Obese Animals as Models for Numerous Diseases: Advantages and Applications
Abstract
:Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Spieker, E.A.; Pyzocha, N. Economic impact of obesity. Prim. Care 2016, 43, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Ghanemi, A.; Yoshioka, M.; St-Amand, J. Will an obesity pandemic replace the coronavirus disease-2019 (COVID-19) pandemic? Med. Hypotheses 2020, 144, 110042. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Gutin, I. In BMI we trust: Reframing the body mass index as a measure of health. Soc. Theory Health 2018, 16, 256–271. [Google Scholar] [CrossRef]
- Ghanemi, A.; Yoshioka, M.; St-Amand, J. Broken energy homeostasis and obesity pathogenesis: The surrounding concepts. J. Clin. Med. 2018, 7, 453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghanemi, A.; Yoshioka, M.; St-Amand, J. Obesity as a neuroendocrine reprogramming. Medicina 2021, 57, 66. [Google Scholar] [CrossRef]
- Donini, L.M.; Rosano, A.; di Lazzaro, L.; Lubrano, C.; Carbonelli, M.; Pinto, A.; Giusti, A.M.; Lenzi, A.; Siervo, M. Impact of disability, psychological status, and comorbidity on health-related quality of life perceived by subjects with obesity. Obes. Facts 2020, 13, 191–200. [Google Scholar] [CrossRef]
- Jokinen, E. Obesity and cardiovascular disease. Minerva Pediatr. 2015, 67, 25–32. [Google Scholar]
- Saliba, L.J.; Maffett, S. Hypertensive heart disease and obesity: A review. Heart Fail. Clin. 2019, 15, 509–517. [Google Scholar] [CrossRef]
- Karczewski, J.; Śledzińska, E.; Baturo, A.; Jończyk, I.; Maleszko, A.; Samborski, P.; Begier-Krasińska, B.; Dobrowolska, A. Obesity and inflammation. Eur. Cytokine Netw. 2018, 29, 83–94. [Google Scholar] [CrossRef]
- Cox, A.J.; West, N.P.; Cripps, A.W. Obesity, inflammation, and the gut microbiota. Lancet Diabetes Endocrinol. 2015, 3, 207–215. [Google Scholar] [CrossRef]
- Dixon, A.E.; Peters, U. The effect of obesity on lung function. Expert Rev. Respir. Med. 2018, 12, 755–767. [Google Scholar] [CrossRef]
- Meurling, I.J.; Shea, D.O.; Garvey, J.F. Obesity and sleep: A growing concern. Curr. Opin. Pulm. Med. 2019, 25, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.N.; Liebeskind, D.S.; Towfighi, A. The Role of Diabetes, Obesity, and Metabolic Syndrome in Stroke. Semin. Neurol. 2017, 37, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Yawoot, N.; Govitrapong, P.; Tocharus, C.; Tocharus, J. Ischemic stroke, obesity, and the anti-inflammatory role of melatonin. BioFactors 2021, 47, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Chobot, A.; Górowska-Kowolik, K.; Sokołowska, M.; Jarosz-Chobot, P. Obesity and diabetes—Not only a simple link between two epidemics. Diabetes Metab. Res. Rev. 2018, 34, e3042. [Google Scholar] [CrossRef] [Green Version]
- Barnes, A.S. The epidemic of obesity and diabetes: Trends and treatments. Texas Heart Inst. J. 2011, 38, 142–144. [Google Scholar]
- Milaneschi, Y.; Simmons, W.K.; van Rossum, E.F.C.; Penninx, B.W. Depression and obesity: Evidence of shared biological mechanisms. Mol. Psychiatry 2019, 24, 18–33. [Google Scholar] [CrossRef] [PubMed]
- Romain, A.J.; Marleau, J.; Baillot, A. Impact of obesity and mood disorders on physical comorbidities, psychological well-being, health behaviours and use of health services. J. Affect. Disord. 2018, 225, 381–388. [Google Scholar] [CrossRef]
- Aigner, E.; Feldman, A.; Datz, C. Obesity as an emerging risk factor for iron deficiency. Nutrients 2014, 6, 3587–3600. [Google Scholar] [CrossRef]
