A School-Based Educational Intervention for School-Aged Children and Caregivers about Rational Use of Antibiotics in Urban Areas of Shaanxi Province: A Study Protocol for a Randomized Controlled Research
Abstract
:1. Introduction
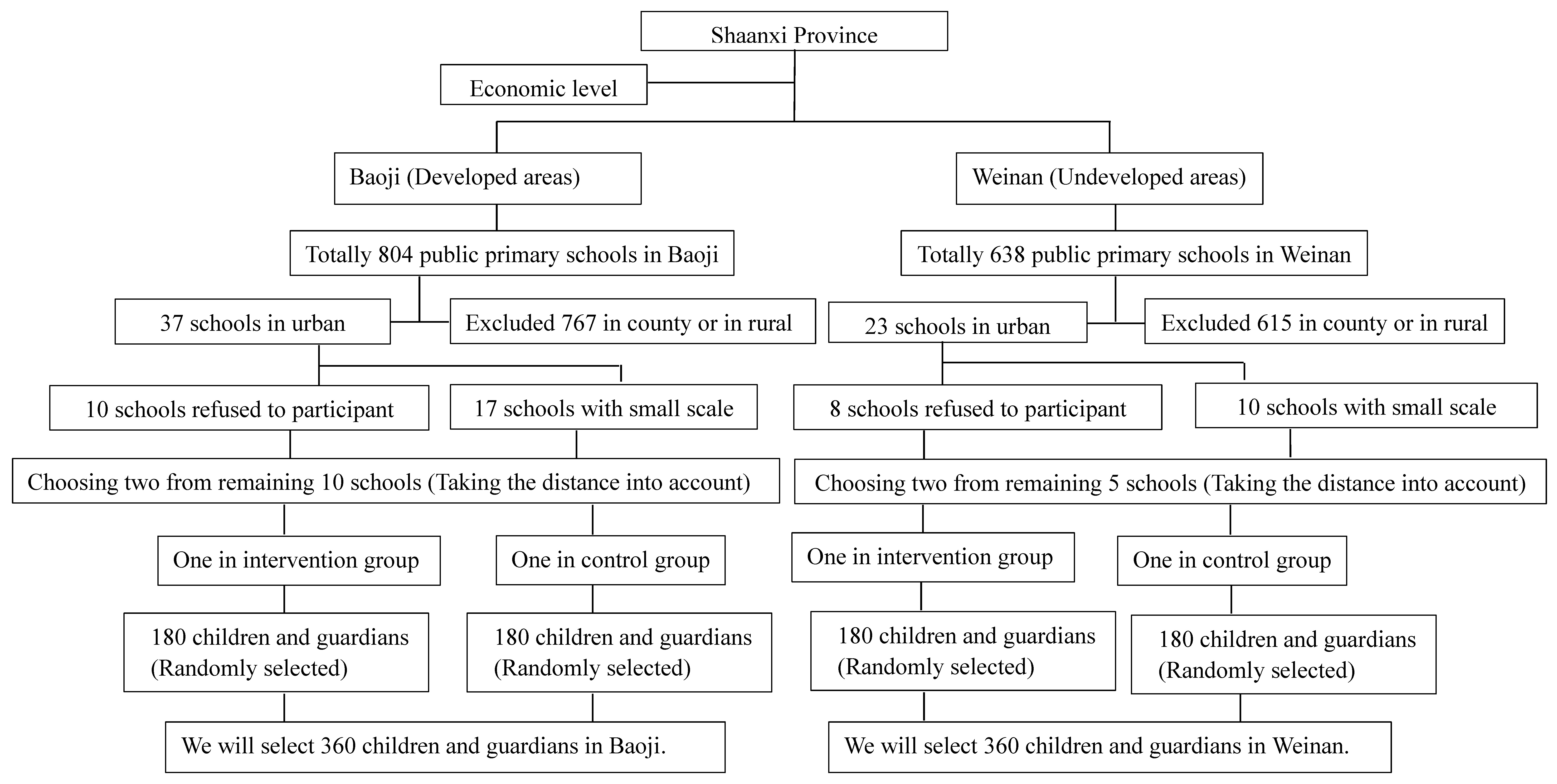
2. Materials and Methods
2.1. Study Design
2.2. Sample Size
2.3. Eligibility Criteria for Participants
- We will include healthy children (aged 8–12) and caregivers who have the primary responsibility for the children and have normal understanding, cognitive, and communication skills.
