Validation of the Short-Form Health Literacy Questionnaire (HLS-SF12) and Its Determinants among People Living in Rural Areas in Vietnam
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Settings
2.2. Sampling and Sample Size
2.3. Health Literacy Assessment
2.4. Personal Characteristics
2.5. Data Collection Procedure
2.6. Ethical Approval
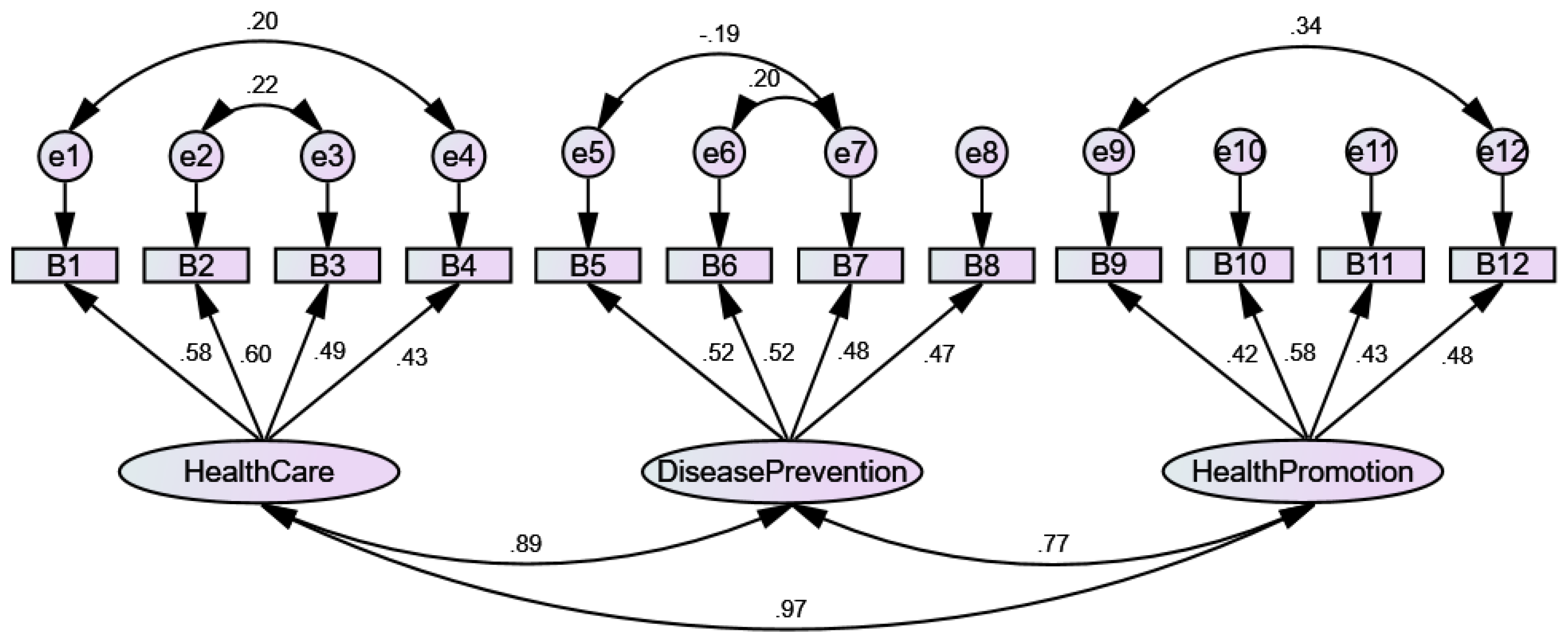
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- United Nations Development Group. Transforming our world: The 2030 Agenda for Sustainable Development. United Nations, 2015. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication (accessed on 31 December 2015).
