The Beneficial Effects of Traditional Chinese Exercises for Adults with Low Back Pain: A Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
2.4. Synthesized Analysis
3. Results
3.1. Search Results
3.2. Study Characteristics and Quality
3.3. Synthesis of Results
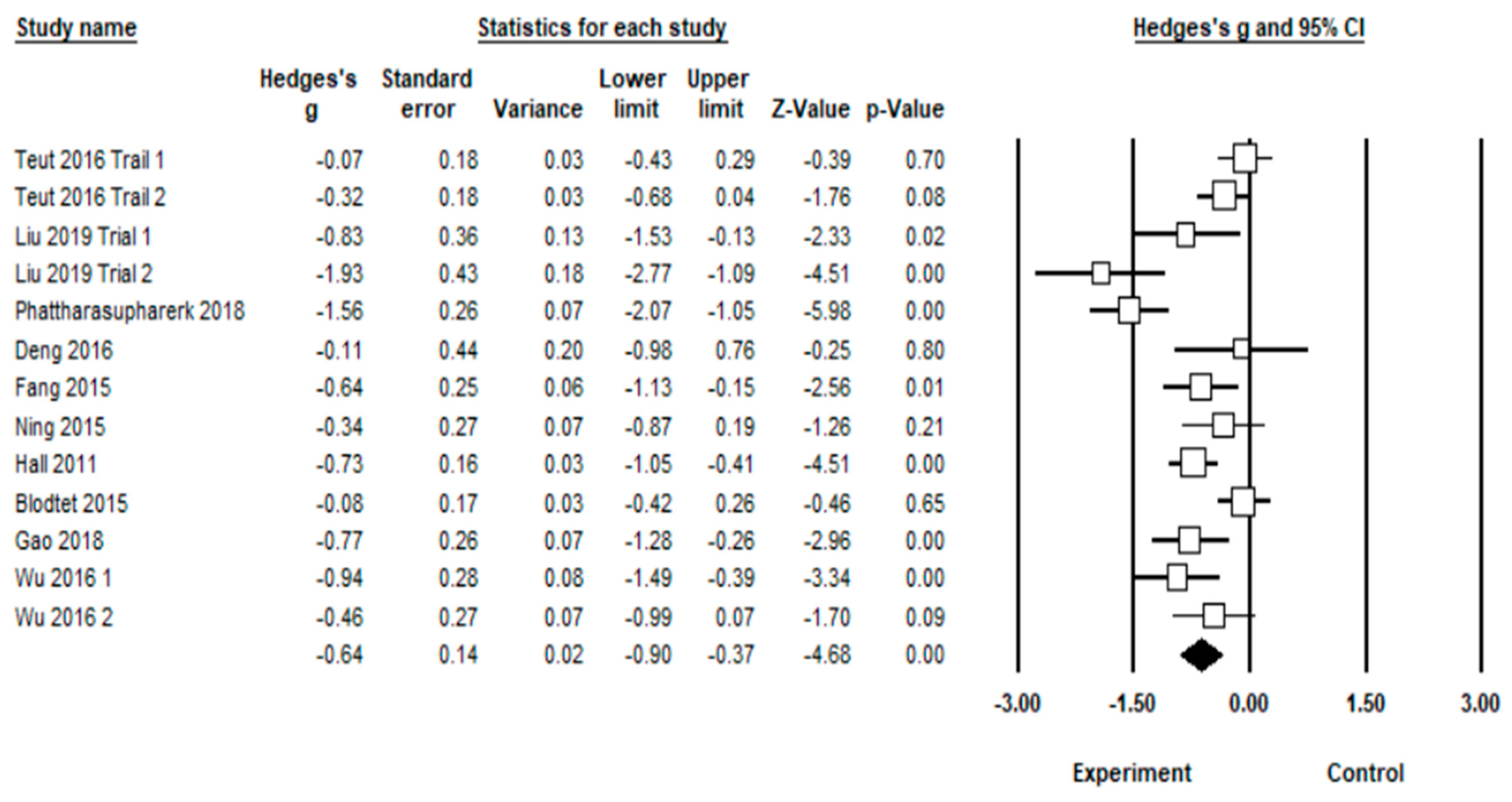
3.3.1. Effect of TCE on Pain Intensity
3.3.2. Effects of MBE on RMDQ and ODI
3.3.3. Moderator Analysis
3.3.4. Meta-Regression
3.3.5. Publication Bias
4. Discussion
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Koes, B.W.; Van, T.; Thomas, S. Diagnosis and treatment of low back pain. J. Orthop. Trauma 2006, 332, 1430–1434. [Google Scholar] [CrossRef] [Green Version]
- Croft, P.; Ferreira, M.; Kongsted, A.; Anema, J.R.; Chou, R.; Ferreira, P.H.; Koes, B.W.; Woolf, A.; Menezes Costa, L.; Louw, Q. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [Green Version]
- Maher, C.G.; Pereira, L.S.M.; Stevens, M.L.; Steffens, D.; Hancock, M.J.; Oliveira, V.C.; Chapple, M.; Teixeira-Salmela, L.F. Prevention of low back pain. JAMA Intern. Med. 2016, 176, 199. [Google Scholar]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef] [Green Version]
- Van-Middelkoop, M.; Rubinstein, S.M.; Verhagen, A.P.; Ostelo, R.W.; Koes, B.W.; Van-Tulder, M.W. Exercise therapy for chronic nonspecific low-back pain. Best Pract. Res. Clin. Rheumatol. 2010, 24, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; Tulder, M.W.; Tomlinson, G. Systematic review: Strategies for using exercise therapy to improve outcomes in chronic low back pain. Anna. Inter. Med. 2005, 9, 776–785. [Google Scholar] [CrossRef]
- Holtzman, S.; Rt, B. Yoga for chronic low back pain: A meta-analysis of randomized controlled trials. Pain Res. Manag. 2013, 18, 267–273. [Google Scholar] [CrossRef]
- Smeets, R.J.E.M.; Machado, L.A.C.; Ferreira, P.H.; Kamper, S.J.; Ferreira, M.L. Can we explain heterogeneity among randomized clinical trials of exercise for chronic back pain? A meta-regression analysis of randomized controlled trials. Phys. Ther. 2010, 90, 1383–1403. [Google Scholar] [CrossRef]
- Searle, A.; Spink, M.; Ho, A.; Chuter, V. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin. Rehabil. 2015, 29, 1155–1167. [Google Scholar] [CrossRef]
- Cho, H.; Kim, E.; Kim, J. Effects of the CORE exercise program on pain and active range of motion in patients with chronic low back pain. J. Phys. Ther. Sci. 2014, 26, 1237–1240. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Zhang, Y.; Liu, Y.; Tian, X.; Xiao, T.; Liu, X.; Yeung, A.S.; Liu, J.; Wang, X.; Yang, Q. The effects of Tai Chi Chuan versus core stability training on lower-limb neuromuscular function in aging individuals with non-specific chronic lower back pain. Medicina 2019, 55, 60. [Google Scholar] [CrossRef]
