The Associations between Dietary Patterns and Short Sleep Duration in Polish Adults (LifeStyle Study)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Study Design and Sample Collection
2.3. Eating Habits
2.4. Sleep Duration
2.5. Sociodemographic Variables
2.6. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Dietary Patterns
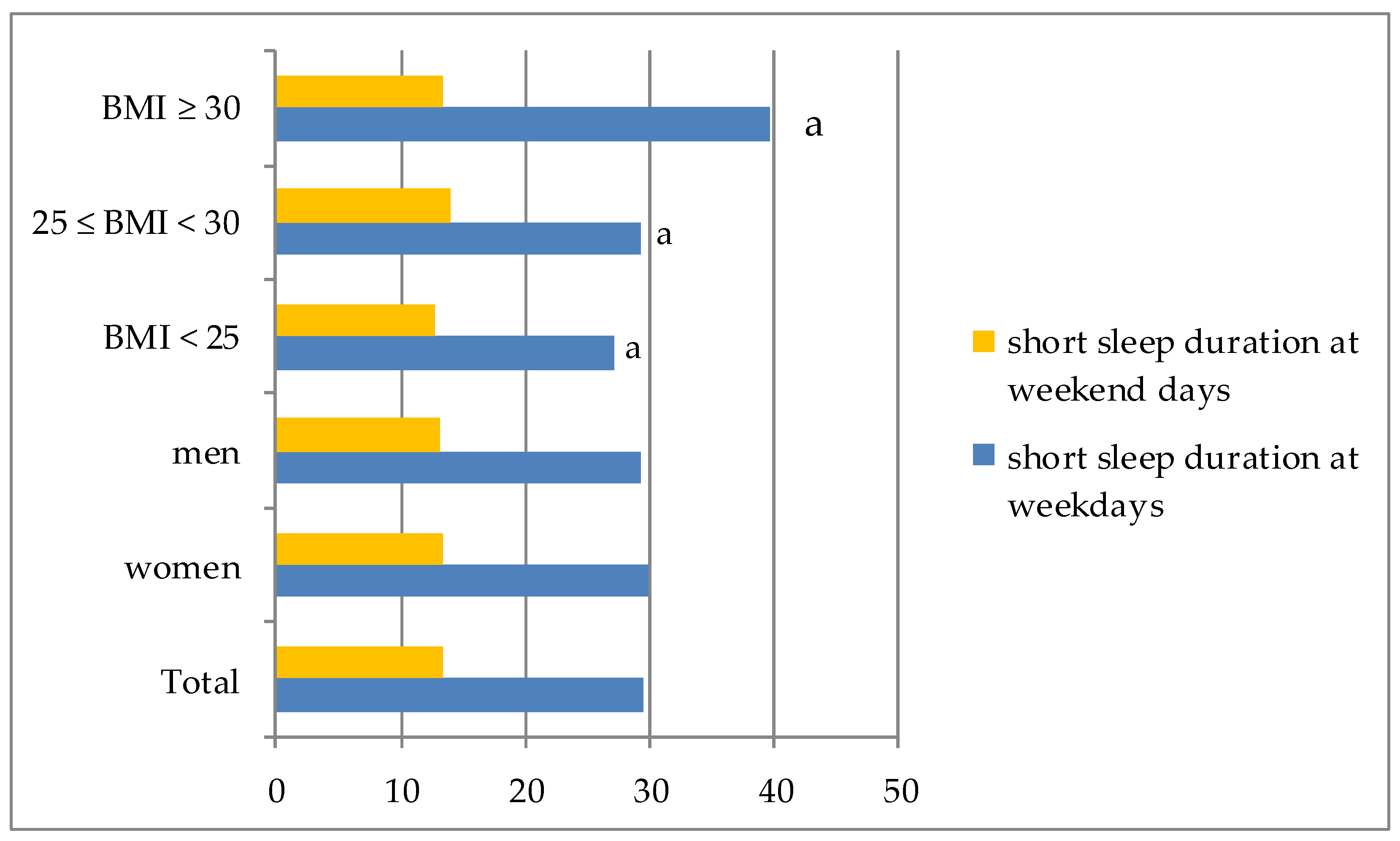
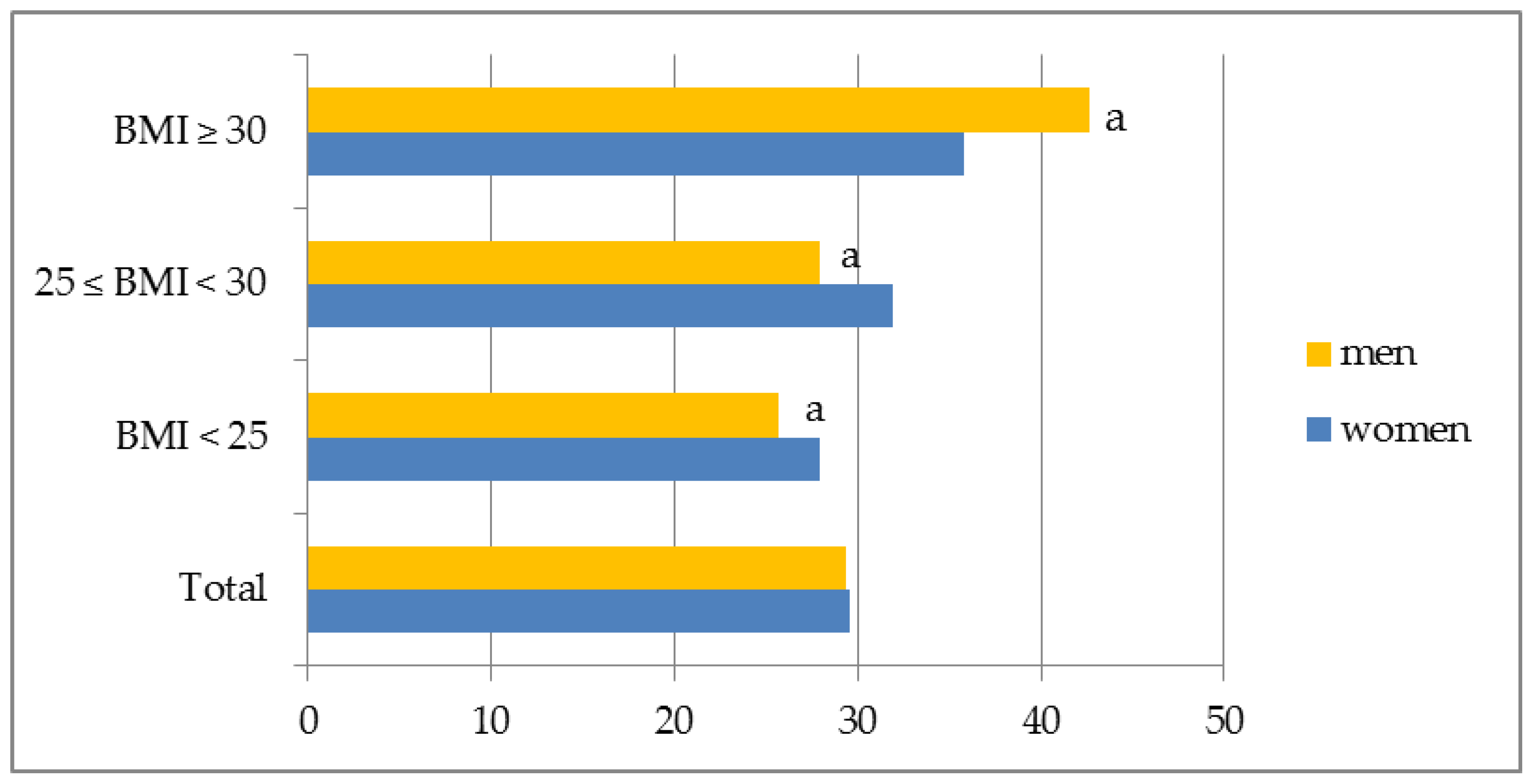
3.3. Sleep Duration
3.4. Dietary Patterns versus Sleep Duration
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hubáček, J.A. Eat less and exercise more—Is it really enough to knock down the obesity pandemia. Physiol. Res. 2009, 58, S1–S6. [Google Scholar] [PubMed]
- Knutson, K.L. Does inadequate sleep play a role in vulnerability to obesity? Am. J. Hum. Biol. 2012, 24, 361–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, S.R. Reduced sleep as an obesity risk factor. Obes. Rev. 2009, 10, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.R.; Hu, F.B. Short sleep duration and weight gain: A systematic review. Obesity 2008, 16, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Keith, S.W.; Redden, D.T.; Katzmarzyk, P.T.; Boggiano, M.M.; Hanlon, E.C.; Benca, R.M.; Ruden, D.; Pietrobelli, A.; Barger, J.L.; Fontaine, K. Putative contributors to the secular increase in obesity: Exploring the roads less traveled. Int. J. Obes. 2006, 30, 1585–1594. [Google Scholar] [CrossRef] [PubMed]
- Stranges, S.; Cappuccio, F.P.; Kandala, N.-B.; Miller, M.A.; Taggart, F.M.; Kumari, M.; Ferrie, J.E.; Shipley, M.J.; Brunner, E.J.; Marmot, M.G. Cross-sectional versus prospective associations of sleep duration with changes in relative weight and body fat distribution: The Whitehall II Study. Am. J. Epidemiol. 2007, 167, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 2017, 32, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Nagai, M.; Tomata, Y.; Watanabe, T.; Kakizaki, M.; Tsuji, I. Association between sleep duration, weight gain, and obesity for long period. Sleep Med. 2013, 14, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Horne, J. Short sleep is a questionable risk factor for obesity and related disorders: Statistical versus clinical significance. Biol. Psychol. 2008, 77, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Ikehara, S.; Iso, H.; Date, C.; Kikuchi, S.; Watanabe, Y.; Wada, Y.; Inaba, Y.; Tamakoshi, A.; Group, J.S. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: The JACC study. Sleep 2009, 32, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Golem, D.L.; Martin-Biggers, J.T.; Koenings, M.M.; Davis, K.F.; Byrd-Bredbenner, C. An integrative review of sleep for nutrition professionals. Adv. Nutr. 2014, 5, 742–759. [Google Scholar] [CrossRef] [PubMed]
