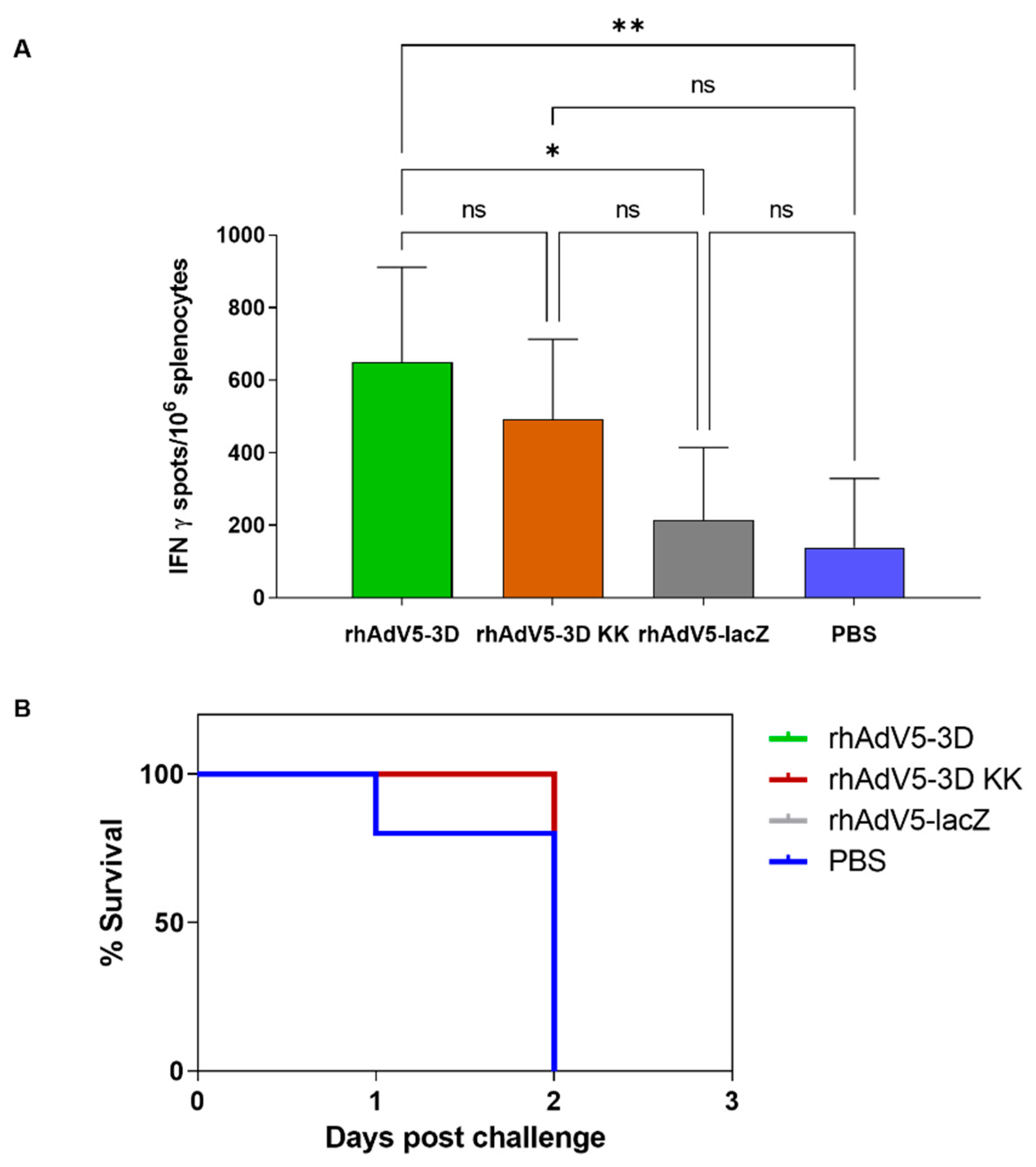
2.2. Recombinant Adenoviruses Expressing the FMDV 3D RNA Polymerase Can Induce Specific Cellular Responses In Vivo
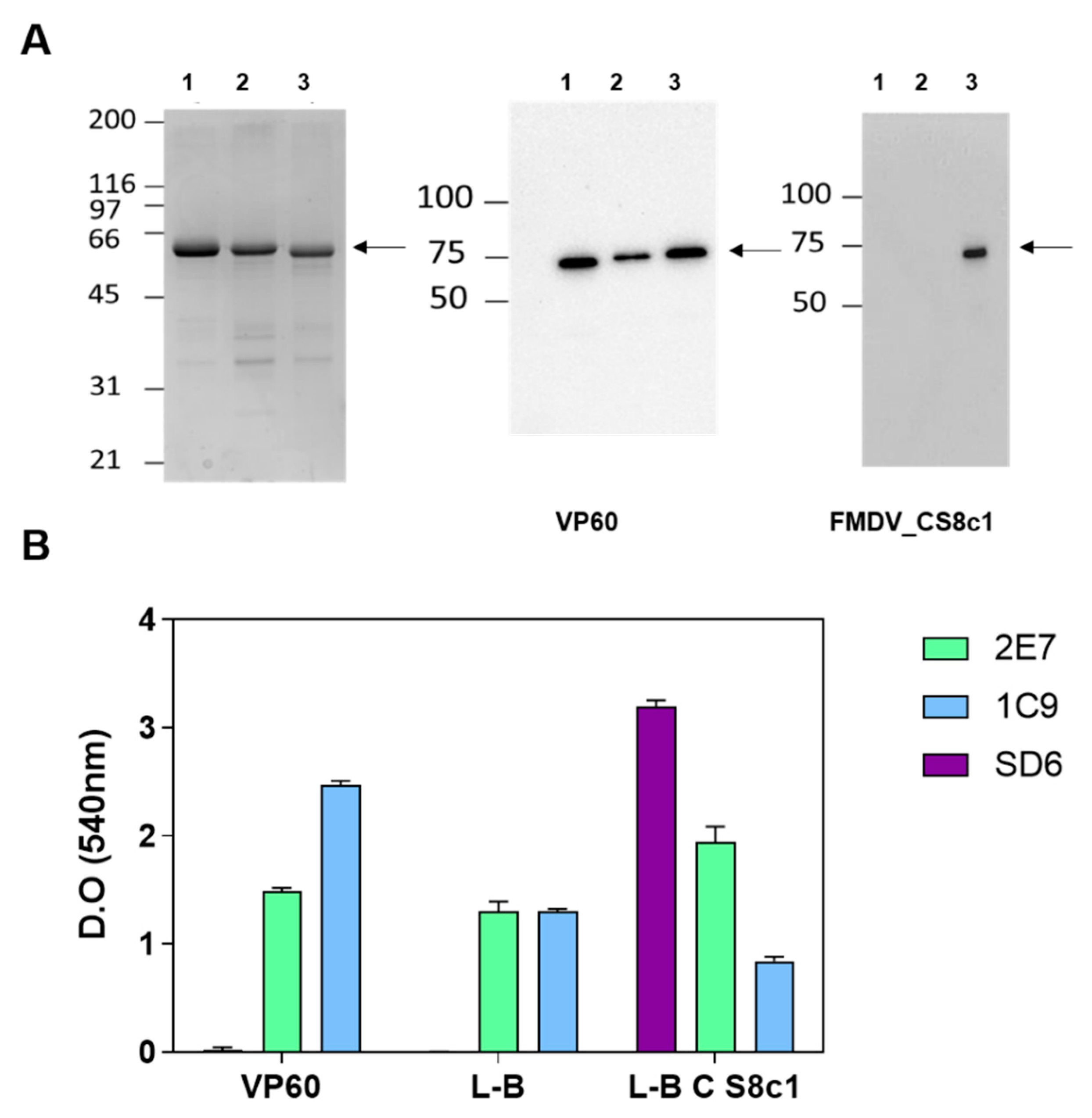
2.3. Generation of Chimeric VLPs Bearing an FMDV Neutralizing Epitope from Serotype C
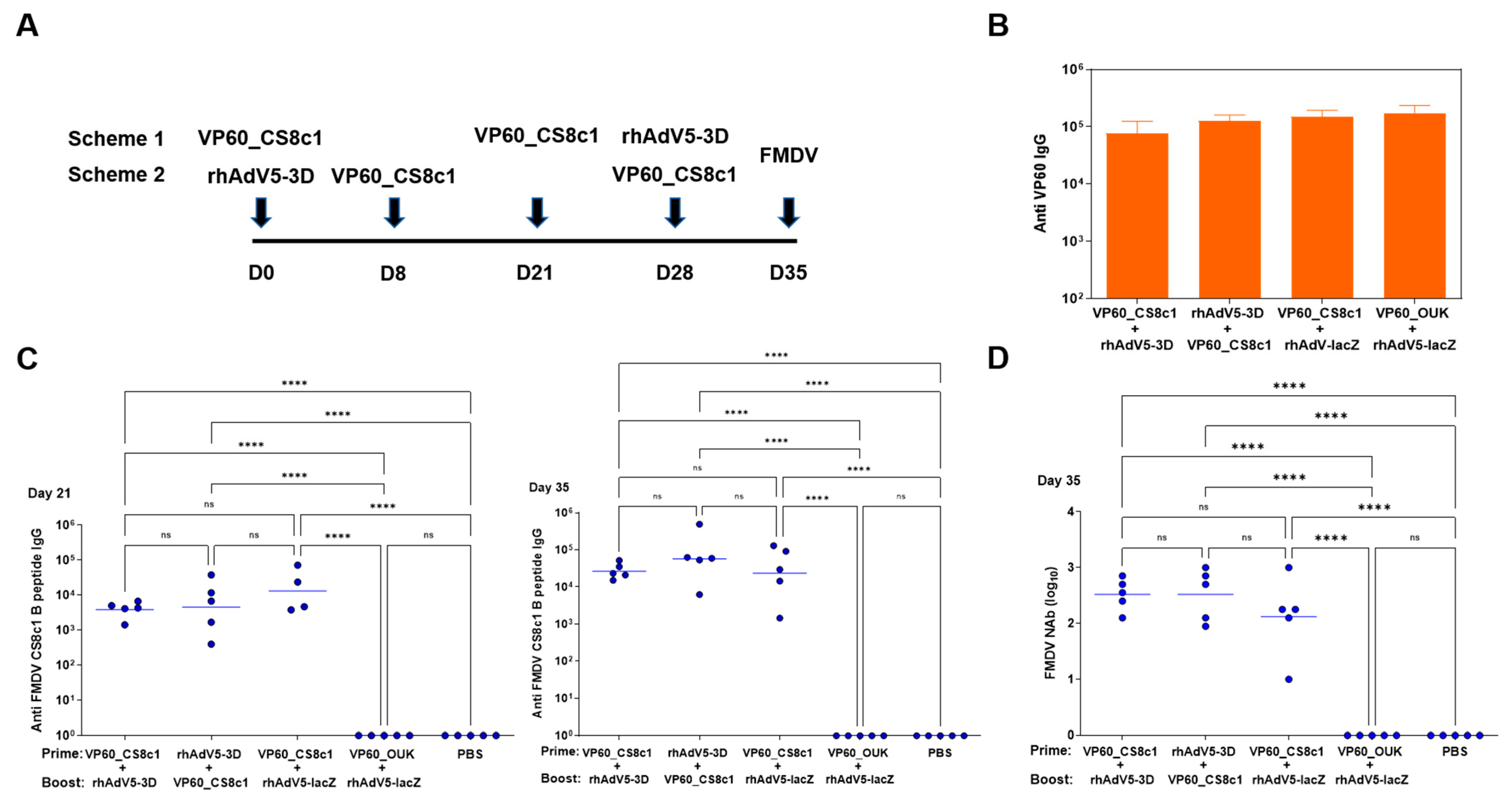
2.4. A Combined Vaccination Scheme Including rhAdV5-3D and RHDV-FMDV C_S8c1 VLPs Induces Both Specific Neutralizing Antibodies and Cellular Responses in Mice
3. Materials and Methods
3.1. Cells and Viruses
3.2. Generation of Recombinant Adenoviruses and Baculoviruses
3.3. Purification of Virus-Like Particles
3.4. Protein Transfer and Immunodetection on Membranes (Western Blot)
3.5. Immunodetection by ELISA Assays
3.6. Detection of Specific IFNγ-Secreting Cells by ELISPOT
3.7. FMDV Neutralization Assay
3.8. Immunization and Challenge of C57BL/6 Mice
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stenfeldt, C.; Diaz-San Segundo, F.; de Los Santos, T.; Rodriguez, L.L.; Arzt, J. The Pathogenesis of Foot-and-Mouth Disease in Pigs. Front. Vet. Sci. 2016, 3, 41. [Google Scholar] [CrossRef]
- Burrows, R.; Mann, J.A.; Garland, A.J.; Greig, A.; Goodridge, D. The Pathogenesis of Natural and Simulated Natural Foot-and-Mouth Disease Infection in Cattle. J. Comp. Pathol. 1981, 91, 599–609. [Google Scholar] [CrossRef]
- Knight-Jones, T.J.D.; Rushton, J. The Economic Impacts of Foot and Mouth Disease—What Are They, How Big Are They and Where Do They Occur? Prev. Vet. Med. 2013, 112, 161–173. [Google Scholar] [CrossRef] [Green Version]
- Paton, D.J.; Gubbins, S.; King, D.P. Understanding the Transmission of Foot-and-Mouth Disease Virus at Different Scales. Curr. Opin. Virol. 2018, 28, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Arzt, J.; Belsham, G.J.; Lohse, L.; Bøtner, A.; Stenfeldt, C. Transmission of Foot-and-Mouth Disease from Persistently Infected Carrier Cattle to Naive Cattle via Transfer of Oropharyngeal Fluid. mSphere 2018, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belsham, G.J.; Kristensen, T.; Jackson, T. Foot-and-Mouth Disease Virus: Prospects for Using Knowledge of Virus Biology to Improve Control of This Continuing Global Threat. Virus Res. 2020, 281, 197909. [Google Scholar] [CrossRef] [PubMed]