- Children and caregivers who volunteer to participate in this study must have lived in the sample area for more than a year and those with less mobility will be included. A written informed consent will be collected from all of the participants.
- We will exclude children with severe liver, kidney disease, chronic diseases, and severe syndromes.
- We will preclude caregivers who work in the health field.
2.4. Intervention Procedures
2.5. Outcome Indicators
2.6. Data Management
2.7. Data Analysis
2.8. Ethical Considerations
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kingston, W. Antibiotics, invention and innovation. Res. Policy 2000, 29, 679–710. [Google Scholar] [CrossRef]
- Agarwal, S.; Yewale, V.N.; Dharmapalan, D. Antibiotics Use and Misuse in Children: A Knowledge, Attitude and Practice Survey of Parents in India. J. Clin. Diagn. Res. 2015, 9, SC21–SC24. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.M.; Daschner, F.D. Colony-stimulating factors and antibiotics—A new prospect in treating infectious diseases? Clin. Microbiol. Infect. 1998, 4, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Morgan, D.J.; Okeke, I.N.; Laxminarayan, R.; Perencevich, E.N.; Weisenberg, S. Non-prescription antimicrobial use worldwide: A systematic review. Lancet Infect. Dis. 2011, 11, 692–701. [Google Scholar] [CrossRef]
- Hoffmann, K.; Wagner, G.; Apfalter, P.; Maier, M. Antibiotic resistance in primary care in Austria—A systematic review of scientific and grey literature. BMC Infect. Dis. 2011, 11, 330. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.F.L.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic resistance—The need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef]
- Lupo, A.; Coyne, S.; Berendonk, T.U. Origin and evolution of antibiotic resistance: The common mechanisms of emergence and spread in water bodies. Front. Microbiol. 2012, 3, 18. [Google Scholar] [CrossRef] [PubMed]
- Clavenna, A.; Bonati, M. Adverse drug reactions in childhood: A review of prospective studies and safety alerts. Arch. Dis. Child. 2009, 94, 724–728. [Google Scholar] [CrossRef] [PubMed]
- English, B.K.; Gaur, A.H. The Use and Abuse of Antibiotics and the Development of Antibiotic Resistance. Hot Top. Infect. Immun. Child. VI 2010, 659, 73–82. [Google Scholar]
- Hsu, C.Y.; Hsu, B.M.; Ji, W.T.; Chang, T.Y.; Kao, P.M.; Tseng, S.F.; Shen, T.Y.; Shih, F.C.; Fan, C.W.; Liu, J.H. A Potential Association between Antibiotic Abuse and Existence of Related Resistance Genes in Different Aquatic Environments. Water Air Soil Pollut. 2015, 226, 2235–2243. [Google Scholar] [CrossRef]
- Kumarasamy, K.K.; Toleman, M.A.; Walsh, T.R.; Bagaria, J.; Butt, F.; Balakrishnan, R.; Chaudhary, U.; Doumith, M.; Giske, C.G.; Irfan, S.; et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: A molecular, biological, and epidemiological study. Lancet Infect. Dis. 2010, 10, 597–602. [Google Scholar] [CrossRef]
- Hsueh, P.R. World Health Day 2011—Antimicrobial Resistance: No Action Today, No Cure Tomorrow. J. Formosan Med. Assoc. 2011, 110, 213–214. [Google Scholar] [CrossRef]
- Hey, S.P.; Kesselheim, A.S. Reprioritizing Research Activity for the Post-Antibiotic Era: Ethical, Legal, and Social Considerations. Hastings Cent. Rep. 2017, 47, 16–20. [Google Scholar] [CrossRef] [PubMed]
- China Antimicrobial Resistance Surveillance System—National Antimicrobial Resistance Surveillance Report in 2015. Available online: http://www.carss.cn/Report/Details/282 (accessed on 10 January 2018).
