Emergency Department Discharge Outcome and Psychiatric Consultation in North African Patients
Abstract
:1. Introduction
2. Methods
2.1. Design
2.1.1. Setting
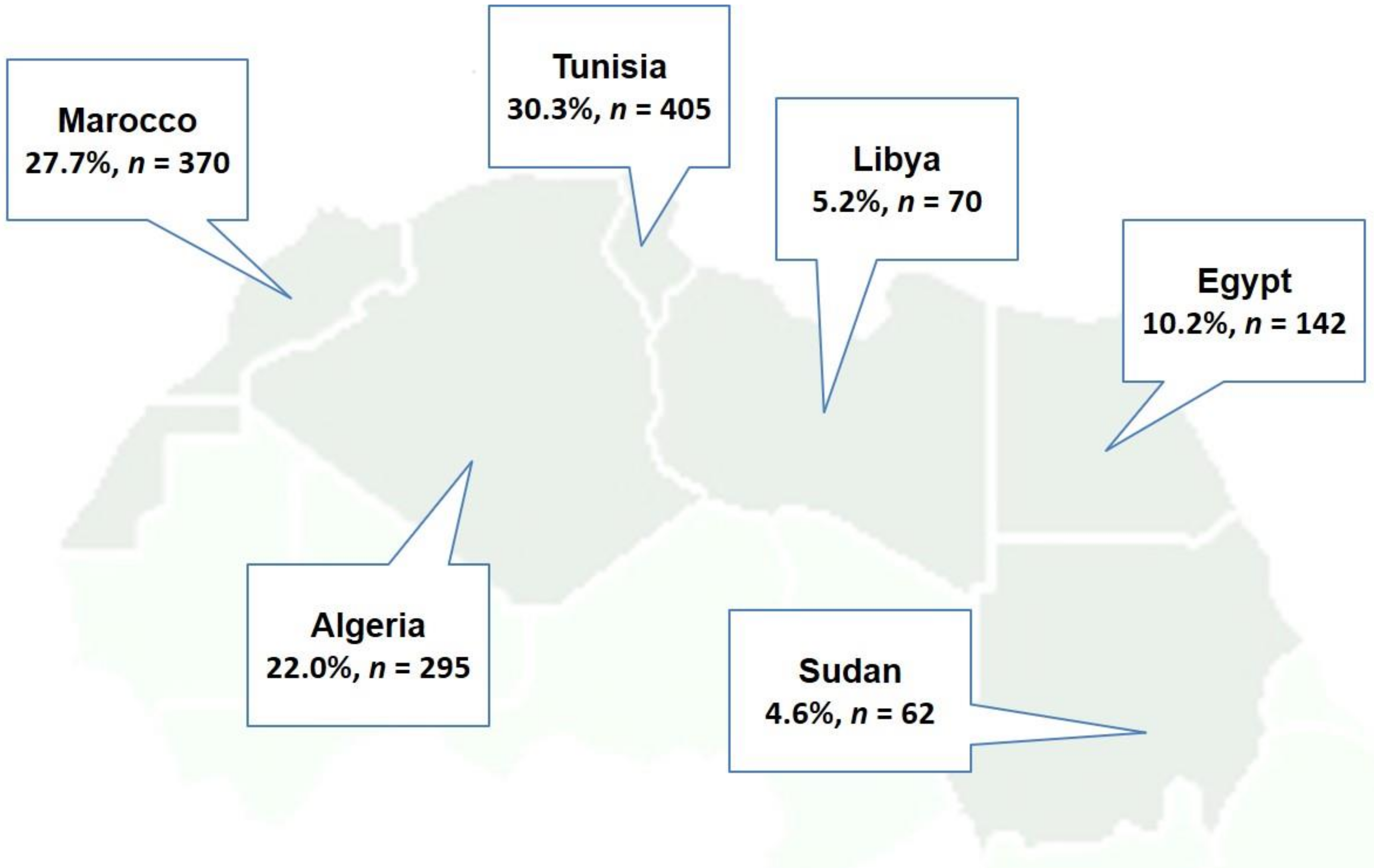
2.1.2. Participants
2.2. Data Collection
Variables
2.3. Statistical Analysis
3. Results
3.1. Comparison between NA and Swiss Origin ED Patients’ Consultations Characteristics
3.2. Predictors of Ambulatory Discharge
3.3. Predictors of Psychiatry Referral
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Approval
Availability of Data and Material
Abbreviations
| ED | Emergency Department |
| HPC | Health care providers |
| NA | North Africa |
| CDC | Non Communicable Disease |
| IPSO | International Psychosocial Organization |
References
- International Organization for Migration (IOM). Who Is a Migrant? Available online: https://www.iom.int/who-is-a-migrant (accessed on 26 July 2018).
