Albumin Nanoparticle Formulation for Heart-Targeted Drug Delivery: In Vivo Assessment of Congestive Heart Failure
Abstract
:1. Introduction
2. Results
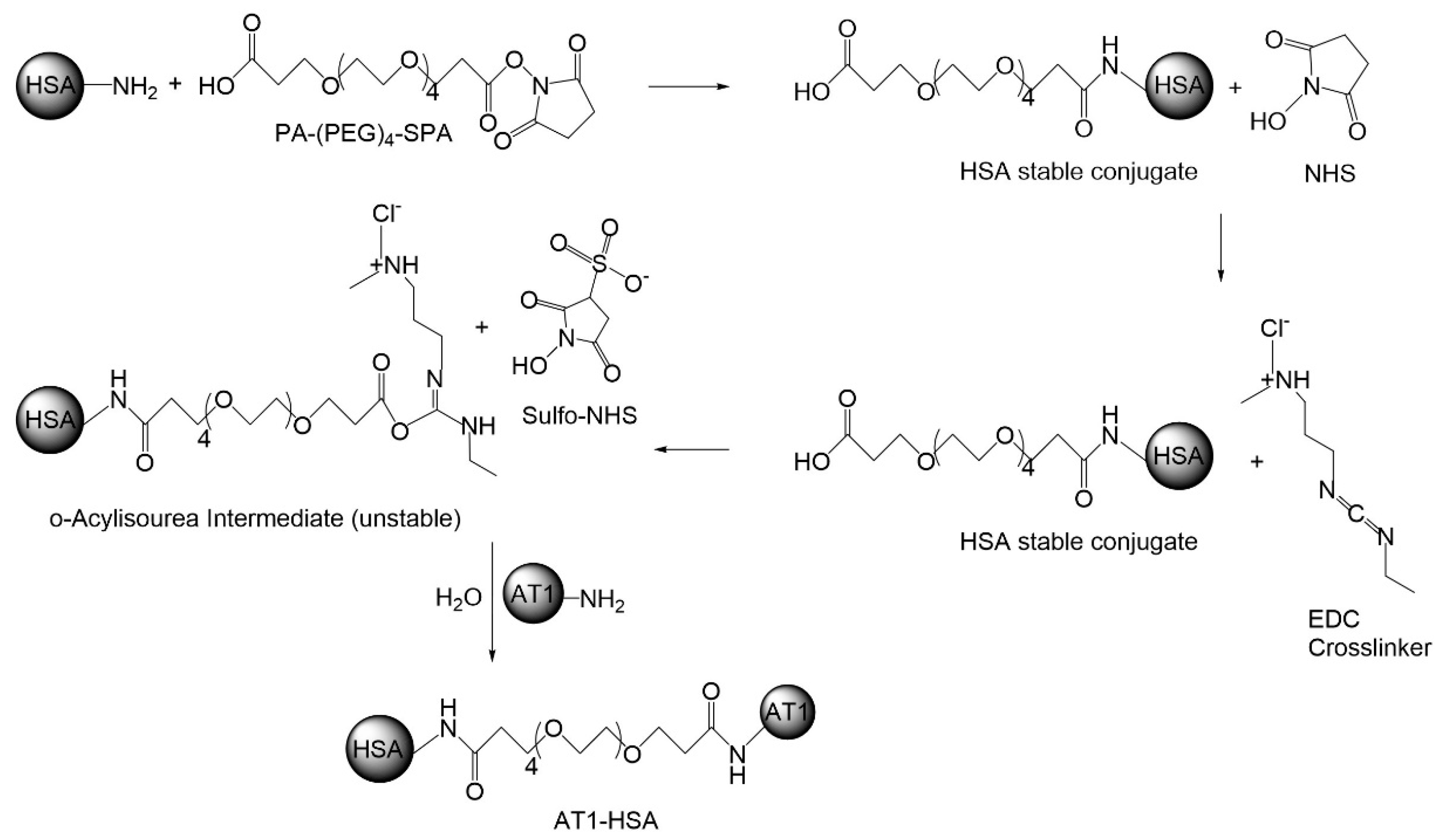
2.1. Synthesis of AT1-HSA-MRN-NPs
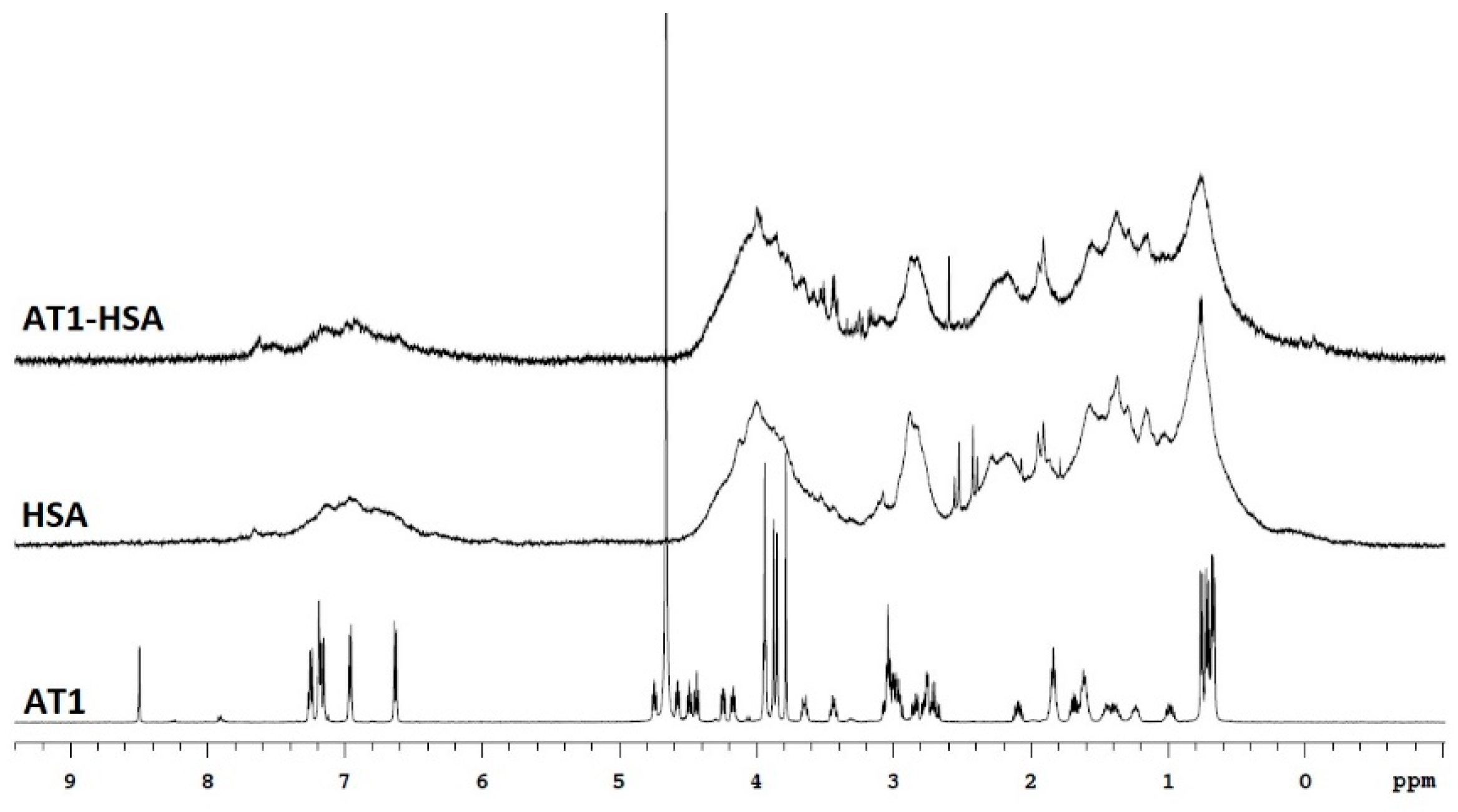
2.2. Nuclear Magnetic Resonance
2.3. Mass Spectrometry
2.4. Quantification of the AT1 Peptide
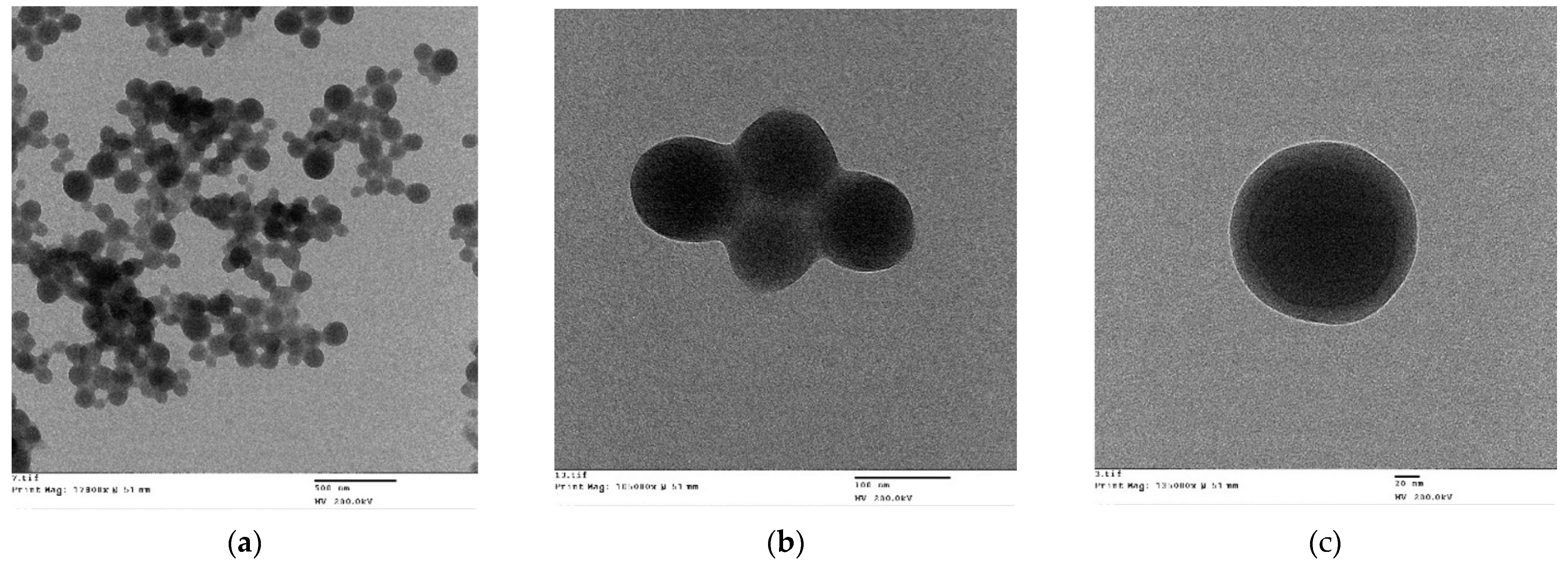
2.5. Characterization of the AT1-HSA-MRN-NPs
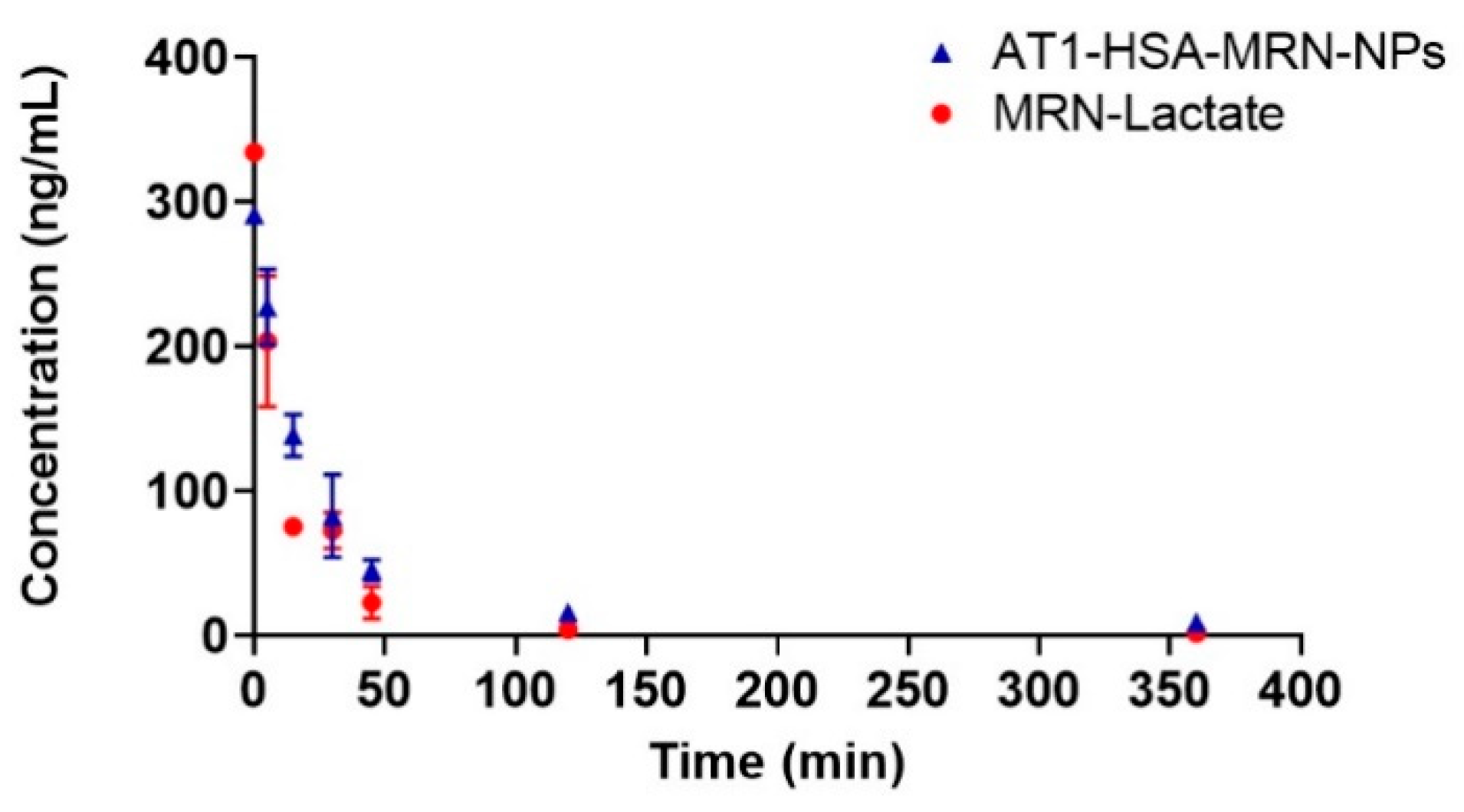
2.6. Pharmacokinetic Parametersv
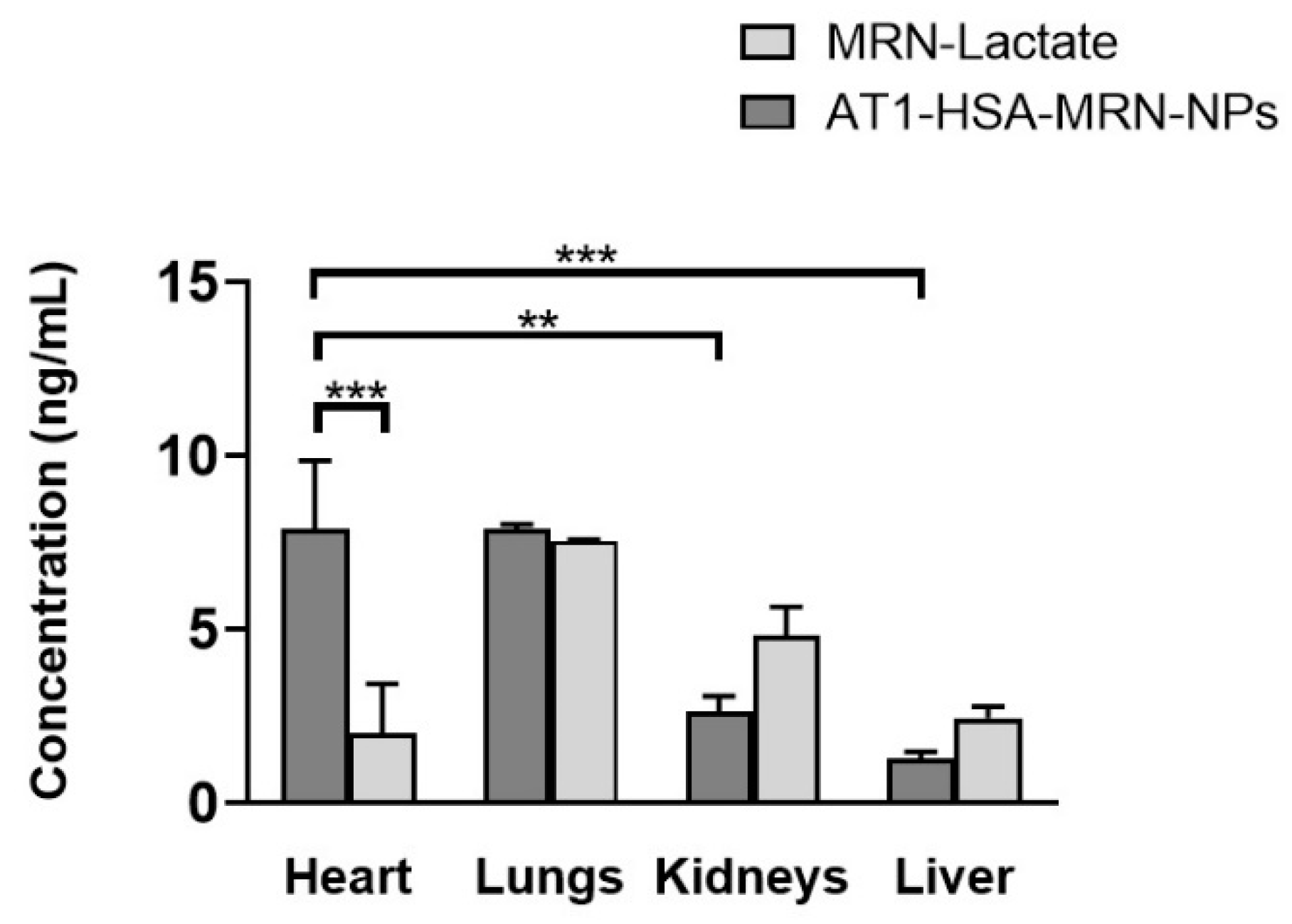
2.7. Tissue Distribution Study
2.8. Cardiac Function Assessment
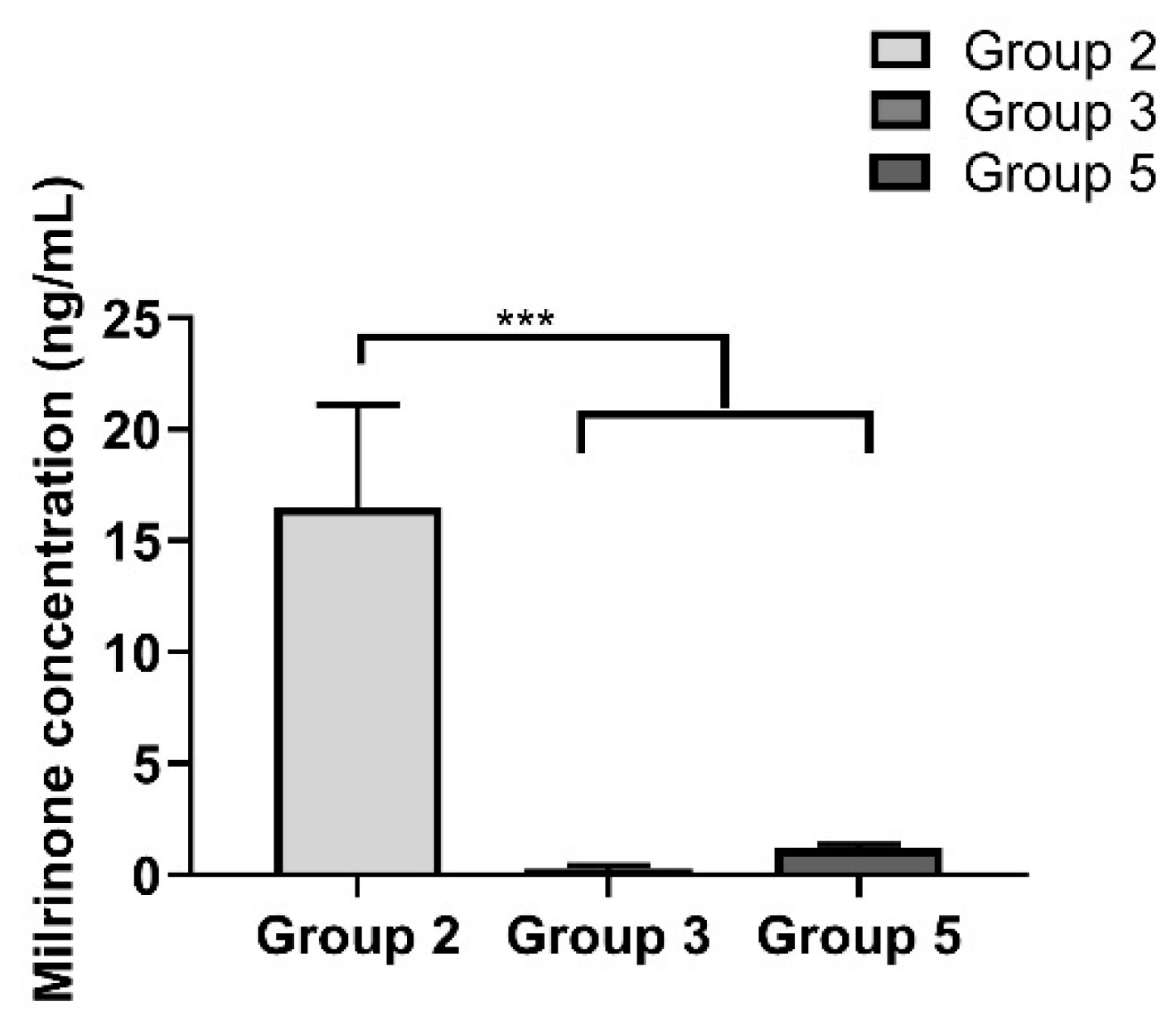
2.9. Milrinone Quantification from Rat Plasma
2.10. Safety and Toxicity of the AT1-HSA-MRN-NPs
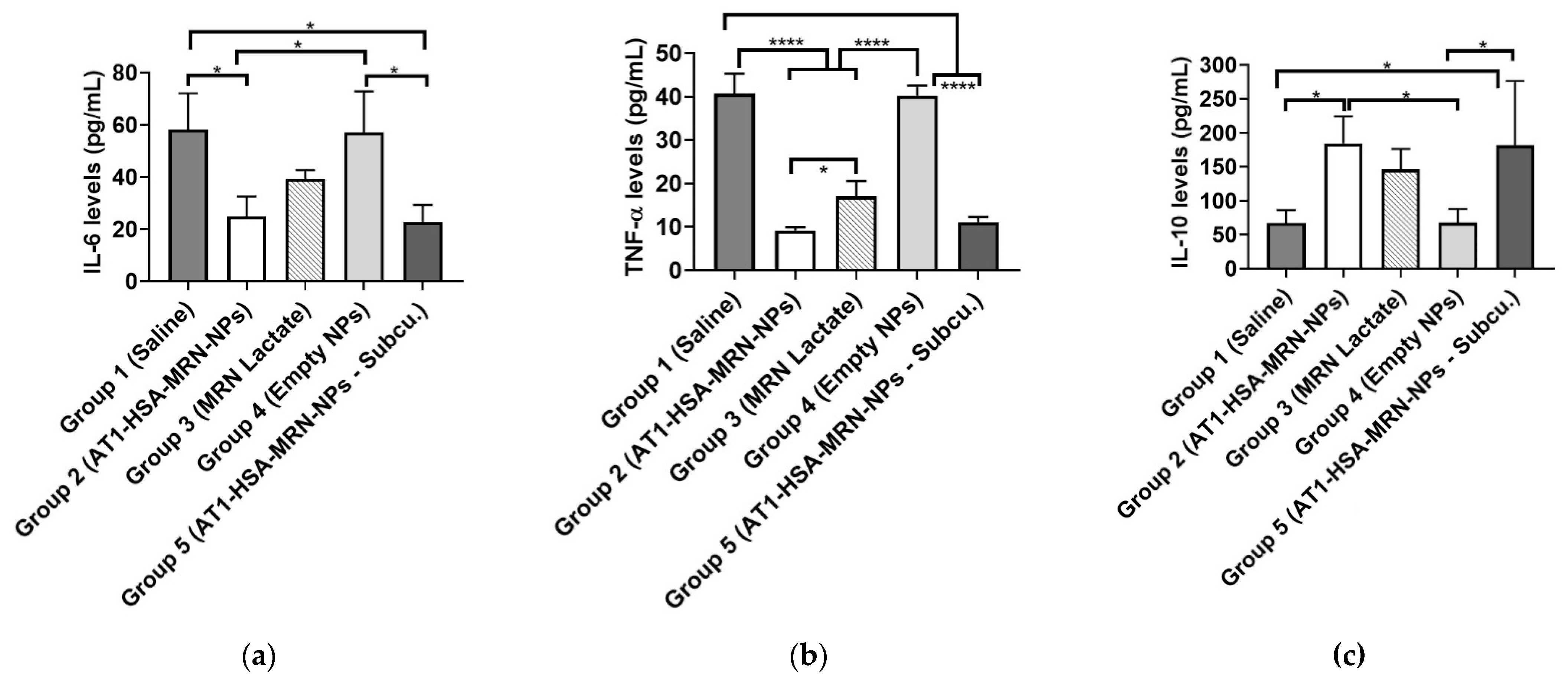
2.11. Serum Cytokine Measurements
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Synthesis of the AT1 Peptide
4.3. Surface Modification of HSA with AT1 Peptide
4.4. Nuclear Magnetic Resonance
4.5. Mass Spectrometry
4.6. Quantification of AT1 Peptide Attached to HSA
4.7. Nanoparticle Preparation
4.8. Nanoparticle Characterization
4.9. In Vivo Studies
4.10. Pharmacokinetics and Biodistribution Study
4.11. Ligation of the Left Anterior Descending Coronary Artery to Induce CHF
4.12. Animal Mortality
4.13. Blood Serum and Plasma Collection
4.14. Quantification of Milrinone from Rat Plasma
4.15. Echocardiography Procedure
4.16. Cytokine Measurement
4.17. Tissue Collection and Histological Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics—2018 Update: A Report From the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef]
- Benetis, R. Surgical treatment of congestive heart failure in coronary artery disease. Rocz. Akad. Med. w Bialymstoku (1995) 2005, 50. [Google Scholar]
