Association between Ambient Air Pollution and Emergency Room Visits for Respiratory Diseases in Spring Dust Storm Season in Lanzhou, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Methods
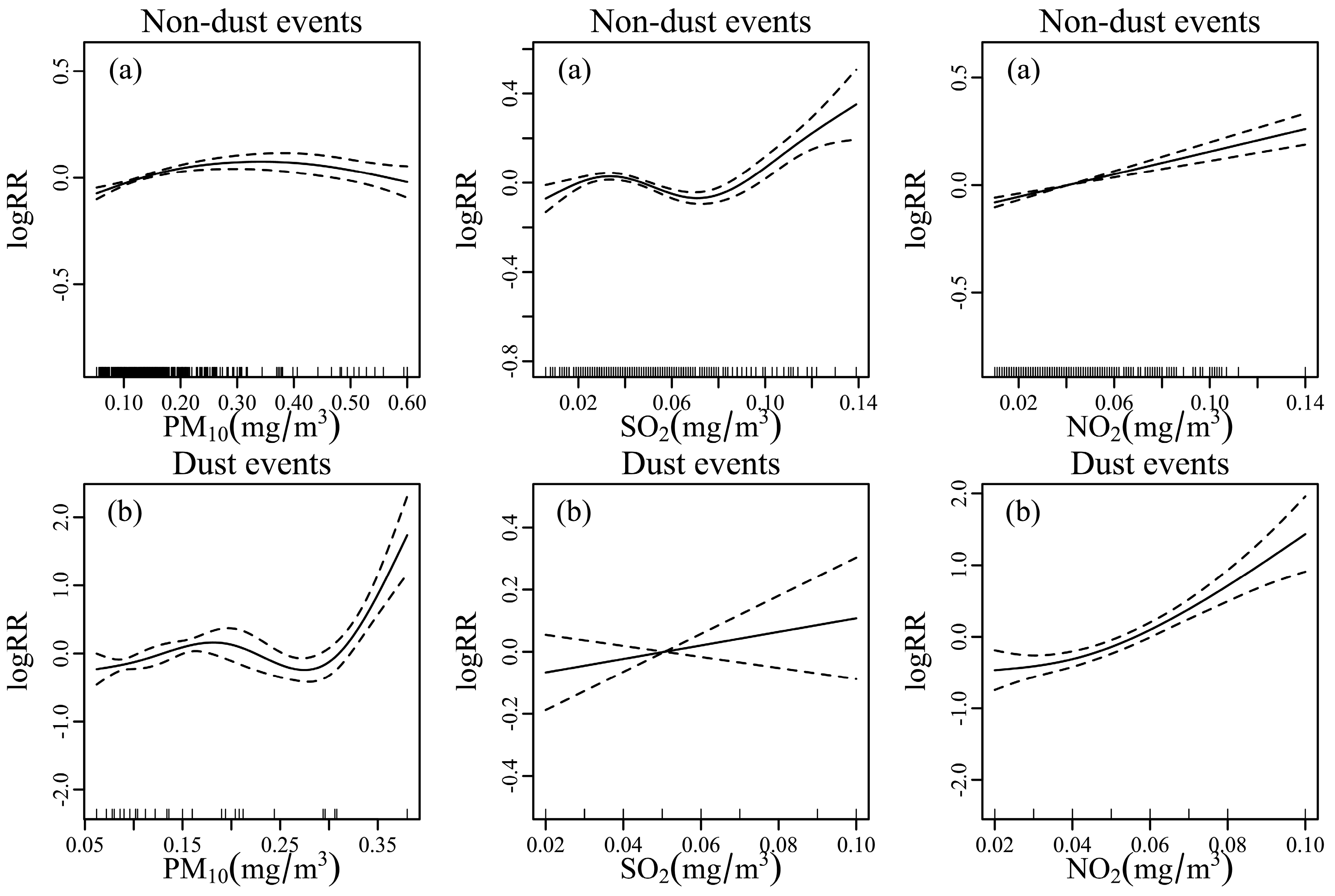
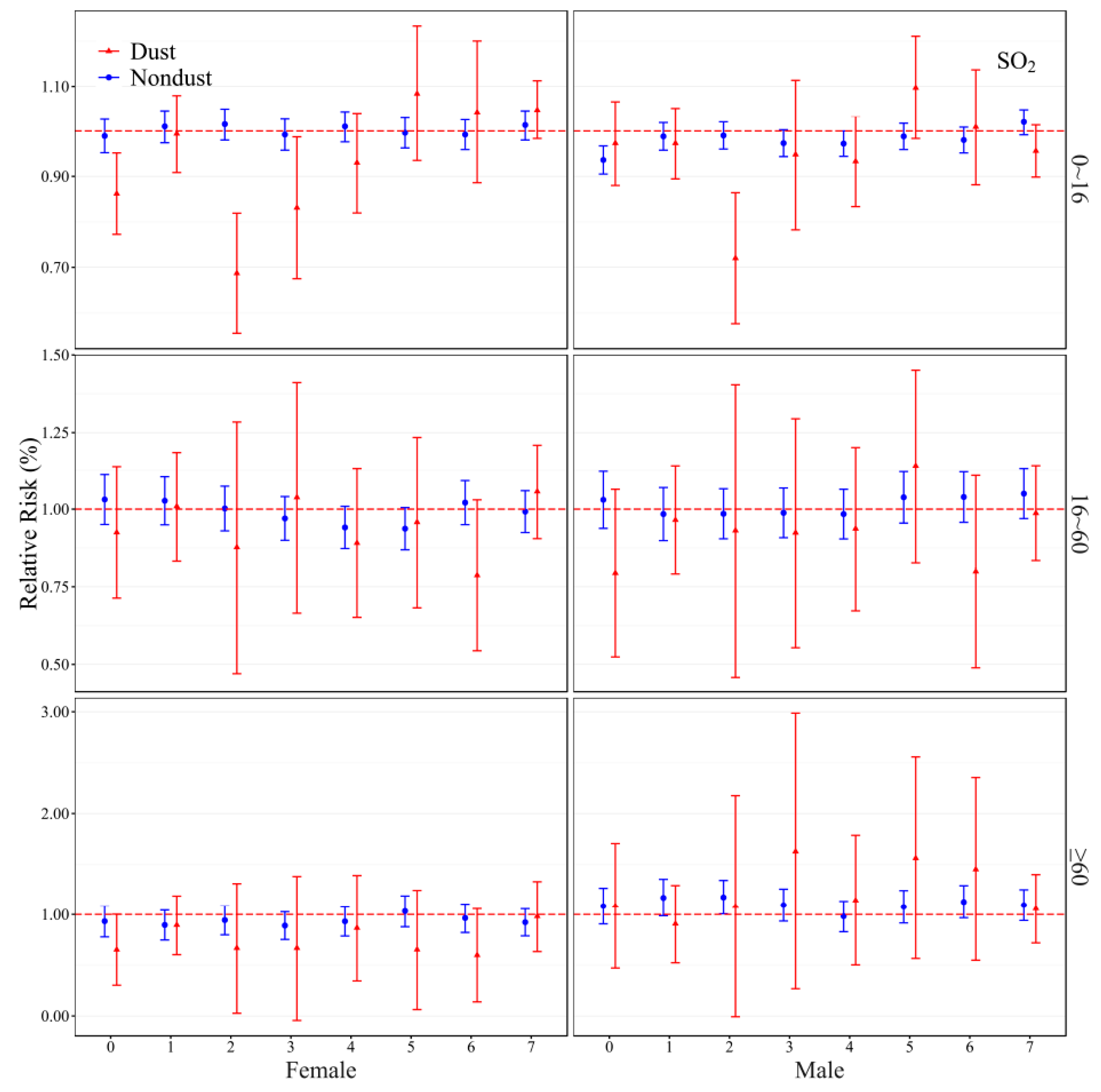
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO. Fact Sheet on Outdoor Air Pollution (N°133): Ambient Air Quality and Health, Updated March 2014. Available online: http://www.who.int/mediacentre/factssheets/fs313/en/ (accessed on 1 March 2014).