- Zou, L.; Wang, C.; Chen, K.; Shu, Y.; Chen, X.; Luo, L.; Zhao, X. The effect of Taichi practice on attenuating bone mineral density loss: A systematic review and meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2017, 14, 1000. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Yeung, A.; Quan, X.; Hui, S.C.; Hu, X.; Chan, J.S.M.; Wang, C.; Boyden, S.D.; Sun, L.; Wang, H. Mindfulness-based Baduanjin exercise for depression and anxiety in people with physical or mental illnesses: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2018, 15, 321. [Google Scholar] [CrossRef]
- Zou, L.; Wang, C.; Chen, X.; Wang, H. Baduanjin exercise for stroke rehabilitation: A systematic review with meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2018, 15, 600. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Yeung, A.; Zeng, N.; Wang, C.; Sun, L.; Thomas, G.A.; Wang, H. Effects of mind-body exercises for mood and functional capabilities in patients with stroke: An analytical review of randomized controlled trials. Int. J. Environ. Res. Public Health 2018, 15, 721. [Google Scholar] [CrossRef]
- Zou, L.; Yeung, A.; Li, C.; Chiou, S.Y.; Zeng, N.; Tzeng, H.M.; Wang, L.; Ren, Z.; Dean, T.; Thomas, G.A. Effects of mind–body movements on balance function in stroke survivors: A meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2018, 15, 1292. [Google Scholar] [CrossRef]
- Zou, L.; Yeung, A.; Li, C.; Wei, G.X.; Chen, K.W.; Kinser, P.A.; Chan, J.S.M.; Ren, Z. Effects of meditative movements on major depressive disorder: A systematic review and meta-analysis of randomized controlled trials. J. Clin. Med. 2018, 7, 195. [Google Scholar] [CrossRef]
- Zou, L.; Wang, C.; Tian, Z.; Wang, H.; Shu, Y. Effect of Yang-Style Tai Chi on gait parameters and musculoskeletal flexibility in healthy Chinese older women. Sports 2017, 5, 52. [Google Scholar] [CrossRef]
- Liu, S.J.; Ren, Z.; Wang, L.; Wei, G.X.; Zou, L. Mind–body (Baduanjin) exercise prescription for chronic obstructive pulmonary disease: A systematic review with meta-analysis. Int. J. Environ. Res. Public Health 2018, 15, 1830. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Sasaki, J.E.; Wei, G.-X.; Huang, T.; Yeung, A.S.; Neto, O.B.; Chen, K.W.; Hui, S.-C. Effects of mind–body exercises (Tai Chi/Yoga) on heart rate variability parameters and perceived stress: A systematic review with meta-analysis of randomized controlled trials. J. Clin. Med. 2018, 7, 404. [Google Scholar] [CrossRef]
- Zou, L.; Loprinzi, P.D.; Yeung, A.S.; Zeng, N.; Huang, T. The beneficial effects of mind-body exercises for people with mild cognitive impairment: A systematic review with meta-analysis. Arch Phys Med Rehabil. 2019. S0003-9993(19)30239-30244. [Google Scholar] [CrossRef] [PubMed]