- Giardiello, M.; Liptrott, N.J.; McDonald, T.O.; Moss, D.; Siccardi, M.; Martin, P.; Smith, D.; Gurjar, R.; Rannard, S.P.; Owen, A. Accelerated oral nanomedicine discovery from miniaturized screening to clinical production exemplified by paediatric HIV nanotherapies. Nat. Commun. 2016, 7, 13184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giménez, V.M.M.; Kassuha, D.E.; Manucha, W. Nanomedicine applied to cardiovascular diseases: Latest developments. Ther. Adv. Cardiovasc. Dis. 2017, 11, 133–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferreira, M.P.A.; Ranjan, S.; Kinnunen, S.; Correia, A.; Talman, V.; Mäkilä, E.; Barrios-Lopez, B.; Kemell, M.; Balasubramanian, V.; Salonen, J.; et al. Drug-Loaded Multifunctional Nanoparticles Targeted to the Endocardial Layer of the Injured Heart Modulate Hypertrophic Signaling. Small 2017, 13, 1701276. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.-Y.; Yang, Y.-J.; Chang, C.-H.; Tang, A.C.L.; Liao, W.-Y.; Cheng, F.-Y.; Yeh, C.-S.; Lai, J.J.; Stayton, P.S.; Hsieh, P.C.H. Functionalized nanoparticles provide early cardioprotection after acute myocardial infarction. J. Control. Release 2013, 170, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Diao, J.; Wang, H.; Chang, N.; Zhou, X.-H.; Zhu, X.; Wang, J.; Xiong, J.-W. PEG–PLA nanoparticles facilitate siRNA knockdown in adult zebrafish heart. Dev. Biol. 2015, 406, 196–202. [Google Scholar] [CrossRef] [Green Version]
- Hennig, R.; Goepferich, A.; Pollinger, K.; Tessmar, J. Multivalent targeting of AT1 receptors with angiotensin II-functionalized nanoparticles. J. Drug Target. 2015, 23, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Lomis, N.; Westfall, S.; Farahdel, L.; Malhotra, M.; Shum-Tim, D.; Prakash, S. Human Serum Albumin Nanoparticles for Use in Cancer Drug Delivery: Process Optimization and In Vitro Characterization. Nanomaterials 2016, 6, 116. [Google Scholar] [CrossRef] [Green Version]
- Lomis, N.; Gaudreault, F.; Malhotra, M.; Westfall, S.; Shum-Tim, D.; Prakash, S. Novel Milrinone Nanoformulation for Use in Cardiovascular Diseases: Preparation and in Vitro Characterization. Mol. Pharm. 2017, 15, 2489–2502. [Google Scholar] [CrossRef] [Green Version]