- United Nations, Department of Economic and Social Affairs. International Migration Report 2015: Highlights. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=2ahUKEwj2xaTdwLTdAhUSdt4KHRy6ALEQFjAAegQIAhAC&url=http%3A%2F%2Fwww.un.org%2Fen%2Fdevelopment%2Fdesa%2Fpopulation%2Fmigration%2Fpublications%2Fmigrationreport%2Fdocs%2FMigrationReport2015_Highlights.pdf&usg=AOvVaw1CdU51k4MwZnMzi0--XT74 (accessed on 26 July 2018).
- International Organization for Migration (IOM). World Migration Report 2015. Migrants and Cities: New Partnerships to Manage Mobility. Available online: publications.iom.int/system/files/wmr2015_en.pdf (accessed on 26 July 2018).
- Hatton, T.J. Seeking asylum in Europe. Econ.Policy 2004, 19, 6–62. [Google Scholar] [CrossRef]
- Swiss Confederation, Federal Department of Home Affairs. Switzerland Population. Facts and Figures 2016. Available online: www.statistics.admin.ch (accessed on 26 July 2018).
- Swiss Confedaration, Department of Justice. Migration Report 2015. Available online: https://www.sem.admin.ch/dam/data/sem/publiservice/berichte/migration/migrationsbericht-2015-e.pdf (accessed on 26 July 2018).
- Swiss Confedaration, Department of Justice. Migration Report 2016. Available online: https://www.sem.admin.ch/dam/.../migration/migrationsbericht-2016-e.pdf (accessed on 1 September 2018).
- Gadd, M.; Johansson, S.-E.; Sundquist, J.; Wändell, P. Morbidity in cardiovascular diseases in immigrants in Sweden. J. Int. Med. 2003, 254, 236–243. [Google Scholar] [CrossRef] [Green Version]
- Hedlund, E.; Lange, A.; Hammar, N. Acute myocardial infarction incidence in immigrants to Sweden. Country of birth, time since immigration, and time trends over 20 years. Eur. J. Epidemiol. 2007, 22, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Khyatti, M.; Trimbitas, R.-D.; Zouheir, Y.; Benani, A.; Messaoudi, M.-D.E.; Hemminki, K. Infectious diseases in North Africa and North African immigrants to Europe. Eur. J. Public Health 2014, 24, 47–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abebe, D.S.; Lien, L.; Hjelde, K.H. What we know and don’t know about mental health problems among immigrants in Norway. J. Immigr. Minor Health 2014, 16, 60–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Markkula, N.; Lehti, V.; Gissler, M.; Suvisaari, J. Incidence and prevalence of mental disorders among immigrants and native Finns: A register-based study. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 523–1540. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.; Klingberg, K.; Srivastava, D.; Exadaktylos, A.K. Consultations by Asylum Seekers: Recent Trends in the Emergency Department of a Swiss University Hospital. PLoS ONE 2016, 11, e0155423. [Google Scholar] [CrossRef] [PubMed]
- Crede, S.H.; Such, E.; Mason, S. International migrants’ use of emergency departments in Europe compared with non-migrants’ use: A systematic review. Eur. J. Public Health 2018, 28, 61–73. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, I.; Hou, X.Y. Immigrants and the utilization of hospital emergency departments. World J. Emerg. Med. 2012, 3, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Norredam, M.; Mygind, A.; Nielsen, A.S.; Bagger, J.; Krasnik, A. Motivation and relevance of emergency room visits among immigrants and patients of Danish origin. Eur. J. Public Health 2007, 17, 497–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rue, M.; Cabré, X.; Soler-Gonzále, J.; Bosch, A.; Almirall, M.; Serna, M.C. Emergency hospital services utilization in Lleida (Spain): A cross-sectional study of immigrant and Spanish-born populations. BMC Health Serv. Res. 2008, 8, 81. [Google Scholar] [CrossRef] [PubMed]
- Smaland Goth, U.G.; Berg, J.E. Migrant participation in Norwegian health care. A qualitative study using key informants. Eur. J. Gen. Pract. 2011, 17, 28–33. [Google Scholar] [CrossRef]
- Petersen, L.A.; Burstin, H.R.; O’Neil, A.C.; Orav, E.J.; Brennan, T.A. Nonurgent emergency department visits: The effect of having a regular doctor. Med. Care 1998, 36, 1249–1255. [Google Scholar] [CrossRef] [PubMed]
