Predominant Complications of Type 2 Diabetes in Kumasi: A 4-Year Retrospective Cross-Sectional Study at a Teaching Hospital in Ghana
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design/Area
2.2. Study Population and Data Collection
2.3. Ethical Considerations
2.4. Definition of Terms
2.5. Data Analysis
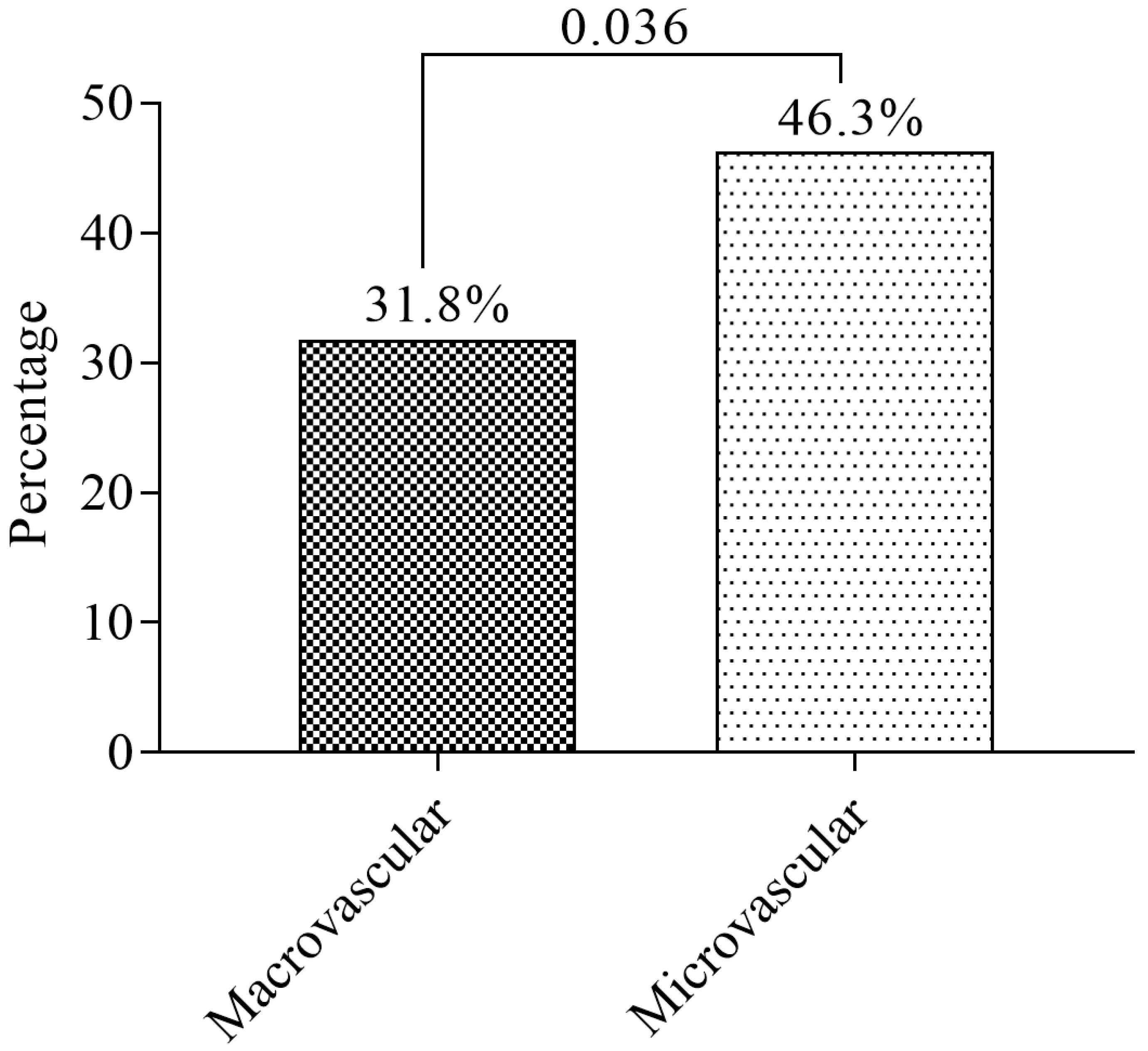