- Mudshinge, S.R.; Deore, A.; Patil, S.; Bhalgat, C.M. Nanoparticles: Emerging carriers for drug delivery. Saudi Pharm. J. 2011, 19, 129–141. [Google Scholar] [CrossRef] [Green Version]
- Blanco, E.; Shen, H.; Ferrari, M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat. Biotechnol. 2015, 33, 941–951. [Google Scholar] [CrossRef]
- Binsalamah, Z.M.; Paul, A.; Khan, A.A.; Prakash, S.; Shum-Tim, D. Intramyocardial sustained delivery of placental growth factor using nanoparticles as a vehicle for delivery in the rat infarct model. Int. J. Nanomed. 2011, 6, 2667. [Google Scholar]
- Paul, A.; Chen, G.; Khan, A.; Rao, V.T.S.; Shum-Tim, M.; Prakash, S. Genipin-Cross-Linked Microencapsulated Human Adipose Stem Cells Augment Transplant Retention Resulting in Attenuation of Chronically Infarcted Rat Heart Fibrosis and Cardiac Dysfunction. Cell Transplant. 2012, 21, 2735–2751. [Google Scholar] [CrossRef] [Green Version]
- Loureiro, A.; Azoia, N.G.; Gomes, A.C.; Cavaco-Paulo, A. Albumin-Based Nanodevices as Drug Carriers. Curr. Pharm. Des. 2016, 22, 1371–1390. [Google Scholar] [CrossRef] [PubMed]
- Dvir, T.; Bauer, M.; Schroeder, A.; Tsui, J.H.; Anderson, D.G.; Langer, R.; Liao, R.; Kohane, D.S. Nanoparticles Targeting the Infarcted Heart. Nano Lett. 2011, 11, 4411–4414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paradis, P.; Dali-Youcef, N.; Paradis, F.W.; Thibault, G.; Nemer, M. Overexpression of angiotensin II type I receptor in cardiomyocytes induces cardiac hypertrophy and remodeling. Proc. Natl. Acad. Sci. USA 2000, 97, 931–936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, J.; Carretero, O.A.; Lin, C.X.; Cavasin, M.A.; Shesely, E.G.; Yang, J.J.; Reudelhuber, T.L.; Yang, X.P. Role of cardiac overexpression of angiotensin II in the regulation of cardiac function and remodeling post-myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H1900–H1907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakano, Y.; Matoba, T.; Tokutome, M.; Funamoto, D.; Katsuki, S.; Ikeda, G.; Nagaoka, K.; Ishikita, A.; Nakano, K.; Koga, J.