- Gele, A.A.; Pettersen, K.S.; Torheim, L.E.; Kumar, B. Health literacy: The missing link in improving the health of Somali immigrant women in Oslo. BMC Public Health 2016, 16, 1134. [Google Scholar] [CrossRef] [PubMed]
- Bhugra, D. Migration and mental health. Acta Psychiatrca Scand. 2004, 109, 243–258. [Google Scholar] [CrossRef]
- Exadaktylos A, H.W. Emergency medicine in Switzerland. ICU Manag. 2015, 15, 160–162. [Google Scholar]
- Christ, M.; Grossmann, F.; Winter, D.; Bingisser, R.; Platz, E. Modern Triage in the Emergency Department. Dtsch. Arzteblatt Int. 2010, 107, 892–898. [Google Scholar] [CrossRef] [PubMed]
- Swiss Confedaration, Federal Department of Home Affairs, Families, Generations and Society Department. Child and Youth Promotion Act. 2008. Available online: http://www.youthpolicy.org/national/Switzerland_2008_Youth_Policy_Strategy.pdf (accessed on 1 September 2018). (In German)
- Tarraf, W.; Vega, W.; Gonzalez, H.M. Emergency department services use among immigrant and non-immigrant groups in the United States. J. Immigr. Minor Health 2014, 16, 595–606. [Google Scholar] [CrossRef] [PubMed]
- Hacker, K.; Anies, M.; Folb, B.L.; Zallman, L. Barriers to health care for undocumented immigrants: A literature review. Risk Manag. Healthc Policy 2015, 8, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Mantwill, S.; Schulz, P.J. Low health literacy and healthcare utilization among immigrants and non-immigrants in Switzerland. Patient Educ. Couns. 2017, 100, 2020–2027. [Google Scholar] [CrossRef] [PubMed]
- Kreps, G.L.; Sparks, L. Meeting the health literacy needs of immigrant populations. Patient Educ. Couns. 2008, 71, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Yamaguchi, I.; Nutbeam, D.; Kato, M.; Okuhara, T.; Okada, M.; Kiuchi, T. Improving health literacy in a Japanese community population—A pilot study to develop an educational programme. Health Expect 2018. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D.; McGill, B.; Premkumar, P. Improving health literacy in community populations: A review of progress. Health Promot. Int. 2017. [Google Scholar] [CrossRef] [PubMed]
- McCormack, L.; Thomas, V.; Lewis, M.A.; Rudd, R. Improving low health literacy and patient engagement: A social ecological approach. Patient Educ. Couns. 2017, 100, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Silove, D.; Ventevogel, P.; Rees, S. The contemporary refugee crisis: An overview of mental health challenges. World Psychiatry 2017, 16, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Turrini, G.; Purgato, M.; Ballette, F.; Nosè, M.; Ostuzzi, G.; Barbui, C. Common mental disorders in asylum seekers and refugees: Umbrella review of prevalence and intervention studies. Int. J. Ment. Health Syst. 2017, 11, 51. [Google Scholar] [CrossRef] [PubMed]
- Griner, D.; Smith, T.B. Culturally adapted mental health intervention: A meta-analytic review. Psychotherapy 2006, 43, 531–548. [Google Scholar] [CrossRef] [PubMed]
- International Psychosocial Organization (IPSO). Helping People Help Themselves—Refugees for Refugees. Available online: https://ipsocontext.org/ (accessed on 1 September 2018).
- Ayoughi, S.; Missmahl, I.; Weierstall, R.; Elbert, T. Provision of mental health services in resource-poor settings: A randomised trial comparing counselling with routine medical treatment in North Afghanistan (Mazar-e-Sharif). BMC Psychiatry 2012, 12, 14. [Google Scholar] [CrossRef] [PubMed]
- Casillas, A.; Paroz, S.; Green, A.R.; Wolff, H.; Weber, O.; Faucherre, F.; Ninane, F.; Bodenmann, P. Cultural competency of health-care providers in a Swiss University Hospital: Self-assessed cross-cultural skillfulness in a cross-sectional study. BMC Med. Educ. 2014, 14, 19. [Google Scholar] [CrossRef] [PubMed]
- Pelikan, J.M. Health promoting hospitals–Assessing developments in the network. Ital. J. Public Health 2012. [Google Scholar] [CrossRef]
- Swiss Confedaration, Federal Department of Home Affairs. Swiss Hospitals for Equity. Available online: http://www.hospitals4equity.ch/index.php/en/ (accessed on 1 September 2018).