- Knowles, N.J.; Hovi, T.; King, A.M.Q.; Stanway, G. Overview of Taxonomy. Picornaviruses 2010, 19–32. [Google Scholar] [CrossRef]
- Domingo, E.; Baranowski, E.; Escarmís, C.; Sobrino, F. Foot-and-Mouth Disease Virus. Comp. Immunol. Microbiol. Infect. Dis. 2002, 25, 297–308. [Google Scholar] [CrossRef]
- Brito, B.P.; Rodriguez, L.L.; Hammond, J.M.; Pinto, J.; Perez, A.M. Review of the Global Distribution of Foot-and-Mouth Disease Virus from 2007 to 2014. Transbound. Emerg. Dis. 2017, 64, 316–332. [Google Scholar] [CrossRef]
- Rangel, G.; Bárcena, J.; Moreno, N.; Mata, C.P.; Castón, J.R.; Alejo, A.; Blanco, E. Chimeric RHDV Virus-Like Particles Displaying Foot-and-Mouth Disease Virus Epitopes Elicit Neutralizing Antibodies and Confer Partial Protection in Pigs. Vaccines 2021, 9, 470. [Google Scholar] [CrossRef]
- Nagesha, H.S.; Wang, L.F.; Hyatt, A.D.; Morrissy, C.J.; Lenghaus, C.; Westbury, H.A. Self-Assembly, Antigenicity, and Immunogenicity of the Rabbit Haemorrhagic Disease Virus (Czechoslovakian Strain V-351) Capsid Protein Expressed in Baculovirus. Arch. Virol. 1995, 140, 1095–1108. [Google Scholar] [CrossRef]
- Nagesha, H.S.; Wang, L.F.; Hyatt, A.D. Virus-like Particles of Calicivirus as Epitope Carriers. Arch. Virol. 1999, 144, 2429–2439. [Google Scholar] [CrossRef] [PubMed]
- Moreno, N.; Mena, I.; Angulo, I.; Gómez, Y.; Crisci, E.; Montoya, M.; Castón, J.R.; Blanco, E.; Bárcena, J. Rabbit Hemorrhagic Disease Virus Capsid, a Versatile Platform for Foreign B-Cell Epitope Display Inducing Protective Humoral Immune Responses. Sci. Rep. 2016, 6, 31844. [Google Scholar] [CrossRef]
