Cosmetic, Biomedical and Pharmaceutical Applications of Fish Gelatin/Hydrolysates
Abstract
:1. Introduction
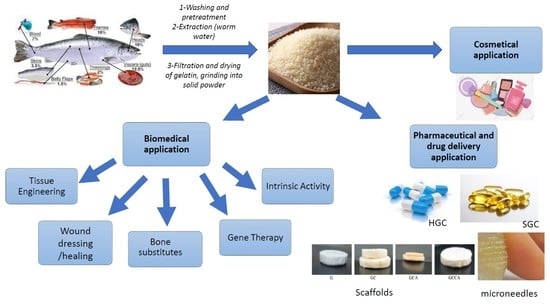
2. Cosmetic Applications
3. Biomedical Applications
3.1. Intrinsic Activities of Fish Gelatin Hydrolystaes
3.1.1. Antihypertensive Activity
3.1.2. Antioxidant Activity
- The polypeptide molecular weight: lower molecular weight peptides had higher antioxidant activity.
- The presence of hydrophobic amino acids, preferably aromatic amino acids, at the carboxyl and amino terminals.
- Specific free amino acids or sequences, like the dipeptide of Gly-Tyr and the amino acid Tyr, subfractions with peptides rich in Arg, Tyr, and Phe; Tyr.
3.1.3. Dipeptidyl Peptidase Inhibitory Activity
3.1.4. Anti-Cancer Activity
3.1.5. Antimicrobial Activity
3.1.6. Nutritional Supplement
3.2. Wound Dressing and Wound Healing
3.3. Gene Therapy
3.4. Tissue Engineering
3.5. Bone Substitutes
4. Pharmaceutical Applications
4.1. Production of Drug Capsules
4.2. Coating of Microparticles/Oils by Coacervation/Phase Separation
4.3. Tablet Coating
- -
- Fish gelatin 5–25 w/w %
- -
- Sodium stearoyl lactylate
- -
- Sodium sulfate
- -
- Propylene glycol monostearate in water
- -
- Sodium acetate
- -
- Sodium lactate.
4.4. Emulsion Stabilizers
4.5. Drug Delivery
4.5.1. Microspheres
4.5.2. Nanospheres
4.5.3. Scaffolds
4.5.4. Microneedles
4.5.5. Hydrogels
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Abd Elgadir, M.; Mirghani, M.E.; Adam, A. Fish Gelatin and Its Applications in Selected Pharmaceutical Aspects as Alternative Source to Pork Gelatin. J. Food Agric. Environ. 2013, 11, 73–79. [Google Scholar] [CrossRef]
- Karim, A.; Bhat, R. Fish Gelatin: Properties, Challenges, and Prospects as an Alternative to Mammalian Gelatins. Food Hydrocoll. 2009, 23, 563–576. [Google Scholar] [CrossRef]
- Schrieber, R.; Gareis, H. Gelatine Handbook: Theory and Industrial Practice, 1st ed.; John Wiley & Sons: Eberbach, Germany, 2007; p. 347. [Google Scholar]
- León-López, A.; Morales-Peñaloza, A.; Martínez-Juárez, V.M.; Vargas-Torres, A.; Zeugolis, D.I.; Aguirre-Álvarez, G. Hydrolyzed Collagen-Sources and Applications. Molecules 2019, 24, 4031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rawdkuen, S.; Thitipramote, N.; Benjakul, S. Preparation and Functional Characterisation of Fish Skin Gelatin and Comparison with Commercial Gelatin. J. Food Sci. Technol. 2013, 48, 1093–1102. [Google Scholar] [CrossRef]
- Eastoe, J. The Amino Acid Composition of Fish Collagen and Gelatin. Biochem. J. 1957, 65, 363–368. [Google Scholar] [CrossRef] [Green Version]
- Boran, G.; Regenstein, J.M. Fish Gelatin. Adv. Food Nutr. Res. 2010, 60, 119–143. [Google Scholar] [CrossRef]
- Karayannakidis, P.D.; Zotos, A. Fish Processing by-Products as a Potential Source of Gelatin: A Review. J. Aquat. Food Prod. Technol. 2016, 25, 65–92. [Google Scholar] [CrossRef]
- Gómez-Guillén, M.; Pérez-Mateos, M.; Gómez-Estaca, J.; López-Caballero, E.; Giménez, B.; Montero, P. Fish Gelatin: A Renewable Material for Developing Active Biodegradable Films. Trends Food Sci. Technol. 2009, 20, 3–16. [Google Scholar] [CrossRef] [Green Version]
- Doğdu, S.A.; Turan, C.; Ayas, D. Isolation and Characterization of Collagen and Gelatin from Skin of Silver Cheeked Pufferfish Lagocephalus Sceleratus for Pharmaceutical and Biomedical Applications. Period. Eng. Nat. Sci. 2019, 308–314. [Google Scholar] [CrossRef]
- Karim, A.A.; Bhat, R. Gelatin Alternatives for the Food Industry: Recent Developments, Challenges and Prospects. Trends Food Sci. Technol. 2008, 19, 644–656. [Google Scholar] [CrossRef]
- Muhammad, K.M.L.; Ariffin, F.; Abd Razak, H.K.B.; Sulaiman, P.D.S. Review of Fish Gelatin Extraction, Properties and Packaging Applications. Food Sci. Nutr. 2016, 56, 47–59. [Google Scholar]
- Simpson, B.K.; Nollet, L.M.; Toldrá, F.; Benjakul, S.; Paliyath, G.; Hui, Y. Food Biochemistry and Food Processing, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar] [CrossRef]