- Kan, H.D.; Chen, B.H.; Hong, C.J. Health impact of outdoor air pollution in China: Current knowledge and future research needs. Environ. Health Perspect. 2009, 117. [Google Scholar] [CrossRef] [PubMed]
- Rowshan, G.R.; Khosh, A.F.; Negahban, S.; Mirkatouly, J. Impact of air pollution on climate fluctuations in Tehran city. Environ. Sci. 2009, 7, 173–191. [Google Scholar]
- Curriero, F.C.; Heiner, K.S.; Samet, J.M.; Zeger, S.L.; Lisa, S. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 2002, 155, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Haines, A.; McMichael, A.J.; Epstein, P.R. Environment and health: 2. Global climate change and health. Can. Med. Assoc. J. 2000, 163, 729–734. [Google Scholar]
- Chen, R.; Chu, C.; Tan, J.; Cao, J.; Song, W.; Xu, X. Ambient air pollution and hospital admission in Shanghai, China. J. Hazard. Mater. 2010, 181, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Fung, K.Y.; Luginaah, I.; Gorey, K.M.; Webser, G. Air pollution and daily hospitalization rates for cardiovascular and respiratory disease in London, Ontario. Int. J. Environ. Stud. 2005, 1, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Zemp, E.; Elsasser, S.; Schindler, C.; Kunzli, N.; Perruchoud, A.P.; Domenighetti, G.; Medici, T.; Ackermann-Liebrich, U.; Leuenberger, P.; Monn, C. Long-term ambient air pollution and respiratory symptoms in adults (SAPALDIA study). Am. J. Respir. Crit. Care Med. 1999, 159, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- Andersen, Z.J.; Loft, S.; Ketzel, M.; Stage, M.; Scheike, T.; Hermansen, M.N. Ambient air pollution triggers wheezing symptoms in infants. Thorax 2008, 63, 710–716. [Google Scholar] [CrossRef] [PubMed]
- Samoli, E.; Analitis, A.; Touloumi, G. Estimating the exposure-response relationships between particulate matter and mortality within the Aphea multicity project. Envion. Health Perspect. 2005, 113, 88–95. [Google Scholar] [CrossRef]
- Roberts, S.; Martin, M.A. Applying a moving total mortality count to the cities in the NMMAPS database to estimate the mortality effects of particulate matter air pollution. Occup. Environ. Med. 2006, 63, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J. Harvesting and long term exposure effects in the relation between air pollution and mortality. Am. J. Epidemiol. 2000, 151, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; McDermott, A.M.; Zeger, S.L.; Samet, J.M. Revised analyses of the national morbidity, mortality, and air pollution study: Mortality among residents of 90 cities. J. Toxicol. Environ. Health Part A 2005, 68, 1071–1092. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.M.; Vichit-Vadakan, N.; Kan, H.; Qian, Z. Public health and air pollution in Asia (PAPA): A multicity study of short-term effects of air pollution on mortality. Environ. Health Perspect. 2008, 116, 1195–1202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, Y.; Jia, Y.; Pan, X.; Liu, L.; Wichmann, H.E. The association between fine particulate air pollution and hospital emergency room visits for cardiovascular diseases in Beijing, China. Sci. Total Environ. 2009, 407, 4826–4830. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, S.G.; Ma, Y.X.; Shang, K.Z.; Cheng, Y.F.; Li, X.; Ning, G.C.; Zhao, W.J.; Li, N.R. Association between ambient air pollution and hospital emergency admissions for respiratory and cardiovascular diseases in Beijing: A time series study. Biomed. Environ. Sci. 2015, 28, 352–363. [Google Scholar] [PubMed]