- Gangwisch, J.E.; Heymsfield, S.B.; Boden-Albala, B.; Buijs, R.M.; Kreier, F.; Pickering, T.G.; Rundle, A.G.; Zammit, G.K.; Malaspina, D. Short sleep duration as a risk factor for hypertension: Analyses of the first National Health and Nutrition Examination Survey. Hypertension 2006, 47, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.-B.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Fatima, Y.; Doi, S.A.R.; Mamun, A.A. Sleep quality and obesity in young subjects: A meta-analysis. Obes. Rev. 2016, 17, 1154–1166. [Google Scholar] [CrossRef] [PubMed]
- Peltzer, K.; Pengpid, S. Sleep duration, sleep quality, body mass index, and waist circumference among young adults from 24 low-and middle-income and two high-income countries. Int. J. Environ. Res. Public Health 2017, 14, 566. [Google Scholar] [CrossRef] [PubMed]
- Ferrie, J.E.; Shipley, M.J.; Cappuccio, F.P.; Brunner, E.; Miller, M.A.; Kumari, M.; Marmot, M.G. A prospective study of change in sleep duration: Associations with mortality in the Whitehall II cohort. Sleep 2007, 30, 1659–1666. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.R.; Malhotra, A.; Gottlieb, D.J.; White, D.P.; Hu, F.B. Correlates of long sleep duration. Sleep 2006, 29, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Hale, L.; Emanuele, E.; James, S. Recent updates in the social and environmental determinants of sleep health. Curr. Sleep Med. Rep. 2015, 1, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Vézina-Im, L.-A.; Moreno, J.P.; Thompson, D.; Nicklas, T.A.; Baranowski, T. Individual, social and environmental determinants of sleep among women: Protocol for a systematic review and meta-analysis. BMJ Open 2017, 7, e016592. [Google Scholar] [CrossRef] [PubMed]
- Ohida, T.; Kamal, A.M.M.; Uchiyama, M.; Kim, K.; Takemura, S.; Sone, T.; Ishii, T. The influence of lifestyle and health status factors on sleep loss among the Japanese general population. Sleep 2001, 24, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Imaki, M.; Hatanaka, Y.; Ogawa, Y.; Yoshida, Y.; Tanada, S. An epidemiological study on relationship between the hours of sleep and life style factors in Japanese factory workers. J. Physiol. Anthropol. Appl. Human Sci. 2002, 21, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Basner, M.; Fomberstein, K.M.; Razavi, F.M.; Banks, S.; William, J.H.; Rosa, R.R.; Dinges, D.F. American time use survey: Sleep time and its relationship to waking activities. Sleep 2007, 30, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Lin, H.M.; Papaliaga, M.; Calhoun, S.; Vela-Bueno, A.; Chrousos, G.P.; Bixler, E.O. Short sleep duration and obesity: The role of emotional stress and sleep disturbances. Int. J. Obes. 2008, 32, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Peuhkuri, K.; Sihvola, N.; Korpela, R. Diet promotes sleep duration and quality. Nutr. Res. 2012, 32, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhai, L.; Zhang, D. Sleep duration and obesity among adults: A meta-analysis of prospective studies. Sleep Med. 2014, 15, 1456–1462. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Chakravorty, S.; Perlis, M.L.; Oliver, L.; Gurubhagavatula, I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014, 15, 42–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004, 1, e62. [Google Scholar] [CrossRef] [PubMed]