- Arnesen, J.A.; Gildberg, A. Extraction and Characterisation of Gelatine from Atlantic Salmon (Salmo Salar) Skin. Bioresour. Technol. 2007, 98, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Montero, M.; Acosta, Ó.G. Tuna Skin Gelatin Production: Optimization of Extraction Steps and Process Scale-Up. CyTA J. Food 2020, 18, 580–590. [Google Scholar] [CrossRef]
- Benjakul, S.; Kittiphattanabawon, P.; Regenstein, J.M. Fish Gelatin. J. Food Biochem. 2012, 388–405. [Google Scholar] [CrossRef]
- Khrunyk, Y.; Lach, S.; Petrenko, I.; Ehrlich, H. Progress in Modern Marine Biomaterials Research. Mar. Drugs 2020, 18, 589. [Google Scholar] [CrossRef]
- Wasswa, J.; Tang, J.; Gu, X. Utilization of Fish Processing by-Products in the Gelatin Industry. Food Rev. Int. 2007, 23, 159–174. [Google Scholar] [CrossRef]
- Regenstein, J.; Zhou, P. Food Biochemistry and Food Processing, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2007; pp. 279–303. [Google Scholar] [CrossRef]
- Alves, A.L.; Marques, A.L.; Martins, E.; Silva, T.H.; Reis, R.L. Cosmetic Potential of Marine Fish Skin Collagen. Cosmetics 2017, 4, 39. [Google Scholar] [CrossRef] [Green Version]
- Jamilah, B.; Harvinder, K. Properties of Gelatins from Skins of Fish—Black Tilapia (Oreochromis Mossambicus) and Red Tilapia (Oreochromis Nilotica). Food Chem. 2002, 77, 81–84. [Google Scholar] [CrossRef]
- Kim, Y.-J.; Uyama, H. Biocompatible Hydrogel Formation of Gelatin from Cold Water Fish via Enzymatic Networking. Polym. J. 2007, 39, 1040–1046. [Google Scholar] [CrossRef] [Green Version]
- Derkach, S.R.; Voron’ko, N.G.; Yuliya, A.; Kuchina, Y.A.; Kolotova, D.S. Modified Fish Gelatin as an Alternative to Mammalian Gelatin in Modern Food Technologies. Polymers 2020, 12, 3051. [Google Scholar] [CrossRef]
- Nitsuwat, S.; Zhang, P.; Ng, K.; Fang, Z. Fish Gelatin As An Alternative To Mammalian Gelatin For Food Industry: A Meta-Analysis. Lwt Food Sci. Tech. 2021, 141, 110899. [Google Scholar] [CrossRef]
- Siburian, W.Z.; Rochima, E.; Andriani, Y.; Praseptiangga, D. Fish Gelatin (Definition, Manufacture, Analysis of Quality Characteristics, and Application): A Review. Int. J. Fish. Aquat. 2020, 8, 90–95. [Google Scholar]
- Da Trindade Alfaro, A.; Balbinot, E.; Weber, C.I.; Tonial, I.B.; Machado-Lunkes, A. Fish Gelatin: Characteristics, Functional Properties, Applications and Future Potentials. Food Eng. Rev. 2015, 7, 33–44. [Google Scholar] [CrossRef]
- Kavoosi, G.; Rahmatollahi, A.; Dadfar, S.M.M.; Purfard, A.M. Effects of Essential Oil on the Water Binding Capacity, Physico-Mechanical Properties, Antioxidant and Antibacterial Activity of Gelatin Films. Lwt Food Sci. Tech. 2014, 57, 556–561. [Google Scholar] [CrossRef]
- Sánchez, J.T.; García, A.V.; Martínez-Abad, A.; Vilaplana, F.; Jiménez, A.; Garrigós, M.C. Physicochemical and Functional Properties of Active Fish Gelatin-Based Edible Films Added with Aloe Vera Gel. Foods 2020, 9, 1248. [Google Scholar] [CrossRef]
- Barcellos, C.C.C.; Fonseca, A.B.M.; Aronovich, M.; Brígida, A.I.S.; Keller, L.A.M.; Marques de Mesquita, E. Antioxidant Effect Of The Hydrolysate Derived From Fish Gelatin On The Shelf Life Of Rainbow Trout. Int. J. Dev. Res. 2020, 10, 36164–36170. [Google Scholar] [CrossRef]
- Denis, A.; Brambati, N.; Dessauvages, B.; Guedj, S.; Ridoux, C.; Meffre, N.; Autier, C. Molecular Weight Determination of Hydrolyzed Collagens. Food Hydrocoll. 2008, 22, 989–994. [Google Scholar] [CrossRef]
- Kim, S.-K.; Ngo, D.-H.; Vo, T.-S. Marine Fish-Derived Bioactive Peptides as Potential Antihypertensive Agents. J. Pharm. Pharm. Sci. 2012, 65, 249–260. [Google Scholar] [CrossRef]
- Choonpicharn, S.; Jaturasitha, S.; Rakariyatham, N.; Suree, N.; Niamsup, H. Antioxidant and Antihypertensive Activity of Gelatin Hydrolysate from Nile Tilapia Skin. J. Food Sci. Technol. 2015, 52, 3134–3139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neves, A.C.; Harnedy, P.A.; O’Keeffe, M.B.; Alashi, M.A.; Aluko, R.E.; FitzGerald, R.J. Peptide Identification in a Salmon Gelatin Hydrolysate with Antihypertensive, Dipeptidyl Peptidase Iv Inhibitory and Antioxidant Activities. Food Res. Int. 2017, 100, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Vo, T.S.; Ngo, D.H.; Kim, J.A.; Ryu, B.; Kim, S.K. An Antihypertensive Peptide from Tilapia Gelatin Diminishes Free Radical Formation in Murine Microglial Cells. J. Adv. Pharm. 2011, 59, 12193–12197. [Google Scholar] [CrossRef]