- Cohen, A.; Dempster, D.W.; Recker, R.R.; Lappe, J.M.; Zhou, H.; Zwahlen, A.; Müller, R.; Zhao, B.; Guo, X.E.; Lang, T.; et al. Abdominal fat is associated with lower bone formation and inferior bone quality in healthy premenopausal women: A transiliac bone biopsy study. J. Clin. Endocrinol. Metab. 2013, 98, 2562–2572. [Google Scholar] [CrossRef]
- Lloret, A.; Monllor, P.; Esteve, D.; Cervera-Ferri, A.; Lloret, M.-A. Obesity as a risk factor for Alzheimer’s disease: Implication of leptin and glutamate. Front. Neurosci. 2019, 13, 508. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, M.; Tashiro, Y.; Shinohara, M.; Hirokawa, J.; Suzuki, K.; Onishi-Takeya, M.; Mukouzono, M.; Takeda, S.; Saito, T.; Fukumori, A.; et al. Increased levels of Aβ42 decrease the lifespan of ob/ob mice with dysregulation of microglia and astrocytes. FASEB J. 2020, 34, 2425–2435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazon, J.N.; de Mello, A.H.; Ferreira, G.K.; Rezin, G.T. The impact of obesity on neurodegenerative diseases. Life Sci. 2017, 182, 22–28. [Google Scholar] [CrossRef]
- Avgerinos, K.I.; Spyrou, N.; Mantzoros, C.S.; Dalamaga, M. Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism 2019, 92, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Pischon, T.; Nimptsch, K. Obesity and risk of cancer: An introductory overview. Methods Mol. Biol. 2016, 208, 1–15. [Google Scholar]
- Ghanemi, A.; Yoshioka, M.; St-Amand, J. Regeneration during obesity: An impaired homeostasis. Animals 2020, 10, 2344. [Google Scholar] [CrossRef]
- Andersen, T.; Gluud, C. Liver morphology in morbid obesity: A literature study. Int. J. Obes. 1984, 8, 97–106. [Google Scholar] [PubMed]
- Di Meo, S.; Iossa, S.; Venditti, P. Improvement of obesity-linked skeletal muscle insulin resistance by strength and endurance training. J. Endocrinol. 2017, 234, R159–R181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barazzoni, R.; Bischoff, S.; Boirie, Y.; Busetto, L.; Cederholm, T.; Dicker, D.; Toplak, H.; Van Gossum, A.; Yumuk, V.; Vettor, R. Sarcopenic Obesity: Time to Meet the Challenge. Obes. Facts 2018, 11, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Dashty, M. A quick look at biochemistry: Carbohydrate metabolism. Clin. Biochem. 2013, 46, 1339–1352. [Google Scholar] [CrossRef]
- Milić, S.; Lulić, D.; Štimac, D. Non-alcoholic fatty liver disease and obesity: Biochemical, metabolic and clinical presentations. World J. Gastroenterol. 2014, 20, 9330–9337. [Google Scholar]
- Engin, A. The Definition and Prevalence of Obesity and Metabolic Syndrome. Adv. Exp. Med. Biol. 2017, 960, 1–17. [Google Scholar]
- Unamuno, X.; Gómez-Ambrosi, J.; Rodríguez, A.; Becerril, S.; Frühbeck, G.; Catalán, V. Adipokine dysregulation and adipose tissue inflammation in human obesity. Eur. J. Clin. Investig. 2018, 48, e12997. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghanemi, A.; St-Amand, J. Redefining obesity toward classifying as a disease. Eur. J. Intern. Med. 2018, 55, 20–22. [Google Scholar] [CrossRef] [PubMed]
- Wilding, J.P.H.; Mooney, V.; Pile, R. Should obesity be recognised as a disease? BMJ 2019, 366, l4258. [Google Scholar] [CrossRef]
- Arrieta, F.; Pedro-Botet, J. Recognizing obesity as a disease: A true challenge. Rev. Clín. Esp. 2020. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Romano, L.; di Renzo, L.; di Lorenzo, N.; Cenname, G.; Gualtieri, P. Obesity: A preventable, treatable, but relapsing disease. Nutrition 2020, 71, 110615. [Google Scholar] [CrossRef]
- Christensen, S. Recognizing obesity as a disease. J. Am. Assoc. Nurse Pract. 2020, 32, 497–503. [Google Scholar] [CrossRef]