- Wagner, D.A. Learning, Literacy and Sustainable Development: Inclusion, Vulnerability and the SDGs. In Children and Sustainable Development: Ecological Education in a Globalized World; Battro, A.M., Léna, P., Sánchez Sorondo, M., Von Braun, J., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 45–65. [Google Scholar]
- Rowlands, G.; Dodson, S.; Leung, A.; Levin-Zamir, D. Global health systems and policy development: Implications for health literacy research, theory and practice. Stud. Health Technol. Inform. 2017, 240, 359–391. [Google Scholar]
- Sørensen, K.; Van den Broucke, S.; Brand, H.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonszka, Z. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Nhung, N.T.T.; Long, T.K.; Linh, B.N.; Vos, T.; Huong, N.T.; Anh, N.D. Estimation of Vietnam national burden of disease 2008. Asia Pac. J. Public Health 2014, 26, 527–535. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global burden of disease study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Nugent, R.; Bertram, M.Y.; Jan, S.; Niessen, L.W.; Sassi, F.; Jamison, D.T.; Pier, E.G.; Beaglehole, R. Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. Lancet 2018, 391, 2029–2035. [Google Scholar] [CrossRef]
- Niessen, L.W.; Mohan, D.; Akuoku, J.K.; Mirelman, A.J.; Ahmed, S.; Koehlmoos, T.P.; Trujillo, A.; Khan, J.; Peters, D.H. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet 2018, 391, 2036–2046. [Google Scholar] [CrossRef] [Green Version]
- Son, P.T.; Quang, N.N.; Viet, N.L.; Khai, P.G.; Wall, S.; Weinehall, L.; Bonita, R.; Byass, P. Prevalence, awareness, treatment and control of hypertension in Vietnam—Results from a national survey. J. Hum. Hypertens. 2012, 26, 268. [Google Scholar] [CrossRef]
- Nguyen, Q.N.; Pham, S.T.; Nguyen, V.L.; Weinehall, L.; Bonita, R.; Byass, P.; Wall, S. Time Trends in blood pressure, body mass index and smoking in the Vietnamese population: A meta-analysis from multiple cross-sectional surveys. PLoS ONE 2012, 7, e42825. [Google Scholar] [CrossRef]
- The World Bank. Country Profile: Vietnam; World Bank Group: Washington, DC, USA, 2018; Available online: https://data.worldbank.org/country/vietnam (accessed on 8 August 2019).
- Hoa, N.P.; Rao, C.; Hoy, D.G.; Hinh, N.D.; Chuc, N.T.K.; Ngo, D.A. Mortality measures from sample-based surveillance: Evidence of the epidemiological transition in Viet Nam. Bull. World Health Organ. 2012, 90, 764–772. [Google Scholar]
- Meiqari, L.; Nguyen, T.-P.-L.; Essink, D.; Zweekhorst, M.; Wright, P.; Scheele, F. Access to hypertension care and services in primary health-care settings in Vietnam: A systematic narrative review of existing literature. Glob. Health Action 2019, 12, 1610253. [Google Scholar] [CrossRef]
- Nguyen, T.-P.-L.; Schuiling-Veninga, C.C.M.; Nguyen, T.B.Y.; Vu, T.-H.; Wright, E.P.; Postma, M.J. Adherence to hypertension medication: Quantitative and qualitative investigations in a rural Northern Vietnamese community. PLoS ONE 2017, 12, e0171203. [Google Scholar] [CrossRef]
- Meiqari, L.; Essink, D.; Wright, P.; Scheele, F. Prevalence of hypertension in Vietnam: A systematic review and meta-analysis. Asia Pac. J. Public Health 2019, 31, 101–112. [Google Scholar] [CrossRef]
- Hien, H.A.; Tam, N.M.; Tam, V.; Derese, A.; Devroey, D. Prevalence, Awareness, Treatment, and Control of Hypertension and Its Risk Factors in (Central) Vietnam. Int. J. Hypertens. 2018, 2018, 12. [Google Scholar] [CrossRef]
- Guntzviller, L.M.; King, A.J.; Jensen, J.D.; Davis, L.A. Self-efficacy, health literacy, and nutrition and exercise behaviors in a low-income, Hispanic population. J. Immigr. Minor. Health 2016, 19, 489–493. [Google Scholar] [CrossRef]