- Yuan, L.; Sun, L.; Zhunag, Y. Preparation and Identification of Novel Inhibitory Angiotensin-I-Converting Enzyme Peptides from Tilapia Skin Gelatin Hydrolysates: Inhibition Kinetics and Molecular Docking. Food Funct. 2018, 9, 5251–5259. [Google Scholar] [CrossRef]
- Ngo, D.-H.; Kang, K.-H.; Ryu, B.; Vo, T.-S.; Jung, W.-K.; Byun, H.-G.; Kim, S.-K. Angiotensin-I Converting Enzyme Inhibitory Peptides from Antihypertensive Skate (Okamejei Kenojei) Skin Gelatin Hydrolysate in Spontaneously Hypertensive Rats. Food Chem. 2015, 174, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Li, B.; Liu, Z.; Dong, S.; Zhao, X.; Zeng, M. Antihypertensive Effect and Purification of an Ace Inhibitory Peptide from Sea Cucumber Gelatin Hydrolysate. Process Biochem. 2007, 42, 1586–1591. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, M.; Yaping Shi, Y.; Qiao, R.; Tang, W.; Sunc, Z. Production of the Angiotensin I Converting. Enzyme Inhibitory Peptides and Isolation of Four Novel Peptides from Jellyfish (Rhopilema Esculentum) Protein Hydrolysate. J. Sci. Food Agric. 2016, 96, 3240–3248. [Google Scholar] [CrossRef]
- Matsumoto, H. Clinical Effects of Fish Type I Collagen Hydrolysate on Skin Properties. ITE. Lett. Batter. New Technol. Med. 2006, 7, 386–390. [Google Scholar]
- Orwin, E.J.; Hubel, A. In Vitro Culture Characteristics of Corneal Epithelial, Endothelial, and Keratocyte Cells in a Native Collagen Matrix. Tissue Eng. 2000, 6, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Xu, T.; Yan, J.; Li, X.; Xie, Y.; Chen, H. Fabrication and Characterization of Matrine-Loaded Konjac Glucomannan/Fish Gelatin Composite Hydrogel as Antimicrobial Wound Dressing. Food Hydrocoll. 2020, 104, 105702–105735. [Google Scholar] [CrossRef]
- Lv, L.C.; Huang, Q.Y.; Ding, W.; Xiao, X.H.; Zhang, H.Y.; Xiong, L.X. Fish Gelatin: The Novel Potential Applications. J. Funct. Foods 2019, 63, 103581103594. [Google Scholar] [CrossRef]
- Atef, M.; Ojagh, S.M. Health Benefits and Food Applications of Bioactive Compounds from Fish Byproducts: A Review. J. Funct. Foods 2017, 35, 673–681. [Google Scholar] [CrossRef]
- Lin, L.; Lv, S.; Li, B. Angiotensin-I-Converting Enzyme (Ace)-Inhibitory and Antihypertensive Properties of Squid Skin Gelatin Hydrolysates. Food Chem. 2012, 131, 225–230. [Google Scholar] [CrossRef]
- Mendis, E.; Rajapakse, N.; Kim, S.-K. Antioxidant Properties of a Radical-Scavenging Peptide Purified from Enzymatically Prepared Fish Skin Gelatin Hydrolysate. J. Adv. Pharm. 2005, 53, 581–587. [Google Scholar] [CrossRef]
- Nikoo, M.; Benjakul, S.; Xu, X. Antioxidant and Cryoprotective Effects of Amur Sturgeon Skin Gelatin Hydrolysate in Unwashed Fish Mince. Food Chem. 2015, 181, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Li-Chan, E.C.; Hunag, S.L.; Jao, C.L.; Ho, K.P.; Hsu, K.C. Peptides Derived from Atlantic Salmon Skin Gelatin as Dipeptidyl-Peptidase Iv Inhibitors. J. Adv. Pharm. 2012, 60, 973–978. [Google Scholar] [CrossRef] [PubMed]
- Alemán, A.; Pérez-Santín, E.; Bordenave-Juchereau, S.; Arnaudin, I.; Gómez-Guillén, M.; Montero, P. Squid Gelatin Hydrolysates with Antihypertensive, Anticancer and Antioxidant Activity. Food Res. Int. 2011, 44, 1044–1051. [Google Scholar] [CrossRef] [Green Version]
- Najafian, L.; Babji, A. A Review of Fish-Derived Antioxidant and Antimicrobial Peptides: Their Production, Assessment, and Applications. Peptides 2012, 33, 178–185. [Google Scholar] [CrossRef]
- Ennaas, N.; Hammami, R.; Gomaa, A.; Bédard, F.; Biron, É.; Subirade, M.; Beaulieu, L.; Fliss, I. Collagencin, an Antibacterial Peptide from Fish Collagen: Activity, Structure and Interaction Dynamics with Membrane. Biochem. Biophys. Res. Commun. 2016, 473, 642–647. [Google Scholar] [CrossRef]