- Phattharasupharerk, S.; Purepong, N.; Eksakulkla, S.; Siriphorn, A. Effects of Qigong practice in office workers with chronic non-specific low back pain: A randomized control trial. J. Bodywork Move. Ther. 2018, 2, 1–7. [Google Scholar] [CrossRef]
- Liu, J.; Yeung, A.; Xiao, T.; Tian, X.; Kong, Z.; Zou, L.; Wang, X. Chen-Style Tai Chi for individuals (aged 50 years old or above) with chronic non-specific low back pain: A randomized controlled trial. Int. J. Environ. Res. Public Health 2019, 16, 517. [Google Scholar] [CrossRef]
- Li, H.; Di, G.; Liu, S.; Zhang, W.; Si, J.; Wang, J.; Si, J.; Zhai, J. Baduanjin exercise for low back pain: A systematic review and meta-analysis. Complement. Ther. Med. 2019, 43, 109–116. [Google Scholar] [CrossRef]
- Maher, C.; Sherrington, C.; Herbert, R.; Moseley, A.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Hedges, L.V.; Higgin, J.T.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Chichester, UK, 2009. [Google Scholar]
- Boonstra, A.M.; Preuper, H.R.S.; Balk, G.A.; Stewart, R.E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014, 155, 2545–2550. [Google Scholar] [CrossRef]
- Hall, A.M.; Maher, C.G.; Lam, P.; Ferreira, M.; Latimer, J. Tai Chi exercise for treatment of pain and disability in people with persistent low back pain: A randomized controlled trial. Arthritis Care Res. 2011, 63, 1576–1583. [Google Scholar] [CrossRef] [PubMed]
- Blödt, S.; Pach, D.; Kaster, T.; Lüdtke, R.; Icke, K.; Reisshauer, A.; Witt, C.M. Qigong versus exercise therapy for chronic low back pain in adults—A randomized controlled non-inferiority trial. Eur. J. Pain 2015, 19, 123–131. [Google Scholar] [CrossRef]
- Fang, L.; Yan, J.; Cao, Y.; Zhang, G. The efect of Wuqinxi Exercise on mechanics characteristic of abdominal and back muscles and pain in patients with chronic nonspecific low back pain. Shanghai J. Tradit. Chin. Med. 2015, 49, 49–53. [Google Scholar]
- Ning, X.; Wu, L.; Wang, T.; He, X.; Yu, Y. Clinical study on five mimic—Animal boxing combined with core muscular strength exercise for the treatment of nonspecific low back pain. J. Tradit. Chin. Orthop. Traumatol. 2015, 27, 25–28. [Google Scholar]
- Teut, M.; Knilli, J.; Daus, D.; Roll, S.; Witt, C.M. Qigong or yoga versus no intervention in older adults with chronic low back pain—A randomized controlled trial. J. Pain 2016, 17, 796–805. [Google Scholar] [CrossRef]
- Wu, L. The clinical research of chronic non-specific low back pain which based on the theory of muscle imbalance. Chengdu Tradit. Chin. Univ. 2016, 5, 1–44. [Google Scholar]
- Deng, P. Preliminary study on the improvement of traditional exercise on relieving pain of patients with low back pain and dysfunction. Phys. Educ. Rev. 2016, 35, 89–91. [Google Scholar]
- Gao, F.; Yuan, S.; Liu, N.; Zheng, S. Effect observation of Baduanjin training on chronic nonspecific low back pain. Rehabil. Med. 2018, 28, 13–17. [Google Scholar]