- Bodenmann, P.; Velonaki, V.-S.; Griffin, J.L.; Baggio, S.; Iglesias, K.; Moschetti, K.; Ruggeri, O.; Burnand, B.; Wasserfallen, J.-B.; Vu, F.; et al. Case Management may Reduce Emergency Department Frequent use in a Universal Health Coverage System: A Randomized Controlled Trial. J. Gen. Int. Med. 2017, 32, 508–515. [Google Scholar] [CrossRef] [PubMed]
| NA Nationals | Swiss National | |||
|---|---|---|---|---|
| Total, n (%) | 1338 | 1.1 | 115,521 | 98.9 |
| Gender | ||||
| Male | 996 | 74.4 | 64,250 | 55.6 |
| Female | 342 | 25.6 | 51,271 | 44.4 |
| Reason for admission, n (%) | ||||
| Surgical | 425 | 31.8 | 24,756 | 21.4 |
| Medical | 412 | 30.8 | 30,637 | 26.5 |
| Psychiatric | 102 | 7.6 | 5258 | 4.6 |
| other discipline | 399 | 29.8 | 54,870 | 47.5 |
| Way of admission, n (%) | ||||
| Ambulance | 155 | 11.6 | 19,305 | 16.7 |
| previous medical contact | 55 | 4.1 | 18,104 | 15.7 |
| legal admission | 101 | 7.5 | 946 | 0.8 |
| walk-in | 743 | 55.5 | 48,772 | 42.2 |
| Other | 48 | 3.6 | 4609 | 4.0 |
| Triage, n (%) | ||||
| 1 (life threatening) | 42 | 3.6 | 10,386 | 9.0 |
| 2 (urgent conditions) | 232 | 17.3 | 28,942 | 25.1 |
| 3 (semi-urgent conditions) | 909 | 67.9 | 66,308 | 57.4 |
| 4 (low urgent conditions) | 113 | 8.6 | 7531 | 6.5 |
| 5 (not urgent conditions) | 42 | 3.1 | 2354 | 2.0 |
| ED outcome, n (%) | ||||
| discharge at home | 859 | 64.2 | 54,989 | 47.6 |
| hospital admission | 268 | 20.0 | 41,508 | 35.9 |
| Death | 0 | 0.0 | 222 | 0.2 |
| Not specific | 170 | 12.7 | 17,510 | 15.2 |
| Other | 41 | 3.1 | 1292 | 1.1 |
| Weekend admission, n (%) | 437 | 32.7 | 39,137 | 33.9 |
| Multiple visit, n (%) | 306 | 45.4 | 38,632 | 33.4 |
| Seen by psychiatrist, n (%) | 193 | 14.4 | 8417 | 7.3 |
| Age, med (IQR) | 38.0 | 28–51 | 52.0 | 32–52 |
| Duration in ED (hours), med (IQR) | 3.4 | 2.0–5.4 | 3.6 | 2.2–6.2 |
| Number of visits, med (IQR) | 2.0 | 1.0–4.0 | 2.0 | 1.0–3.0 |
| Age Group | ||||
|---|---|---|---|---|
| Sex | 16–24 | 25–39 | 40–64 | 65–Max |
| Female | 0.89 (95% CI: 0.38–2.06) | 1.45 (95% CI: 0.96–2.19) | 1.56 (95% CI: 1.01–2.39) | 3.31 (95% CI: 0.93–11.76) |
| Male | 0.94 (95% CI: 0.61–1.46) | 1.02 (95% CI: 0.81–1.27) | 1.28 (95% CI: 1.01–1.63) | 1.78 (95% CI: 0.76–4.14) |
| Age Group | ||||
|---|---|---|---|---|
| Sex | 16–24 | 25–39 | 40–64 | 65–Max |
| Female | 1.25 (95% CI: 0.48–3.24) | 0.51 (95% CI: 0.27–0.94) | 0.68 (95% CI: 0.36–1.3) | 2.81 (95% CI: 0.37–21.64) |
| Male | 3.45 (95% CI: 2.22–5.38) | 1.95 (95% CI: 1.53–2.49) | 1.94 (95% CI: 1.44–2.61) | 2.98 (95% CI: 0.7–12.68) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keidar, O.; Jegerlehner, S.N.; Ziegenhorn, S.; Brown, A.D.; Müller, M.; Exadaktylos, A.K.; Srivastava, D.S. Emergency Department Discharge Outcome and Psychiatric Consultation in North African Patients. Int. J. Environ. Res. Public Health 2018, 15, 2033. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15092033
Keidar O, Jegerlehner SN, Ziegenhorn S, Brown AD, Müller M, Exadaktylos AK, Srivastava DS. Emergency Department Discharge Outcome and Psychiatric Consultation in North African Patients. International Journal of Environmental Research and Public Health. 2018; 15(9):2033. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15092033
Chicago/Turabian StyleKeidar, Osnat, Sabrina N. Jegerlehner, Stephan Ziegenhorn, Adam D. Brown, Martin Müller, Aristomenis K. Exadaktylos, and David S. Srivastava. 2018. "Emergency Department Discharge Outcome and Psychiatric Consultation in North African Patients" International Journal of Environmental Research and Public Health 15, no. 9: 2033. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15092033