- Gudipati, V. Fish Gelatin: A Versatile Ingredient for the Food and Pharmaceutical Industries. In Marine Proteins and Peptides: Biological Activities and Applications, 1st ed.; Kim, S.-K., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2013; pp. 271–295. [Google Scholar] [CrossRef]
- Jeevithan, E.; Qingbo, Z.; Bao, B.; Wu, W. Biomedical and Pharmaceutical Application of Fish Collagen and Gelatin: A Review. J. Nutr. Ther. 2013, 2, 218–227. [Google Scholar] [CrossRef]
- Liu, L.; Liu, L.; Liu, C.-K.; Fishman, M.L.; Hicks, K.B. Composite Films from Pectin and Fish Skin Gelatin or Soybean Flour Protein. J. Adv. Pharm. 2007, 55, 2349–2355. [Google Scholar] [CrossRef]
- Aguirre-Cruz, G.; León-López, A.; Cruz-Gómez, V.; Jiménez-Alvarado, R.; Aguirre-Álvarez, G. Collagen Hydrolysates for Skin Protection: Oral Administration and Topical Formulation. Antioxidants 2020, 9, 181. [Google Scholar] [CrossRef] [Green Version]
- Venkatesan, J.; Anil, S.; Kim, S.-K.; Shim, M.S. Marine Fish Proteins and Peptides for Cosmeceuticals: A Review. Mar. Drugs 2017, 15, 143. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Hou, H. Protective Effect of Gelatin Polypeptides from Pacific Cod (Gadus Macrocephalus) against Uv Irradiation-Induced Damages by Inhibiting Inflammation and Improving Transforming Growth Factor-Β/Smad Signaling Pathway. J. Photochem. Photobiol. B 2016, 162, 633–640. [Google Scholar] [CrossRef]
- Sun, L.; Zhang, Y.; Zhuang, Y. Antiphotoaging Effect and Purification of an Antioxidant Peptide from Tilapia (Oreochromis Niloticus) Gelatin Peptides. J. Funct. Foods 2013, 5, 154–162. [Google Scholar] [CrossRef]
- Guillén, G.; López Caballero, M.; Alemán, A.; Lacey, A.L.D.; Giménez, B.; Montero García, P. Antioxidant and Antimicrobial Peptide Fractions from Squid and Tuna Skin Gelatin. In Sea by-Products as Real Material: New Ways of Application; Bihan, E.L., Ed.; Transworld Research Network: Trivandrum, India, 2010. [Google Scholar]
- Huang, C.-Y.; Wu, T.-C.; Hong, Y.-H.; Hsieh, S.-L.; Guo, H.-R.; Huang, R.-H. Enhancement of Cell Adhesion, Cell Growth, Wound Healing, and Oxidative Protection by Gelatins Extracted from Extrusion-Pretreated Tilapia (Oreochromis sp.) Fish Scale. Molecules 2018, 23, 2406. [Google Scholar] [CrossRef] [Green Version]
- Zeng, Y.; Zhu, L.; Han, Q.; Liu, W.; Mao, X.; Li, Y.; Yu, N.; Feng, S.; Fu, Q.; Wang, X. Preformed Gelatin Microcryogels as Injectable Cell Carriers for Enhanced Skin Wound Healing. Acta Biomater. 2015, 25, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Xu, S.; Wang, Z. Pre-Treatment Optimization and Properties of Gelatin from Freshwater Fish Scales. Food Bioprod. Process. 2011, 89, 185–193. [Google Scholar] [CrossRef]
- Sghayyar, H.N.; Lim, S.S.; Ahmed, I.; Lai, J.Y.; Cheong, X.Y.; Chong, Z.W.; Lim, A.F.X.; Loh, H.-S. Fish Biowaste Gelatin Coated Phosphate-Glass Fibres for Wound-Healing Application. Eur. Polym. J. 2020, 122, 109386–109396. [Google Scholar] [CrossRef]
- Jeevithan, E.; Shakila, R.J.; Varatharajakumar, A.; Jeyasekaran, G.; Sukumar, D. Physico-Functional and Mechanical Properties of Chitosan and Calcium Salts Incorporated Fish Gelatin Scaffolds. Int. J. Biol. Macromol. 2013, 60, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Weir, B.; Zhao, X.; Meyerson, M. Somatic Alterations in the Human Cancer Genome. Cancer Cell 2004, 6, 433–438. [Google Scholar] [CrossRef] [Green Version]
- Williams, D.F. On the Mechanisms of Biocompatibility. Biomaterials 2008, 29, 2941–2953. [Google Scholar] [CrossRef]
- Yue, K.; Trujillo-de Santiago, G.; Alvarez, M.M.; Tamayol, A.; Annabi, N.; Khademhosseini, A. Synthesis, Properties, and Biomedical Applications of Gelatin Methacryloyl (Gelma) Hydrogels. Biomaterials 2015, 73, 254–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoon, H.J.; Shin, S.R.; Cha, J.M.; Lee, S.-H.; Kim, J.-H.; Do, J.T.; Song, H.; Bae, H. Cold Water Fish Gelatin Methacryloyl Hydrogel for Tissue Engineering Application. PLoS ONE 2016, 11, e0163902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallace, D.G.; Rosenblatt, J. Collagen Gel Systems for Sustained Delivery and Tissue Engineering. Adv. Drug Deliv. Rev. 2003, 55, 1631–1649. [Google Scholar] [CrossRef] [PubMed]
