1. Introduction
Percutaneous coronary interventions (PCI) for chronic total occlusions (CTO) remains one of the most difficult subsets for the interventional cardiologist because of the perceived procedural complexity. The widespread introduction of the latest CTO revascularization techniques, especially the retrograde approach [
1,
2], has made it possible to increase the number of successful procedures above 90%. The key to success in CTO PCI is diligent planning, which includes patient selection [
3,
4]. In selecting patients for CTO PCI it is important to consider patient-specific clinical and anatomical risk factors for the procedure [
4]. Choosing the appropriate patients for CTO will maximize the benefits for the patient and minimize the risk of complications. To enhance procedural success, the pre-procedural case evaluation is important. Various scoring systems have been developed to evaluate CTO PCI procedural potential success. The most commonly used ones in the world are J CTO score (Multicenter CTO Registry in Japan) [
4], the Prospective Global Registry for the Study of Chronic Total Occlusion Intervention score (PROGRESS CTO) [
5], the clinical and lesion related score (CL) [
6], and the coronary artery bypass grafting (CABG) history, age (≥70 y), stump anatomy (blunt or invisible), tortuosity degree (severe or unseen), length of occlusion (≥20 mm) and extent of calcification (severe) score (CASTLE) [
7].
The concept of long-term outcome in interventional cardiology is not well defined. In most publications, the observation period ranges from one to five years, but there are studies, where it is up to 10 years [
8].
Randomized studies do not prove a reduction in mortality after CTO recanalization [
9,
10]. Multiple observational studies have demonstrated the association of successful CTO revascularization with improved clinical outcomes compared to non-successful CTO revascularization: A meta-analysis of 25 studies compared successful (71%) with failed (29%) CTO PCIs in 28,486 patients. During a mean follow-up of 3.11 years, compared with failed procedures, successful CTO PCI was associated with lower mortality (odds ratio, 0.52), less residual angina (odds ratio, 0.38), lower risk of stroke (odds ratio, 0.72), and less need for subsequent CABG (odds ratio, 0.18) [
8].
However, comparison of long-term results of successful and unsuccessful procedures has been reasonably criticized, because it is not a randomized comparison and it is likely that patients in whom CTO PCI fails have more complex angiographic characteristics and more comorbidities that can adversely affect subsequent outcomes [
11]. Several clinical studies have also shown the relationship between the complexity of the procedure and procedural success [
4,
5,
6,
7]. The relationship between pre-procedural assessment results and the long-term outcome has been relatively poorly studied.
This study is a retrospective cohort single-center study, where we analyzed different scoring systems not only in predicting the procedural success but also in predicting long-term outcome (survival) after a successful CTO PCI procedure.
2. Materials and Methods
A total of 551 patients who underwent elective CTO PCI in Riga East University hospital from January 2007 to December 2016 were included in the study. These patients were stratified into two groups according to the CTO PCI procedure result: Successful cases group (n = 454) and unsuccessful cases group (n = 97). All CTO PCI procedures were performed by one operator. Patients’ medical history and symptoms were collected by physicians. All patients signed an informed consent on the interventional operation. The study was approved by the Riga Stradins University Ethics committee on 14 January 2010.
The J CTO score, PROGRESS CTO score, CL score, and CASTLE score were calculated retrospectively on the basis of coronary angiography and medical documentation. The primary endpoint was procedural success and all-cause death. CTO was defined as coronary complete occlusion (thrombolysis in myocardial infarction (MI) flow grade 0) with a duration of at least three months. The occlusion duration was estimated according to a previous history of myocardial infarction, the first onset of angina symptoms, or comparison with a previous angiogram [
11,
12].
If a single CTO lesion were attempted in two or more separate procedures during the enrolling period, only the last procedure was considered as a first and only attempt and subsequently included in the analysis. If two or more CTO PCIs were attempted for two or more separate CTO lesions during the enrolling period with a different result (one procedure successful, other not), the patient was excluded.
Procedural success was defined as the complete restoration of the antegrade blood flow (thrombolysis in MI flow grade 3) with an arterial lumen diameter reduction to less than 10% in the culprit CTO vessel.