- Zhang, F.Y.; Li, L.P.; Hhomas, K. Study on the association between ambient air pollution and daily cardiovascular and respiratory mortality in an urban district of Beijing. Sci. Total Environ. 2011, 8, 2109–2123. [Google Scholar] [CrossRef] [PubMed]
- Kan, H.D.; London, S.J.; Chen, G.H.; Zhang, Y.H.; Song, G.X. Season, sex age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: The Public Health and Air Pollution in Asia (PAPH) study. Environ. Health Perspect. 2008, 116, 1183–1188. [Google Scholar] [CrossRef] [PubMed]
- Yu, I.T.S.; Zhang, Y.H.; Tam, W.W.S.; Yan, Q.H.; Xu, Y.J. Effect of ambient air pollution on daily mortality rates in Guangzhou, China. Atmos. Environ. 2011, 46, 528–535. [Google Scholar] [CrossRef]
- Wang, T.W.; Lau, T.S.; Yu, T.S.; Neller, A.; Wong, S.L.; Tam, W.; Pang, S.W. Air pollution and hospital admissions for respiratory and cardiovascular diseases in Hong Kong. Occup. Environ. Med. 1999, 56, 679–683. [Google Scholar]
- Meng, Z.Q.; Lu, B.; Pan, J.J. Relationship between dust weather and the cases of respiratory diseases. J. Public Health 2007, 23, 284–286. [Google Scholar]
- Ye, X.F. Effect of dust particles on children’s maximum expiratory flow rates. J. Environ. Health 2008, 25, 571–574. [Google Scholar]
- Chen, X.Y. Effect of dust storms on the respiratory diseases. J. Environ. Health 2007, 24, 63–65. [Google Scholar]
- Huang, Y.X.; Wang, B.J. Analysis on the relationship between dust events and respiratory diseases. Gansu Meteorol. 2001, 19, 41–44. [Google Scholar]
- Wang, S.G.; Yang, M.; Qi, B. Effect of dust storm in Gansu Hexi area on air pollution in Lanzhou city. J. Desert Res. 1999, 19, 154–158. [Google Scholar]
- Ta, W.Q.; Wang, T.; Xiao, H.L.; Zhu, X.Y.; Xiao, Z. Gaseous and particulate air pollution in the Lanzhou Valley, China. Sci. Total Environ. 2004, 320, 163–176. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.D.; Tian, L.; Zhang, X.Y. Effect of dust events in area on low stream atmospheric PM10. J. Environ. Sci. 2004, 24, 528–532. [Google Scholar]
- Samet, J.M.; Dominici, F.; Zeger, S.L. The National Morbidity, Mortality, and Air Pollution Study. Part I: Methods and Methodologic Issues; Research Report; Health Effects Institute: Cambridge, MA, USA, 2000; 94 Part 1; pp. 5–91. [Google Scholar]
- Wang, S.G.; Wang, J.Y.; Zhou, Z.J.; Shang, K.Z. Regional characteristics of three kinds of dust storm events in China. Atmos. Environ. 2005, 39, 509–520. [Google Scholar] [CrossRef]
- Cao, J.; Li, W.; Tan, J. Association of ambient air pollution with hospital outpatient and emergency room visits in Shanghai, China. Sci. Total Environ. 2009, 407, 5531–5536. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Barnett, A.G.; Yu, W. A large change in temperature between neighboring days increases the risk of mortality. PLoS ONE 2011, 6, e16511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qiu, H.; Yu, I.T.; Wang, X.; Tian, L.; Tse, L.A.; Wong, T.W. Season and humidity dependence of the effects of air pollution on COPD hospitalizations in Hong Kong. Atmos. Environ. 2013, 76, 74–80. [Google Scholar] [CrossRef]
- R Version 3.1.3. Available online: http://cran.r-project.org/bin/windows/base/ (accessed on 9 March 2015).
