Socio Economic Status and Traumatic Brain Injury amongst Pediatric Populations: A Spatial Analysis in Greater Vancouver
Abstract
:1. Introduction
2. Methods
2.1. Data
2.2. Geographic Variables
2.3. Hotspot Identification
2.4. Statistical Analysis
3. Results
3.1. Descriptive Analysis
| Age Group | Girls | Boys | All | % Difference |
|---|---|---|---|---|
| 0–4 | 65 | 97 | 162 | 19.80 |
| 5–9 | 27 | 65 | 92 | 41.30 |
| 10–14 | 31 | 119 | 150 | 58.70 |
| 15–18 | 59 | 190 | 249 | 52.60 |
| 0–18 | 182 | 471 | 653 | 44.30 |
| Age Group (Years) | |||||
|---|---|---|---|---|---|
| Median ISS (IQR) | 0–4 | 5–9 | 10–14 | 15–18 | All |
| n = 162 | n = 92 | n = 151 | n = 248 | N = 653 | |
| Female | 17 (9.5) | 20 (13) | 26 (17) | 26 (15) | 25 (13) |
| Male | 17 (9) | 25 (16.5) | 25 (13) | 26 (16 | 25 (12) |
| Injury Mechanism, n (%) | |||||
| Assault | 15 (9%) | 0 (0%) | 4 (3%) | 48 (19%) | 67 (10%) |
| Fall | 101 (62%) | 28 (30%) | 23 (15%) | 18 (7%) | 170 (26%) |
| MVC | 27 (17%) | 57 (62%) | 107 (71%) | 160 (65%) | 351 (54%) |
| Other | 19 (12%) | 7 (8%) | 17 (11%) | 22 (9%) | 65 (10%) |
| Motivation, n (%) | |||||
| Intentional | 12 (7%) | 1 (1%) | 9 (6%) | 57 (23%) | 79 (12%) |
| Unintentional | 141 (87%) | 91 (99%) | 139 (92%) | 187 (75%) | 558 (85%) |
| Unknown | 9 (6%) | 0 (0%) | 3 (2%) | 4 (2%) | 16 (3%) |
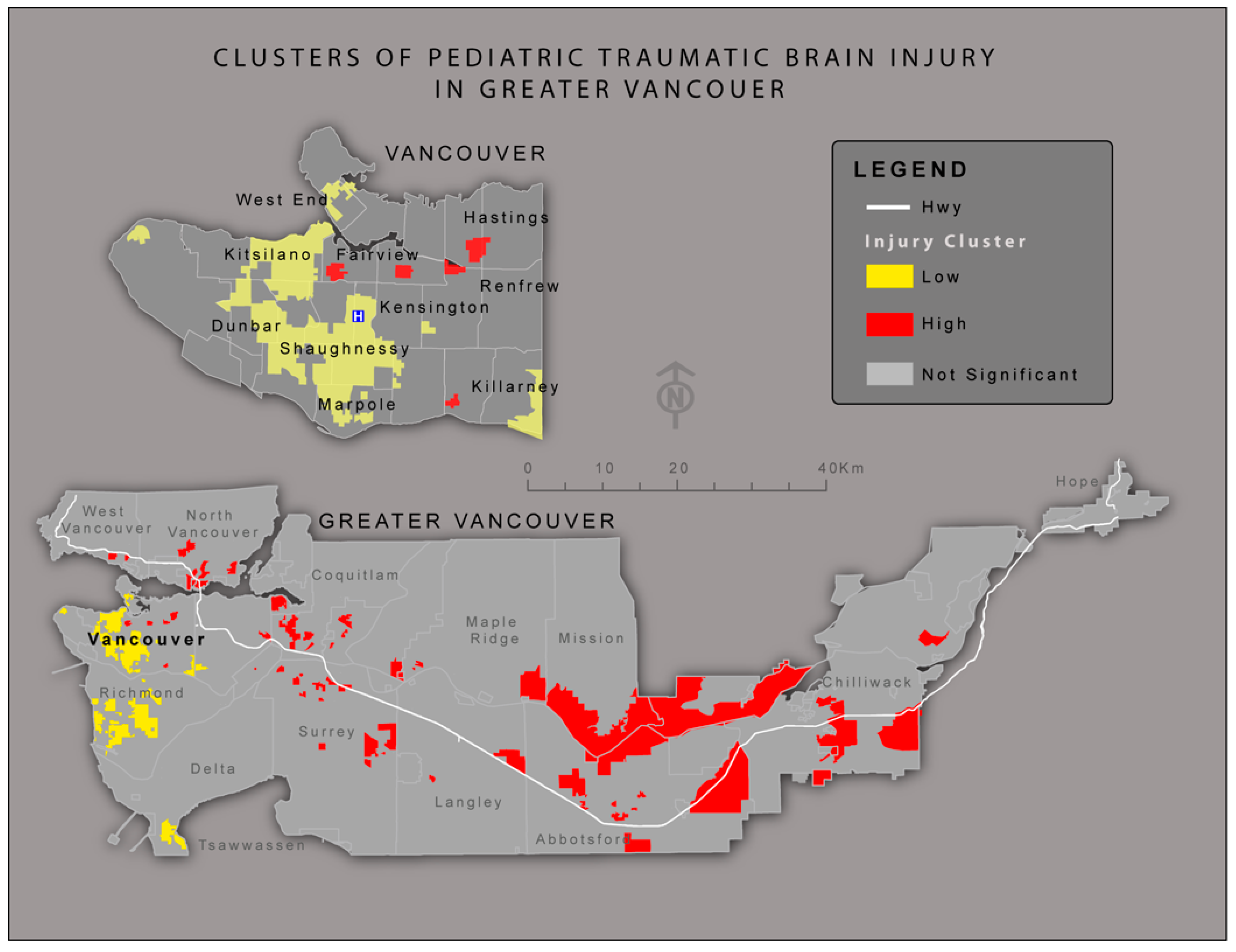
3.2. Hotspot Analysis
3.3. Statistical Analysis
3.3.1. Individual Census Variables
| Name | Description | OR | Group | Pass Criteria for Final Model |