- Liu, J.; Zhao, W.; Yuan, Y. Effects of Tai Chi on the event-related potential of patients with chronic non-specific low back pain. Chin. J. Sport. Med. 2018, 37, 826–832. [Google Scholar]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Ostelo, R.W.J.G.; de Vet, H.C.W. Clinically important outcomes in low back pain. Best Pract. Res. Clin. Rheumatol. 2005, 19, 593–607. [Google Scholar] [CrossRef] [PubMed]
- Munafò, M.R.; Flint, J. Meta-analysis of genetic association studies. Ann. Lab. Med. 2015, 35, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core stability exercise principles. Curr. Sports Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Wang, H.; Xiao, Z.; Fang, Q.; Zhang, M.; Li, T.; Du, G.; Liu, Y. Tai Chi for health benefits in patients with multiple sclerosis: A systematic review. PLoS ONE 2017, 12, 45–63. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, B.; Dalby, P.; Belfer, I.; Bergese, S.D. Mechanism of pain relief through Tai Chi and Qigong. J. Pain Reli. 2013, 2, 115. [Google Scholar]
- Zou, L.; Yeung, A.; Quan, X.; Boyden, S.D.; Wang, H. A systematic review and meta-analysis of mindfulness-based (Baduanjin) exercise for alleviating musculoskeletal pain and improving sleep quality in people with chronic diseases. Int. J. Environ. Res. Public Health 2018, 15, 206. [Google Scholar] [CrossRef] [PubMed]
- Gordon, R.; Bloxham, S. A systematic review of the effects of exercise and physical activity on non-specific chronic low back pain. Healthcare 2016, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Masharawi, Y.; Nadaf, N. The effect of non-weight bearing group-exercising on females with non-specific chronic low back pain: A randomized single blind controlled pilot study. J. Back Musculoskelet. Rehabil. 2013, 26, 353–359. [Google Scholar] [CrossRef] [PubMed]

| Study | Participants | Interventions | Outcomes Measured | Safety | ||||
|---|---|---|---|---|---|---|---|---|
| Publication Year | Status | Sample size | Age (years) | Experiment | Control | Duration | Primary and/or | Adverse |
| (PI) | (female, male) | secondary outcome | effect | |||||
| Phattharasupharerket al., (2018) [23] | LBP (50) | 72 | 35.2 | 1 × 60 min/week + daily practice Qigong | Waitlist | 6 weeks | Pain intensity (VAS), | No |
| E = 36; C = 36 | Low back pain disability (RMDQ) | |||||||
| Liu et al., (2019) [24] | LBP (57) | 43 | 74 | 3 × 60 min/week | C1: Core training | 12 weeks | Pain intensity (VAS) | No |
| E = 15; C1 = 15; C2 = 13 | Tai Chi | C2: no intervention | ||||||
| Hall et al., (2011) [29] | LBP (50) | 160 | 44 | 2 × 40 min/week | Wait-list | 10 weeks | Pain intensity (NRS), | No |
| E = 80; C = 80 | Tai Chi | Low back pain disability (RMDQ) | ||||||