- Campiglio, C.E.; Nicola Contessi Negrini, N.C.; Silvia Farè, S.; Draghi, L. Cross-Linking Strategies for Electrospun Gelatin Scaffolds. Materials 2019, 12, 2476. [Google Scholar] [CrossRef] [Green Version]
- Piacentini, E.; Giorno, L.; Dragosavac, M.M.; Vladisavljević, G.T.; Holdich, R.G. Microencapsulation of Oil Droplets Using Cold Water Fish Gelatine/Gum Arabic Complex Coacervation by Membrane Emulsification. Food Res. Int. 2013, 53, 362–372. [Google Scholar] [CrossRef] [Green Version]
- Anvari, M.; Joyner, H.S. Effect of Fish Gelatin-Gum Arabic Interactions on Structural and Functional Properties of Concentrated Emulsions. Food Res. Int. 2017, 102, 1–7. [Google Scholar] [CrossRef]
- Beishenaliev, A.; Lim, S.S.; Tshai, K.Y.; Khiew, P.S.; Sghayyar, H.N.M.; Loh, H.-S. Fabrication and preliminary in vitro evaluation of ultravioletcrosslinked electrospun fish scale gelatin nanofibrous scaffolds. J. Mater. Sci. 2019, 30, 62. [Google Scholar] [CrossRef]
- Kathpalia, H.; Sharma, K.; Doshi, G. Recent Trends in Hard Gelatin Capsule Delivery System. J. Adv. Pharm. 2014, 4. [Google Scholar] [CrossRef]
- Prasad, V.D. Formulation and Modifying Drug Release from Hard and Soft Gelatin Capsules for Oral Drug Delivery. Int. J. Res. Dev. Pharm. Life Sci. 2017, 6, 2663–2677. [Google Scholar] [CrossRef]
- Apfel, M.A.; Ghebre-Sellassie, I.; Nesbitt, R.U. Water Insoluble Drugs Coated by Coacervated Fish Gelatin. U.S. Patent 5035896, 30 July 1991. [Google Scholar]
- Becsey, J.G. Process for Making Minute Capsules and Capsule Product. U.S. Patent 3594327, 20 July 1971. [Google Scholar]
- Choi, S.M.; Singh, D.; Kumar, A.; Oh, T.H.; Cho, Y.W.; Han, S.S. Porous Three-Dimensional Pva/Gelatin Sponge for Skin Tissue Engineering. Int. J. Polym. Mater. 2013, 62, 384–389. [Google Scholar] [CrossRef]
- Yu, C.T.; Wang, F.M.; Liu, Y.T.; Lee, A.K.X.; Lin, T.L.; Chen, Y.W. Enhanced Proliferation and Differentiation of Human Mesenchymal Stem Cell-Laden Recycled Fish Gelatin/Strontium Substitution Calcium Silicate 3d Scaffolds. Appl. Sci. 2020, 10, 2168. [Google Scholar] [CrossRef] [Green Version]
- Yun, B.G.; Lee, S.H.; Jeon, J.H.; Kim, S.W.; Jung, C.K.; Park, G.; Kim, S.Y.; Jeon, S.; Lee, M.S.; Park, S.H. Accelerated Bone Regeneration Via Three-Dimensional Cell-Printed Constructs Containing Human Nasal Turbinate-Derived Stem Cells as a Clinically Applicable Therapy. ACS Biomater. Sci. Eng. 2019, 5, 6171–6185. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.T.; Wang, F.M.; Liu, Y.T.; Ng, H.Y.; Jhong, Y.R.; Hung, C.H.; Chen, Y.W. Effect of Bone Morphogenic Protein-2-Loaded Mesoporous Strontium Substitution Calcium Silicate/Recycled Fish Gelatin 3d Cell-Laden Scaffold for Bone Tissue Engineering. Processes 2020, 8, 493. [Google Scholar] [CrossRef] [Green Version]
- Stegemann, S.; Bornem, C. Hard Gelatin Capsules Today-and Tomorrow. Capsugel Libr. 2002, 13–35. [Google Scholar]
- Park, H.J.; Yi, J.B.; Bae, H.J.; Kim, Y.T.; Cha, D.S. Film-Forming Composition for Hard Capsules Comprising Fish Gelatin and Its Preparation Method. U.S. Patent Application 12/162894, 12 March 2009. [Google Scholar]
- Gómez-Guillén, M.C.; Turnay, J.; Fernández-Dıaz, M.; Ulmo, N.; Lizarbe, M.A.; Montero, P. Structural and Physical Properties of Gelatin Extracted from Different Marine Species: A Comparative Study. Food Hydrocoll. 2002, 16, 25–34. [Google Scholar] [CrossRef] [Green Version]
- Nurilmala, M.; Adinugraha, S.C.; Jacoeb, A.M.; Susilawati, S.; Ochiai, Y. Evaluation of the Properties of Tuna Skin Gelatin as a Hard Capsule Material. Fish. Sci. 2020, 86, 917–924. [Google Scholar] [CrossRef]
- Daher, L.J.; Callahan, T.P.; Lonesky, S.M. Gelatin Spray Coating. U.S. Patent 6077540, 20 June 2000. [Google Scholar]
- Zhang, T.; Sun, R.; Ding, M.; Li, L.; Tao, N.; Wang, X.; Zhong, J. Commercial Cold-Water Fish Skin Gelatin and Bovine Bone Gelatin: Structural, Functional, and Emulsion Stability Differences. Lwt Food Sci. Tech. 2020, 109207. [Google Scholar] [CrossRef]
- Freiberg, S.; Zhu, X. Polymer Microspheres for Controlled Drug Release. Int. J. Pharm. 2004, 282, 1–18. [Google Scholar] [CrossRef]