Statistical Analysis
IBM SPSS Statistics 22 software was used to perform statistical analysis. Categorical variables were summarized as proportions or percentages. Chi-square test or chi-square test for trend was used to assess the differences. Continuous variables, such as age, CL score, and follow-up time, were presented as mean values with standard deviations (SD) or median values with interquartile range (IQR). Student’s t-test was used to compare age and Mann–Whitney U test to compare score distributions between patients with successful and unsuccessful procedures.
Receiver operating characteristics (ROC) curves showing the area under the curve (AUC) were used to characterize the prognostic value of J CTO, PROGRESS, CASTLE, and CL scores in respect to procedure success.
Survival analysis was performed using Kaplan–Meier curves and Cox regression. Follow-up started at the date of PCI procedure and ended at the date of death or 15 April 2019, whichever came first. The endpoint was all-cause death. Log-rank test was used to compare Kaplan–Meier survival curves. Pairwise comparisons were made where necessary. Standard errors of survival proportions were used to estimate 95% confidence intervals (CI) and to calculate z-score to assess the difference in five-year survival by disease severity group. Mortality risk of patients with higher disease severity scores compared to the less severe group was estimated as hazard ratios (HR) measures using Cox regression model. They were adjusted for sex, age, and other baseline characteristics, such as smoking history, hypertension, dyslipidaemia, diabetes, history of MI, prior CABG, and prior PCI. The set of co-factors was specified for each model not to duplicate parameters that are already included in the specific disease severity score. p value below 0.05 was set as a value for statistical significance.
3. Results
Among 551 CTO PCI patients enrolled, 454 cases were successful. Mean age was 63.5 years and 80% were male. Forty-five percent had a history of coronary artery bypass grafting (CABG) and 52.5 had a prior PCI. Twenty percent of patients had diabetes, 72.6% had prior myocardial infarction (
Table 1). We did not find significant differences between baseline characteristics in successful and unsuccessful cases group, except disease severity (
Table 1) which was higher in the case of unsuccessful procedures, as would be expected. The distribution of patients according to the severity of the disease was uneven, with the majority of patients being in the low and intermediate difficulty group (
Table 2).
With increasing disease complexity, the procedural success rate was significantly reduced in all scoring systems. (
Table 3). All four score systems showed a moderate predictive capacity (AUC for J CTO score 0.714,
p < 0.001; AUC for PROGRESS CTO score 0.605,
p < 0.001; AUC for CL score 0.624,
p < 0.001; AUC for CASTLE score 0.641,
p < 0.001) (
Table 4). However, the J CTO score demonstrates an advantage over other scores (
Figure 1).
Median follow-up time was 6.8 years (IQR 4.1–9.3 years), the minimum and maximum follow-up was 1.2 years and 12.3 years, respectively. Statistical better survival was found in the successful procedure group (
p = 0.041) (
Figure 2).