| Blödt et al., (2015) [30] | LBP (56) | 127 | 46.7 | 1 × 90 min/week, | 1 × 60 min/week | 12 weeks | Pain intensity (VAS), | Dizziness (n = 12) |
| E = 64; C = 63 | Qigong | Strengthening | Low back pain disability (RMDQ | Increased pain (n = 2) | ||||
| Ning et al., (2015) [31] | LBP (58) | 52 | 41.4 | 3 × 30 min/week, | 3 × 30 min/week | 12 weeks | Pain intensity (VAS), | No |
| E = 26; C = 26 | Wuqinxi | Core training | Low back pain disability (ODI) | |||||
| Fang et al., (2015) [32] | LBP (52) | 63 | 53.4 | 3–4 × 45 min/week, | 3–4 × 45 min/week, | 24 weeks | Pain intensity (VAS) | No |
| E = 32; C = 31 | Wuqinxi | McKenzie training | ||||||
| Deng (2016) [33] | LBP (70) | 15 | 50.4 | 2 × 20 min/day | 1 × 20 min/day | 2 weeks | Pain intensity (VAS), | No |
| E = 8; C = 7 | Yijinjing | Acupuncture | Low back pain disability (MRMQ) | |||||
| Teut et al., (2016) [34] | LBP (51) | 176 | 73 | 1 × 90 min/week, | C1: 2 × 45 min/week | 12 weeks | Pain intensity (VAS) | No |
| E = 58; C1 = 61; C2 = 57 | Qigong | Yoga; C2: Waitlist | ||||||
| Wu 2016 [35] | LBP 53 | 78 | 39 | 3 × 30–35 min/week, | C1: 3 × 30–40 min/week (SB) | 12 weeks | Pain intensity (VAS), | No |
| E = 26; C1 = 26; C2 = 26 | Wuqinxi | C2: 3 × 30–40 min/week (CT) | Low back pain disability (ODI) | |||||
| Gao et al., (2018) [36] | LBP (76) | 60 | 36 | 2 × 30 min/day, | Usual care | 8 weeks | Pain intensity (VAS), | No |
| E = 30; C = 30 | Baduanjin | Low back pain disability (ODI) | ||||||
| Liu et al., (2018) [37] | LBP (31) | 40 | 57 | 3 × 60 min/week | C1: Core training | 12 weeks | Low back pain disability (ODI) | No |
| E = 14; C1 = 13; C2 = 13 | Tai Chi | C2: no intervention | ||||||
| Study | Score | Methodological Quality | PEDro Item Number | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |||
| Phattharasupharerk et al. 2018 [23] | 8 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Liu et al. 2019 [24] | 7 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Hall et al. 2011 [29] | 8 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Blödt et al. 2015 [30] | 8 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Ning et al. 2015 [31] | 8 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Fang et al. 2015 [32] | 8 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Deng 2016 [33] | 7 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Teut et al. 2016 [34] | 8 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Wu 2016 [35] | 8 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Gao et al. 2018 [36] | 7 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Liu et al. 2018 [37] | 7 | Good | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Studies were classified as having excellent (9–10), good (6–8), fair (4–5), or poor (<4). | |||||||||||||