- Mladenovska, K.; Kumbaradzi, E.; Dodov, G.; Makraduli, L.; Goracinova, K. Biodegradation and Drug Release Studies of Bsa Loaded Gelatin Microspheres. Int. J. Pharm. 2002, 242, 247–249. [Google Scholar] [CrossRef]
- Schwick, H.; Heide, K. Immunochemistry and Immunology of Collagen and Gelatin. In Modified Gelatins as Plasma Substitutes, 1st ed.; Hässig, A., Lundsgaard-Hansen, P., Nitschmann, H., Eds.; Karger Publishers: Basel, Switzerland, 1969; Volume 33, pp. 111–125. [Google Scholar] [CrossRef]
- Jahanshahi, M.; Sanati, M.; Hajizadeh, S.; Babaei, Z. Gelatin Nanoparticle Fabrication and Optimization of the Particle Size. Phys. Status Solidi 2008, 205, 2898–2902. [Google Scholar] [CrossRef]
- Lévy, M.C.; Rambourg, P.; Levy, J.; Potron, G. Microencapsulation Iv: Cross-Linked Hemoglobin Microcapsules. J. Pharm. Sci. 1982, 71, 759–762. [Google Scholar] [CrossRef]
- Murray, O.; Hall, M.; Kearney, P.; Green, R. Fast-Dispersing Dosage Forms Containing Fish Gelatin. U.S. Patent 9192580, 24 November 2015. [Google Scholar]
- Pathan, A.; Shaikh, J.; Shaikh, R. Gelatin Beads as Sustained Release Drug Delivery System. J. Innov. Pharm. Biol. Sci. 2014, 1, 10–16. [Google Scholar]
- Silva, D.M.; Vyas, H.K.N.; Sanderson-Smith, M.L.; Sencadas, V. Development and Optimization of Ciprofloxacin-Loaded Gelatin Microparticles by Single-Step Spray-Drying Technique. Powder Technol. 2018, 330, 201–209. [Google Scholar] [CrossRef] [Green Version]
- Subara, D.; Jaswir, I.; Alkhatib, M.F.R.; Noorbatcha, I.A. Synthesis of Fish Gelatin Nanoparticles and Their Application for the Drug Delivery Based on Response Surface Methodology. ANSN 2018, 9, 045014. [Google Scholar] [CrossRef]
- Chen, L.; Liu, J.; Guan, M.; Zhou, T.; Duan, X.; Xiang, Z. Growth Factor and Its Polymer Scaffold-Based Delivery System for Cartilage Tissue Engineering. Int. J. Nanomed. 2020, 15, 6097. [Google Scholar] [CrossRef]
- Asghar, W.; Islam, M.; Wadajkar, A.S.; Wan, Y.; Ilyas, A.; Nguyen, K.T.; Iqbal, S.M. Plga Micro-and Nanoparticles Loaded into Gelatin Scaffold for Controlled Drug Release. IEEE Trans. Nanotechnol. 2012, 11, 546–553. [Google Scholar] [CrossRef]
- Ali, A.F.; Ahmed, M.M.; El-Kady, A.M.; Abd El-Hady, B.M.; Ibrahim, A.M. Synthesis of Gelatin-Agarose Scaffold for Controlled Antibiotic Delivery and Its Modification by Glass Nanoparticles Addition as a Potential Osteomyelitis Treatment. Silicon 2020, 1–18. [Google Scholar] [CrossRef]
- Etxabide, A.; Long, J.; Guerrero, P.; de la Caba, K.; Seyfoddin, A. 3d Printed Lactose-Crosslinked Gelatin Scaffolds as a Drug Delivery System for Dexamethasone. Eur. Polym. J. 2019, 114, 90–97. [Google Scholar] [CrossRef]
- Boontheekul, T.; Mooney, D.J. Protein-Based Signaling Systems in Tissue Engineering. Curr. Opin. Biotechnol. 2003, 14, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.R.; Mooney, D.J. Polymeric Growth Factor Delivery Strategies for Tissue Engineering. Pharm. Res. 2003, 20, 1103–1112. [Google Scholar] [CrossRef] [Green Version]
- Gomes, D.M.B.; Rodrigues, G.; Martins, G.; Henriques, C.; Silva, J. Vitro Evaluation of Crosslinked Electrospun Fish Gelatin Scaffolds. Mater. Sci. Eng. C 2013, 33, 1219–1227. [Google Scholar] [CrossRef]
- Shankar, K.G.; Gostynska, N.; Montesi, M.; Panseri, S.; Sprio, S.; Kon, E.; Marcacci, M.; Tampieri, A.; Sandri, M. Investigation of Different Cross-Linking Approaches on 3d Gelatin Scaffolds for Tissue Engineering Application: A Comparative Analysis. Int. J. Biol. Macromol. 2017, 95, 1199–1209. [Google Scholar] [CrossRef] [PubMed]
- Etxabide, A.; Ribeiro, R.; Guerrero, P.; Ferreira, A.; Stafford, G.; Dalgarno, K.; de la Caba, K.; Gentile, P. Lactose-Crosslinked Fish Gelatin-Based Porous Scaffolds Embedded with Tetrahydrocurcumin for Cartilage Regeneration. Int. J. Biol. Macromol. 2018, 117, 199–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwak, H.W.; Woo, H.; Kimc, I.-C.; Lee, K.H. Fish gelatin nanofibers prevent drug crystallization and enable ultrafast delivery. RSC Adv. 2017, 7, 40411–40417. [Google Scholar] [CrossRef] [Green Version]