- Fuijkschot, W.W.; Morrison, M.C.; Zethof, I.P.; Krijnen, P.A.; Kleemann, R.; Niessen, H.W.; Smulders, Y.M. LPS-induced systemic inflammation does not alter atherosclerotic plaque area or inflammation in APOE3*LEIDEN mice in the early phase up to 15 days. Shock 2018, 50, 360–365. [Google Scholar] [CrossRef]
- Furman, B.L. Streptozotocin-induced diabetic models in mice and rats. Curr. Protoc. Pharmacol. 2015, 70, 5.47.1–5.47.20. [Google Scholar] [CrossRef] [PubMed]
- Lutz, T.A.; Woods, S.C. Overview of animal models of obesity. Curr. Protoc. Pharmacol. 2012, 58, 5.61.1–5.61.18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kleinert, M.; Clemmensen, C.; Hofmann, S.M.; Moore, M.C.; Renner, S.; Woods, S.C.; Huypens, P.; Beckers, J.; de Angelis, M.H.; Schürmann, A.; et al. Animal models of obesity and diabetes mellitus. Nat. Rev. Endocrinol. 2018, 14, 140–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soto, M.; Orliaguet, L.; Reyzer, M.L.; Manier, M.L.; Caprioli, R.M.; Kahn, C.R. Pyruvate induces torpor in obese mice. Proc. Natl. Acad. Sci. USA 2018, 115, 810–815. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.Y.; Liao, J.K. A mouse model of diet-induced obesity and insulin resistance. Methods Mol. Biol. 2012, 821, 421–433. [Google Scholar]
- Shin, J.-H.; Nam, M.H.; Lee, H.; Lee, J.-S.; Kim, H.; Chung, M.-J.; Seo, J.-G. Amelioration of obesity-related characteristics by a probiotic formulation in a high-fat diet-induced obese rat model. Eur. J. Nutr. 2017, 57, 2081–2090. [Google Scholar] [CrossRef]
- Val-Laillet, D. Review: Impact of food, gut–brain signals and metabolic status on brain activity in the pig model: 10 years of nutrition research using in vivo brain imaging. Animal 2019, 13, 2699–2713. [Google Scholar] [CrossRef] [Green Version]
- Jerez, S.; Scacchi, F.; Sierra, L.; Karbiner, S.; de Bruno, M.P. Vascular hyporeactivity to angiotensin II and noradrenaline in a rabbit model of obesity. J. Cardiovasc. Pharmacol. 2012, 59, 49–57. [Google Scholar] [CrossRef]
- Siino, V.; Amato, A.; di Salvo, F.; Caldara, G.F.; Filogamo, M.; James, P.; Vasto, S. Impact of diet-induced obesity on the mouse brain phosphoproteome. J. Nutr. Biochem. 2018, 58, 102–109. [Google Scholar] [CrossRef]
- Lopomo, A.; Burgio, E.; Migliore, L. Epigenetics of obesity. Prog. Mol. Biol. Transl. Sci. 2016, 140, 151–184. [Google Scholar]
- Catalano, P.M.; Shankar, K. Obesity and pregnancy: Mechanisms of short term and long term adverse consequences for mother and child. BMJ 2017, 356, j1. [Google Scholar] [CrossRef]
- Goossens, G.H. The metabolic phenotype in obesity: Fat mass, body fat distribution, and adipose tissue function. Obes. Facts 2017, 10, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Yin, D.P.; Gao, Q.; Ma, L.L.; Yan, W.; Williams, P.E.; McGuinness, O.P.; Wasserman, D.H.; Abumrad, N.N. Assessment of different bariatric surgeries in the treatment of obesity and insulin resistance in mice. Ann. Surg. 2011, 254, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Houpt, K.A.; Houpt, T.R.; Pond, W.G. The pig as a model for the study of obesity and of control of food intake: A review. Yale J. Boil. Med. 1979, 52, 307–329. [Google Scholar]
- Tang, L.-L.; Tang, X.-H.; Li, X.; Yu, H.-B.; Xie, Z.-G.; Liu, X.-Y.; Zhou, Z.-G. Effect of high-fat or high-glucose diet on obesity and visceral adipose tissue in mice. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2014, 36, 614–619. [Google Scholar]
- Chen, H.; Guan, K.; Qi, X.; Wang, R.; Ma, Y. α-lactalbumin ameliorates hepatic lipid metabolism in high-fat-diet induced obese C57BL/6J mice. J. Funct. Foods 2020, 75, 104253. [Google Scholar] [CrossRef]
- Chu, D.-T.; Malinowska, E.; Jura, M.; Kozak, L.P. C57BL/6J mice as a polygenic developmental model of diet-induced obesity. Physiol. Rep. 2017, 5, e13093. [Google Scholar] [CrossRef]