| Outcomes | Number of Trials | Meta-Analysis | Heterogeneity | ||||
|---|---|---|---|---|---|---|---|
| Hedges’g | 95% CI | p-Value | I2 % | Q-Value | df(Q) | ||
| RMDQ | 4 | −0.41 | −0.79 to −0.03 | 0.03 | 66.1% | 8.86 | 3 |
| ODI | 5 | −0.96 | −1.42 to −0.50 | 0.00 | 67.5% | 12.32 | 4 |
| Categorical Moderator | Outcome | Level | No. of Studies/ Comparisons | Hedges’ g | 95% Confidence Interval | I2, % | Test for Between-Group Heterogeneity | ||
| Q-Value | df(Q) | p-Value | |||||||
| Study design moderators | |||||||||
| Control Type | VAS | Active | 8 | −0.40 | −0.64 to −0.15 | 45.2 % | 4.50 | 1 | 0.03 |
| Passive | 5 | −0.99 | −1.48 to −0.50 | 82.3% | |||||
| Allocation Concealment | VAS | Yes | 7 | −0.34 | −0.57 to −0.12 | 65.2% | 8.73 | 1 | 0.01 |
| No | 6 | −1.04 | −1.45 to −0.64 | 49.7% | |||||
| Baseline pain intensity | VAS | Moderate | 8 | −0.57 | −0.90 to −0.25 | 79.2% | 0.40 | 1 | 0.53 |
| Severe | 5 | −0.77 | −1.28 to −0.26 | 66.7% | |||||
| Exercise moderators | |||||||||
| Exercise Type | VAS | TC | 9 | −0.87 | −1.38 to −0.36 | 69.9% | 1.15 | 1 | 0.28 |
| Qigong | 4 | −0.54 | −0.86 to −0.23 | 75.9% | |||||
| Frequency | VAS | 1–2 | 5 | −0.53 | −0.98 to −0.07 | 86.8% | |||
| 3–4 | 6 | −0.78 | −1.15 to −0.42 | 57.3% | 0.90 | 2 | 0.64 | ||
| ≥5 | 2 | −0.54 | −1.16 to 0.08 | 39.6% | |||||
| Exercise session time | VAS | ≤45 | 7 | −0.64 | −0.82 to −0.46 | 0% | 0.10 | 1 | 0.75 |
| >45 | 6 | −0.73 | −1.26 to −0.19 | 87.6% | |||||
| Continuous Moderator | Outcome | No. of Studies/ Comparisons | 95% Confidence Interval | Q-Value | df(Q) | p-Value | |||
| Age | VAS | 13 | 0.01036 | 0.00163 to 0.01909 | 5.41 | 1 | 0.02 | ||
| Total exercise of time | VAS | 13 | −0.00020 | −0.00036 to −0.00005 | 6.79 | 1 | 0.01 | ||
| Pain intensity of participants | VAS | 13 | −0.00016 | −0.01902 to 0.01871 | 0.01 | 1 | 0.99 | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Loprinzi, P.D.; Yang, L.; Liu, J.; Liu, S.; Zou, L. The Beneficial Effects of Traditional Chinese Exercises for Adults with Low Back Pain: A Meta-Analysis of Randomized Controlled Trials. Medicina 2019, 55, 118. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina55050118
Zhang Y, Loprinzi PD, Yang L, Liu J, Liu S, Zou L. The Beneficial Effects of Traditional Chinese Exercises for Adults with Low Back Pain: A Meta-Analysis of Randomized Controlled Trials. Medicina. 2019; 55(5):118. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina55050118
Chicago/Turabian StyleZhang, Yanjie, Paul D. Loprinzi, Lin Yang, Jing Liu, Shijie Liu, and Liye Zou. 2019. "The Beneficial Effects of Traditional Chinese Exercises for Adults with Low Back Pain: A Meta-Analysis of Randomized Controlled Trials" Medicina 55, no. 5: 118. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina55050118