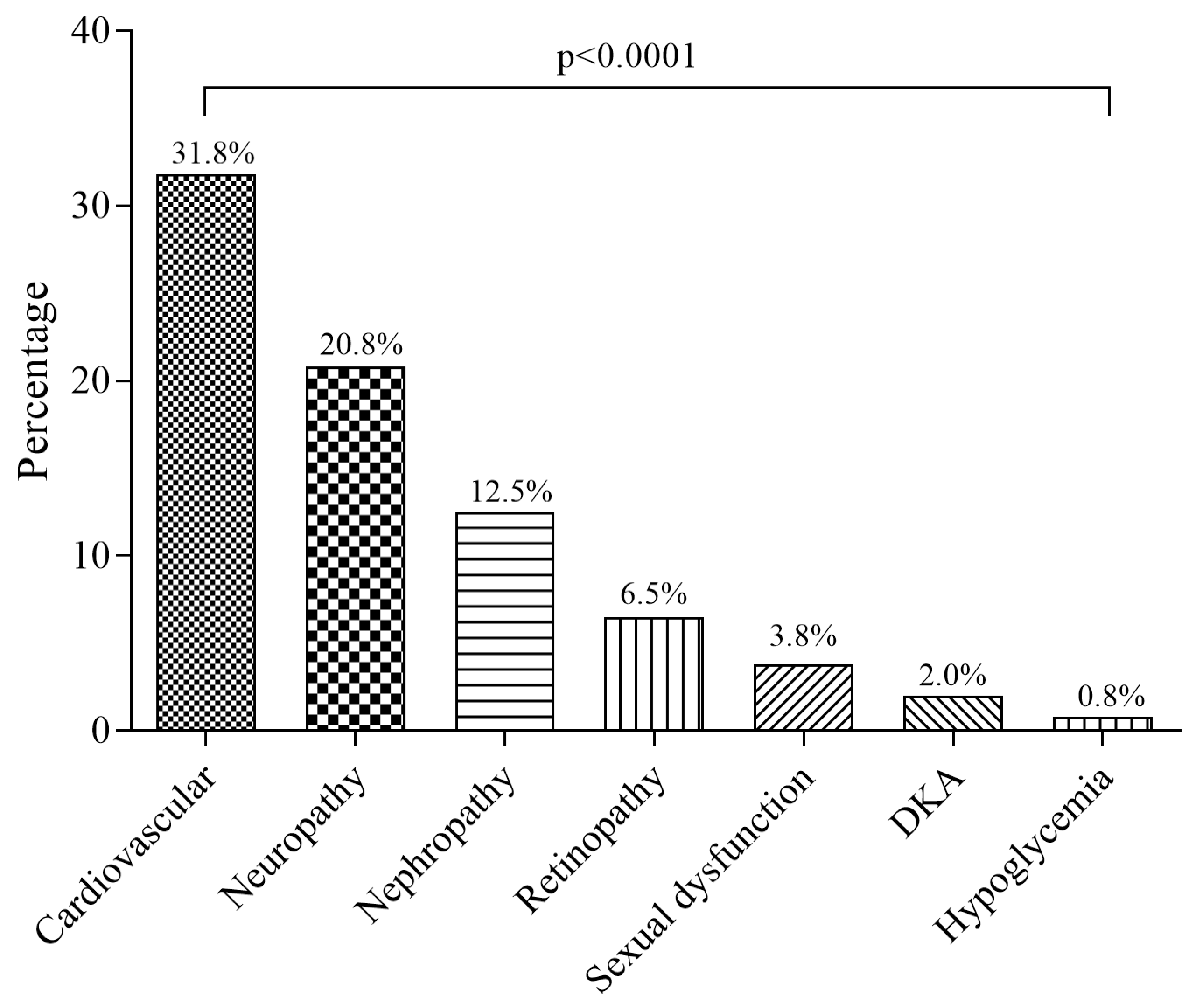
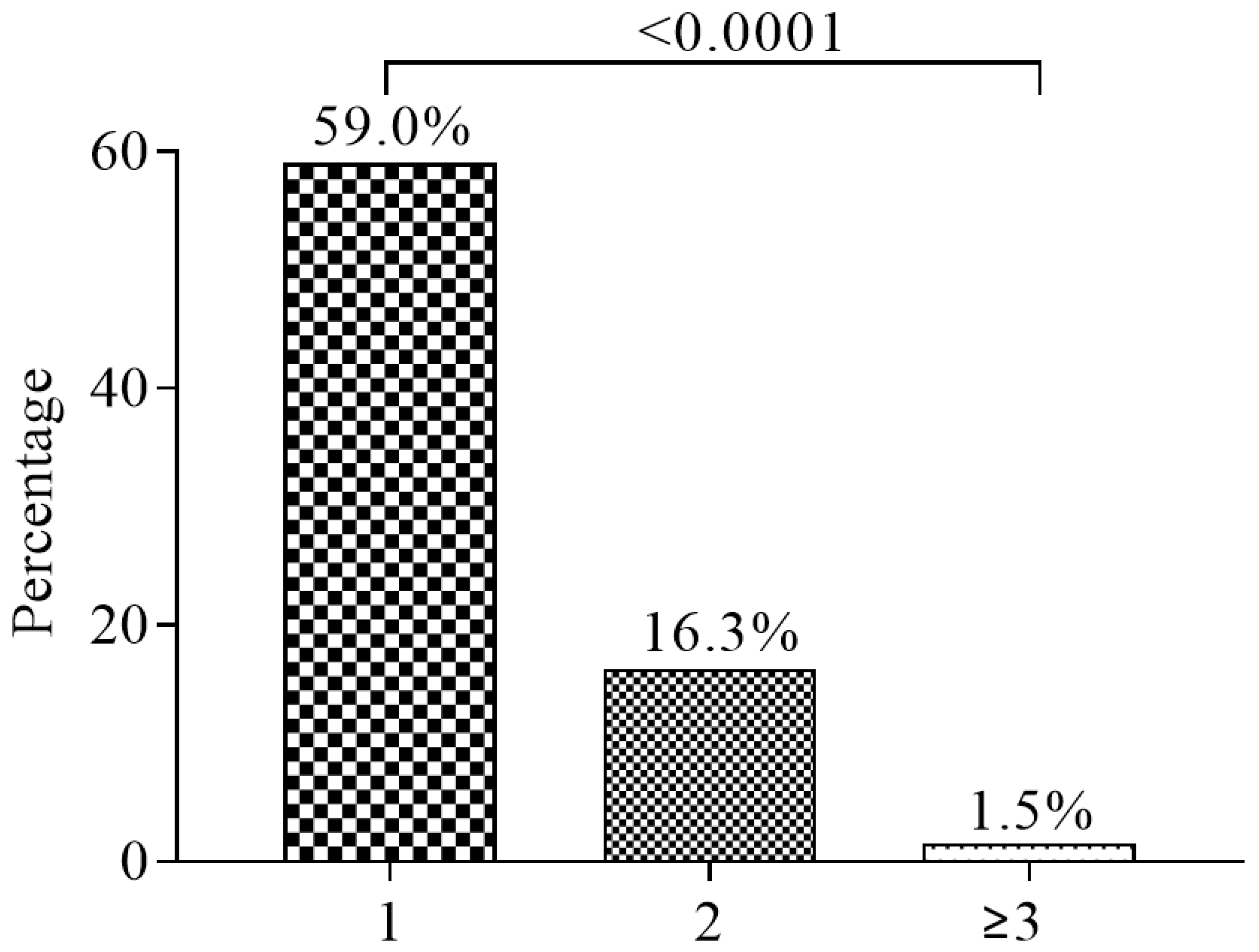
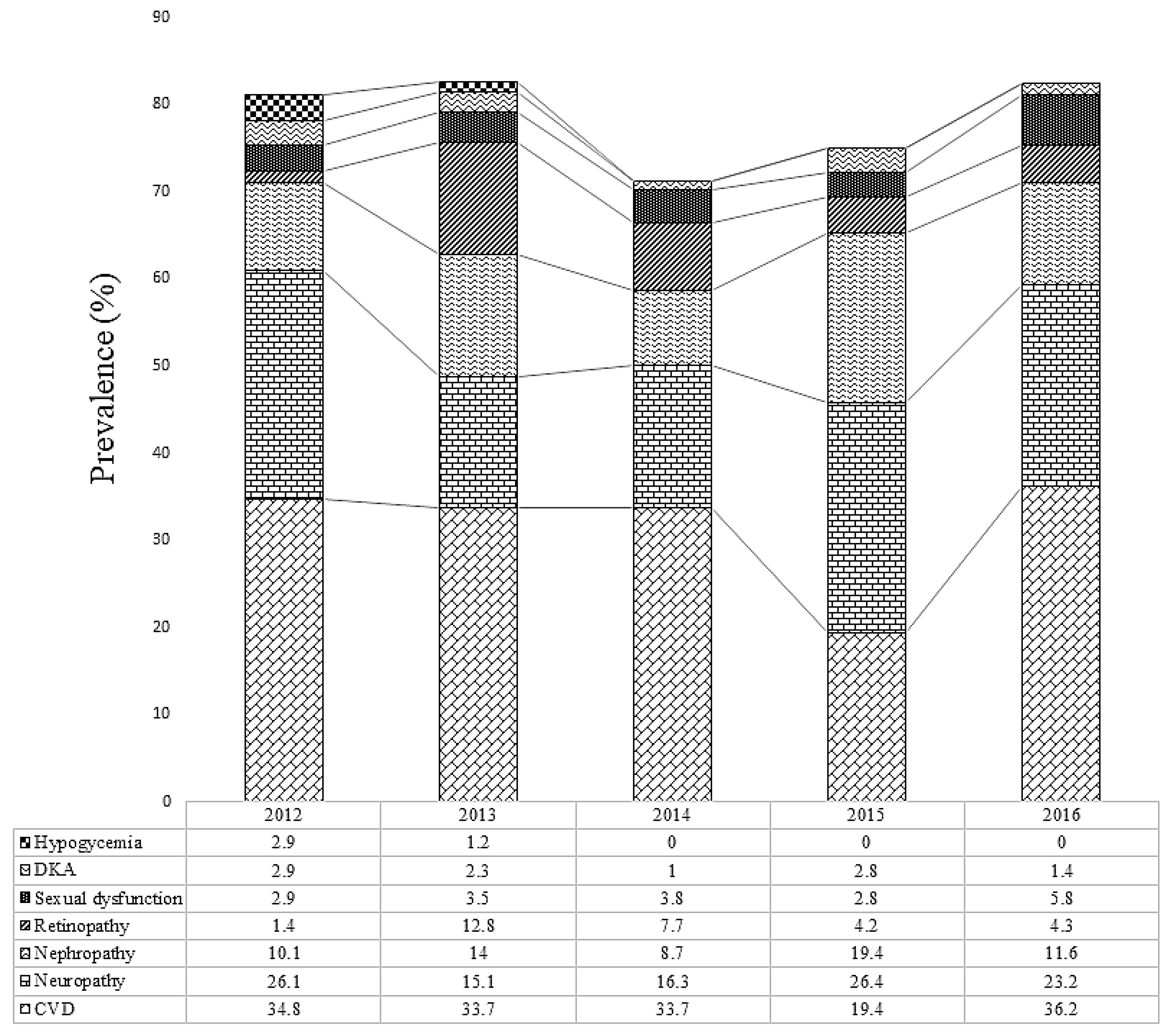
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Diabetes Cases Could Double in Developing Countries in Next 30 Years. 2003. Available online: https://www.who.int/mediacentre/news/releases/2003/pr86/en/ (accessed on 1 December 2018).