- Ghanemi, A.; Melouane, A.; Mucunguzi, O.; Yoshioka, M.; St-Amand, J. Energy and metabolic pathways in trefoil factor family member 2 (Tff2) KO mice beyond the protection from high-fat diet-induced obesity. Life Sci. 2018, 215, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Zhou, A.; Ward, R. Milk polar lipids modulate lipid metabolism, gut permeability, and systemic inflammation in high-fat-fed C57BL/6J ob/ob mice, a model of severe obesity. J. Dairy Sci. 2019, 102, 4816–4831. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.; Ali, T.; Kim, M.W.; Khan, A.; Jo, M.H.; Rehman, S.U.; Khan, M.S.; Abid, N.B.; Khan, M.; Ullah, R.; et al. Adiponectin homolog novel osmotin protects obesity/diabetes-induced NAFLD by upregulating AdipoRs/PPARα signaling in ob/ob and db/db transgenic mouse models. Metabolism 2019, 90, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Yanagita, T.; Tsuge, K.; Koga, M.; Inoue, N.; Nagao, K. Eicosapentaenoic acid-containing polar lipids from seaweed Susabinori (Pyropia yezoensis) alleviate hepatic steatosis in obese db/db mice. Arch. Biochem. Biophys. 2020, 691, 108486. [Google Scholar] [CrossRef]
- Noratto, G.D.; Murphy, K.; Chew, B.P. Quinoa intake reduces plasma and liver cholesterol, lessens obesity-associated inflammation, and helps to prevent hepatic steatosis in obese db/db mouse. Food Chem. 2019, 287, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Grigorova, N.; Ivanova, Z.; Bjorndal, B.; Vachkova, E.; Penchev, G.; Berge, R.; Ribarski, S.; Georgieva, T.M.; Yonkova, P.; Georgiev, I.P. Effect of fish oil supplementation and restricted feeding on body fat distribution and blood lipid profile in a rabbit model of castration-induced obesity. Res. Vet. Sci. 2019, 124, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Georgiev, I.P.; Georgieva, T.M.; Ivanov, V.; Dimitrova, S.; Kanelov, I.; Vlaykova, T.; Tanev, S.; Zaprianova, D.; Dichlianova, E.; Penchev, G.; et al. Effects of castration-induced visceral obesity and antioxidant treatment on lipid profile and insulin sensitivity in New Zealand white rabbits. Res. Vet. Sci. 2011, 90, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Keleher, M.R.; Zaidi, R.; Shah, S.; Oakley, M.E.; Pavlatos, C.; El Idrissi, S.; Xing, X.; Li, D.; Wang, T.; Cheverud, J.M. Maternal high-fat diet associated with altered gene expression, DNA methylation, and obesity risk in mouse offspring. PLoS ONE 2018, 13, e0192606. [Google Scholar]
- Liu, J.; He, Z.; Ma, N.; Chen, Z.Y. Beneficial Effects of Dietary Polyphenols on High-Fat Diet-Induced Obesity Linking with Modulation of Gut Microbiota. J. Agric. Food Chem. 2020, 68, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Herbert, D.; Franz, S.; Popkova, Y.; Anderegg, U.; Schiller, J.; Schwede, K.; Lorz, A.; Simon, J.C.; Saalbach, A. High-fat diet exacerbates early psoriatic skin inflammation independent of obesity: Saturated fatty acids as key players. J. Investig. Dermatol. 2018, 138, 1999–2009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Lu, X.; Li, X.; Du, P.; Qin, G. High-fat diet triggers obesity-related early infiltration of macrophages into adipose tissue and transient reduction of blood monocyte count. Mol. Immunol. 2020, 117, 139–146. [Google Scholar] [CrossRef]
- Tung, Y.-T.; Chen, H.-L.; Wu, H.-S.; Ho, M.-H.; Chong, K.-Y.; Chen, C.-M. Kefir peptides prevent hyperlipidemia and obesity in high-fat-diet-induced obese rats via lipid metabolism modulation. Mol. Nutr. Food Res. 2018, 62, 62. [Google Scholar] [CrossRef]