- Weiss, A.; Xu, F.; Storfer-Isser, A.; Thomas, A.; Ievers-Landis, C.E.; Redline, S. The association of sleep duration with adolescents’ fat and carbohydrate consumption. Sleep 2010, 33, 1201–1209. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.-P.; Roberts, A.L.; Chen, J.; Kelleman, M.; O’Keeffe, M.; RoyChoudhury, A.; Jones, P.J.H. Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. Am. J. Clin. Nutr. 2011, 94, 410–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grandner, M.A.; Kripke, D.F.; Naidoo, N.; Langer, R.D. Relationships among dietary nutrients and subjective sleep, objective sleep, and napping in women. Sleep Med. 2010, 11, 180–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nedeltcheva, A.V.; Kilkus, J.M.; Imperial, J.; Kasza, K.; Schoeller, D.A.; Penev, P.D. Sleep curtailment is accompanied by increased intake of calories from snacks. Am. J. Clin. Nutr. 2008, 89, 126–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grandner, M.A.; Jackson, N.; Gerstner, J.R.; Knutson, K.L. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite 2013, 64, 71–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haghighatdoost, F.; Karimi, G.; Esmaillzadeh, A.; Azadbakht, L. Sleep deprivation is associated with lower diet quality indices and higher rate of general and central obesity among young female students in Iran. Nutrition 2012, 28, 1146–1150. [Google Scholar] [CrossRef] [PubMed]
- Katagiri, R.; Asakura, K.; Kobayashi, S.; Suga, H.; Sasaki, S. Low intake of vegetables, high intake of confectionary, and unhealthy eating habits are associated with poor sleep quality among middle-aged female Japanese workers. J. Occup. Health 2014, 56, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Jaussent, I.; Dauvilliers, Y.; Ancelin, M.-L.; Dartigues, J.-F.; Tavernier, B.; Touchon, J.; Ritchie, K.; Besset, A. Insomnia symptoms in older adults: Associated factors and gender differences. Am. J. Geriatr. Psychiatry 2011, 19, 88–97. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.-P.; Mikic, A.; Pietrolungo, C.E. Effects of diet on sleep quality. Adv. Nutr. 2016, 7, 938–949. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, E.; Yatsuya, H.; Uemura, M.; Murata, C.; Otsuka, R.; Toyoshima, H.; Tamakoshi, K.; Sasaki, S.; Kawaguchi, L.; Aoyama, A. Associations of protein, fat, and carbohydrate intakes with insomnia symptoms among middle-aged Japanese workers. J. Epidemiol. 2013, 23, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.; Alén, M.; Cheng, S.M.; Mikkola, T.M.; Tenhunen, J.; Lyytikäinen, A.; Wiklund, P.; Cong, F.; Saarinen, A.; Tarkka, I. Associations of disordered sleep with body fat distribution, physical activity and diet among overweight middle-aged men. J. Sleep Res. 2015, 24, 414–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dashti, H.S.; Scheer, F.A.J.L.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short sleep duration and dietary intake: Epidemiologic evidence, mechanisms, and health implications. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef] [PubMed]
