Translation and Validation of the Korean Version of the Revised Health Care System Distrust Scale (HCSD-K) in Korean American Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Healthcare System Distrust
2.2.2. Perceived Discrimination in Health Care
2.2.3. Trust in Physician
2.3. Translation Process
2.3.1. Step 1: Committee-Based Translation
2.3.2. Step 2: Expert Review
2.3.3. Step 3: Cognitive Interviews
2.3.4. Step 4: Review of Translated Scale
2.4. Statistical Analysis
2.4.1. Descriptive Statistics
2.4.2. Construct Validity
2.4.3. Reliability
3. Results
3.1. Participants
3.2. Translation, Cognitive Interviewing and Adaptation
3.3. Construct Validity
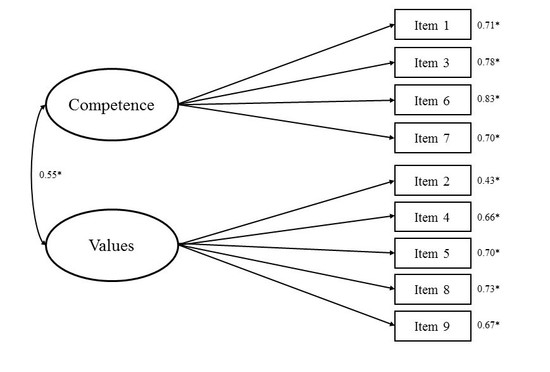
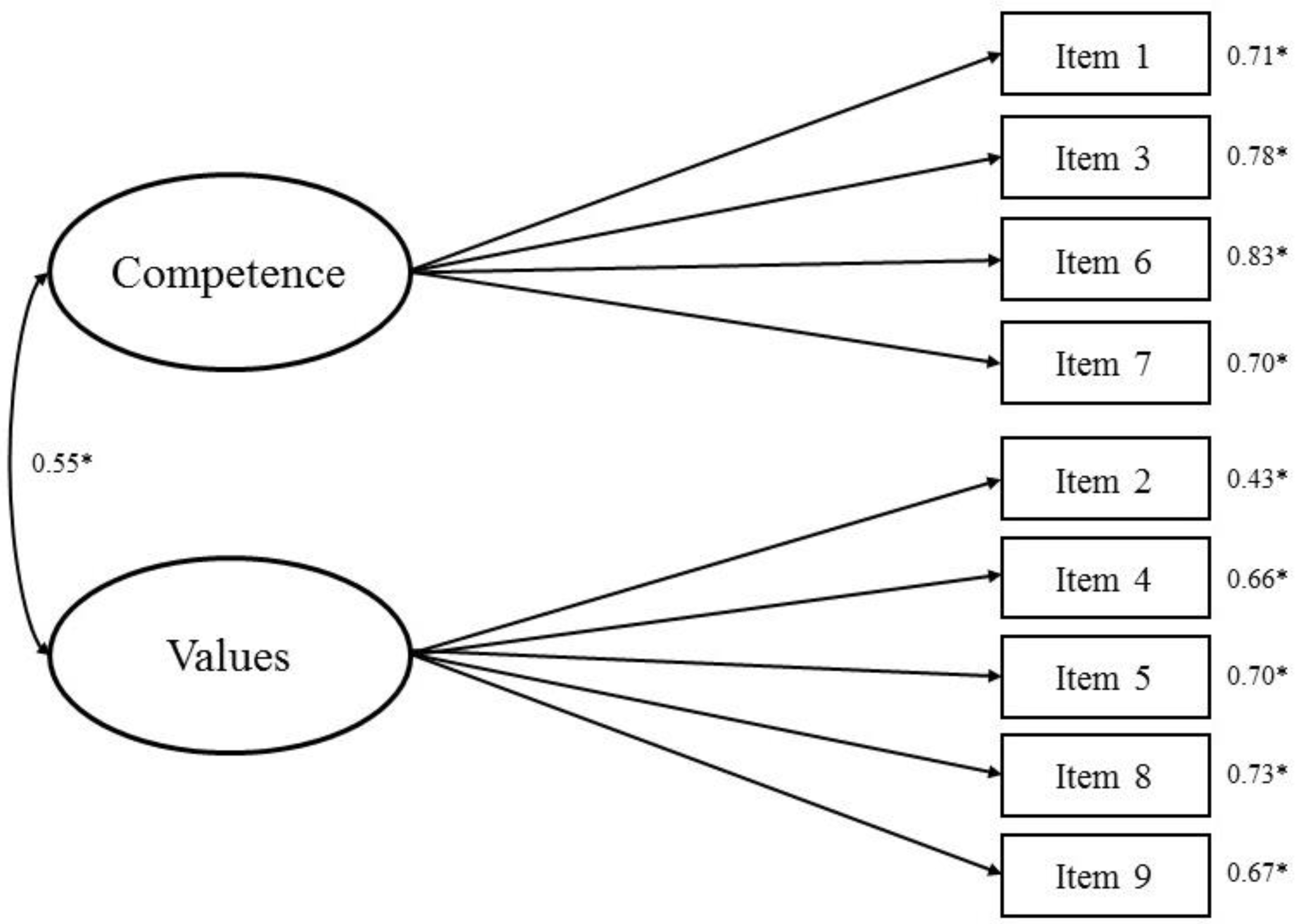
3.4. Reliability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A
References
- Mayer, R.C.; Davis, J.H.; Schoorman, F.D. An integrative model of organizational trust. Acad. Manag. Rev. 1995, 20, 709–734. [Google Scholar] [CrossRef]
- Goold, S.D. Trust, distrust and trustworthiness. J. Gen. Int. Med. 2002, 17, 79–81. [Google Scholar] [CrossRef] [Green Version]
- Hall, M.A.; Dugan, E.; Zheng, B.; Mishra, A.K. Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Q. 2001, 79, 613–639. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, D. Managed care, rationing, and trust in medical care. J. Urban Health 1998, 75, 118–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rose, A.; Peters, N.; Shea, J.A.; Armstrong, K. Development and testing of the health care system distrust scale. J. Gen. Int. Med. 2004, 19, 57–63. [Google Scholar] [CrossRef] [Green Version]