- Heydemann, A. An overview of murine high fat diet as a model for type 2 diabetes mellitus. J. Diabetes Res. 2016, 2016, 2902351. [Google Scholar] [CrossRef] [Green Version]
- Varlamov, O. Western-style diet, sex steroids and metabolism. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 1147–1155. [Google Scholar] [CrossRef]
- Komorowski, J.M. Role of the hypothalamus in the pathogenesis of obesity in the light of modern studies. Pol. Tyg. Lek. 1978, 33, 657–659. [Google Scholar] [PubMed]
- Mercer, J.G.; Speakman, J.R. Hypothalamic neuropeptide mechanisms for regulating energy balance: From rodent models to human obesity. Neurosci. Biobehav. Rev. 2001, 25, 101–116. [Google Scholar] [CrossRef]
- Nishida, Y.; Yoshioka, M.; St-Amand, J. Regulation of hypothalamic gene expression by glucocorticoid: Implications for energy homeostasis. Physiol. Genomics 2006, 25, 96–104. [Google Scholar] [CrossRef] [Green Version]
- Nishida, Y.; Yoshioka, M.; St-Amand, J. The top 10 most abundant transcripts are sufficient to characterize the organs functional specificity: Evidences from the cortex, hypothalamus and pituitary gland. Gene 2005, 344, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Thaler, J.P.; Yi, C.X.; Schur, E.A.; Guyenet, S.J.; Hwang, B.H.; Dietrich, M.O.; Zhao, X.; Sarruf, D.A.; Izgur, V.; Maravilla, K.R.; et al. Obesity is associated with hypothalamic injury in rodents and humans. J. Clin. Investig. 2012, 122, 153–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velloso, L.A.; Schwartz, M.W. Altered hypothalamic function in diet-induced obesity. Int. J. Obes. (Lond.) 2011, 35, 1455–1465. [Google Scholar] [CrossRef] [Green Version]
- Mercer, J.G.; Archer, Z.A. Putting the diet back into diet-induced obesity: Diet-induced hypothalamic gene expression. European Eur. J. Pharmacol. 2008, 585, 31–37. [Google Scholar] [CrossRef]
- De Giorgio, M.R.; Yoshioka, M.; St-Amand, J. Feeding induced changes in the hypothalamic transcriptome. Clin. Chim. Acta. 2009, 406, 103–107. [Google Scholar] [CrossRef]
- Stahl, S.M. Neuropharmacology of obesity: My receptors made me eat it. J. Clin. Psychiatry 1998, 59, 447–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, C.F.; Panciera, J.I.; Sabino, V.; Cottone, P. Neuropharmacology of compulsive eating. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2018, 373, 20170024. [Google Scholar] [CrossRef] [PubMed]
- Leibowitz, S.F.; Alexander, J.T. Hypothalamic serotonin in control of eating behavior, meal size, and body weight. Biol. Psychiatry 1998, 44, 851–864. [Google Scholar] [CrossRef]
- Weiss, G.F.; Rogacki, N.; Fueg, A.; Buchen, D.; Leibowitz, S.F. Impact of hypothalamic d-norfenfluramine and peripheral d-fenfluramine injection on macronutrient intake in the rat. Brain Res. Bull. 1990, 25, 849–859. [Google Scholar] [CrossRef]
- Weiss, G.F.; Rogacki, N.; Fueg, A.; Buchen, D.; Suh, J.S.; Wong, D.T.; Leibowitz, S.F. Effect of hypothalamic and peripheral fluoxetine injection on natural patterns of macronutrient intake in the rat. Psychopharmacology 1991, 105, 467–476. [Google Scholar] [CrossRef]
- van Lingen, M.; Sidorova, M.; Alenina, N.; Klempin, F. Lack of Brain Serotonin Affects Feeding and Differentiation of Newborn Cells in the Adult Hypothalamus. Front. Cell Dev. Biol. 2019, 7, 65. [Google Scholar] [CrossRef] [PubMed]
- Rao, D.P.; Patel, P.; Roberts, K.C.; Thompson, W. Obesity and healthy aging: Social, functional and mental well-being among older Canadians. Health Promot. Chronic Dis. Prev. Can. 2018, 38, 437–444. [Google Scholar] [CrossRef] [Green Version]
- Anonymous. Body mass index (BMI) charts. Pediatr. Dent. 2017, 39, 461–462. [Google Scholar]