- Machón, M.; Mateo-Abad, M.; Vrotsou, K.; Zupiria, X.; Güell, C.; Rico, L.; Vergara, I. Dietary Patterns and Their Relationship with Frailty in Functionally Independent Older Adults. Nutrients 2018, 10, 406. [Google Scholar] [CrossRef] [PubMed]
- Mazidi, M.; Kengne, A.P.; Vatanparast, H. Association of dietary patterns of American adults with bone mineral density and fracture. Public Health Nutr. 2018, 21, 2417–2423. [Google Scholar] [CrossRef] [PubMed]
- Wadolowska, L.; Kowalkowska, J.; Lonnie, M.; Czarnocinska, J.; Jezewska-Zychowicz, M.; Babicz-Zielinska, E. Associations between physical activity patterns and dietary patterns in a representative sample of Polish girls aged 13–21 years: A cross-sectional study (GEBaHealth Project). BMC Public Health 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Cespedes, E.M.; Hu, F.B. Nutrition: Dietary prevention of obesity and cardiometabolic disease. Nat. Rev. Endocrinol. 2015, 11, 448–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bixler, E. Sleep and society: An epidemiological perspective. Sleep Med. 2009, 10, S3–S6. [Google Scholar] [CrossRef] [PubMed]
- Denova-Gutiérrez, E.; Castañón, S.; Talavera, J.O.; Flores, M.; Macías, N.; Rodríguez-Ramírez, S.; Flores, Y.N.; Salmerón, J. Dietary patterns are associated with different indexes of adiposity and obesity in an urban Mexican population. J. Nutr. 2011, 141, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Umairah, S.N.; Yahya, B.T.; Datin, M.; Yusof, S.M. Relationship between dietary pattern and body mass index among primary school children. Asian J. Clin. Nutr. 2012, 4, 142–150. [Google Scholar] [CrossRef]
- Meisinger, C.; Heier, M.; Löwel, H.; Schneider, A.; Döring, A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: The MONICA/KORA Augsburg cohort study. Sleep 2007, 30, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Suarez, E.C. 93. Gender-specific associations between disturbed sleep and biomarkers of inflammation, coagulation and insulin resistance. Brain Behav. Immun. 2008, 4, 29–30. [Google Scholar] [CrossRef]
- Kim, S.; DeRoo, L.A.; Sandler, D.P. Eating patterns and nutritional characteristics associated with sleep duration. Public Health Nutr. 2011, 14, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Jezewska-Zychowicz, M.; Gębski, J.; Guzek, D.; Świątkowska, M.; Stangierska, D.; Plichta, M.; Wasilewska, M. The Associations between Dietary Patterns and Sedentary Behaviors in Polish Adults (LifeStyle Study). Nutrients 2018, 10, 1004. [Google Scholar] [CrossRef] [PubMed]
- Beliefs and Eating Habits Questionnaire; Behavioral Conditions of Nutrition Team, Committee of Human Nutrition Science, Polish Academy of Science: Warsaw, Poland, 2014; Available online: http://www.knozc.pan.pl/ (accessed on 15 November 2016).