- Kengne, A.; Amoah, A.; Mbanya, J. Cardiovascular complications of diabetes mellitus in sub-Saharan Africa. Circulation 2005, 112, 3592–3601. [Google Scholar] [CrossRef] [PubMed]
- Peer, N.; Kengne, A.-P.; Motala, A.A.; Mbanya, J.C. Diabetes in the Africa Region: an update. Diabetes Res. Clin. Pract. 2014, 103, 197–205. [Google Scholar] [CrossRef]
- Whiting, D.R.; Guariguata, L.; Weil, C.; Shaw, J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res. Clin. Pract. 2011, 94, 311–321. [Google Scholar] [CrossRef] [PubMed]
- de-Graft Aikins, A.; Awuah, R.B.; Pera, T.A.; Mendez, M.; Ogedegbe, G. Explanatory models of diabetes in urban poor communities in Accra, Ghana. Ethn. Health. 2015, 20, 391–408. [Google Scholar] [CrossRef] [PubMed]
- Kitabchi, A.E.; Umpierrez, G.E.; Murphy, M.B.; Barrett, E.J.; Kreisberg, R.A.; Malone, J.I.; Wall, B.M. Management of hyperglycemic crises in patients with diabetes. Diabetes Care. 2001, 24, 131–153. [Google Scholar] [CrossRef] [PubMed]
- Fowler, M. Microvascular and macrovascular complications of diabetes. Clin. Diabetes. 2011, 29, 116–122. [Google Scholar] [CrossRef]
- Maiorino, M.; Bellastella, G.; Esposito, K. Diabetes and sexual dysfunction: current perspectives. Diabetes Metab. Syndr. Obes. 2014, 7, 95–105. [Google Scholar] [PubMed] [Green Version]
- Gerstein, H.C. Reduction of cardiovascular events and microvascular complications in diabetes with ACE inhibitor treatment: HOPE and MICRO-HOPE. Diabetes Metab. Res. Rev. 2002, 18, 82–85. [Google Scholar] [CrossRef]
- Fowler, M. Microvascular and macrovascular complications of diabetes. Clin. Diabetes. 2008, 26, 77–82. [Google Scholar] [CrossRef]
- Smith-Spangler, C.M.; Bhattacharya, J.; Goldhaber-Fiebert, J.D. Diabetes, its treatment, and catastrophic medical spending in 35 developing countries. Diabetes Care. 2012, 35, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Mutyambizi, C.; Pavlova, M.; Chola, L.; Hongoro, C.; Groot, W. Cost of diabetes mellitus in Africa: A systematic review of existing literature. Global. Health. 2018, 14. [Google Scholar] [CrossRef]
- Quaye, E.; Amporful, E.; Akweongo, P.; Aikins, M. Analysis of the financial cost of diabetes mellitus in four cocoa clinics of Ghana. Value Health Reg. Issues. 2015, 7, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Association, A.D. Economic costs of diabetes in the US in 2012. Diabetes Care. 2013, 36, 1033–1046. [Google Scholar] [CrossRef]
- Adams, R. Improving health outcomes with better patient understanding and education. Risk Manag. Healthc. Policy. 2010, 3, 61–72. [Google Scholar] [CrossRef] [Green Version]
- Howell, D.; Harth, T.; Brown, J.; Bennett, C.; Boyko, S. Self-management education interventions for patients with cancer: a systematic review. Support. Care Cancer. 2017, 25, 1323–1355. [Google Scholar] [CrossRef]
- Obirikorang, Y.; Obirikorang, C.; Anto, E.; Acheampong, E.; Batu, E.; Stella, A.; Constance, O.; Brenya, P. Knowledge of complications of diabetes mellitus among patients visiting the diabetes clinic at Sampa Government Hospital, Ghana: A descriptive study. BMC Public Health. 2016, 16. [Google Scholar] [CrossRef]
- Ovenseri-Ogbomo, G.; Abokyi, S.; Koffuor, G.; Abokyi, E. Knowledge of diabetes and its associated ocular manifestations by diabetic patients: A study at Korle-Bu Teaching Hospital, Ghana. Niger. Med. J. 2013, 54, 217–223. [Google Scholar] [CrossRef]
- Ghana Demographic and Health Survey 2003. Available online: https://dhsprogram.com/pubs/pdf/FR152/FR152.pdf (accessed on 1 December 2018).