- Pfaff, E.; Mussgay, M.; Böhm, H.O.; Schulz, G.E.; Schaller, H. Antibodies against a Preselected Peptide Recognize and Neutralize Foot and Mouth Disease Virus. EMBO J. 1982, 1, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Gullberg, M.; Lohse, L.; Bøtner, A.; McInerney, G.M.; Burman, A.; Jackson, T.; Polacek, C.; Belsham, G.J. A Prime-Boost Vaccination Strategy in Cattle to Prevent Foot-and-Mouth Disease Using a “Single-Cycle” Alphavirus Vector and Empty Capsid Particles. PLoS ONE 2016, 11, e0157435. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Stirling, C.M.A.; Denyer, M.S.; Hamblin, P.; Hutchings, G.; Takamatsu, H.-H.; Barnett, P. V Dramatic Improvement in FMD DNA Vaccine Efficacy and Cross-Serotype Antibody Induction in Pigs Following a Protein Boost. Vaccine 2008, 26, 2647–2656. [Google Scholar] [CrossRef]
- Colby, M.; Coats, M.; Brake, D.; Fine, J. The Role of the Department of Homeland Security, Science and Technology Directorate in the Development of Vaccines and Diagnostics for Transboundary Animal Diseases. Dev. Biol. 2013, 135, 3–14. [Google Scholar] [CrossRef]
- Martinez-Salas, E.; Ortin, J.; Domingo, E. Sequence of the Viral Replicase Gene from Foot-and-Mouth Disease Virus C1-Santa Pau (C-S8). Gene 1985, 35, 55–61. [Google Scholar] [CrossRef]
- García-Briones, M.M.; Blanco, E.; Chiva, C.; Andreu, D.; Ley, V.; Sobrino, F. Immunogenicity and T Cell Recognition in Swine of Foot-and-Mouth Disease Virus Polymerase 3D. Virology 2004, 322, 264–275. [Google Scholar] [CrossRef] [Green Version]
- Gerner, W.; Denyer, M.S.; Takamatsu, H.-H.; Wileman, T.E.; Wiesmüller, K.-H.; Pfaff, E.; Saalmüller, A. Identification of Novel Foot-and-Mouth Disease Virus Specific T-Cell Epitopes in c/c and d/d Haplotype Miniature Swine. Virus Res. 2006, 121, 223–228. [Google Scholar] [CrossRef]
- Collen, T.; Baron, J.; Childerstone, A.; Corteyn, A.; Doel, T.R.; Flint, M.; Garcia-Valcarcel, M.; Parkhouse, R.M.; Ryan, M.D. Heterotypic Recognition of Recombinant FMDV Proteins by Bovine T-Cells: The Polymerase (P3Dpol) as an Immunodominant T-Cell Immunogen. Virus Res. 1998, 56, 125–133. [Google Scholar] [CrossRef]