- Halbert, C.H.; Armstrong, K.; Gandy, O.H., Jr.; Shaker, L. Racial differences in trust in health care providers. Arch. Int. Med. 2006, 166, 896–901. [Google Scholar] [CrossRef] [PubMed]
- Boulware, L.E.; Cooper, L.A.; Ratner, L.E.; LaVeist, T.A.; Powe, N.R. Race and trust in the health care system. Public Health Rep. 2003, 118, 358–365. [Google Scholar] [CrossRef]
- Thompson, H.S.; Valdimarsdottir, H.B.; Winkel, G.; Jandorf, L.; Redd, W. The group-based medical mistrust scale: Psychometric properties and association with breast cancer screening. Prev. Med. 2004, 38, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Katapodi, M.C.; Pierce, P.F.; Facione, N.C. Distrust, predisposition to use health services and breast cancer screening: Results from a multicultural community-based survey. Int. J. Nurs. Stud. 2010, 47, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.C.; Matthews, S.A.; Hillemeier, M.M. Effect of health care system distrust on breast and cervical cancer screening in Philadelphia, Pennsylvania. Am. J. Public Health. 2011, 101, 1297–1305. [Google Scholar] [CrossRef] [PubMed]
- Asian Pacific Islander American Health Forum. Demographic and Socioeconomic profiles of Asian Americans, Native Hawaiians, and Pacific Islanders in the United States. 2011. Available online: http://www.apiahf.org/sites/default/files/Demographic_Socioeconomic_Profiles_AANHPI.pdf (accessed on 5 January 2018).
- Heo, H.H.; Braun, K.L. Culturally tailored interventions of chronic disease targeting Korean Americans: A systematic review. Ethn. Health 2014, 19, 64–85. [Google Scholar] [CrossRef] [PubMed]
- The U.S. Bureau of labor Statistics. The Asian Population: 2010. 2012. Available online: https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf (accessed on 5 January 2018).