- Zeka, A.; Zanobetti, A.; Schwartz, J. Individual-level modifiers if the effects of particulate matter on matter on daily mortality. Am. J. Epidemiol. 2006, 163, 849–859. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Ebisu, K.; Peng, R.D. Seasonal and regional short-term effects of fine particles on hospital admissions in 202 U.S. counties, 1999–2005. Am. J. Epidemiol. 2008, 168, 1301–1310. [Google Scholar] [CrossRef] [PubMed]
- Tao, Y.; Mi, S.Q.; Zhou, S.H.; Wang, S.G.; Xie, X.Y. Air pollution and hospital admissions for respiratory diseases in Lanzhou, China. Environ. Pollut. 2014, 185, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Wang, M.Z.; Wang, S.G.; Tao, Y.; Shang, K.Z. Short-term effects of gaseous pollutants and particulate matter on daily hospital admissions for cardio-cerebrovascular disease in Lanzhou: Evidence from a heavily polluted city in China. Int. J. Environ. Res. Public Health 2013, 10, 462–477. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z. Effect evaluation on smoking control plan for one year in Beijing, China, WHO smoking control capability construction cooperation items. Chin. J. Health Educ. 2005, 21, 412–416. [Google Scholar]
- Künzli, N.; Jerrett, M.; Mack, W.J. Ambient air pollution and atherosclerosis in Los Angeles. Environ. Health Perspect. 2005, 113, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.G.; Feng, X.Y.; Zeng, X.Q.; Ma, Y.X.; Shang, K.Z. A study on variation of concentrations of particulate matter with different sizes in Lanzhou, China. Atmos. Sci. 2009, 43, 2823–2828. [Google Scholar] [CrossRef]
- Reyes, M.; Diaz, J.; Tobias, A. Impact of Saharan dust particles on hospital admissions in Madrid (Spain). Int. J. Environ. Health Res. 2014, 24, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Mallone, S.; Staffogia, M.; Faustini, A. Saharan dust and associations between particulate matter and daily mortality in Rome, Italy. Environ. Health Perspect. 2011, 119, 1409–1414. [Google Scholar] [CrossRef] [PubMed]
- Kanatani, K.T. Desert dust exposure is associated with increased risks of asthma hospitalization in children. Am. J. Respir. Crit. Care Med. 2010, 182, 1475–1481. [Google Scholar] [CrossRef] [PubMed]
- Chien, L.C.; Yang, C.H.; Yu, H.L. Estimated effects of Asian Dust Storms on spatiotemporal distributions of clinic visits for respiratory diseases in Taipei children (Taiwan). Environ. Health Perspect. 2012, 120, 1215–1220. [Google Scholar] [CrossRef] [PubMed]
- Ghio, A.J.; Delvin, R.B. Inflammatory lung injury after bronchial instillation of air pollution particles. Am. J. Respir. Crit. Care Med. 2001, 164, 704–708. [Google Scholar] [CrossRef] [PubMed]
- Nagar, J.K.; Akolkar, A.B.; Kumar, R. A review on airborne particulate matter and its sources, chemical composition and impact on human respiratory system. Int. J. Environ. Sci. 2014, 5, 447–463. [Google Scholar]
- Wang, M.Z.; Zheng, S.; Wang, S.G. The weather temperature and air pollution interaction and its effect on hospital admissions due to respiratory system diseases in western China. Biomed. Environ. Sci. 2013, 26, 403–407. [Google Scholar] [PubMed]