- Owusu–Ansah, A.; Panyin, A.B.; Obirikorang, C.; Agyare, C.; Acheampong, E.; Kwofie, S.; Anto, E.O.; Batu, E.N. Metabolic Syndrome among Schizophrenic Patients: A Comparative Cross-Sectional Study in the Middle Belt of Ghana. Schizophr. Res. Treat. 2018, 2018. [Google Scholar] [CrossRef]
- Danquah, I.; Bedu-Addo, G.; Terpe, K.J.; Micah, F.; Amoako, Y.A.; Awuku, Y.A.; Dietz, E.; van der Giet, M.; Spranger, J.; Mockenhaupt, F.P. Diabetes mellitus type 2 in urban Ghana: characteristics and associated factors. BMC Public Health 2012, 12, 210. [Google Scholar] [CrossRef]
- Fondjo, L.; Sakyi, S.; Owiredu, W.; Laing, E.; Owiredu, E.; Awusi, E.; Ephraim, R.; Kantanka, O. Evaluating Vitamin D Status in Pre- and Postmenopausal Type 2 Diabetics and Its Association with Glucose Homeostasis. BioMed Res. Int. 2018, 2018. [Google Scholar] [CrossRef]
- Mbanya, J.; Sobngwi, E. Diabetes in Africa. Diabetes microvascular and macrovascular disease in Africa. J. Cardiovasc. Risk. 2003, 10, 97–102. [Google Scholar] [CrossRef]
- Arfken, C.; Reno, P.; Santiago, J.; Klein, R. Development of proliferative diabetic retinopathy in African-Americans and whites with type 1 diabetes. Diabetes Care. 1998, 21, 792–795. [Google Scholar] [CrossRef]
- Morgan, C.; Currie, C.; Stott, N.; Smithers, M.; Butler, C.C.; Peters, J. The prevalence of multiple diabetes-related complications. Diabet. Med. 2000, 17, 146–151. [Google Scholar] [CrossRef]
- Shi, W.; Li, X.; Li, J. The morbidity of chronic diabetic complication with logistic regression analysis of related potential risk factors. Zhonghua Liu Xing Bing Xue Za Zhi. 2004, 25, 60–64. [Google Scholar]
- Yang, W.; Lu, J.; Weng, J.; Jia, W.; Ji, L.; Xiao, J.; Shan, Z.; Liu, J.; Tian, H.; Ji, Q. Prevalence of diabetes among men and women in China. N. Engl. J. Med. 2010, 362, 1090–1101. [Google Scholar] [CrossRef]
- Zhang, G.; Chen, H.; Chen, W.; Zhang, M. Prevalence and risk factors for diabetic retinopathy in China: A multi-hospital-based cross-sectional study. Br. J. Ophthalmol. 2017, 1591–1595. [Google Scholar] [CrossRef] [PubMed]
- Pang, C.; Jia, L.; Jiang, S.; Liu, W.; Hou, X.; Zuo, Y.; Gu, H.; Bao, Y.; Wu, Q.; Xiang, K.; et al. Determination of diabetic retinopathy prevalence and associated risk factors in Chinese diabetic and pre-diabetic subjects: Shanghai diabetic complications study. Diabetes Metab. Res. Rev. 2012, 28, 276–283. [Google Scholar]
- Wang, F.; Liang, Y.; Peng, X.; Wang, J.; Zhang, F.; WB, W.; Sun, L.; Friedman, D.; Wang, N.; Wong, T.; et al. Risk factors for diabetic retinopathy in a rural Chinese population with type 2 diabetes: the Handan Eye Study. Acta Ophthalmol. 2011, 89, 336–343. [Google Scholar] [CrossRef]
- Xu, J.; Wei, W.; Yuan, M.; Yuan, S.; Wan, G.; Zheng, Y.; Li, Y.; Wang, S.; Xu, L.; Fu, H.; et al. Prevalence and risk factors for diabetic retinopathy: the Beijing Communities Diabetes Study 6. Retina 2012, 32, 322–329. [Google Scholar] [CrossRef]
- Harzallah, F.; Ncibi, N.; Alberti, H.; Brahim, A.; Smadhi, H.; Kanoun, F.; Slimane, H. Clinical and metabolic characteristics of newly diagnosed diabetes patients: experience of a university hospital in Tunis. Diabetes Metab. 2006, 32, 632–635. [Google Scholar] [CrossRef]