- Chu, D.-T.; Nguyet, N.T.M.; Nga, V.T.; Lien, N.V.T.; Vo, D.D.; Ngoc, V.T.N.; Son, L.H.; Le, D.-H.; Van Tu, P.; Van To, T.; et al. An update on obesity: Mental consequences and psychological interventions. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 155–160. [Google Scholar] [CrossRef]
- Oliosa, P.R.; Zaniqueli, D.; Alvim, R.O.; Barbosa, M.C.R.; Mill, J.G. Body fat percentage is better than indicators of weight status to identify children and adolescents with unfavorable lipid profile. J. Pediatr. 2019, 95, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Rogers, P.; Webb, G.P. Estimation of body fat in normal and obese mice. Br. J. Nutr. 1980, 43, 83–86. [Google Scholar] [CrossRef]
- Air, E.L.; Strowski, M.Z.; Benoit, S.C.; Conarello, S.L.; Salituro, G.M.; Guan, X.-M.; Liu, K.; Woods, S.C.; Zhang, B.B. Small molecule insulin mimetics reduce food intake and body weight and prevent development of obesity. Nat. Med. 2002, 8, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Melega, W.P.; Lacan, G.; Gorgulho, A.A.; Behnke, E.J.; de Salles, A.A.F. Hypothalamic deep brain stimulation reduces weight gain in an obesity-animal model. PLoS ONE 2012, 7, e30672. [Google Scholar] [CrossRef]
- Shoelson, S.E.; Herrero, L.; Naaz, A. Obesity, inflammation, and insulin resistance. Gastroenterology 2007, 132, 2169–2180. [Google Scholar] [CrossRef] [PubMed]
- Fock, K.M.; Khoo, J. Diet and exercise in management of obesity and overweight. J. Gastroenterol. Hepatol. 2013, 28, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Rebello, C.J.; Greenway, F.L. Obesity medications in development. Expert Opin. Investig. Drugs 2020, 29, 63–71. [Google Scholar] [CrossRef]
- Wolfe, B.M.; Kvach, E.; Eckel, R.H. Treatment of obesity: Weight loss and bariatric surgery. Circ. Res. 2016, 118, 1844–1855. [Google Scholar] [CrossRef]
- Monteiro, R.; Azevedo, I. Chronic inflammation in obesity and the metabolic syndrome. Mediat. Inflamm. 2010, 2010, 1–10. [Google Scholar] [CrossRef]
- Sonne, S.B.; Yadav, R.; Yin, G.; Dalgaard, M.D.; Myrmel, L.S.; Gupta, R.; Wang, J.; Madsen, L.; Kajimura, S.; Kristiansen, K. Obesity is associated with depot-specific alterations in adipocyte DNA methylation and gene expression. Adipocyte 2017, 6, 124–133. [Google Scholar] [CrossRef]
- Ghanemi, A.; Melouane, A.; Yoshioka, M.; St-Amand, J. Exercise and high-fat diet in obesity: Functional genomics perspectives of two energy homeostasis pillars. Genes 2020, 11, 875. [Google Scholar] [CrossRef]
- Mucunguzi, O.; Melouane, A.; Ghanemi, A.; Yoshioka, M.; Boivin, A.; Calvo, E.L.; St-Amand, J. Identification of the principal transcriptional regulators for low-fat and high-fat meal responsive genes in small intestine. Nutr. Metab. 2017, 14, 66. [Google Scholar] [CrossRef] [Green Version]
- Sardon Puig, L.; Pillon, N.J.; Näslund, E.; Krook, A.; Zierath, J.R. Influence of obesity, weight loss, and free fatty acids on skeletal muscle clock gene expression. Am. J. Physiol. Endocrinol. Metab. 2020, 318, e1–e10. [Google Scholar] [CrossRef]
- Ghanemi, A.; Yoshioka, M.; St-Amand, J. High-fat diet-induced trefoil factor family member 2 (TFF2) to counteract the immune-mediated damage in mice. Animals 2021, 11, 258. [Google Scholar] [CrossRef]
- Ghanemi, A.; Yoshioka, M.; St-Amand, J. Secreted protein acidic and rich in cysteine as a regeneration factor: Beyond the tissue repair. Life 2021, 11, 38. [Google Scholar] [CrossRef] [PubMed]