|---|---|---|---|---|
| (95%CI) | ||||
| p-Value | ||||
| PercAboriginal | Percentage of Aboriginal | 1.002 | Cultural | Yes |
| 1.003–1.02 | ||||
| 0.02 | ||||
| PercLonFamily | Percentage of Lone Families | 1.002 | Demographic | No |
| 0.994–1.011 | ||||
| 0.6 | ||||
| PercNoHSchl | Percentage of age 15 and older with no high school certificate | 1.013 | Education | Yes |
| 1.005–1.021 | ||||
| 0.001 | ||||
| AllRdBfr | Sum of length of roads within 1000 m | 0.999 | Environmental | Yes |
| 0.998–1.000 | ||||
| 0.003 | ||||
| PercNoDetHous | Percentage of no Detached Housing | 0.999 | Housing | No |
| 0.996–1.001 | ||||
| 0.35 | ||||
| AvgInc | Average income | 1 | Income | Yes |
| 1.001–1.002 | ||||
| 0.176 | ||||
| MedInc | Median Income | 1 | Income | No |
| 1.001–1.002 | ||||
| 0.41 | ||||
| UnEmpRate | Unemployment rate | 0.796 | Occupation | No |
| 0.93–1.02 | ||||
| 0.88 | ||||
| Within30min | Within 30 min of BC Children Hospital | 0.796 | Rural/Suburban | Yes |
| 0.674–0.941 | ||||
| 0.01 | ||||
| VANDIX | Composite SES Index | 1.089 | Composite SES Index | Yes |
| 1.031–1.151 | ||||
| 0.002 |
| Predictor Variable | Models | |
|---|---|---|
| Census Variables | VANDIX | |
| OR (95%CI) p-Value | OR (95%CI) p-Value | |
| (n = x) | (n = x) | |
| No high school | 1.13 | - |
| (1.03–1.23) | ||
| 0.009 | ||
| Outside of 30 min (drive time) | 1.22 | 1.25 |
| (1.01–1.48) | (1.04–1.51) | |
| 0.039 | 0.020) | |
| VANDIX | - | 1.08 |