- Bi, P.; Tong, S.L.; Parton, K.A. Family self-medication and antibiotics abuse for children and juveniles in a Chinese city. Soc. Sci. Med. 2000, 50, 1445–1450. [Google Scholar] [CrossRef]
- Grossman, Z.; del Torso, S.; Hadjipanayis, A.; van Esso, D.; Drabik, A.; Sharland, M. Antibiotic prescribing for upper respiratory infections: European primary paediatricians’ knowledge, attitudes and practice. Acta Paediatr. 2012, 101, 935–940. [Google Scholar] [CrossRef] [PubMed]
- File, T.M.; Hadley, J.A. Rational use of antibiotics to treat respiratory tract infections. Am. J. Manag. Care 2002, 8, 713–727. [Google Scholar] [PubMed]
- Stone, S.; Gonzales, R.; Maselli, J.; Lowenstein, S.R. Antibiotic prescribing for patients with colds, upper respiratory tract infections, and bronchitis: A national study of hospital-based emergency departments. Ann. Emerg. Med. 2000, 36, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Cantrell, R.; Young, A.F.; Martin, B.C. Antibiotic prescribing in ambulatory care settings for adults with colds, upper respiratory tract infections, and bronchitis. Clin. Ther. 2002, 24, 170–182. [Google Scholar] [CrossRef]
- Matthys, J.; De Meyere, M. Antibiotics for acute sore throat. Lancet Infect. Dis. 2014, 14, 919–920. [Google Scholar] [CrossRef]
- Ding, L.L.; Sun, Q.; Sun, W.S.; Du, Y.H.; Li, Y.; Bian, X.F.; He, G.Q.; Bai, H.D.; Dyar, O.J. Antibiotic use in rural China: A cross-sectional survey of knowledge, attitudes and self-reported practices among caregivers in Shandong province. BMC Infect. Dis. 2015, 15, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Hawker, J.I.; Smith, S.; Smith, G.E.; Morbey, R.; Johnson, A.P.; Fleming, D.M.; Shallcross, L.; Hayward, A.C. Trends in antibiotic prescribing in primary care for clinical syndromes subject to national recommendations to reduce antibiotic resistance, UK 1995–2011: Analysis of a large database of primary care consultations. J. Antimicrob. Chemother. 2014, 69, 3423–3430. [Google Scholar] [CrossRef] [PubMed]
- Parimi, N.; Pinto Pereira, L.M.; Prabhakar, P. Caregivers’ practices, knowledge and beliefs of antibiotics in paediatric upper respiratory tract infections in Trinidad and Tobago: A cross-sectional study. BMC Fam. Pract. 2004, 5, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seedat, F.; Stinton, C.; Patterson, J.; Geppert, J.; Tan, B.; Robinson, E.R.; McCarthy, N.D.; Uthman, O.A.; Freeman, K.; Johnson, S.A.; et al. Adverse events in women and children who have received intrapartum antibiotic prophylaxis treatment: A systematic review. BMC Pregnancy Childbirth 2017, 17, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Niu, W.; Guo, L.Y.; Jin, X.P.; Wang, G.J.; Shi, X.; Liu, B.H. Analysis on adverse reactions caused annually by cases of antibiotic use in a hospital of China. Afr. J. Microbiol. Res. 2013, 6, 6838–6842. [Google Scholar]
- Rouusounides, A.; Papaevangelou, V.; Hadjipanayis, A.; Panagakou, S.; Theodoridou, M.; Syrogiannopoulos, G.; Hadjichristodoulou, C. Descriptive Study on Parents’ Knowledge, Attitudes and Practices on Antibiotic Use and Misuse in Children with Upper Respiratory Tract Infections in Cyprus. Int. J. Environ. Res. Public Health 2011, 8, 3246–3262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panagakou, S.G.; Spyridis, N.; Papaevangelou, V.; Theodoridou, K.M.; Goutziana, G.P.; Theodoridou, M.N.; Syrogiannopoulos, G.A.; Hadjichristodoulou, C.S. Antibiotic use for upper respiratory tract infections in children: A cross-sectional survey of knowledge, attitudes, and practices (KAP) of parents in Greece. BMC Pediatr. 