-I.; et al. Nanoparticle-Mediated Delivery of Irbesartan Induces Cardioprotection from Myocardial Ischemia-Reperfusion Injury by Antagonizing Monocyte-Mediated Inflammation. Sci. Rep. 2016, 6, 29601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, J.; Gu, C.; Cabigas, E.B.; Pendergrass, K.D.; Brown, M.E.; Luo, Y.; Davis, M.E. Functionalized dendrimer-based delivery of angiotensin type 1 receptor siRNA for preserving cardiac function following infarction. Biomaterials 2013, 34, 3729–3736. [Google Scholar] [CrossRef] [Green Version]
- Al Kindi, H.; Paul, A.; You, Z.; Nepotchatykh, O.; Schwertani, A.; Prakash, S.; Shum-Tim, D. Sustained release of milrinone delivered via microparticles in a rodent model of myocardial infarction. J. Thorac. Cardiovasc. Surg. 2014, 148, 2316–2324. [Google Scholar] [CrossRef] [Green Version]
- Lindsay, C.A.; Barton, P.; Lawless, S.; Kitchen, L.; Zorka, A.; Garcia, J.; Kouatli, A.; Giroir, B. Pharmacokinetics and pharmacodynamics of milrinone lactate in pediatric patients with septic shock. † 288. Pediatr. Res. 1996, 39, 50. [Google Scholar] [CrossRef] [Green Version]
- Friedman, S.E.C.A.R.L.A.D.; Claypool, S.; Liu, R. The Smart Targeting of Nanoparticles. Curr. Pharm. Des. 2013, 19, 6315–6329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, B.; He, X.Y.; Yi, X.Q.; Zhuo, R.X.; Cheng, S.X. Dual-Peptide-Functionalized Albumin-Based Nanoparticles with pH-Dependent Self-Assembly Behavior for Drug Delivery. ACS Appl. Mater. Interfaces 2015, 7, 15148–15153. [Google Scholar] [CrossRef] [PubMed]
- Bobo, D.; Robinson, K.J.; Islam, J.; Thurecht, K.J.; Corrie, S.R. Nanoparticle-Based Medicines: A Review of FDA-Approved Materials and Clinical Trials to Date. Pharm. Res. 2016, 33, 2373–2387. [Google Scholar] [CrossRef]