| (1.02–1.15) | ||
| 0.01 | ||

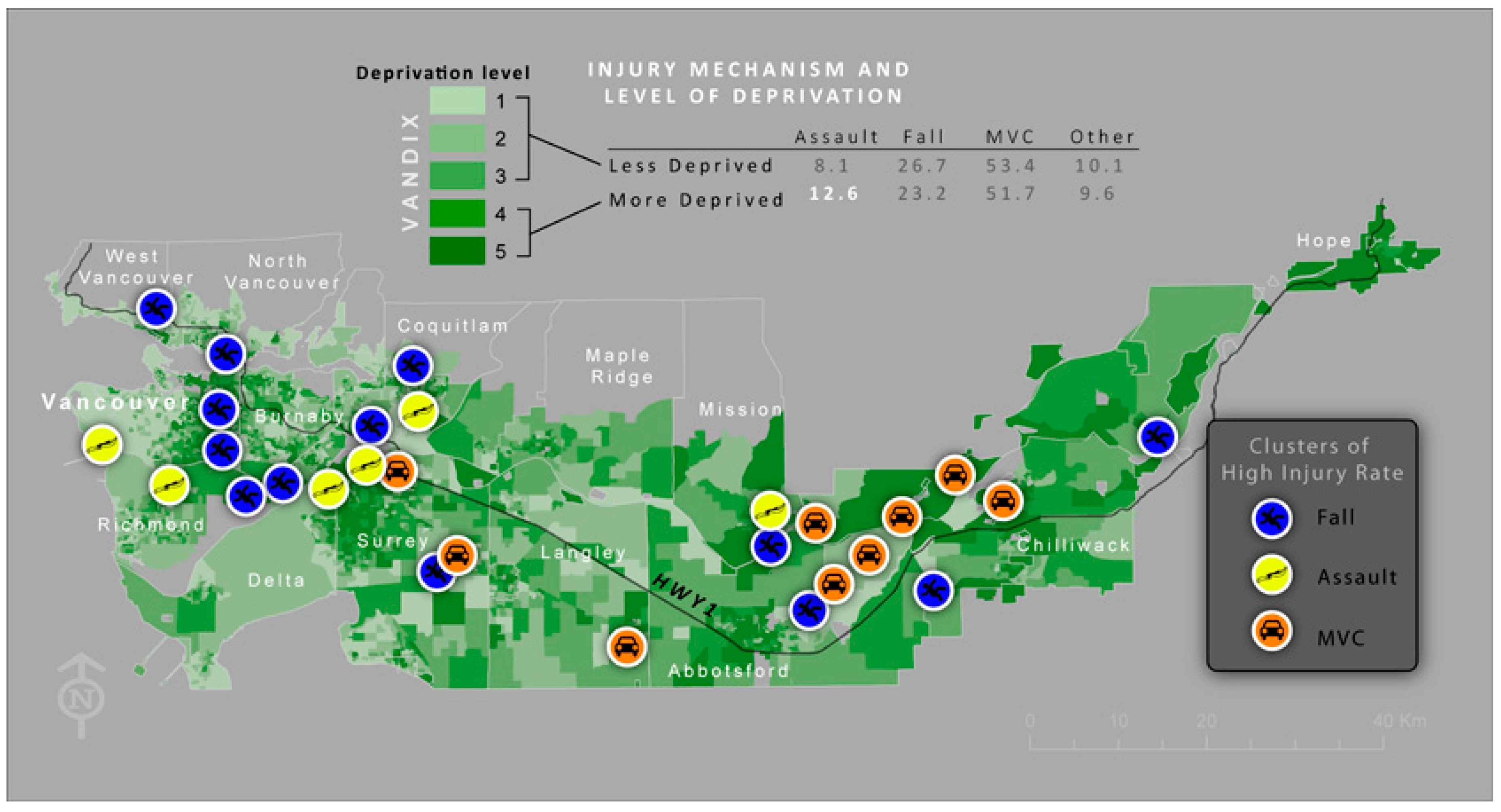
3.3.2. Composite SES Model
3.3.3. Injury Mechanism and SES
4. Discussion
5. Study Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Birken, C.S.; Parkin, P.C.; To, T.; Macarthur, C. Trends in rates of death from unintentional injury among Canadian children in urban areas: Influence of socioeconomic status. Can. Med. Assoc. J. 2006, 175, 867–867. [Google Scholar] [CrossRef] [PubMed]
- Birken, C.S.; MacArthur, C. Socioeconomic status and injury risk in children. Paediatr. Child Health 2004, 9, 323–325. [Google Scholar] [PubMed]
- Faelker, T.; Pickett, W.; Brison, R.J. Socioeconomic differences in childhood injury: A population based epidemiologic study in Ontario, Canada. Injury Prev. 2000, 6, 203–208. [Google Scholar] [CrossRef]
- Simpson, K.; Janssen, I.; Craig, W.M.; Pickett, W. Multilevel analysis of associations between socioeconomic status and injury among Canadian adolescents. J. Epidemiol. Commun. Health 2005, 59, 1072–1077. [Google Scholar] [CrossRef] [PubMed]
- Potter, B.; Speechley, K.; Koval, J. Socioeconomic status and non-fatal injuries among Canadian adolescents: Variations across SES and injury measures. BMC Public Health 2005, 5. [Google Scholar] [CrossRef] [PubMed]
- Davison, C.; Russel, K.; Piedt, S.; Pike, I.; Pickett, W. Injury among Young Canadians: A National Study of Contextual Determinants. Available online: http://www.jcsh-cces.ca (accessed on 10 April 2015).
