Assessing Students’ Knowledge on WASH-Related Diseases
Abstract
:1. Introduction
2. Methods
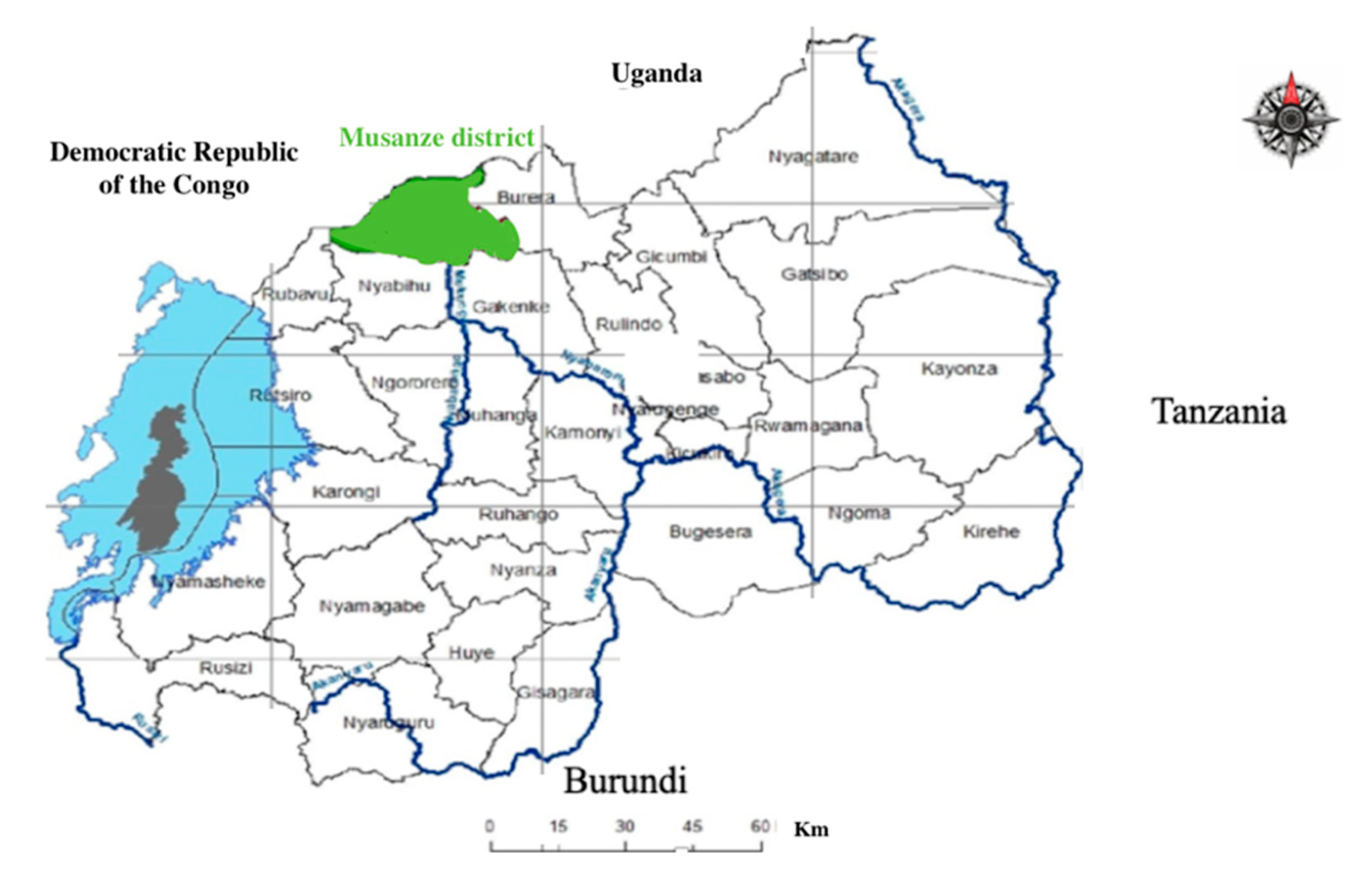
2.1. Study Area
2.2. Sample Size
2.3. Gender and Location
3. Results and Discussion
3.1. Type of Human Waste Disposal Used by Students
3.2. Knowledge on Diseases Caused by Contact with Human Faeces
3.3. Knowledge on Selected WASH-Related Diseases
3.3.1. Causes
3.3.2. Prevention
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- UNICEF. About WASH. Available online: https://www.unicef.org/wash/3942_3952.html (accessed on 22 May 2019).