- Rivard, K.; Grandy, S.A.; Douillette, A.; Paradis, P.; Nemer, M.; Allen, B.G.; Fiset, C. Overexpression of type 1 angiotensin II receptors impairs excitation-contraction coupling in the mouse heart. Am. J. Physiol. Circ. Physiol. 2011, 301, H2018–H2027. [Google Scholar] [CrossRef] [Green Version]
- Fasano, M.; Curry, S.; Terreno, E.; Galliano, M.; Fanali, G.; Narciso, P.; Notari, S.; Ascenzi, P. The extraordinary ligand binding properties of human serum albumin. IUBMB Life 2005, 57, 787–796. [Google Scholar] [CrossRef]
- Merlot, A.M.; Kalinowski, D.S.; Richardson, D.R. Unraveling the mysteries of serum albumin—More than just a serum protein. Front. Physiol. 2014, 5, 299. [Google Scholar] [CrossRef] [Green Version]
- Hirn, S.; Semmler-Behnke, M.; Schleh, C.; Wenk, A.; Lipka, J.; Schäffler, M.; Takenaka, S.; Möller, W.; Schmid, G.; Simon, U.; et al. Particle size-dependent and surface charge-dependent biodistribution of gold nanoparticles after intravenous administration. Eur. J. Pharm. Biopharm. 2011, 77, 407–416. [Google Scholar] [CrossRef] [Green Version]
- Suen, W.-L.L.; Chau, Y. Size-dependent internalisation of folate-decorated nanoparticles via the pathways of clathrin and caveolae-mediated endocytosis in ARPE-19 cells. J. Pharm. Pharmacol. 2014, 66, 564–573. [Google Scholar] [CrossRef]
- Nanayakkara, S.; Byrne, M.; Mak, V.; Carter, K.; Dean, E.; Kaye, D.M. Extended-Release Oral Milrinone for the Treatment of Heart Failure with Preserved Ejection Fraction. J. Am. Heart Assoc. 2020, 9, e015026. [Google Scholar] [CrossRef]
- Ayres, J.K.; Maani, C.V. Milrinone, in StatPearls. StatPearls Publishing. 2019. Available online: https://0-www-ncbi-nlm-nih-gov.brum.beds.ac.uk/books/NBK532943/ (accessed on 1 July 2019).
- Chong, L.Y.Z.; Satya, K.; Kim, B.; Berkowitz, R. Milrinone Dosing and a Culture of Caution in Clinical Practice. Cardiol. Rev. 2018, 26, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Langer, K.; Balthasar, S.; Vogel, V.; Dinauer, N.; von Briesen, H.; Schubert, D. Optimization of the preparation process for human serum albumin (HSA) nanoparticles. Int. J. Pharm. 2003, 257, 169–180. [Google Scholar] [CrossRef]