- Kant, A.K.; Graubard, B.I. Association of self-reported sleep duration with eating behaviors of American adults: NHANES 2005–2010. Am. J. Clin. Nutr. 2014, 100, 938–947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stern, J.H.; Grant, A.S.; Thomson, C.A.; Tinker, L.; Hale, L.; Brennan, K.M.; Woods, N.F.; Chen, Z. Short sleep duration is associated with decreased serum leptin, increased energy intake and decreased diet quality in postmenopausal women. Obesity 2014, 22, E55–E61. [Google Scholar] [CrossRef] [PubMed]
- Patterson, R.E.; Emond, J.A.; Natarajan, L.; Wesseling-Perry, K.; Kolonel, L.N.; Jardack, P.; Ancoli-Israel, S.; Arab, L. Short Sleep Duration Is Associated with Higher Energy Intake and Expenditure among African-American and Non-Hispanic White Adults, 2. J. Nutr. 2014, 144, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; McNeil, J.; Despres, J.-P.; Bouchard, C.; Tremblay, A. Seven to eight hours of sleep a night is associated with a lower prevalence of the metabolic syndrome and reduced overall cardiometabolic risk in adults. PLoS ONE 2013, 8, e72832. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Field, A. Discopering Statistics Using SPSS, 3rd ed.; Sage Publications: London, UK, 2009. [Google Scholar]
- Ursin, R.; Bjorvatn, B.; Holsten, F. Sleep duration, subjective sleep need, and sleep habits of 40-to 45-year-olds in the Hordaland Health Study. Sleep 2005, 28, 1260–1269. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, K.A.; Brownson, R.C. Sleep duration and obesity-related risk factors in the rural Midwest. Prev. Med. 2008, 46, 439–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noorwali, E.A.; Cade, J.E.; Burley, V.J.; Hardie, L.J. The relationship between sleep duration and fruit/vegetable intakes in UK adults: A cross-sectional study from the National Diet and Nutrition Survey. BMJ Open 2018, 8, e020810. [Google Scholar] [CrossRef] [PubMed]
- Tu, X.; Cai, H.; Gao, Y.-T.; Wu, X.; Ji, B.-T.; Yang, G.; Li, H.; Zheng, W.; Shu, X.O. Sleep duration and its correlates in middle-aged and elderly Chinese women: The Shanghai Women’s Health Study. Sleep Med. 2012, 13, 1138–1145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jabs, J.; Devine, C.M. Time scarcity and food choices: An overview. Appetite 2006, 47, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Gładysz, G.; Kobos, E.; Czarnecka, J.; Imiela, J. Zachowania Żywieniowe Pielęgniarek w Środowisku Pracy. Pielęgniarstwo Pol. Pol. Nurs. 2016, 149. [Google Scholar] [CrossRef]
- Powell, L.M.; Nguyen, B.T.; Han, E. Energy intake from restaurants: Demographics and socioeconomics, 2003–2008. Am. J. Prev. Med. 2012, 43, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Moffat, T.; Galloway, T. Food consumption patterns in elementary school children. Can. J. Diet. Pract. Res. 2008, 69, 152–154. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, G.; Pammolli, A.; Azzolini, E.; Simi, R.; Meoni, V.; de Wet, D.R.; Giacchi, M.V. Association between fruits and vegetables intake and frequency of breakfast and snacks consumption: A cross-sectional study. Nutr. J. 2013, 12, 123. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.V. Supporting healthful eating through retail environmental change: Communities putting prevention to work. Prev. Chronic Dis. 2013, 10, E189. [Google Scholar] [CrossRef] [PubMed]
- Hampl, J.S.; Heaton, C.L.B.; Taylor, C.A. Snacking patterns influence energy and nutrient intakes but not body mass index. J. Hum. Nutr. Diet. 2003, 16, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Kerr, M.A.; Rennie, K.L.; McCaffrey, T.A.; Wallace, J.M.W.; Hannon-Fletcher, M.P.; Livingstone, M.B.E. Snacking patterns among adolescents: A comparison of type, frequency and portion size between Britain in 1997 and Northern Ireland in 2005. Br. J. Nutr. 2008, 101, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Paxton, S.J.; Hannan, P.J.; Haines, J.; Story, M. Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. J. Adolesc. Heal. 2006, 39, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Jezewska-Zychowicz, M.; Wadolowska, L.; Kowalkowska, J.; Lonnie, M.; Czarnocinska, J.; Babicz-Zielinska, E. Perceived Health and Nutrition concerns as predictors of dietary patterns among Polish Females aged 13–21 years (GEBaHealth Project). Nutrients 2017, 9, 613. [Google Scholar] [CrossRef] [PubMed]