- Sack, R.B. Human diarrheal disease caused by enterotoxigenic Escherichia coli. Annu. Rev. Microbiol. 1975, 29, 333–353. [Google Scholar] [CrossRef]
- Bryce, J.; Boschi-Pinto, C.; Shibuya, K.; Black, R.E. The Child Health Epidemiology Reference Group WHO estimates of the causes of death in children. Lancet 2005, 365, 1147–1152. [Google Scholar] [CrossRef]
- Nicole, W. The WASH Approach: Fighting Waterborne Diseases in Emergency Situations. Environ. Health Perspect. 2015. [Google Scholar] [CrossRef]
- World Health Organization. Water-Related Diseases. Available online: https://www.who.int/water_sanitation_health/diseases-risks/diseases/diseasefact/en/ (accessed on 22 May 2019).
- Saeed, A.; Abd, H.; Sandstorm, G. Microbial aetiology of acute diarrhoea in children under five years of age in Khartoum, Sudan. J. Med. Microbiol. 2015, 64, 432–437. [Google Scholar] [CrossRef]
- CIDRAP. Studies: Diarrheal Disease Rates Vary across Africa, World. Center for Infectious Disease Research and Policy, University of Minnesota: Minneapolis, MN, USA. Available online: http://www.cidrap.umn.edu/news-perspective/2018/09/studies-diarrheal-disease-rates-vary-across-africa-world (accessed on 5 June 2019).
- Mayo Clink. Cholera. Available online: https://www.mayoclinic.org/diseases-conditions/cholera/symptoms-causes/syc-20355287 (accessed on 5 June 2019).
- Gaffga, N.H.; Tauxe, R.V.; Mintz, E.D. Cholera: A new homeland in Africa? Extern. Am. J. Trop. Med. Hyg. 2007, 77, 705–713. [Google Scholar] [CrossRef]
- Boyd, K.; Jimenez, M.E. What is Trachoma. American Academy of Ophthalmology 2019, San Francisco, USA. Available online: https://www.aao.org/eye-health/diseases/what-is-trachoma (accessed on 22 May 2019).
- Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED). Shigella—Shigellosis. 2018. Available online: https://www.cdc.gov/shigella/index.html (accessed on 22 May 2019).
- Bowen, A. Infectious Diseases Related to Travel. Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED), 2017. Available online: https://wwwnc.cdc.gov/travel/yellowbook/2018/infectious-diseases-related-to-travel/shigellosis (accessed on 22 May 2019).
- WHO. Typhoid. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/typhoid (accessed on 23 May 2019).
- Di Gennaro, F.; Marotta, C.; Pizzol, D.; Chhaganlal, K.; Monno, L.; Putoto, G.; Saracino, A.; Casuccio, A.; Mazzucco, W. Prevalence and Predictors of Malaria in Human Immunodeficiency Virus Infected Patients in Beira, Mozambique. Int. J. Environ. Res. Public Health 2018, 15, 2032. [Google Scholar] [CrossRef]
- Idemyor, V. Human immunodeficiency virus (HIV) and malaria interaction in sub-Saharan Africa: The collision of two Titans. HIV Clin. Trials 2007, 8, 246–253. [Google Scholar] [CrossRef]
- Murray, C.J.; Rosenfeld, L.C.; Lim, S.S.; Andrews, K.G.; Foreman, K.J.; Haring, D.; Fullman, N.; Naghavi, M.; Lozano, R.; Lopez, A.D. Global Malaria mortality between 1980 and 2010: A systematic analysis. Lancet 2012, 379, 413–431. [Google Scholar] [CrossRef]
- Australian Water Association. WASH Fact Sheet. NSW, Australia. Available online: https://www.awa.asn.au/AWA_MBRR/Publications/Fact_Sheets/WASH_Fact_Sheet.aspx (accessed on 5 June 2019).