- Macky, T.; Khater, N.; Al-Zamil, M.; El Fishawy, H.; Soliman, M. Epidemiology of diabetic retinopathy in Egypt: a hospital-based study. Ophthalmic Res. 2011, 45, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Hamed, S.; Amine, N.; Galal, G.; Helal, S.; El-Din, L.; Shawky, O.; Ahmed, E.; Rahman, M. Vascular risks and complications in diabetes mellitus: the role of Helicobacter pylori infection. J. Stroke Cerebrovasc. Dis. 2008, 17, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Elbagir, M.; Eltom, M.; Mahadi, E.; Berne, C. Pattern of long-term complications in Sudanese insulin-treated diabetic patients. Diabetes Res. Clin. Pract. 1995, 30, 59–67. [Google Scholar] [CrossRef]
- Yang, H.; Wei, Y.; Gao, X.; Xu, X.; Fan, L.; He, J.; Hu, Y.; Liu, X.; Chen, X.; Yang, Z. Risk factors for gestational diabetes mellitus in Chinese women—a prospective study of 16 286 pregnant women in China. Diabet. Med. 2009, 26, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, R. Correlation of duration, hypertension and glycemic control with microvascular complications of diabetes mellitus at a tertiary care hospital. Integr. Mol. Med. 2017, 4. [Google Scholar] [CrossRef] [Green Version]
- Zoungas, S.; Woodward, M.; Li, Q.; Cooper, M.; Hamet, P.; Harrap, S.; Heller, S.; Marre, M.; Patel, A.; Poulter, N.; et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia 2014, 57, 2465–2474. [Google Scholar] [CrossRef] [Green Version]
| Variables | Total (n = 1600) | Complications (944/59.0%) | No Complications (656/41.0%) | p value |
|---|---|---|---|---|
| Gender | 0.876 | |||
| Male | 640 (40.0) | 376 (39.8) | 264 (40.2) | |
| Female | 960 (60.0) | 568 (60.2) | 392 (59.2) | |
| Age (years) | 55.9 ± 14.3 | 58.5 ± 13.6 | 52.3 ± 14.4 | <0.0001 |
| <30 | 60 (3.8) | 32 (3.4) | 28 (4.3) | 0.001 |
| 30–50 | 484 (30.3) | 216 (22.9) | 268 (40.8) | |
| 51–70 | 800 (50.0) | 520 (55.1) | 280 (42.7) | |
| ≥71 | 256 (16.0) | 176 (18.6) | 80 (12.2) | |
| Gender-wise age ratio (m:f; p value) | 56.2:56.2; p = 0.968 | 56.7:55.4; p = 0.188 | 57.4:55.6; p = 0.105 | |
| Marital status | 0.012 | |||
| Single | 156 (9.8) | 80 (8.5) | 76 (11.6) | |
| Married | 1108 (69.3) | 644 (68.2) | 464 (70.7) | |
| Widowed | 232 (14.5) | 156 (16.5) | 76 (11.6) | |
| Divorced | 104 (6.5) | 64 (6.8) | 40 (6.1) | |
| Educational status | 0.329 | |||
| Illiterate | 356 (22.3) | 216 (22.9) | 140 (21.3) | |
| Basic | 640 (40) | 360 (38.1) | 280 (42.7) | |
| Secondary | 312 (19.5) | 192 (20.3) | 120 (18.3) | |
| Tertiary | 292 (18.3) | 176 (18.6) | 116 (17.7) | |
| Occupational status | <0.0001 | |||
| Informal | 1228 (76.8) | 700 (74.2) | 528 (80.5) | |
| Formal | 176 (11.0) | 100 (10.6) | 76 (11.6) | |
| Retired | 196 (12.3) | 144 (15.3) | 52 (7.9) | |
| Duration of diabetes (years) | <0.0001 | |||
| <5 | 1016 (63.5) | 540 (57.2) | 476 (72.2) | |
| 5–10 | 320 (20.0) | 204 (21.2) | 116 (17.7) | |
| >10 | 264 (16.5) | 200 (21.2) | 64 (9.7) |
| Complications | CVD | Neuropathy | Nephropathy | Retinopathy | Sexual Dysfunction | DKA | Hypoglycemia |
|---|---|---|---|---|---|---|---|
| Sex | |||||||
| Male | 176 (34.6) | 144 (43.4) | 80 (40.0) | 32 (30.8) | 48 (80.0) ‡ | 16 (50.0) | 0 (0.0) |
| Female | 332 (65.4) † | 188 (56.6) | 120 (60.0) | 72 (69.2) | 12 (20.0) | 16 (50.0) | 12 (100.0) ‡ |
| Age (years) | |||||||