- Vandivere, S.; Hair, E.C.; Theokas, C.; Cleveland, K.; McNamara, M.; Atienza, A. How Housing Affects Child Well-Being; Funders’ Network for Smart Growth and Livable Communities: Coral Gables, FL, USA, 2006. [Google Scholar]
- Cubbin, C.; Smith, G.S. Socioeconomic inequalities injury: Critical issues in design and analysis. Ann. Rev. Public Health 2002, 23, 349–375. [Google Scholar] [CrossRef] [PubMed]
- Keenan, H.T.; Bratton, S.L. Epidemiology and outcomes of pediatric traumatic brain injury. Dev. Neurosci. 2006, 28, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Selassie, A.W.; Zaloshnja, E.; Langlois, J.A.; Miller, T.; Jones, P.; Steiner, C. Incidence of long-term disability following traumatic brain injury hospitalization, United States, 2003. J. Head Trauma Rehab. 2008, 23, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Griesdale, D.E.; Örtenwall, V.; Norena, M.; Wong, H.; Sekhon, M.S.; Kolmodin, L.; Henderson, W.R.; Dodek, P. Adherence to guidelines for management of cerebral perfusion pressure and outcome in patients who have severe traumatic brain injury. J. Crit. Care 2015, 30, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Hawley, C.A.; Ward, A.B.; Magnay, A.R.; Long, J. Parental stress and burden following traumatic brain injury amongst children and adolescents. Brain Injury 2003, 17, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Yeates, K.O.; Swift, E.; Taylor, H.G.; Wade, S.; Drotar, D.; Stancin, T.; Minich, N. Short- and long-term social outcomes following pediatric traumatic brain injury. J. Int. Neuropsychol. Soc. 2004, 10, 412–426. [Google Scholar] [CrossRef] [PubMed]
- Spatial, D. GeoPinPoint; DMTI Spatial Inc.: Markham, ON, Canada, 2011. [Google Scholar]
- Statistics Canada. Dissemination Area. Secondary Dissemination Area 2011. Available online: https://www12.statcan.gc.ca/census-recensement/2011/ref/dict/geo021-eng.cfm (accessed on 15 February 2015).
- Bell, N.; Arrington, A.; Adams, S.A. Census-based socioeconomic indicators for monitoring injury causes in the USA: A review. Inj. Prev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Schuurman, N.; Bell, N.; Dunn, J.; Oliver, L. Deprivation indices, population health and geography: An evaluation of the spatial effectiveness of indices at multiple scales. J. Urban Health 2007, 84, 591–603. [Google Scholar] [CrossRef] [PubMed]
- ArcGIS [Program]. 10.1 Version; ESRI: Redlands, CA, USA, 2013.
- Spatial, D. Route Logistic; DMTI: Markham, ON, Canada, 2011. [Google Scholar]
- Kafadar, K. Smoothing geographical data, particularly rates of disease. Stat. Med. 1996, 15, 2539–2560. [Google Scholar] [CrossRef]
- Anselin, L.; Syabri, I.; Kho, Y. GeoDa: An Introduction to spatial data analysis. Geogr. Anal. 2006, 38, 5–22. [Google Scholar] [CrossRef]
- SPSS [Program]. 19 Version; IBM: Armonk, NY, USA, 2013.