- Cao, J.; Yang, C.X.; Li, J.X. Association between long-term exposure to outdoor air pollution and mortality in China: A cohort study. J. Hazard. Mater. 2011, 186, 1594–1600. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A.; Dochery, D.W. Health effects of fine particulate air pollution: Lines that connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef] [PubMed]
- Chiusolo, M.; Cadum, E.; Stafoggia, M.; Galassi, C.; Berti, G.; Faustini, A. Short term effects of nitrogen dioxide on mortality and susceptibility factors in ten Italian cities: The EpiAir study. Environ. Health Perspect. 2011. [Google Scholar] [CrossRef] [PubMed]
- Simoli, E.; Aga, E.; Touloumi, G. Short-term effects of nitrogen dioxide on mortality: An analysis within the APHEA project. Eur. Respir. J. 2006, 27, 1129–1138. [Google Scholar] [CrossRef] [PubMed]
- Burnett, R.T.; Stieb, D.; Brook, J.R. Association between short-term changes in nitrogen dioxide and mortality in Canadian cities. Arch. Environ. Health 2004, 59, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.J.; Pan, G.W.; Kan, H.D. Ambient air pollution and daily mortality in Anshan, China: A time-stratified case-crossover analysis. Sci. Total Environ. 2010, 408, 6086–6091. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Sioutas, C.; Cho, A.; Schmitz, D.; Misra, C.; Sempf, J. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ. Health Perspect. 2003, 111, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Rahman, I.; Morrison, D.; Donaldson, K.; MacNee, W. Systemic oxidative stress in asthma, COPD, and smokers. J. Respir. Crit. Care Med. 1996, 154, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- Hao, H.; Chang, H.H.; Holmes, H.A.; Mulholland, J.A.; Klein, M.; Darrow, L.A.; Strickland, M.J. Air pollution and preterm birth in the U.S. State of Georgia (2002–2006): Associations with concentrations of 11 Ambent air pollutants estimated by combining Community Multiscale Air Quality Model (CMAQ) simulations with stationary monitor measurements. Environ. Health Perspect. 2016, 124, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.T.; Tam, W.S.; Yu, T.S.; Wong, A.H.S. Association between daily mortalities from respiratory and cardiovascular diseases and air pollution in Hong Kong, China. Occup. Environ. Med. 2002, 59, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.J.; Zhao, A.; Chen, R.J.; Kan, H.D.; Kuang, X.Y. Association between ambient air pollution and outpatient visits for acute brochitis in a Chinese city. Biomed. Environ. Sci. 2014, 27, 833–840. [Google Scholar] [PubMed]
- Park, S.; Askary, H.E.; Sabbah, I.; Kwak, H.; Prasad, A.K.; Lee, W.K.; Kafatos, M. Studying air pollutants origin and associated meteorological parameters over Seoul from 2000 to 2009. Adv. Meteorol. 2015. [Google Scholar] [CrossRef]
- Wang, S.G.; Yang, D.B.; Shang, K.Z.; Huang, J.G.; Wang, C.X. The characteristics of wind and its influence on the air pollution in the atmospheric boundary layer of the urban districts of Lanzhou in cold half year. J. Lanzhou Univ. 1997, 33, 97–105. [Google Scholar]
- Zhang, L.; Chen, C.; Murlis, J. Study on winter air pollution control in Lanzhou, China. Water Air Pollut. 2000, 127, 351–372. [Google Scholar] [CrossRef]