- Mayr, G.A.; Chinsangaram, J.; Grubman, M.J. Development of Replication-Defective Adenovirus Serotype 5 Containing the Capsid and 3C Protease Coding Regions of Foot-and-Mouth Disease Virus as a Vaccine Candidate. Virology 1999, 263, 496–506. [Google Scholar] [CrossRef] [Green Version]
- Ferrer-Orta, C.; de la Higuera, I.; Caridi, F.; Sanchez-Aparicio, M.T.; Moreno, E.; Perales, C.; Singh, K.; Sarafianos, S.G.; Sobrino, F.; Domingo, E.; et al. Multifunctionality of a Picornavirus Polymerase Domain: Nuclear Localization Signal and Nucleotide Recognition. J. Virol. 2015, 89, 6848–6859. [Google Scholar] [CrossRef] [Green Version]
- Sørensen, K.J.; Madsen, K.G.; Madsen, E.S.; Salt, J.S.; Nqindi, J.; Mackay, D.K.J. Differentiation of Infection from Vaccination in Foot-and-Mouth Disease by the Detection of Antibodies to the Non-Structural Proteins 3D, 3AB and 3ABC in ELISA Using Antigens Expressed in Baculovirus. Arch. Virol. 1998, 143, 1461–1476. [Google Scholar] [CrossRef] [Green Version]
- Kumar, R.; Hosamani, M.; Sreenivasa, B.P.; Kotyal, A.; Venkataramanan, R. Expression of Foot-and-Mouth Disease Virus Non-Structural Protein, 3D in Insect Cells and Its Application in Detection of Anti-FMDV Antibodies. Indian J. Virol. 2012, 23, 326–332. [Google Scholar] [CrossRef]
- Sumida, S.M.; Truitt, D.M.; Lemckert, A.A.C.; Vogels, R.; Custers, J.H.; Addo, M.M.; Lockman, S.; Peter, T.; Peyerl, F.W.; Kishko, M.G.; et al. Neutralizing Antibodies to Adenovirus Serotype 5 Vaccine Vectors Are Directed Primarily against the Adenovirus Hexon Protein. J. Immunol. 2005, 174, 7179–7185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradley, R.R.; Lynch, D.M.; Iampietro, M.J.; Borducchi, E.N.; Barouch, D.H. Adenovirus Serotype 5 Neutralizing Antibodies Target Both Hexon and Fiber Following Vaccination and Natural Infection. J. Virol. 