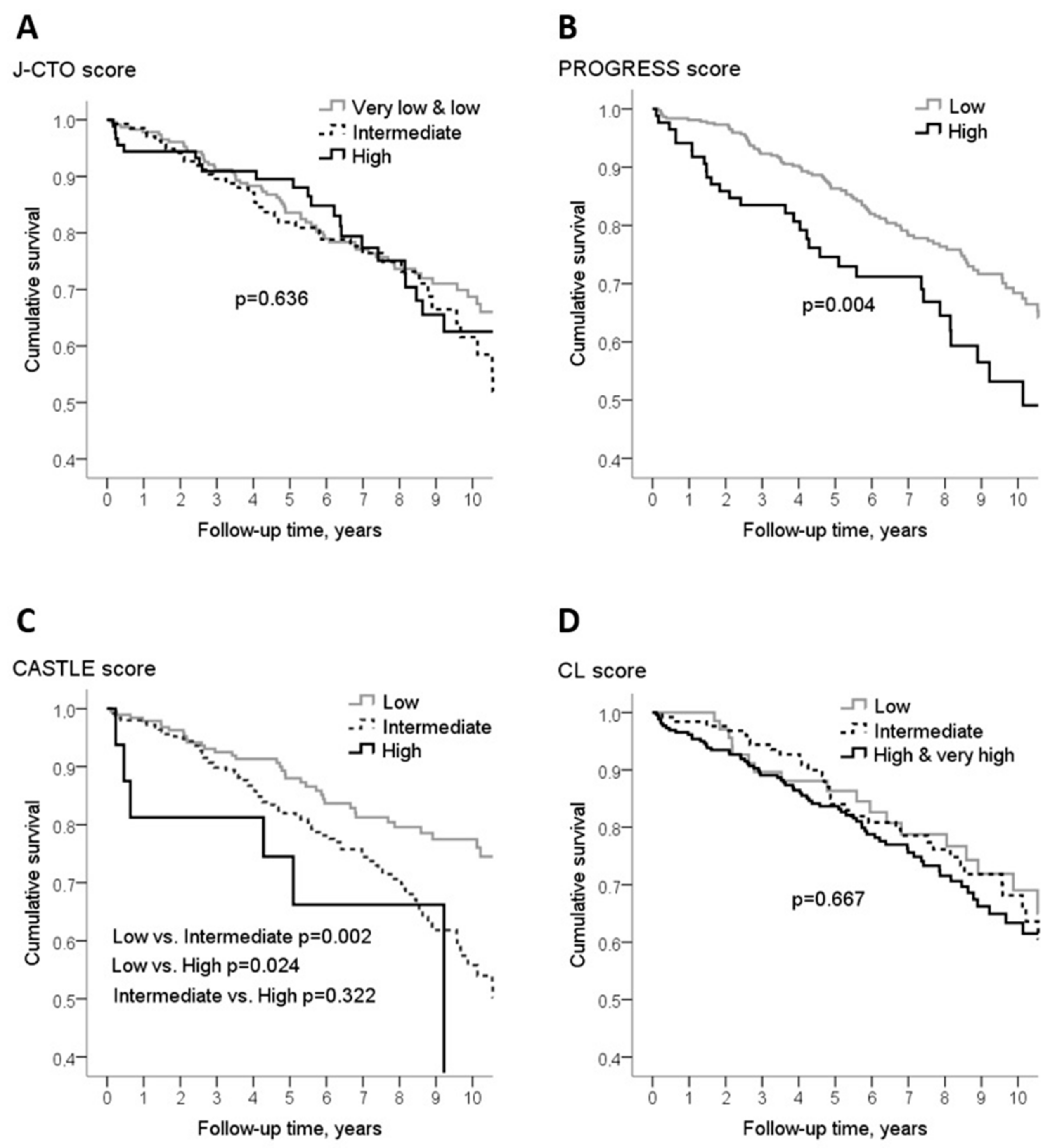
Disease severity assessed by PROGRESS score and CASTLE score showed an association with the risk of all-cause death (
Figure 3) over the entire follow-up, however, five-year survival rate differed only in the case of PROGRESS score (
Table 5). During the entire follow-up, patients having high PROGRESS score had almost two times higher risk of dying compared to the patients with low score (HR 1.81(95% CI 1.20–2.72)), and those with high and intermediate CASTLE score experienced almost three (HR 2.80(95% CI 1.18–6.66)) and two (HR 1.88(95%CI 1.26–2.78)) times higher risk of dying from any cause than the low score patients, respectively (
Table 6). Adjustment for sex, age, and other baseline characteristics did not affect the estimates substantially (
Table 6). The association between PROGRESS score and survival, after adjustment for age, sex, smoking history, hypertension, dyslipidemia, diabetes, prior MI, and prior PCI, was the same: HR 1.81(95%Cl 1.19–2.75). Whereas the association between CASTLE score and risk of all-cause death, adjusted for sex, smoking history, hypertension, dyslipidemia, diabetes, prior MI, prior PCI, and prior CABG, became even stronger: The risk of dying in patients with high CASTLE score was almost four times higher (HR3.68(95%Cl 1.50–9.05)) and in patients with intermediate score it was twice higher (HR 2.15(95%Cl 1.42–3.23)) compared to the patients with low CASTLE score.