- Anderson, G.; Jun, M.; Choi, K. Breast cancer screening for Korean women must consider traditional risks as well as two genetic risk factors: Genetic polymorphisms and inheritable gene mutations. Cancer Nurs. 2007, 30, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Ju, E.; Vang, P.D.; Lundquist, M. Breast and cervical cancer screening disparity among Asian American women: Does race/ethnicity matter? J. Women’s Health 2010, 19, 1877–1884. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Hofstetter, C.R.; Irvin, V.L.; Kang, S.; Chhay, D.; Reyes, W.D.; Hovell, M.F. Korean American women’s preventive health care practices: Stratified samples in California, USA. Health Care Women Int. 2012, 33, 422–439. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y. Cultural factors associated with breast and cervical cancer screening in Korean American women in the US: An integrative literature review. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2015, 9, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, K.; Rose, A.; Peters, N.; Long, J.A.; McMurphy, S.; Shea, J.A. Distrust of the health care system and self-reported health in the United States. J. Gen. Int. Med. 2006, 21, 292–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benkert, R.; Hollie, B.; Nordstrom, C.K.; Wickson, B.; Bins-Emerick, L. Trust, mistrust, racial identity and patient satisfaction in urban African American primary care patients of nurse practitioners. J. Nurs. Scholarship 2009, 41, 211–219. [Google Scholar] [CrossRef] [PubMed]
- LaVeist, T.A.; Isaac, L.A.; Williams, K.P. Mistrust of health care organizations is associated with underutilization of health services. Health Serv. Res. 2009, 44, 2093–2105. [Google Scholar] [CrossRef] [PubMed]
- Mohseni, M.; Lindstrom, M. Social capital, trust in the health-care system and self-rated health: The role of access to health care in a population-based study. Soc. Sci. Med. 2007, 64, 1373–1383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shea, J.A.; Micco, E.; Dean, L.T.; McMurphy, S.; Schwartz, J.S.; Armstrong, K. Development of a revised Health Care System Distrust scale. J. Gen. Int. Med. 2008, 23, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.C.; Ferrans, C.E.; Park, C.; Lee, H.; Quinn, L.; Collins, E.G. Effects of perceived discrimination and trust on breast cancer screening among Korean American women. Women’s Health Issues 2018, 28, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Jo, A.M.; Maxwell, A.E.; Yang, B.; Bastani, R. Conducting health research in Korean American churches: Perspectives from church leaders. J. Commun. Health 2010, 35, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Oh, K.M.; Jun, J.; Zhao, X.; Kreps, G.L.; Lee, E.E. Cancer information seeking behaviors of Korean American women: A mixed-methods study using surveys and focus group interviews. J. Health Commun. 2015, 20, 1143–1154. [Google Scholar] [CrossRef] [PubMed]
- Bird, S.T.; Bogart, L.M. Perceived race-based and socioeconomic status(SES)-based discrimination in interactions with health care providers. Ethn. Dis. 2001, 11, 554–563. [Google Scholar] [PubMed]
- Williams, D.R.; Yan, Y.; Jackson, J.S.; Anderson, N.B. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J. Health Psychol. 1997, 2, 335–351. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, K.L.; Harding, A.K.; Lambert, W.E.; Fu, R.; Henderson, W.G. Perceived experiences of discrimination in health care: A barrier for cancer screening among American Indian women with type 2 diabetes. Women’s Health Issues 2013, 23, e61–e67. [Google Scholar] [CrossRef] [PubMed]
- Peek, M.E.; Nunez-Smith, M.; Drum, M.; Lewis, T.T. Adapting the everyday discrimination scale to medical settings: Reliability and validity testing in a sample of African American patients. Ethn. Dis. 2011, 21, 502–509. [Google Scholar] [PubMed]
- Sheppard, V.B.; Wang, J.; Yi, B.; Harrison, T.M.; Feng, S.; Huerta, E.E.; Mandelblatt, J.S. Are health-care relationships important for mammography adherence in Latinas? J. Gen. Int. Med. 2008, 23, 2024–2030. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, K.S.; Park, S.Y.; Shin, J.; Cho, S.; Park, Y. Acculturation, discrimination and depressive symptoms among Korean immigrants in New York City. Community Ment. Health J. 2011, 47, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.A.; Dedrick, R.F. Development of the trust in physician scale: A measure to assess interpersonal trust in patient-physician relationships. Psychol. Rep. 1990, 67, 1091–1100. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.A.; Zhang, M.; Dong, X. Trust in physicians among U.S. Chinese older adults. J. Gerontol. 2014, 69, S46–S53. [Google Scholar] [CrossRef] [PubMed]
- Thom, D.H.; Ribisl, K.M.; Stewart, A.L.; Luke, D.A. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Med. Care 1999, 37, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, R.; Driessnack, M.; Colclough, Y. A committee approach maintaining cultural originality in translation. Appl. Nurs. Res. 2014, 27, 144–146. [Google Scholar] [CrossRef] [PubMed]