- Sheppard, L.; Slaughter, J.C.; Schildcrout, J.; Liu, L.J.; Lumley, T. Exporsure and measurement contributions to estimates of acute air pollution effects. J. Expo. Anal. Environ. Epidemiol. 2005, 15, 366–376. [Google Scholar] [CrossRef] [PubMed]
- Wilson, W.E.; Mar, T.F.; Koenig, J.Q. Influence of exposure error and effect modification by socioeconomic status on the association of acute cardiovascular mortality with particulate matter in Phoenix. J. Expo. Sci. Environ. Epidemiol. 2007, 17, S11–S19. [Google Scholar] [CrossRef] [PubMed]


| Daily Data | Mean | SD | Min | P25 | Median | P75 | Max |
|---|---|---|---|---|---|---|---|
| Metrologic measures | |||||||
| Temperature (°C) | 12.9 | 6.2 | −5.1 | 8.3 | 13.6 | 17.9 | 24.8 |
| Relative humidity (%) | 26.8 | 14.8 | 4.0 | 15.3 | 23.0 | 33.0 | 87.0 |
| Air pollutants concentrations | |||||||
| PM10 (µg/m3) | 159.2 | 103.0 | 52.0 | 94.0 | 134.0 | 183.0 | 600.0 |
| SO2 (µg/m3) | 45.0 | 22.0 | 10.0 | 30.0 | 40.0 | 60.0 | 140.0 |
| NO2 (µg/m3) | 42.7 | 22.0 | 10.0 | 30.0 | 50.0 | 50.0 | 140.0 |
| Dust days | |||||||
| PM10 (µg/m3) | 324.0 | 178.0 | 86.0 | 175.0 | 268.0 | 491.0 | 600.0 |
| SO2 (µg/m3) | 54.0 | 22.0 | 14.0 | 43.0 | 51.0 | 61.0 | 122.0 |
| NO2 (µg/m3) | 46.0 | 16.0 | 10.0 | 37.0 | 44.0 | 59.0 | 78.0 |
| Non-dust days | |||||||
| PM10 (µg/m3) | 146.0 | 83.0 | 52.0 | 92.0 | 130.0 | 168.0 | 600.0 |
| SO2 (µg/m3) | 43.0 | 22.0 | 6.0 | 28.0 | 39.0 | 55.0 | 139.0 |
| NO2 (µg/m3) | 41.0 | 22.0 | 11.0 | 25.0 | 34.0 | 51.0 | 140.0 |
| ER visits | |||||||
| Total | 91.0 | 47.6 | 12.0 | 51.0 | 83.0 | 120.0 | 246.0 |
| Respiratory | 66.6 | 28.4 | 10.0 | 44.0 | 66.0 | 88.0 | 165.0 |
| Models/PM10 | RR (95% CI) | p | SO2 | RR (95% CI) | p | NO2 | RR (95% CI) | p |
|---|---|---|---|---|---|---|---|---|
| Non-dust days | ||||||||
| PM10 | 0.974 (0.96–0.99) | <0.01 | SO2 | 0.714 (0.63–0.81) | <0.01 | NO2 | 1.054 (1.04–31.07) | <0.01 |
| +SO2+NO2 | 0.966 (0.95–0.98) | <0.01 | +PM10+NO2 | 0.789 (0.70–0.90) | <0.01 | +PM10+SO2 | 1.068 (1.05–1.08) | <0.01 |
| Dust days | ||||||||
| PM10 | 1.140 (1.07–1.21) | <0.01 | SO2 | 0.970 (0.95–0.99) | <0.01 | NO2 | 1.220 (1.13–1.32) | <0.01 |
| +SO2+NO2 | 1.084 (1.01–1.16) | 0.018 | +PM10+NO2 | 0.947 (0.93–0.97) | <0.01 | +PM10+SO2 | 1.150 (1.07–1.24) | <0.01 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, Y.; Xiao, B.; Liu, C.; Zhao, Y.; Zheng, X. Association between Ambient Air Pollution and Emergency Room Visits for Respiratory Diseases in Spring Dust Storm Season in Lanzhou, China. Int. J. Environ. Res. Public Health 2016, 13, 613. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph13060613
Ma Y, Xiao B, Liu C, Zhao Y, Zheng X. Association between Ambient Air Pollution and Emergency Room Visits for Respiratory Diseases in Spring Dust Storm Season in Lanzhou, China. International Journal of Environmental Research and Public Health. 2016; 13(6):613. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph13060613
Chicago/Turabian StyleMa, Yuxia, Bingshuang Xiao, Chang Liu, Yuxin Zhao, and Xiaodong Zheng. 2016. "Association between Ambient Air Pollution and Emergency Room Visits for Respiratory Diseases in Spring Dust Storm Season in Lanzhou, China" International Journal of Environmental Research and Public Health 13, no. 6: 613. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph13060613