2011, 11, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Alexandrino, A.S.; Santos, R.; Melo, C.; Bastos, J.M. Impact of caregivers’ education regarding respiratory infections on the health status of day-care children: A randomized trial. Fam. Pract. 2016, 33, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Cebotarenco, N.; Bush, P.J. Reducing antibiotics for colds and flu: A student-taught program. Health Educ. Res. 2008, 23, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.S.; Rifas-Shiman, S.L.; Kleinman, K.; Kotch, J.; Schiff, N.; Stille, C.J.; Steingard, R.; Finkelstein, J.A. Parental knowledge about antibiotic use: Results of a cluster-randomized, multicommunity intervention. Pediatrics 2007, 119, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.A.; Kwan-Gett, T.S.C.; McMahon, E.M. Effectiveness of an educational intervention in modifying parental attitudes about antibiotic usage in children. Pediatrics 2003, 111, e548–e554. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.A.; Kwan-Gett, T.S.C.; McMahon, E.M. Effectiveness of a parental educational intervention in reducing antibiotic use in children—A randomized controlled trial. Pediatr. Infect. Dis. J. 2005, 24, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Zhang, Z.; Walley, J.D. Effect of a training and educational intervention for physicians and caregivers on antibiotic prescribing for upper respiratory tract infections in children at primary care facilities in rural China: A cluster-randomised controlled trial. Lancet Glob. Health 2018, 6, e1258–e1267. [Google Scholar] [CrossRef]
- Young, V.L.; Cole, A.; Lecky, D.M.; Fettis, D.; Pritchard, B.; Verlander, N.Q.; Eley, C.V.; McNulty, C.A.M. A mixed-method evaluation of peer-education workshops for school-aged children to teach about antibiotics, microbes and hygiene. J. Antimicrob. Chemother. 2017, 72, 2119–2126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Formoso, G.; Paltrinieri, B.; Marata, A.M.; Gagliotti, C.; Pan, A.; Moro, M.L.; Capelli, O.; Magrini, N.; Group, L.S. Feasibility and effectiveness of a low cost campaign on antibiotic prescribing in Italy: Community level, controlled, non-randomised trial. BMJ 2013, 347, f5391. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.M.; Pan, D.S.T.; Huang, J.H.; Chen, M.I.C.; Chong, J.W.C.; Goh, E.H.; Jiang, L.L.; Leo, Y.S.; Lee, T.H.; Wong, C.S.; et al. Results from a Patient-Based Health Education Intervention in Reducing Antibiotic Use for Acute Upper Respiratory Tract Infections in the Private Sector Primary Care Setting in Singapore. Antimicrob. Agents Chemother. 2017, 61, e02257-16. [Google Scholar] [CrossRef] [PubMed]
- Sabuncu, E.; David, J.; Bernede-Bauduin, C.; Pepin, S.; Leroy, M.; Boelle, P.Y.; Watier, L.; Guillemot, D. Significant Reduction of Antibiotic Use in the Community after a Nationwide Campaign in France, 2002–2007. PLoS Med. 2009, 6, e1000084. [Google Scholar] [CrossRef] [PubMed]
- Finch, R.G.; Metlay, J.P.; Davey, P.G.; Baker, L.J. Educational interventions to improve antibiotic use in the community: Report from the International Forum on Antibiotic Resistance (IFAR) colloquium, 2002. Lancet Infect. Dis. 2004, 4, 44–53. [Google Scholar] [CrossRef]