| <30 | 16 (3.1) | 28 (8.4) | 8 (4.0) | 0 (0.0) | 4 (6.7) | 8 (25.0) | 0 (0.0) |
| 30–50 | 176 (34.6) | 96 (28.9) | 68 (34.0) | 16 (15.4) | 12 (20.0) | 4 (12.5) | 0 (0.0) |
| 51–70 | 224 (44.1) † | 156 (47.0) ‡ | 92 (46.0) | 68 (65.4) ‡ | 40 (66.7) † | 16 (50.0) ‡ | 8 (66.7) |
| >71 | 92 (18.1) | 52 (15.7) | 32 (16.0) | 20 (19.2) | 4 (6.7) | 4 (12.5) | 4 (33.3) |
| Marital status | |||||||
| Single | 52 (10.2) | 40 (12.0) | 12 (6.0) | 12 (11.5) | 4 (6.7) | 4 (12.5) | 0 (0.0) |
| Married | 340 (66.9) | 236 (71.1) † | 136 (68.0) | 72 (69.2) † | 36 (60.0) † | 24 (75.0) | 12 (100.0) |
| Divorced | 40 (7.9) | 16 (4.8) | 16 (8.0) | 12 (11.5) | 16 (26.7) | 0 (0.0) | 0 (0.0) |
| Widow | 76 (15.0) | 40 (12.0) | 36 (18.0) | 8 (7.7) | 4 (6.7) | 4 (12.5) | 0 (0.0) |
| Education | |||||||
| None | 104 (20.5) | 76 (22.9) | 44 (22.0) | 40 (38.5) ‡ | 8 (13.3) | 4 (12.5) | 0 (0.0) |
| Basic | 212 (41.7) | 124 (37.3) † | 100 (50.0) ‡ | 40 (38.5) ‡ | 28 (46.7) ‡ | 16 (50.0) | 8 (66.7) † |
| Secondary | 100 (19.7) | 56 (16.9) | 28 (14.0) | 12 (11.5) | 20 (33.3) | 4 (12.5) | 4 (33.3) |
| Tertiary | 92 (18.1) | 76 (22.9) | 28 (14.0) | 12 (11.5) | 4 (6.7) | 8 (25.0) | 0 (0.0) |
| Occupation | |||||||
| Retired | 68 (13.4) | 36 (10.8) | 20 (10.0) | 4 (3.8) | 8 (13.3) | 4 (12.5) | 0 (0.0) |
| Formal | 60 (11.8) | 44 (13.3) | 20 (10.0) | 12 (11.5) | 8 (13.3) | 4 (12.5) | 0 (0.0) |
| Informal | 380 (74.8) | 252 (75.9) | 160 (80.0) | 88 (84.6) † | 44 (73.3) | 24 (75.0) | 12 (100.0) |
| Variable | aOR (95% CI) | p value |
|---|---|---|
| Age (years) | ||
| <30 | 1 | |
| 30–50 | 0.705 (0.412–1.208) | 0.203 |
| 51–70 | 1.625 (0.959–2.754) | 0.071 |
| >71 | 1.925 (1.087–3.411) | 0.025 |
| Gender | ||
| Male | 1 | |
| Female | 1.017 (0.830–1.247) | 0.868 |
| Educational level | ||
| No education | 1 | |
| Basic | 0.833 (0.640–1.085) | 0.176 |
| Secondary | 1.04 (0.759–1.417) | 0.819 |
| Tertiary | 0.983 (0.717–1.349) | 0.917 |
| Occupational status | ||
| Retired | 1 | |
| Informal | 0.479 (0.342–0.670) | <0.0001 |
| Formal | 0.475 (0.307–0.734) | 0.0008 |
| Duration of DM (years) | ||
| <5 | 1 | |
| 5–10 | 1.550 (1.196–2.009) | 0.0009 |
| >10 | 2.755 (2.026–3.746) | <0.0001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Annani-Akollor, M.E.; Addai-Mensah, O.; Fondjo, L.A.; Sallah, L.; Owiredu, E.-W.; Acheampong, E.; Akamugri, S. Predominant Complications of Type 2 Diabetes in Kumasi: A 4-Year Retrospective Cross-Sectional Study at a Teaching Hospital in Ghana. Medicina 2019, 55, 125. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina55050125
Annani-Akollor ME, Addai-Mensah O, Fondjo LA, Sallah L, Owiredu E-W, Acheampong E, Akamugri S. Predominant Complications of Type 2 Diabetes in Kumasi: A 4-Year Retrospective Cross-Sectional Study at a Teaching Hospital in Ghana. Medicina. 2019; 55(5):125. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina55050125
Chicago/Turabian StyleAnnani-Akollor, Max Efui, Otchere Addai-Mensah, Linda Ahenkorah Fondjo, Lorraine Sallah, Eddie-Williams Owiredu, Emmanuel Acheampong, and Solomon Akamugri. 2019. "Predominant Complications of Type 2 Diabetes in Kumasi: A 4-Year Retrospective Cross-Sectional Study at a Teaching Hospital in Ghana" Medicina 55, no. 5: 125. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina55050125