- Yaya, S.; Hudani, A.; Udenigwe, O.; Shah, V.; Ekholuenetale, M.; Bishwajit, G. Improving Water, Sanitation and Hygiene Practices, and Housing Quality to Prevent Diarrhea among Under-Five Children in Nigeria. Trop. Med. Infect. Dis. 2018, 3, 41. [Google Scholar] [CrossRef] [PubMed]
- UNICEF for Every Child. Water, Sanitation and Hygiene. Available online: https://www.unicef.org/wash/index_wes_related.html (accessed on 5 June 2019).
- United Nations. Goal 6: Ensure Access to Water and Sanitation for All. 2017. Available online: https://www.un.org/sustainabledevelopment/water-and-sanitation/ (accessed on 22 May 2019).
- Kazora, A.S.; Mourad, K.A. Assessing the Sustainability of Decentralized Wastewater Treatment Systems in Rwanda. Sustainability 2018, 10, 4617. [Google Scholar] [CrossRef]
- Tsinda, A.; Pamela, A.; Steve, P.; Katrina, C.; Jane, A.; Kenan, O.; Jonathan, C. Challenges to Achieving Sustainable Sanitation in Informal Settlements of Kigali, Rwanda. Int. J. Environ. Res. Public Health 2013, 10, 6939–6954. [Google Scholar] [CrossRef]
- The United Nations in Rwanda. Social Protection, Water Sanitation and Hygiene. Available online: http://www.rw.one.un.org/what-we-do/human-development/social-protection-water-sanitation-and-hygiene (accessed on 23 May 2019).
- Niyitegeka, T. Rubavu Puts Up Camp for Cholera Patients. 2016. Available online: http://en.igihe.com/news/rubavu-puts-up-camp-for-cholera-patients.html (accessed on 23 May 2019).
- Mukaneza, M.A.; Mukwaya, O. Impunzi Umunani Zaturutse Muri RDC Zagaragayeho Cholera. 2017. Available online: https://www.igihe.com/amakuru/u-rwanda/article/rubavu-impunzi-umunani-zaturutse-muri-rdc-zagaragayeho-cholera (accessed on 23 May 2019).
- RBC. Rwanda Biomedical Center, Annual Reports. Available online: http://www.rbc.gov.rw/index.php?id=283 (accessed on 23 May 2019).
- Nyamusore, J. Cholera Outbreak Inventory, Seasonality and Risk Factors. Epidemic Surveillance and Response, 2015. Available online: http://www.rbc.gov.rw/fileadmin/user_upload/cholera_outbreak_inventory_and_seasonality_august_2015-2.pdf (accessed on 23 May 2019).
- Republic of Rwanda—Ministry of Local Government. Available online: http://minaloc.gov.rw/index.php?id=492 (accessed on 23 May 2019).
- Maniriho, A.; Bizoza, A.R. Financial Benefit-Cost Analysis of Agricultural Production in Musanze District, Rwanda. Acad. Arena 2013, 5, 30–39. [Google Scholar]
- Repubulika y’u Rwanda Intara y’Amajyaruguru Akarere ka Musanze. Available online: https://musanze.gov.rw/index.php?id=83 (accessed on 23 May 2019).
- Krejcie, R.V.; Morgan, D.W. Determining Sample Size for Research Activities. Educ. Psychol. Meas. 1970, 30, 607–610. [Google Scholar] [CrossRef]
- Chuan, C.L.; Penyelidikan, J. Sample Size Estimation Using Krejcie and Morgan and Cohen Statistical Power Analysis: A Comparison. Available online: http://www.ipbl.edu.my/portal/penyelidikan/jurnalpapers/jurnal2006/chua06.pdf (accessed on 22 May 2019).