- Boutron, I.; Altman, D.G.; Moher, D.; Schulz, K.F.; Ravaud, P. CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts. Ann. Intern. Med. 2017, 167, 40–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, J.; Lv, B.; Zhu, S.; Yu, J.L.; Zhang, Y.; Ye, D.; Aziz, M.M.; Yang, C.J.; Fang, Y. Non-prescription use of antibiotics among children in urban China: A cross-sectional survey of knowledge, attitudes, and practices. Expert Rev. Anti-Infect. Ther. 2018, 16, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Weddle, G.; Goldman, J.; Myers, A.; Newland, J. Impact of an Educational Intervention to Improve Antibiotic Prescribing for Nurse Practitioners in a Pediatric Urgent Care Center. J. Pediatr. Health Care 2017, 31, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Belongia, E.A.; Naimi, T.S.; Gale, C.M.; Besser, R.E. Antibiotic use and upper respiratory infections: A survey of knowledge, attitudes, and experience in Wisconsin and Minnesota. Prev. Med. 2002, 34, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Gu, J.R.; Zhang, M.Y.; Ren, Z.; Yang, W.D.; Chen, Y.; Fu, Y.M.; Chen, X.B.; Cals, J.W.L.; Zhang, F.M. Knowledge, attitude and practice of antibiotics: A questionnaire study among 2500 Chinese students. BMC Med. Educ. 2013, 13, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Panagakou, S.G.; Theodoridou, M.N.; Papaevangelou, V.; Papastergiou, P.; Syrogiannopoulos, G.A.; Goutziana, G.P.; Hadjichristodoulou, C.S. Development and assessment of a questionnaire for a descriptive cross-sectional study concerning parents’ knowledge, attitudes and practices in antibiotic use in Greece. BMC Infect. Dis. 2009, 9, 52–64. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Zhao, G.M.; Lundborg, C.S.; Zhu, Y.P.; Zhao, Q.; Xu, B. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: A cross-sectional study. BMC Infect. Dis. 2014, 14, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Zyoud, S.H.; Abu Taha, A.; Araj, K.F.; Abahri, I.A.; Sawalha, A.F.; Sweileh, W.M.; Awang, R.; Al-Jabi, S.W. Parental knowledge, attitudes and practices regarding antibiotic use for acute upper respiratory tract infections in children: A cross-sectional study in Palestine. BMC Pediatr. 2015, 15, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Index. Available online: http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm (accessed on 10 January 2018).
- China’s WeChat Becoming Way of Life. Available online: http://www.chinadaily.com.cn/business/tech/2017-04/26/content_29094390.htm (accessed on 10 March 2018).
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Kabba, J.; Chang, J.; Ji, W.; Zhu, S.; Yu, J.; Xu, S.; Fang, Y. A School-Based Educational Intervention for School-Aged Children and Caregivers about Rational Use of Antibiotics in Urban Areas of Shaanxi Province: A Study Protocol for a Randomized Controlled Research. Int. J. Environ. Res. Public Health 2018, 15, 1912. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15091912
Zhang Y, Kabba J, Chang J, Ji W, Zhu S, Yu J, Xu S, Fang Y. A School-Based Educational Intervention for School-Aged Children and Caregivers about Rational Use of Antibiotics in Urban Areas of Shaanxi Province: A Study Protocol for a Randomized Controlled Research. International Journal of Environmental Research and Public Health. 2018; 15(9):1912. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15091912
Chicago/Turabian StyleZhang, Yu, John Kabba, Jie Chang, Wenjing Ji, Shan Zhu, Jiale Yu, Sen Xu, and Yu Fang. 2018. "A School-Based Educational Intervention for School-Aged Children and Caregivers about Rational Use of Antibiotics in Urban Areas of Shaanxi Province: A Study Protocol for a Randomized Controlled Research" International Journal of Environmental Research and Public Health 15, no. 9: 1912. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15091912