2012, 86, 625–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salguero, F.J.; Sánchez-Martín, M.A.; Díaz-San Segundo, F.; de Avila, A.; Sevilla, N. Foot-and-Mouth Disease Virus (FMDV) Causes an Acute Disease That Can Be Lethal for Adult Laboratory Mice. Virology 2005, 332, 384–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berinstein, A.; Tami, C.; Taboga, O.; Smitsaart, E.; Carrillo, E. Protective Immunity against Foot-and-Mouth Disease Virus Induced by a Recombinant Vaccinia Virus. Vaccine 2000, 18, 2231–2238. [Google Scholar] [CrossRef]
- Rodríguez-Calvo, T.; Ojosnegros, S.; Sanz-Ramos, M.; García-Arriaza, J.; Escarmís, C.; Domingo, E.; Sevilla, N. New Vaccine Design Based on Defective Genomes That Combines Features of Attenuated and Inactivated Vaccines. PLoS ONE 2010, 5, e10414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carr, B.V.; Lefevre, E.A.; Windsor, M.A.; Inghese, C.; Gubbins, S.; Prentice, H.; Juleff, N.D.; Charleston, B. CD4+ T-Cell Responses to Foot-and-Mouth Disease Virus in Vaccinated Cattle. J. Gen. Virol. 2013, 94, 97–107. [Google Scholar] [CrossRef]
- Oh, Y.; Fleming, L.; Statham, B.; Hamblin, P.; Barnett, P.; Paton, D.J.; Park, J.-H.; Joo, Y.S.; Parida, S. Interferon-γ Induced by In Vitro Re-Stimulation of CD4+ T-Cells Correlates with In Vivo FMD Vaccine Induced Protection of Cattle against Disease and Persistent Infection. PLoS ONE 2012, 7, e44365. [Google Scholar] [CrossRef] [Green Version]
- Guzman, E.; Taylor, G.; Charleston, B.; Skinner, M.A.; Ellis, S.A. An MHC-Restricted CD8+ T-Cell Response Is Induced in Cattle by Foot-and-Mouth Disease Virus (FMDV) Infection and Also Following Vaccination with Inactivated FMDV. J. Gen. Virol. 2008, 89, 667–675. [Google Scholar] [CrossRef]
- Guzman, E.; Taylor, G.; Charleston, B.; Ellis, S.A. Induction of a Cross-Reactive CD8+ T Cell Response Following Foot-and-Mouth Disease Virus Vaccination. J. Virol. 2010, 84, 12375–12384. [Google Scholar] [CrossRef] [Green Version]