- Battikhi, M.N. Bloody diarrhoea cases caused by Shigella and amoeba in Jordan. New Microbiol. 2004, 27, 37–47. [Google Scholar]
- Clover, J. UNICEF’s Child-Friendly Schools Initiative Aims to Improve Sanitation Facilities in Rwandan Schools. 2011. Available online: https://www.unicef.org/adolescence/rwanda_60191.html (accessed on 23 May 2019).
| Name of School | Location of School | Population Size | Sample Size |
|---|---|---|---|
| Esc. Musanze | Urban | 208 | 136 |
| GS 1. Muhoza II | Urban | 695 | 248 |
| ESSA Ruhengeri | Urban | 140 | 103 |
| GS. Nyange | Rural | 570 | 226 |
| GS. Kampanga | Rural | 912 | 269 |
| GS. Gakoro | Rural | 375 | 191 |
| Total | 2900 | 1173 |
| Gender | Total | ||||
|---|---|---|---|---|---|
| Female | Male | ||||
| Location of school | Rural | Count | 383 | 303 | 686 |
| % | 55.8% | 44.2% | 100% | ||
| Urban | Count | 281 | 206 | 487 | |
| % | 57.7% | 42.3% | 100% | ||
| Total | Count | 664 | 509 | 1173 | |
| % | 56.6% | 43.4% | 100% | ||
| Cholera | Diarrhoea | Dysentery | Malaria | No Answer | Shigellosis | Typhoid | Total | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Location of school | Rural | Count | 417 | 161 | 13 | 0 | 84 | 1 | 10 | 686 |
| % | 60.8% | 23.5% | 1.9% | 0.0% | 12.2% | 0.1% | 1.5% | 100% | ||
| Urban | Count | 251 | 150 | 13 | 3 | 35 | 0 | 35 | 487 | |
| % | 51.5% | 30.8% | 2.7% | 0.6% | 7.2% | 0.0% | 7.2% | 100% | ||
| Total | Count | 668 | 311 | 26 | 3 | 119 | 1 | 45 | 1173 | |
| % | 56.9% | 26.5% | 2.2% | 0.3% | 10.1% | 0.1% | 3.8% | 100% | ||
| Cholera | Diarrhoea | Malaria | No Knowledge | Shigellosis | Trachoma | Typhoid | Total | ||
|---|---|---|---|---|---|---|---|---|---|
| Rural | Count | 86 | 224 | 290 | 74 | 2 | 0 | 10 | 686 |
| % | 12.5% | 32.7% | 42.3% | 10.8% | 0.3% | 0% | 1.5% | 100% | |
| Urban | Count | 99 | 216 | 21 | 127 | 2 | 1 | 21 | 487 |
| % | 20.3% | 44.4% | 4.3% | 26.1% | 0.4% | 0.2% | 4.3% | 100% | |
| Total | Count | 185 | 440 | 311 | 201 | 4 | 1 | 31 | 1173 |
| % | 15.8% | 37.5% | 26.5% | 17.1% | 0.3% | 0.1% | 2.6% | 100% | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mourad, K.A.; Habumugisha, V.; Sule, B.F. Assessing Students’ Knowledge on WASH-Related Diseases. Int. J. Environ. Res. Public Health 2019, 16, 2052. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16112052
Mourad KA, Habumugisha V, Sule BF. Assessing Students’ Knowledge on WASH-Related Diseases. International Journal of Environmental Research and Public Health. 2019; 16(11):2052. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16112052
Chicago/Turabian StyleMourad, Khaldoon A., Vincent Habumugisha, and Bolaji F. Sule. 2019. "Assessing Students’ Knowledge on WASH-Related Diseases" International Journal of Environmental Research and Public Health 16, no. 11: 2052. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16112052