- Langer, K.; Anhorn, M.G.; Steinhauser, I.; Dreis, S.; Celebi, D.; Schrickel, N.; Faust, S.; Vogel, V. Human serum albumin (HSA) nanoparticles: Reproducibility of preparation process and kinetics of enzymatic degradation. Int. J. Pharm. 2008, 347, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, M.R.; Tariq, A.; Ahmad, A.; Chaudhary, M.; Shrivastav, S.M.; Singh, R.K. Application of DDQ and p-Chloranilic Acid for the Spectrophotometric Estimation of Milrinone in Pharmaceutical Formulations. Asian J. Sci. Res. 2009, 2, 135–145. [Google Scholar] [CrossRef]
- Abbasi, S.; Paul, A.; Shao, W.; Prakash, S. Cationic Albumin Nanoparticles for Enhanced Drug Delivery to Treat Breast Cancer: Preparation and In Vitro Assessment. J. Drug Deliv. 2012, 2012, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Drexler, H.; Höing, S.; Faude, F.; Wollschläger, H.; Just, H. Central and regional vascular hemodynamics following intravenous milrinone in the conscious rat: Comparison with dobutamine. J. Cardiovasc. Pharmacol. 1987, 9, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.-H.; Wu, Y.; Nguyen, V.; Rastogi, S.; McConnell, B.K.; Wijaya, C.; Uretsky, B.F.; Poh, K.-K.; Tan, H.-C.; Fujise, K. Heart Protection by Combination Therapy with Esmolol and Milrinone at Late-Ischemia and Early Reperfusion. Cardiovasc. Drugs Ther. 2011, 25, 223–232. [Google Scholar] [CrossRef] [Green Version]
- Davani, S.; Marandin, A.; Mersin, N.; Royer, B.; Kantelip, B.; Hervé, P.; Etievent, J.-P.; Kantelip, J.-P. Mesenchymal Progenitor Cells Differentiate into an Endothelial Phenotype, Enhance Vascular Density, and Improve Heart Function in a Rat Cellular Cardiomyoplasty Model. Circulation 2003, 108, II-253. [Google Scholar] [CrossRef] [Green Version]