- Patch, J.R.; Pedersen, L.E.; Toka, F.N.; Moraes, M.; Grubman, M.J.; Nielsen, M.; Jungersen, G.; Buus, S.; Golde, W.T. Induction of Foot-and-Mouth Disease Virus-Specific Cytotoxic T Cell Killing by Vaccination. Clin. Vaccine Immunol. 2011, 18, 280–288. [Google Scholar] [CrossRef] [Green Version]
- Patch, J.R.; Kenney, M.; Pacheco, J.M.; Grubman, M.J.; Golde, W.T. Characterization of Cytotoxic T Lymphocyte Function after Foot-and-Mouth Disease Virus Infection and Vaccination. Viral Immunol. 2013, 26, 239–249. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Xu, F.; Liu, J.; Gao, B.; Liu, Y.; Zhai, Y.; Ma, J.; Zhang, K.; Baker, T.S.; Schulten, K.; et al. Atomic Model of Rabbit Hemorrhagic Disease Virus by Cryo-Electron Microscopy and Crystallography. PLoS Pathog. 2013, 9. [Google Scholar] [CrossRef] [Green Version]
- Bárcena, J.; Guerra, B.; Angulo, I.; González, J.; Valcárcel, F.; Mata, C.P.; Castón, J.R.; Blanco, E.; Alejo, A. Comparative Analysis of Rabbit Hemorrhagic Disease Virus (RHDV) and New RHDV2 Virus Antigenicity, Using Specific Virus-like Particles. Vet. Res. 2015, 46, 106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wickham, T.J.; Davis, T.; Granados, R.R.; Shuler, M.L.; Wood, H.A. Screening of Insect Cell Lines for the Production of Recombinant Proteins and Infectious Virus in the Baculovirus Expression System. Biotechnol. Prog. 1992, 8, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Condezo, G.N.; Marabini, R.; Ayora, S.; Carazo, J.M.; Alba, R.; Chillón, M.; San Martín, C. Structures of Adenovirus Incomplete Particles Clarify Capsid Architecture and Show Maturation Changes of Packaging Protein L1 52/55k. J. Virol. 2015, 89, 9653–9664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sobrino, F.; Dávila, M.; Ortín, J.; Domingo, E. Multiple Genetic Variants Arise in the Course of Replication of Foot-and-Mouth Disease Virus in Cell Culture. Virology 1983, 128, 310–318. [Google Scholar] [CrossRef]
- Toja, M.; Escarmís, C.; Domingo, E. Genomic Nucleotide Sequence of a Foot-and-Mouth Disease Virus Clone and Its Persistent Derivatives. Implications for the Evolution of Viral Quasispecies during a Persistent Infection. Virus Res. 1999, 64, 161–171. [Google Scholar] [CrossRef]