- Martinez, G.; Marín, B.V.; Schoua-Glusberg, A. Translating from English to Spanish: The 2002 National Survey of Family Growth. Hisp. J. Behav. Sci. 2006, 28, 531–545. [Google Scholar] [CrossRef]
- Beatty, P. The dynamics of cognitive interviewing. In Methods for Testing and Evaluating Survey Questionnaires; Presser, S., Jennifer, M., Rothgeb, J.M., Couper, M.P., Lessler, J.T., Martin, E., Martin, J., Singer, E., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004; pp. 45–66. [Google Scholar]
- Beatty, P.C.; Willis, G.B. Research synthesis: The practice of cognitive interviewing. Public Opin. Q. 2007, 71, 287–311. [Google Scholar] [CrossRef]
- Willis, G.B.; Royston, P.; Bercini, D. The use of verbal report methods in the development and testing of survey questionnaires. Appl. Cognit. Psychol. 1991, 5, 251–267. [Google Scholar] [CrossRef]
- Kaiser, H.F. A second generation Little Jiffy. Psychometrika 1970, 35, 401–415. [Google Scholar] [CrossRef]
- Dziuban, C.D.; Shirkey, E.C. When is a correlation matrix appropriate for factor analysis? Psychol. Bull. 1974, 81, 358–361. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement errors. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Nunnally, J.C. Psychometric Theory, 2nd ed.; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Polit, D.F.; Beck, C.T. Nursing research: Generating and Assessing Evidence for Nursing Practice, 9th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012. [Google Scholar]
- Armstrong, K.; Putt, M.; Halbert, C.H.; Grande, D.; Schwartz, J.S.; Liao, K.; Marcus, N.; Demeter, M.B.; Shea, J.A. Prior experiences of racial discrimination and racial differences in health care system distrust. Med. Care 2013, 51, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Kreps, G.L.; Shin, C.N. The role of social support and social networks in health information-seeking behavior among Korean Americans: A qualitative study. Int. J. Equity Health 2015, 14, 40. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | n (%) |
|---|---|
| Age (years) | |
| 50–59 | 75 (38.2) |
| 60–69 | 84 (42.9) |
| 70–75 | 37 (18.9) |
| Residency in the United States (years) | |
| 0–9 | 13 (6.6) |
| 10–19 | 34 (17.4) |
| 20–29 | 50 (25.5) |
| 30–39 | 62 (31.6) |
| 40 and above | 37 (18.9) |
| Immigration status | |
| Immigrant (Naturalized) | 156 (79.6) |
| Immigrant (Non-citizen) | 34 (17.4) |
| Immigrant-Undocumented | 3 (1.5) |
| Decline to answer | 3 (1.5) |
| Marital status | |
| Married | 147 (75.0) |
| Not married | 49 (25.0) |
| Employment | |
| Part-time | 27 (13.8) |
| Full-time | 60 (30.6) |
| Not working | 109 (55.6) |
| Education | |
| High school or less | 80 (40.8) |
| College or higher | 116 (59.2) |
| Income (US$) | |
| <10,000 | 18 (9.2) |
| 10,000–24,999 | 28 (14.3) |
| 25,000–39,999 | 44 (22.5) |
| 40,000–54,999 | 22 (11.2) |
| 55,000 or more | 51 (26.0) |
| Do not know | 15 (7.6) |
| Decline to answer | 18 (9.2) |
| Regular doctor | |
| Yes | 166 (84.7) |
| No | 30 (15.3) |
| Physician race | |
| Korean | 173 (88.3) |
| Non-Korean | 23 (11.7) |
| Able to find Korean physician | |
| Yes | 181 (92.4) |
| No | 15 (7.6) |
| Able to receive care where wanted | |
| Yes | 141 (71.9) |
| No | 55 (28.1) |
| Model | χ2 | df | p-Value | RMSEA | SRMR | CFI | TLI |
|---|---|---|---|---|---|---|---|
| HCSD-K | |||||||
| Shea two-factor model | 165.32 | 26 | <0.001 | 0.165 | 0.107 | 0.768 | 0.679 |
| Yang two-factor model | 44.18 | 26 | 0.014 | 0.060 | 0.049 | 0.970 | 0.958 |
| A | A1 | A2 | B | C | |
|---|---|---|---|---|---|
| A. Health care system distrust | — | ||||
| A1. Competence | 0.836 *** | — | |||
| A2. Values | 0.853 *** | 0.427 *** | — | ||
| B. Perceived discrimination in health care | 0.655 *** | 0.523 *** | 0.581 *** | — | |
| C. Trust in physician | −0.728 *** | −0.662 *** | −0.570 *** | −0.671 *** | — |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, H.C.; Min, A. Translation and Validation of the Korean Version of the Revised Health Care System Distrust Scale (HCSD-K) in Korean American Women. Int. J. Environ. Res. Public Health 2018, 15, 1964. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15091964
Hong HC, Min A. Translation and Validation of the Korean Version of the Revised Health Care System Distrust Scale (HCSD-K) in Korean American Women. International Journal of Environmental Research and Public Health. 2018; 15(9):1964. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15091964
Chicago/Turabian StyleHong, Hye Chong, and Ari Min. 2018. "Translation and Validation of the Korean Version of the Revised Health Care System Distrust Scale (HCSD-K) in Korean American Women" International Journal of Environmental Research and Public Health 15, no. 9: 1964. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15091964