- Gardner, W.; Mulvey, E.P.; Shaw, E.C. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol. Bull. 1995, 118, 392–404. [Google Scholar] [CrossRef] [PubMed]
- Oliver, L.N.; Kohen, D.E. Unintentional Injury Hospitalizations among Children and Youth in Areas with a High Percentage of Aboriginal Identity Residents: 2001/2002 to 2005/2006. Statistics Canada. 2012. Available online: http://www.statcan.gc.ca/pub/82-003-x/2012003/article/11699-eng.htm (accessed on 3 May 2014).
- Harrop, A.R.; Brant, R.F.; Ghali, W.A.; Macarthur, C. Injury mortality rates in native and non-native children: A population-based study. Public Health Rep. 2007, 122, 339–346. [Google Scholar] [PubMed]
- Pike, I.; McDonald, R.J.; Piedt, S.; Macpherson, A.K. Developing injury indicators for First Nations and Inuit children and youth in Canada: A modified Delphi approach. Chronic Dis. Inj. Can. 2014, 34, 203–209. [Google Scholar] [PubMed]
- Tennant, A. Admission to hospital following head injury in England: Incidence and socio-economic associations. BMC Public Health 2005, 5, 21–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yates, P.J.; Williams, W.H.; Harris, A.; Round, A.; Jenkins, R. An epidemiological study of head injuries in a UK population attending an emergency department. J. Neurol. Neurosurg. Psychiatry 2006, 77, 699–701. [Google Scholar] [CrossRef] [PubMed]
- Karkhaneh, M.; Kalenga, J.-C.; Hagel, B.E.; Rowe, B.H. Effectiveness of bicycle helmet legislation to increase helmet use: A systematic review. Inj. Prev. 2006, 12, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Pike, I.; Desapriya, E.; Turcotte, M.K. Review of International Best-Practices for Improving Child Passenger Safety and Evaluation of Saskatchewan’s Program. BC Injury Research and Prevention Unit (BCIRPU) 2012. Available online: http://www.abipartnership.sk.ca/images/file/Sask%20CPS%20Sys%20Rev%20%26%20Eval.pdf (accessed on 15 March 2014).
- Muscara, F.; Catroppa, C.; Eren, S.; Anderson, V. The impact of injury severity on long-term social outcome following paediatric traumatic brain injury. Neuropsychol. Rehabil. 2009, 19, 541–561. [Google Scholar] [CrossRef] [PubMed]
- Boyle, J.M.; Lampkin, C.; Schulman, Ronca and Bucuvalas, Inc. Motor Vehicle Occupant Safety Survey: Crash Injury and Emergency Medical Services Report. US Department of Transportation, NHTSA, 2007. Available online: http://www.ems.gov/pdf/810977.pdf (accessed on 11 January 2014).
- Palmer, C.D.; Jones, K.H.; Jones, P.A.; Polacarz, S.V.; Evans, G.W.L. Urban legend versus rural reality: Patients’ experience of attendance at accident and emergency departments in west Wales. Emerg. Med. J. 2005, 22, 165–170. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amram, O.; Schuurman, N.; Pike, I.; Yanchar, N.L.; Friger, M.; McBeth, P.B.; Griesdale, D. Socio Economic Status and Traumatic Brain Injury amongst Pediatric Populations: A Spatial Analysis in Greater Vancouver. Int. J. Environ. Res. Public Health 2015, 12, 15594-15604. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph121215009
Amram O, Schuurman N, Pike I, Yanchar NL, Friger M, McBeth PB, Griesdale D. Socio Economic Status and Traumatic Brain Injury amongst Pediatric Populations: A Spatial Analysis in Greater Vancouver. International Journal of Environmental Research and Public Health. 2015; 12(12):15594-15604. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph121215009
Chicago/Turabian StyleAmram, Ofer, Nadine Schuurman, Ian Pike, Natalie L Yanchar, Michael Friger, Paul B. McBeth, and Donald Griesdale. 2015. "Socio Economic Status and Traumatic Brain Injury amongst Pediatric Populations: A Spatial Analysis in Greater Vancouver" International Journal of Environmental Research and Public Health 12, no. 12: 15594-15604. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph121215009