- Knowles, N.J.; Samuel, A.R.; Davies, P.R.; Midgley, R.J.; Valarcher, J.-F. Pandemic Strain of Foot-and-Mouth Disease Virus Serotype O. Emerg. Infect. Dis. 2005, 11, 1887–1893. [Google Scholar] [CrossRef]
- Mateu, M.G.; Rocha, E.; Vicente, O.; Vayreda, F.; Navalpotro, C.; Andreu, D.; Pedroso, E.; Giralt, E.; Enjuanes, L.; Domingo, E. Reactivity with Monoclonal Antibodies of Viruses from an Episode of Foot-and-Mouth Disease. Virus Res. 1987, 8, 261–274. [Google Scholar] [CrossRef]
- Arias, A.; Agudo, R.; Ferrer-Orta, C.; Pérez-Luque, R.; Airaksinen, A.; Brocchi, E.; Domingo, E.; Verdaguer, N.; Escarmís, C. Mutant Viral Polymerase in the Transition of Virus to Error Catastrophe Identifies a Critical Site for RNA Binding. J. Mol. Biol. 2005, 353, 1021–1032. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rangel, G.; Martín, V.; Bárcena, J.; Blanco, E.; Alejo, A. An Adenovirus Vector Expressing FMDV RNA Polymerase Combined with a Chimeric VLP Harboring a Neutralizing Epitope as a Prime Boost Strategy to Induce FMDV-Specific Humoral and Cellular Responses. Pharmaceuticals 2021, 14, 675. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14070675
Rangel G, Martín V, Bárcena J, Blanco E, Alejo A. An Adenovirus Vector Expressing FMDV RNA Polymerase Combined with a Chimeric VLP Harboring a Neutralizing Epitope as a Prime Boost Strategy to Induce FMDV-Specific Humoral and Cellular Responses. Pharmaceuticals. 2021; 14(7):675. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14070675
Chicago/Turabian StyleRangel, Giselle, Verónica Martín, Juan Bárcena, Esther Blanco, and Alí Alejo. 2021. "An Adenovirus Vector Expressing FMDV RNA Polymerase Combined with a Chimeric VLP Harboring a Neutralizing Epitope as a Prime Boost Strategy to Induce FMDV-Specific Humoral and Cellular Responses" Pharmaceuticals 14, no. 7: 675. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14070675