- Drel, V.R.; Mashtalir, N.; Ilnytska, O.; Shin, J.; Li, F.; Lyzogubov, V.V.; Obrosova, I.G. The leptin-deficient (ob/ob) mouse: A new animal model of peripheral neuropathy of type 2 diabetes and obesity. Diabetes 2006, 55, 3335–3343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malloy, V.L.; Perrone, C.E.; Mattocks, D.A.; Ables, G.P.; Caliendo, N.S.; Orentreich, D.S.; Orentreich, N. Methionine restriction prevents the progression of hepatic steatosis in leptin-deficient obese mice. Metabolism 2013, 62, 1651–1661. [Google Scholar] [CrossRef]
- Neelankal John, A.; Ram, R.; Jiang, F.X. RNA-seq analysis of islets to characterise the dedifferentiation in type 2 diabetes model mice db/db. Endocr. Pathol. 2018, 29, 207–221. [Google Scholar] [CrossRef]
- Bogdanov, P.; Corraliza, L.; Villena, J.A.; Carvalho, A.R.; García-Arumí, J.; Ramos, D.; Ruberte, J.; Simó, R.; Hernández, C. The db/db mouse: A useful model for the study of diabetic retinal neurodegeneration. PLoS ONE 2014, 9, e97302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vareniuk, I.; Pavlov, I.A.; Drel, V.R.; Lyzogubov, V.V.; Ilnytska, O.; Bell, S.R.; Tibrewala, J.; Groves, J.T.; Obrosova, I.G. Nitrosative stress and peripheral diabetic neuropathy in leptin-deficient (ob/ob) mice. Exp. Neurol. 2007, 205, 425–436. [Google Scholar] [CrossRef]
- Yu, F.; Han, W.; Zhan, G.; Li, S.; Jiang, X.; Wang, L.; Xiang, S.; Zhu, B.; Yang, L.; Luo, A.; et al. Abnormal gut microbiota composition contributes to the development of type 2 diabetes mellitus in db/db mice. Aging 2019, 11, 10454–10467. [Google Scholar] [CrossRef]
- Larter, C.Z.; Yeh, M.M.; van Rooyen, D.M.; Teoh, N.C.; Brooling, J.; Hou, J.Y.; Williams, J.; Clyne, M.; Nolan, C.J.; Farrell, G.C. Roles of adipose restriction and metabolic factors in progression of steatosis to steatohepatitis in obese, diabetic mice. J. Gastroenterol. Hepatol. 2009, 24, 1658–1668. [Google Scholar] [CrossRef] [PubMed]
- Lauterbach, M.A.R.; Wunderlich, F.T. Macrophage function in obesity-induced inflammation and insulin resistance. Pflügers Archiv 2017, 469, 385–396. [Google Scholar] [CrossRef] [Green Version]
- Van der Heijden, R.A.; Sheedfar, F.; Morrison, M.C.; Hommelberg, P.P.; Kor, D.; Kloosterhuis, N.J.; Gruben, N.; Youssef, S.A.; de Bruin, A.; Hofker, M.H.; et al. High-fat diet induced obesity primes inflammation in adipose tissue prior to liver in C57BL/6j mice. Aging 2015, 7, 256–268. [Google Scholar] [CrossRef] [Green Version]
- Engin, A. Obesity-associated breast cancer: Analysis of risk factors. Adv. Exp. Med. Biol. 2017, 960, 571–606. [Google Scholar] [PubMed]
- Kompaniyets, L.; Goodman, A.B.; Belay, B.; Freedman, D.S.; Sucosky, M.S.; Lange, S.J.; Gundlapalli, A.V.; Boehmer, T.K.; Blanck, H.M. Body mass index and risk for COVID-19—Related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death—United States, March–December 2020. MMWR Morb. Mortal Wkly. Rep. 2021, 70, 355–361. [Google Scholar] [CrossRef]
- Torre, L.A.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global cancer incidence and mortality rates and trends—An update. Cancer Epidemiol. Biomark. Prev. 2015, 25, 16–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2014, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Duranti, S.; Ferrario, C.; van Sinderen, D.; Ventura, M.; Turroni, F. Obesity and microbiota: An example of an intricate relationship. Genes Nutr. 2017, 12, 18. [Google Scholar] [CrossRef] [Green Version]
- Madsen, L.; Myrmel, L.S.; Fjære, E.; Liaset, B.; Kristiansen, K. Links between Dietary Protein Sources, the Gut Microbiota, and Obesity. Front Physiol. 2017, 8, 1047. [Google Scholar] [CrossRef] [Green Version]
- Cuevas-Sierra, A.; Ramos-Lopez, O.; Riezu-Boj, J.I.; Milagro, F.I.; Martinez, J.A. Diet, Gut Microbiota, and Obesity: Links with Host Genetics and Epigenetics and Potential Applications. Adv. Nutr. 2019, 10, s17–s30. [Google Scholar] [CrossRef] [Green Version]