4. Discussion
The present retrospective study analyses a cohort of 551 consecutive patients, who underwent the CTO-PCI procedure in one center over 10 years. Four hundred fifty-four procedures were successful. Our single-center study confirmed that patients after successful CTO PCI have a better long-term outcome in comparison with unsuccessful CTO PCI group. Several non-randomized comparative studies showed a beneficial effect of CTO recanalization on symptoms, quality of life, and left ventricular function [
13,
14], while its impact on survival remains unclear [
12,
13,
14,
15]. The effectiveness of CTO PCI to relieve symptoms has now been confirmed in Euro CTO trial. This trial showed a superior effect of PCI on angina frequency and quality of life, as compared with OMT, 12 months after randomization [
16]. However, there is no evidence that successful CTO PCI can improve the long-term outcome. There was no difference in the incidence of major adverse cardiovascular events with CTO-PCI versus no CTO-PCI, but the study was limited by low power for clinical endpoints and high crossover rates between groups.
In the DECISION-CTO trial, the three-year rate of the composite endpoint of all-cause death, MI, stroke, and any revascularization in the intention-to-treat analysis was similar between the PCI and OMT groups (20.6% vs. 19.6%) [
9].
CTO scoring systems were created to predict the result of the procedure [
14]. Procedures with a higher CTO score are technically more complex and with less success rate.
As the first scoring system J CTO score was created in 2006. The system was designed to predict the possibility of CTO antegrade crossing with wire within 30 min [
5]. Since 2006, coronary intervention techniques have changed and the J CTO scoring system has been criticized for containing subjective and biased factors. Several attempts have been made to create a better scoring system. Nevertheless, the prognostic value of the J CTO score remains high, which is also confirmed by our study. J CTO score contains mainly factors, that cannot in themselves worsen the patient prognosis (CTO stump, occluded segment length, occluded artery tortuosity, previous PCI attempt). This could be the reason, why it has less impact on long-term outcome than other scores.
This study was designed to ascertain whether the scoring results can predict the long-term outcome after successful CTO PCI procedure.
We did not find long-term survival differences among different complexity procedures, analyzing cases with J CTO and CL score systems. At the same time, analyzing cases with PROGERESS CTO score and CASTLE score, more complex patients had a statistically worse long-term prognosis. Some risk factors are included in several scoring systems but some are unique. PROGRESS CTO score differs from others as it is based on four angiographic only variables, among which there are collateral estimation and CTO localization in the left circumflex artery, they are not included in other scores. These two factors obviously make the procedure more difficult and the long-term results worsen. In terms of the maximal number of points, PROGRESS score has the smallest possible sum of points (only four) and patient apportionment is not as wide as in other scores. CASTLE score differs as it contains as risk factors patient age and myocardial infarction in the past. Aging is an independent predictor of adverse cardiovascular events [
17,
18].
The majority of patients (60%) with a CTO did not undergo previous MI [
19].
Patients with a CTO and an implantable cardioverter defibrillator for primary or secondary prevention of sudden cardiac death have a higher incidence of appropriate delivered therapies and shocks as compared to patients with ischemic cardiomyopathy without a CTO [
10]. A CTO in an infarct-related artery has been discovered as an independent predictor for the occurrence of ventricular arrhythmias, resulting in a two/three-fold higher recurrence rate, even after treatment with ablation [
20,
21]. It is possible that the necrotic zone and scar will act as an inducer of ventricular arrhythmias [
20,
21]. Perhaps, that is why patients with a higher CASTLE score have a worse long-term outcome.
Our study has some limitations. First, although all study patients received standard drug therapy, including Aspirin and P2Y12 receptor inhibitors, before PCI, pharmacotherapy during the follow-up period was not analyzed in this study. Second, the study includes CTO patients, treated with PCI from 2007 to 2016. Procedural techniques, experience, and success rates during the last decade have changed. Third, a lot of significant data (medications, comorbidities, procedural data) were not included in the analysis.