- Wykrzykowska, J.; Rosinberg, A.; Lee, S.U.; Voisine, P.; Wu, G.; Appelbaum, E.; Boodhwani, M.; Sellke, F.W.; Laham, R.J. Autologous Cardiomyotissue Implantation Promotes Myocardial Regeneration, Decreases Infarct Size, and Improves Left Ventricular Function. Circulation 2011, 123, 62–69. [Google Scholar] [CrossRef] [Green Version]




| MRN/AT1-HSA (w/w) | Nanoparticle Size (nm) | Zeta Potential (mV) | Encapsulation Efficiency (%) | Yield (%) |
|---|---|---|---|---|
| 1:10 | 190.2 ± 5.7 | −29.5 ± 3.7 | 41.8 ± 2.2 | 77 ± 2.3 |
| 1:20 | 205.6 ± 3.8 | −27.5 ± 4.6 | 40.4 ± 1.5 | 75 ± 2.6 |
| 1:40 | 225.4 ± 2.8 | −20.5 ± 4.4 | 54.1 ± 0.7 | 70 ± 3.5 |
| 1:80 | 245.6 ± 3.5 | −18.7 ± 6.6 | 83.2 ± 1.2 | 68 ± 4.6 |
| Time (min.) | AT1-HSA-MRN-NPs (ng/mL) | MRN Lactate (ng/mL) |
|---|---|---|
| 0 | 291.2 | 334.2 |
| 5 | 227.3 ± 26.2 | 203.5 ± 45.3 |
| 15 | 138.5 ± 14.5 | 75.4 ± 6.2 |
| 30 | 82.6 ± 28.5 | 72.6 ± 12.4 |
| 45 | 45.3 ± 7.1 | 22.9 ± 11.2 |
| 120 | 15.9 ± 3.5 | 4.1 ± 1.5 |
| 360 | 9.1 ± 0.9 | 1.6 ± 0.1 |
| Pharmacokinetic Parameters | MRN Dose: 50 μg/kg | |
|---|---|---|
| MRN-Lactate | AT1-HSA-MRN-NPs | |
| C0 (ng/mL) | 203.5 | 291.2 |
| Cmax (ng/mL) | 334.3 | 227.3 |
| t1/2 (min) | 64.7 | 101.3 |
| MRT (min) | 49.1 | 123.7 |
| AUC0-t (ng*h/mL) | 104.3 | 183.9 |
| AUC0-∞ (ng*h/mL) | 106.7 | 206.1 |
| Vz (L/kg) | 0.73 | 0.59 |
| Vss (L/kg) | 0.38 | 0.5 |
| CL (L/(kg*h)) | 0.47 | 0.24 |
| Left Ventricular Ejection Fraction (LVEF) Shown as % | |||||
|---|---|---|---|---|---|
| Group 1 (Control) | Group 2 (AT1-HSA-MRN-NPs—i.v. Injection) | Group 3 (MRN Lactate—i.v. Injection) | Group 4 (Empty NPs) | Group 5 AT1-HSA-MRN-NPs—Subcutaneous Injection) | |
| Baseline—Pre-Ligation | 88.8 ± 2.1 | 89.9 ± 1.3 | 88.2 ± 1.8 | 88.4 ± 0.9 | 74.9 ± 1.7 |
| 48 h Post Ligation | 69.1 ± 2.0 | 66.1 ± 1.9 | 65.3 ± 2.3 | 69.1 ± 2.2 | 66.4 ± 3.3 |
| 60 min Post Injection | 68.6 ± 2.2 | 84.3 ± 2.9 *** | 80.1 ± 3.3 ** | 70.1 ± 2.3 | 79.2 ± 2.7 ** |
| 24 h Post Injection | 67.1 ± 2.1 | 84.2 ± 4.8 ** | 70.6 ± 3.6 | 67.5 ± 2.5 | 75.5 ± 2.6 ** |