- Duke, C.H.; Williamson, J.A.; Snook, K.R.; Finch, K.C.; Sullivan, K.L. Association between fruit and vegetable consumption and sleep quantity in pregnant women. Mater. Child Health J. 2017, 21, 966–973. [Google Scholar] [CrossRef] [PubMed]
- Magee, C.A.; Caputi, P.; Iverson, D.C. Short sleep mediates the association between long work hours and increased body mass index. J. Behav. Med. 2011, 34, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Kikuchi, H.; Tanaka, K.; Takahashi, M. Association of short sleep duration with weight gain and obesity at 1-year follow-up: A large-scale prospective study. Sleep 2010, 33, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Charlton, K.; Kowal, P.; Soriano, M.M.; Williams, S.; Banks, E.; Vo, K.; Byles, J. Fruit and vegetable intake and body mass index in a large sample of middle-aged Australian men and women. Nutrients 2014, 6, 2305–2319. [Google Scholar] [CrossRef] [PubMed]
- Rangan, A.; Zheng, M.; Olsen, N.J.; Rohde, J.F.; Heitmann, B.L. Shorter sleep duration is associated with higher energy intake and an increase in BMI z-score in young children predisposed to overweight. Int. J. Obes. 2018, 42, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Kleiser, C.; Wawro, N.; Stelmach-Mardas, M.; Boeing, H.; Gedrich, K.; Himmerich, H.; Linseisen, J. Are sleep duration, midpoint of sleep and sleep quality associated with dietary intake among Bavarian adults? Eur. J. Clin. Nutr. 2017, 71, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Hicks, R.A.; Mc Tighe, S.; Juarez, M. Sleep duration and eating behaviors of college students. Percept. Mot. Skills 1986, 62, 25–26. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.S. Principles of Nutritional Assessment; Oxford University Press: New York, NY, USA, 2005; ISBN 0195171691. [Google Scholar]
- Signal, T.L.; Gale, J.; Gander, P.H. Sleep measurement in flight crew: Comparing actigraphic and subjective estimates to polysomnography. Aviat. Space Environ. Med. 2005, 76, 1058–1063. [Google Scholar] [PubMed]
- Marshall, N.S.; Glozier, N.; Grunstein, R.R. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med. Rev. 2008, 12, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Kurina, L.M.; McClintock, M.K.; Chen, J.-H.; Waite, L.J.; Thisted, R.A.; Lauderdale, D.S. Sleep duration and all-cause mortality: A critical review of measurement and associations. Ann. Epidemiol. 2013, 23, 361–370. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total Sample | 18.5 ≤ BMI < 25 | 25 ≤ BMI < 30 | BMI ≥ 30 | |||||
|---|---|---|---|---|---|---|---|---|---|
| N = 972 | 100% | N = 484 | 100% | N = 360 | 100% | N = 128 | 100% | ||
| Gender * | Female | 499 | 51.3 | 305 | 63.0 | 141 | 39.2 | 53 | 41.4 |
| Male | 473 | 48.7 | 179 | 37.0 | 219 | 60.8 | 75 | 58.6 | |
| Age * | 21–34 years old | 346 | 35.6 | 227 | 46.9 | 101 | 28.1 | 18 | 14.1 |
| 35–44 years old | 228 | 23.5 | 116 | 24.0 | 86 | 23.9 | 26 | 20.3 | |
| 45–54 years old | 131 | 13.5 | 49 | 10.1 | 48 | 13.3 | 34 | 26.5 | |
| 55–65 years old | 267 | 27.4 | 92 | 19.0 | 125 | 34.7 | 50 | 39.1 | |
| Place of residence | City ≤ 50,000 residents | 195 | 20.1 | 88 | 18.2 | 81 | 22.5 | 26 | 20.3 |
| City > 50,000 residents | 521 | 53.6 | 269 | 26.2 | 190 | 52.8 | 62 | 48.4 | |
| Rural area | 256 | 26.3 | 127 | 55.6 | 89 | 24.7 | 40 | 31.3 | |
| Education * | Upper secondary and lower | 388 | 39.9 | 156 | 32.2 | 164 | 45.6 | 68 | 53.1 |
| Higher | 584 | 60.1 | 328 | 67.8 | 196 | 54.4 | 60 | 46.9 | |