- Han, T.; Das, D.B. Permeability Enhancement for Transdermal Delivery of Large Molecule Using Low-Frequency Sonophoresis Combined with Microneedles. J. Pharm. Sci. 2013, 102, 3614–3622. [Google Scholar] [CrossRef] [Green Version]
- Chen, B.; Wei, J.; Tay, F.E.; Wong, Y.T.; Iliescu, C. Silicon Microneedle Array with Biodegradable Tips for Transdermal Drug Delivery. Microsyst. Technol. 2008, 14, 1015–1019. [Google Scholar] [CrossRef]
- Donnelly, R.F.; Majithiya, R.; Singh, T.R.R.; Morrow, D.I.; Garland, M.J.; Demir, Y.K.; Migalska, K.; Ryan, E.; Gillen, D.; Scott, C.J. Design, Optimization and Characterisation of Polymeric Microneedle Arrays Prepared by a Novel Laser-Based Micromoulding Technique. Pharm. Res. 2011, 28, 41–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nayak, A.; Das, D.B. Potential of Biodegradable Microneedles as a Transdermal Delivery Vehicle for Lidocaine. Biotechnol. Lett. 2013, 35, 1351–1363. [Google Scholar] [CrossRef] [Green Version]
- Kamal, N.A.M.; Mahmood, T.M.T.; Ahmad, I.; Ramli, S. Improving Rate of Gelatin/Carboxymethylcellulose Dissolving Microneedle for Transdermal Drug Delivery. Sains Malays. 2020, 49, 2269–2279. [Google Scholar] [CrossRef]
- Esposito, E.; Cortesi, R.; Nastruzzi, C. Gelatin Microspheres: Influence of Preparation Parameters and Thermal Treatment on Chemico-Physical and Biopharmaceutical Properties. Biomaterials 1996, 17, 2009–2020. [Google Scholar] [CrossRef]
- Okuda, M.; Ogawa, N.; Takeguchi, M.; Hashimoto, A.; Tagaya, M.; Chen, S.; Hanagata, N.; Ikoma, T. Minerals and Aligned Collagen Fibrils in Tilapia Fish Scales: Structural Analysis Using Dark-Field and Energy-Filtered Transmission Electron Microscopy and Electron Tomography. Microsc. Microanal. 2011, 17, 788–799. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Guillén, M.; Giménez, B.; López-Caballero, M.A.; Montero, M. Functional and Bioactive Properties of Collagen and Gelatin from Alternative Sources: A Review. Food Hydrocoll. 2011, 25, 1813–1827. [Google Scholar] [CrossRef] [Green Version]
- Olatunji, O.; Igwe, C.C.; Ahmed, A.S.; Alhassan, D.O.; Asieba, G.O.; Diganta, B.D. Microneedles from Fish Scale Biopolymer. J. Appl. Polym. Sci. 2014, 131. [Google Scholar] [CrossRef] [Green Version]
- Olatunji, O.; Olsson, R.T. Microneedles from Fishscale-Nanocellulose Blends Using Low Temperature Mechanical Press Method. Pharmaceutics 2015, 7, 363–378. [Google Scholar] [CrossRef] [Green Version]
- Fang, R.H.; Kroll, A.V.; Gao, W.; Zhang, L. Cell Membrane Coating Nanotechnology. Adv. Mater. 2018, 30, 1706759–1706792. [Google Scholar] [CrossRef]
- Kwak, H.W.; Shin, M.; Lee, J.Y.; Yun, H.; Song, D.W.; Yang, Y.; Shin, B.-S.; Park, Y.H.; Lee, K.H. Fabrication of an Ultrafine Fish Gelatin Nanofibrous Web from an Aqueous Solution by Electrospinning. Int. J. Biol. Macromol. 2017, 102, 1092–1103. [Google Scholar] [CrossRef] [PubMed]
- Ninan, G.; Joseph, J.; Aliyamveettil, Z.A. A Comparative Study on the Physical, Chemical and Functional Properties of Carp Skin and Mammalian Gelatins. J. Food Sci. Technol. 2014, 51, 2085–2091. [Google Scholar] [CrossRef] [Green Version]
- Prommajak, T.; Raviyan, P. Physical Properties of Gelatin Extracted from Skin of Thai Panga Fish (Pangasius Bocourti Sauvage). Food Biosci. 2013, 1, 131–145. [Google Scholar]
- Kouhdasht, A.M.; Moosavi-Nasab, M.; Aminlari, M. Gelatin Production Using Fish Wastes by Extracted Alkaline Protease from Bacillus Licheniformis. J. Food Sci. Technol. 2018, 55, 5175–5180. [Google Scholar] [CrossRef] [PubMed]
- Ren, T.; Gan, J.; Zhou, L.; Chen, H. Physically Crosslinked Hydrogels Based on Poly (Vinyl Alcohol) and Fish Gelatin for Wound Dressing Application: Fabrication and Characterization. Polymers 2020, 12, 1729. [Google Scholar] [CrossRef]
- Liu, J.; Tagami, T.; Ozeki, T. Fabrication of 3d-Printed Fish-Gelatin-Based Polymer Hydrogel Patches for Local Delivery of Pegylated Liposomal Doxorubicin. Mar. Drugs 2020, 18, 325. [Google Scholar] [CrossRef] [PubMed]
- Wonganu, B. Application of Gelatin Derived from Waste Tilapia Scales to an Antibiotic Hydrogel Pad. In E3S Web of Conferences; EDP Sciences: Pairs, France, 2020. [Google Scholar]