- Lee, P.; Yacyshyn, B.R.; Yacyshyn, M.B. Gut microbiota and obesity: An opportunity to alter obesity through faecal microbiota transplant (FMT). Diabetes Obes. Metab. 2019, 21, 479–490. [Google Scholar] [CrossRef]
- Marotz, C.A.; Zarrinpar, A. Treating Obesity and Metabolic Syndrome with Fecal Microbiota Transplantation. Yale J. Biol. Med. 2016, 89, 383–388. [Google Scholar]
- Aron-Wisnewsky, J.; Clément, K.; Nieuwdorp, M. Fecal Microbiota Transplantation: A Future Therapeutic Option for Obesity/Diabetes? Curr. Diab. Rep. 2019, 19, 51. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Cai, Y. Gut microbiota and obesity: Implications for fecal microbiota transplantation therapy. Hormones (Athens) 2017, 16, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Mazloom, K.; Siddiqi, I.; Covasa, M. Probiotics: How Effective Are They in the Fight against Obesity? Nutrients 2019, 11, 258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fontané, L.; Benaiges, D.; Goday, A.; Llauradó, G.; Pedro-Botet, J. Influence of the microbiota and probiotics in obesity. Clin. Investig. Arterioscler. 2018, 30, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Nova, E.; Pérez de Heredia, F.; Gómez-Martínez, S.; Marcos, A. The Role of Probiotics on the Microbiota: Effect on Obesity. Nutr Clin. Pract. 2016, 31, 387–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katsiki, N.; Tousoulis, D. Diabetes mellitus and comorbidities: A bad romance. Hellenic J. Cardiol. 2020, 61, 23–25. [Google Scholar] [CrossRef] [PubMed]
- Lehrke, M.; Marx, N. Diabetes mellitus and heart failure. Am. J. Cardiol. 2017, 120, S37–S47. [Google Scholar] [CrossRef] [Green Version]
- Wojciechowska, J.; Krajewski, W.; Bolanowski, M.; Kręcicki, T.; Zatoński, T. Diabetes and cancer: A review of current knowledge. Exp. Clin. Endocrinol. Diabetes 2016, 124, 263–275. [Google Scholar] [CrossRef]
- Cryer, M.J.; Horani, T.; DiPette, D.J. Diabetes and hypertension: A comparative review of current guidelines. J. Clin. Hypertens. 2016, 18, 95–100. [Google Scholar] [CrossRef]
- Shifflett, K.; Marzi, A. Marburg virus pathogenesis—Differences and similarities in humans and animal models. Virol. J. 2019, 16, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
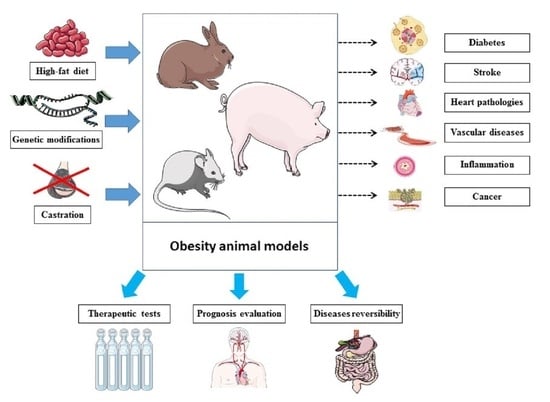
| Developed Disease (Models) | Obesity-Induction and Animal Models | References |
|---|---|---|
| Peripheral diabetic neuropathy | ob/ob mice | [105] |
| Hepatic steatosis | ob/ob mice | [106] |
| Type 2 diabetes and diabetic retinal neurodegeneration | db/db mice | [107,108] |
| Type 2 diabetes | ob/ob mice | [109] |
| Abnormal gut microbiota composition | db/db mice | [110] |
| Steatohepatitis | foz/foz mice fed a high-fat diet | [111] |
| Inflammation | Mice fed a high-fat diet | [112,113] |
| Insulin resistance | Mice fed a high-fat diet | [113] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghanemi, A.; Yoshioka, M.; St-Amand, J. Obese Animals as Models for Numerous Diseases: Advantages and Applications. Medicina 2021, 57, 399. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina57050399
Ghanemi A, Yoshioka M, St-Amand J. Obese Animals as Models for Numerous Diseases: Advantages and Applications. Medicina. 2021; 57(5):399. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina57050399
Chicago/Turabian StyleGhanemi, Abdelaziz, Mayumi Yoshioka, and Jonny St-Amand. 2021. "Obese Animals as Models for Numerous Diseases: Advantages and Applications" Medicina 57, no. 5: 399. https://0-doi-org.brum.beds.ac.uk/10.3390/medicina57050399