| Dietary Patterns | Short Sleep Duration | Model | Total Sample | Women | Men | 18.5 ≤ BMI < 25 | 25 ≤ BMI < 30 | BMI >= 30 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Upper Tertile | p | Upper Tertile | p | Upper Tertile | p | Upper Tertile | p | Upper Tertile | p | Upper Tertile | p | |||
| Fast foods & sweets | at weekdays | Crude a | 0.68 (0.48; 0.95) | * | 0.67 (0.43; 0.95) | * | 0.61 (0.32 0.95) | * | 0.64 (0.39; 0.96) | * | 0.48 (0.26; 0.88) | * | 1.15 (0.44; 3.01 | |
| (ref. bottom tertile) | Adjusted b | 0.63 (0.44; 0.90 | ** | 0.61 (0.38; 0.98) | * | 0.58 (0.33; 0.97) | * | 0.55 (0.32; 0.93) | * | 0.45 (0.23; 0.85) | * | 1.68 (0.59; 4.79) | ||
| at weekend | Crude | 0.69 (0.45; 1.07) | 0.79 (0.44; 1.39) | 0.44 (0.21; 0.92) | * | 0.51 (0.27; 0.96) | * | 0.63 (0.28; 1.41) | 1.23 (0.29; 5.16) | |||||
| Adjusted | 0.61 (0.38; 0.96) | * | 0.70 (0.38; 1.28) | 0.37 (0.17; 0.79) | * | 0.42 (0.22; 0.82) | * | 0.57 (0.24; 1.36) | 1.23 (0.26; 5.78) | |||||
| Fruit & vegetable | at weekdays | Crude | 0.61 (0.44; 0.86) | ** | 0.99 (0.62; 1.57) | 0.33 (0.20; 0.56) | *** | 0.59 (0.35; 0.97) | * | 0.50 (0.28; 0.89) | * | 0.37 (0.13; 0.96) | * | |
| (ref. bottom tertile) | Adjusted | 0.62 (0.44; 0.88) | ** | 1.01 (0.63; 1.61) | 0.34 (0.20; 0.58) | *** | 0.61 (0.36; 0.98) | * | 0.50 (0.27; 0.92) | * | 0.21 (0.06; 0.67) | * | ||
| at weekend | Crude | 1.23 (0.79; 1.92) | 1.71 (1.04; 3.09) | * | 0.88 (0.44; 1.76) | 1.16 (0.61; 2.19) | 1.46 (0.66; 3.21) | 0.15 (0.03; 0.76) | ||||||
| Adjusted | 1.25 (0.80; 1.97) | 1.70 (1.02; 3.11) | * | 0.95 (0.46; 1.93) | 1.22 (0.63; 2.33) | 1.48 (0.64; 3.40) | 0.16 (0.03; 0.91) | |||||||
| Wholemeal food | at weekdays | Crude | 1.25 (0.89; 1.76) | 1.36 (0.85; 2.16) | * | 1.14 (0.67; 1.95) | 1.82 (1.07; 3.08) | * | 0.57 (0.31; 1.04) | 1.66 (0.65; 4.22) | ||||
| (ref. bottom tertile) | Adjusted | 1.22 (0.86; 1.70) | 1.35 (0.85; 2.16) | 1.11 (0.65; 1.90) | 1.80 (1.05; 3.10) | * | 0.57 (0.31; 1.05) | 1.45 (0.55; 3.83) | ||||||
| at weekend | Crude | 0.90 (0.58; 1.40) | 1.16 (0.64; 2.12) | 0.65 (0.33; 1.26) | 1.46 (0.74; 2.88) | 0.43 (0.20; 0.92) | * | 0.84 (0.23; 3.03) | ||||||
| Adjusted | 0.84 (0.54; 1.37) | 1.14 (0.62; 2.09) | 0.58 (0.29; 1.14) | 1.39 (0.70; 2.77) | 0.37 (0.16; 0.83) | * | 0.80 (0.21; 3.00) | |||||||
| Fruit &vegetable juices (ref. bottom tertile) | at weekdays | Crude | 0.97 (0.69; 1.36) | 0.87 (0.54; 1.38) | 1.15 (0.69; 1.90) | 0.80 (0.48; 1.32) | 1.41 (0.80; 2.48) | 0.63 (0.23; 1.70) | ||||||
| Adjusted | 0.99 (0.71; 1.40) | 0.91 (0.57; 1.46) | 1.14 (0.69; 1.30) | 0.79 (0.47; 1.32) | 1.48 (0.83; 2.66) | 0.62 (0.21; 1.83) | ||||||||
| at weekend | Crude | 0.69 (0.44; 1.08) | 0.56 (0.30; 0.96) | * | 0.92 (0.48; 1.76) | 0.65 (0.34; 1.26) | 0.74 (0.34; 1.59) | 0.55 (0.13; 2.26) | ||||||
| Adjusted | 0.70 (0.44; 1.11) | 0.62 (0.33; 1.19) | 0.86 (0.44; 1.70) | 0.67 (0.34; 1.31) | 0.79 (0.35; 1.70) | 0.45 (0.10; 2.11) | ||||||||
| Meat & meat products (ref. bottom tertile) | at weekdays | Crude | 1.13 (0.80; 1.59) | 1.02 (0.63; 1.65) | 1.41 (0.85; 2.34) | 0.98 (0.58; 1.63) | 2.22 (1.23; 4.00) | 0.47 (0.16; 1.39) | ||||||
| Adjusted | 1.14 (0.81; 1.61) | 1.03 (0.64; 1.68) | 1.39 (0.84; 2.30) | 0.96 (0.57; 1.62) | 2.28 (1.24; 4.19) | 0.35 (0.11; 1.15) | ||||||||
| at weekend | Crude | 0.90 (0.57; 1.43) | 0.87 (0.46; 1.62) | 0.97 (0.48; 1.96) | 0.87 (0.44; 1.71) | 1.25 (0.56; 2.77) | ** | 0.14 (0.02; 1.29) | ||||||
| Adjusted | 0.88 (0.55; 1.40) | 0.82 (0.43; 1.55) | 0.89 (0.43; 1.84) | 0.86 (0.43; 1.72) | 1.08 (0.47; 2.48) | ** | 0.13 (0.01; 1.25) | |||||||
| Dietary Patterns | Short Sleep Duration | Model | 18.5 ≤ BMI < 25 | 25 ≤ BMI < 30 | BMI ≥ 30 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | Women | Men | |||||||||
| Upper Tertile | p | Upper Tertile | p | Upper Tertile | p | Upper Tertile | p | Upper Tertile | p | Upper Tertile | p | |||
| Fast foods & sweets | at weekdays | Crude a | 0.58 (0.31; 0.98) | * | 0.60 (0.22; 1.65) | 0.77 (0.31; 1.89) | 0.26 (0.10; 0.67) | ** | 1.22 (0.25; 5.90) | 1.23 (0.30; 5.06) | ||||