- Rattana, M.; Paradee, N.; Sirivat, A.; Niamlang, S. Porcine and Fish Gelatin Hydrogels for Controlled Release of Salicylic Acid and 5-sulfosalicylic Acid. Int. J. Drug Dev. Res. 2015, 7, 107–117. [Google Scholar]
- Neamtu, I.; Rusu, A.G.; Diaconu, A.; Nita, L.E.; Chiriac, A.P. Basic Concepts and Recent Advances in Nanogels as Carriers for Medical Applications. Drug Deliv. 2017, 24, 539–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ud Din, F.; Aman, W.; Ullah, I.; Qureshi, O.S.; Mustapha, O.; Shafique, S.; Zeb, A. Effective Use of Nanocarriers as Drug Delivery Systems for the Treatment of Selected Tumors. Int. J. Nanomed. 2017, 12, 7291–7309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foox, M.; Zilberman, M. Drug Delivery from Gelatin-Based Systems. Expert. Opin. Drug Deliv. 2015, 12, 1547–1563. [Google Scholar] [CrossRef]
- Kang, M.G.; Lee, M.Y.; Cha, J.M.; Lee, J.K.; Lee, S.C.; Kim, J.; Hwang, Y.-S.; Bae, H. Nanogels Derived from Fish Gelatin: Application to Drug Delivery System. Mar. Drugs 2019, 17, 246. [Google Scholar] [CrossRef] [Green Version]








| Fish Part | Enzymes | Isolated Peptides | IC50 | Reference |
|---|---|---|---|---|
| Alaska pollack skin | Alcalase, pronase E, and collagenase | LGP, GLP, PLG, LPG and PGL | 0.72, 1.62, 4.74, 5.73 and 13.93 mM | [31] |
| Nile tilapia skin | Bromelain, papain, trypsin, flavourzyme, alcalase and neutrase | Not determined | Antihypertensive activity: 89–93% | [32] |
| Salmon (skin, bone, and residual meat) | Corolase PP and Alcalase 2.4 L in combination with flavourzyme 500 L | FG-C1 * (4 peptides) (Pro-Pro, Gly-Phe, Gly-Pro-Val-Ala and Gly-Gly-Pro-Ala-Gly-Pro-Ala-Val) and 2 free amino acids (Arg and Tyr) | 0.13 and 0.28 mg/mL | [33] |
| Nile tilapia gelatin (commercially provided) | Alcalase | DPALATEPDPMPF | Antihypertensive activity: 52% | [34] |
| Tilapia skin gelatin | Simulated GI Digestion | VGLPNSR, QAGLSPVR | 80.90, 68.35 μM | [35] |
| Skate (O. kenojei) skin gelatin | Alcalase and alcalase/protease | LGPLGHQ, MVGSAPGVL | 4.22 and 3.09 μM | [36] |
| Sea cucumber (Acaudina molpadioidea) body wall | Bromelain and alcalase | Peptide of five main amino acids (Glu, Asp, Pro, Gly and Ala) | 0.0142 mg/ml | [37] |
| Jellyfish (Rhopilema esculentum) whole | Alcalase | UF3-B2 * was rich in Gly, Pro, Glu, Ala, and Asp | 0.043 mg/ml | [38] |
| Fish Part | Enzymes | Isolated Peptides | Assessment of Activity | Reference |
|---|---|---|---|---|
| Nile tilapia skin | Bromelain, papain, trypsin, flavourzyme, alcalase and neutrase | Not determined | ABTS, lipid peroxidation methods, FRAP, and ferrous ion chelating | [32] |
| Salmon (skin, bone, and residual meat) | Corolase PP and Alcalase 2.4 L in combination with flavourzyme 500 L | FG-C1 * (4 peptides (Pro-Pro, Gly-Phe, Gly-Pro-Val-Ala and Gly-Gly-Pro-Ala-Gly-Pro-Ala-Val) and 2 free amino acids (Arg and Tyr) | Corolase hydrolysates more potent (ORAC) activities than intact SG | [33] |
| Hoki skin | Trypsin, R-chymotrypsin, and pepsin | His-Gly-Pro-Leu-Gly-Pro-Leu | Linoleic acid peroxidation and the activity was closer to the highly active synthetic antioxidant butylated hydroxytoluene. | [45] |
| Amur sturgeon skin | Alcalase or flavourzyme | Oligopeptide; N.D. | Preventing lipid oxidation as evidenced by the lower TBARS formation | [46] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Nimry, S.; Dayah, A.A.; Hasan, I.; Daghmash, R. Cosmetic, Biomedical and Pharmaceutical Applications of Fish Gelatin/Hydrolysates. Mar. Drugs 2021, 19, 145. https://0-doi-org.brum.beds.ac.uk/10.3390/md19030145
Al-Nimry S, Dayah AA, Hasan I, Daghmash R. Cosmetic, Biomedical and Pharmaceutical Applications of Fish Gelatin/Hydrolysates. Marine Drugs. 2021; 19(3):145. https://0-doi-org.brum.beds.ac.uk/10.3390/md19030145
Chicago/Turabian StyleAl-Nimry, Suhair, Alaa Abu Dayah, Inas Hasan, and Rawand Daghmash. 2021. "Cosmetic, Biomedical and Pharmaceutical Applications of Fish Gelatin/Hydrolysates" Marine Drugs 19, no. 3: 145. https://0-doi-org.brum.beds.ac.uk/10.3390/md19030145