| 48 h Post Injection | 67.7 ± 1.8 | 83.1 ± 3.6 ** | 64.8 ± 4.3 | 64.9 ± 2.7 | 72.7 ± 2.3 |
| 1-week Post Injection | 66.7 ± 1.1 | 74.5 ± 2.1 ** | 66.1 ± 4.2 | 67.2 ± 2.9 | 73.3 ± 2.9 * |
| Left Ventricular Fractional Shortening (LVFS) Shown as % | |||||
|---|---|---|---|---|---|
| Group 1 (Control) | Group 2 (AT1-HSA-MRN-NPs—i.v. Injection) | Group 3 (MRN Lactate—i.v. Injection) | Group 4 (Empty NPs) | Group 5 AT1-HSA-MRN-NPs—Subcutaneous Injection) | |
| Baseline—Pre-Ligation | 52.6 ± 2.9 | 53.6 ± 2.1 | 52.6 ± 2.7 | 51.1 ± 1.3 | 54.6 ± 2.2 |
| 48 h Post Ligation | 33.1 ± 1.5 | 29.8 ± 1.0 | 34.3 ± 2.7 | 31.2 ± 1.3 | 30.7 ± 2.5 |
| 60 min Post Injection | 32.8 ± 1.7 | 50.1 ± 3.8 ** | 45.6 ± 3.2 ** | 34.7 ± 4.0 | 47.1 ± 3.9 ** |
| 24 h Post Injection | 31.5 ± 1.2 | 50.4 ± 3.1 *** | 33.6 ± 3.9 | 30.9 ± 2.4 | 40.5 ± 2.8 ** |
| 48 h Post Injection | 31.7 ± 1.0 | 46.5 ± 3.1 ** | 30.2 ± 3.9 | 30.1 ± 1.5 | 34.8 ± 1.7 |
| 1-week Post Injection | 31.3 ± 1.5 | 37.0 ± 2.7 | 30.8 ± 2.8 | 29.6 ± 1.1 | 35.9 ± 3.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lomis, N.; Sarfaraz, Z.K.; Alruwaih, A.; Westfall, S.; Shum-Tim, D.; Prakash, S. Albumin Nanoparticle Formulation for Heart-Targeted Drug Delivery: In Vivo Assessment of Congestive Heart Failure. Pharmaceuticals 2021, 14, 697. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14070697
Lomis N, Sarfaraz ZK, Alruwaih A, Westfall S, Shum-Tim D, Prakash S. Albumin Nanoparticle Formulation for Heart-Targeted Drug Delivery: In Vivo Assessment of Congestive Heart Failure. Pharmaceuticals. 2021; 14(7):697. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14070697
Chicago/Turabian StyleLomis, Nikita, Ziyab K. Sarfaraz, Aiman Alruwaih, Susan Westfall, Dominique Shum-Tim, and Satya Prakash. 2021. "Albumin Nanoparticle Formulation for Heart-Targeted Drug Delivery: In Vivo Assessment of Congestive Heart Failure" Pharmaceuticals 14, no. 7: 697. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14070697