| (ref. bottom tertile) | Adjusted b | 0.48 (0.24; 0.93) | * | 0.58 (0.21; 1.65) | 0.82 (0.32; 2.14) | 0.23 (0.08; 0.63) | ** | 2.07 (0.35; 12.13) | 1.74 (0.36; 8.39) | |||||
| at weekend | Crude | 0.55 (0.25; 1.20) | 0.22 (0.04; 0.98) | * | 1.21 (0.35; 4.19) | 0.27 (0.07; 1.07) | 4.83 (0.18; 127.63) | 1.40 (0.22; 9.09) | ||||||
| Adjusted | 0.44 (0.19; 0.97) | * | 0.20 (0.04; 0.97) | * | 1.21 (0.32; 4.61) | 0.26 (0.06; 1.11) | >999.9 | 0.94 (0.13; 7.11) | ||||||
| Fruit & vegetable | at weekdays | Crude | 1.14 (0.60; 2.15) | 0.22 (0.08; 0.56) | ** | 0.42 (0.14; 1.22) | 0.47 (0.21; 1.05) | 0.92 (0.19; 4.45) | 0.10 (0.02; 0.55) | * | ||||
| (ref. bottom tertile) | Adjusted | 1.14 (0.60; 2.17) | 0.22 (0.08; 0.58) | ** | 0.43 (0.14; 1.29) | 0.45 (0.19; 0.98) | * | 0.34 (0.05; 2.35) | 0.08 (0.01; 0.46) | ** | ||||
| at weekend | Crude | 1.98 (0.88; 4.47) | 0.54 (0.17; 1.67) | 1.40 (0.40; 4.92) | 1.77 (0.53; 5.92) | 0.02 (<0.01; 0.75) | * | 0.17 (0.02; 1.43) | ||||||
| Adjusted | 2.05 (0.90; 4.68) | 0.58 (0.18; 1.85) | 1.17 (0.31; 4.42) | 1.92 (0.53; 7.00) | <0.001 | 0.26 (0.03; 2.55) | ||||||||
| Wholemeal food | at weekdays | Crude | 2.50 (1.30; 4.82) | ** | 0.96 (0.36; 2.52) | 0.66 (0.26; 1.71) | 0.59 (0.26; 1.34) | 0.80 (0.15; 4.38) | 4.76 (0.73; 31.21) | |||||
| (ref. bottom tertile) | Adjusted | 2.56 (1.31; 5.00) | ** | 0.88 (0.32; 2.40) | 0.65 (0.25; 1.71) | 0.56 (0.24; 1.32) | 0.62 (0.11; 3.64) | 4.41 (0.66; 29.44) | ||||||
| at weekend | Crude | 2.96 (1.17; 7.46) | * | 0.41 (0.12; 1.39) | 0.38 (0.12; 1.26) | 0.48 (0.16; 1.45) | 0.03 (<0.01; 2.29) | 1.04 (0.14; 7.67) | ||||||
| Adjusted | 2.83 (1.10; 7.27) | * | 0.37 (0.11; 1.28) | 0.37 (0.11; 1.28) | 0.34 (0.10; 1.13) | <0.001 | 1.41 (0.16; 12.47) | |||||||
| Fruit &vegetable juices (ref. bottom tertile) | at weekdays | Crude | 0.72 (0.37; 1.37) | 1.05 (0.44; 2.55) | 1.03 (0.43; 2.47) | 1.77 (0.81; 3.87) | 1.48 (0.30; 7.21) | 0.42 (0.10; 1.88) | ||||||
| Adjusted | 0.75 (0.38; 1.47) | 0.91 (0.36; 2.25) | 0.97 (0.39; 2.43) | 2.01 (0.90; 4.52) | 0.92 (0.16; 5.49) | 0.47 (0.09; 2.53) | ||||||||
| at weekend | Crude | 0.59 (0.24; 1.44) | 0.79 (0.27; 2.29) | 0.44 (0.13; 1.49) | 0.95 (0.33; 2.73) | 1.62 (0.08; 31.75) | 0.54 (0.08; 3.44) | |||||||
| Adjusted | 0.63 (0.25; 1.59) | 0.74 (0.25; 2.23) | 0.58 (0.16; 2.06) | 0.91 (0.29; 2.83) | <0.001 | 0.46 (0.05; 4.08) | ||||||||
| Meat & meat products (ref. bottom tertile) | at weekdays | Crude | 0.91 (0.47; 1.77) | 1.37 (0.56; 3.36) | 1.89 (0.72; 4.96) | 2.38 (1.08; 5.25) | * | 0.28 (0.04; 2.23) | 0.49 (0.11; 2.19) | |||||
| Adjusted | 0.90 (0.46; 1.77) | 1.30 (0.52; 3.25) | 2.12 (0.78; 5.75) | 2.29 (1.02; 5.17) | * | 0.35 (0.04; 3.37) | 0.42 (0.08; 2.26) | |||||||
| at weekend | Crude | 1.14 (0.46; 2.84) | 0.66 (0.20; 2.18) | 0.51 (0.14; 1.85) | 1.87 (0.62; 5.61) | <0.001 | 0.25 (0.02; 2.91) | |||||||
| Adjusted | 1.07 (0.43; 2.67) | 0.64 (0.19; 2.16) | 0.44 (0.11; 1.71) | 1.54 (0.48; 4.90) | <0.001 | 0.31 (0.02; 4.16) | ||||||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gębski, J.; Jezewska-Zychowicz, M.; Guzek, D.; Świątkowska, M.; Stangierska, D.; Plichta, M. The Associations between Dietary Patterns and Short Sleep Duration in Polish Adults (LifeStyle Study). Int. J. Environ. Res. Public Health 2018, 15, 2497. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15112497
Gębski J, Jezewska-Zychowicz M, Guzek D, Świątkowska M, Stangierska D, Plichta M. The Associations between Dietary Patterns and Short Sleep Duration in Polish Adults (LifeStyle Study). International Journal of Environmental Research and Public Health. 2018; 15(11):2497. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15112497
Chicago/Turabian StyleGębski, Jerzy, Marzena Jezewska-Zychowicz, Dominika Guzek, Monika Świątkowska, Dagmara Stangierska, and Marta Plichta. 2018. "The Associations between Dietary Patterns and Short Sleep Duration in Polish Adults (LifeStyle Study)" International Journal of Environmental Research and Public Health 15, no. 11: 2497. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15112497