- Yokokawa, H.; Fukuda, H.; Yuasa, M.; Sanada, H.; Hisaoka, T.; Naito, T. Association between health literacy and metabolic syndrome or healthy lifestyle characteristics among community-dwelling Japanese people. Diabetol. Metab. Syndr. 2016, 8, 30. [Google Scholar] [CrossRef]
- Duong, T.V.; Sørensen, K.; Pelikan, J.; Van den Broucke, S.; Lin, I.F.; Lin, Y.-C.; Huang, H.-L.; Chang, P.W. Health-related behaviors moderate the association between age and self-reported health literacy among Taiwanese women. Women Health 2017, 58, 632–646. [Google Scholar] [CrossRef]
- Mackert, M. Introduction to a colloquium: Challenges and opportunities in advancing health literacy research. Health Commun. 2015, 30, 1159–1160. [Google Scholar] [CrossRef]
- Pelikan, J.M.; Ganahl, K.; Roethlin, F. Health literacy as a determinant, mediator and/or moderator of health: empirical models using the European Health Literacy Survey dataset. Glob. Health Promot. 2018, 25, 57–66. [Google Scholar] [CrossRef]
- Truman, E.; Bischoff, M.; Elliott, C. Which literacy for health promotion: Health, food, nutrition or media? Health Promot. Int. 2019. [Epub ahead of print]. [Google Scholar] [CrossRef]
- İlgün, G.; Turaç, İ.S.; Orak, S. Health literacy. Procedia Soc. Behav. Sci. 2015, 174, 2629–2633. [Google Scholar] [CrossRef]
- Mackey, L.M.; Doody, C.; Werner, E.L.; Fullen, B. Self-management skills in chronic disease management: What role does health literacy have? Med. Decis. Mak. 2016, 36, 741–759. [Google Scholar] [CrossRef]
- Rasu, R.S.; Bawa, W.A.; Suminski, R.; Snella, K.; Warady, B. Health literacy impact on national healthcare utilization and expenditure. Int. J. Health Policy Manag. 2015, 4, 747–755. [Google Scholar] [CrossRef]
- Haun, J.N.; Patel, N.R.; French, D.D.; Campbell, R.R.; Bradham, D.D.; Lapcevic, W.A. Association between health literacy and medical care costs in an integrated healthcare system: A regional population based study. BMC Health Serv. Res. 2015, 15, 249. [Google Scholar] [CrossRef]
- Wang, C.; Lang, J.; Xuan, L.; Li, X.; Zhang, L. The effect of health literacy and self-management efficacy on the health-related quality of life of hypertensive patients in a western rural area of China: a cross-sectional study. Int. J. Equity Health 2017, 16, 58. [Google Scholar] [CrossRef]
- Moser, D.K.; Robinson, S.; Biddle, M.J.; Pelter, M.M.; Nesbitt, T.S.; Southard, J.; Cooper, L.; Dracup, K. Health literacy predicts morbidity and mortality in rural patients with heart failure. J. Card. Fail. 2015, 21, 612–618. [Google Scholar] [CrossRef]
- Duong, T.V.; Aringazina, A.; Baisunova, G.; Nurjanah; Pham, T.V.; Pham, K.M.; Truong, T.Q.; Nguyen, K.T.; Oo, W.M.; Mohamad, E.; et al. Measuring health literacy in Asia: Validation of the HLS-EU-Q47 survey tool in six Asian countries. J. Epidemiol. 2017, 27, 80–86. [Google Scholar] [CrossRef]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef]
- Nakayama, K.; Osaka, W.; Togari, T.; Ishikawa, H.; Yonekura, Y.; Sekido, A.; Matsumoto, M. Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy. BMC Public Health 2015, 15, 505. [Google Scholar] [CrossRef]
- Duong, T.V.; Aringazina, A.; Baisunova, G.; Nurjanah, N.; Pham, T.V.; Pham, K.M.; Truong, T.Q.; Nguyen, K.T.; Oo, W.M.; Su, T.T.; et al. Development and validation of a new short-form health literacy instrument (HLS-SF12) for the general public in six Asian countries. Health Lit. Res. Pract. 2019, 3, e91–e102. [Google Scholar] [CrossRef]
- Li, X.; Ning, N.; Hao, Y.; Sun, H.; Gao, L.; Jiao, M.; Wu, Q.; Quan, H. Health literacy in rural areas of China: Hypertension knowledge survey. Int. J. Environ. Res. Public Health 2013, 10, 1125–1138. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practices of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Pourhoseingholi, M.A.; Vahedi, M.; Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol. Hepatol. Bed Bench 2013, 6, 14–17. [Google Scholar]
- HLS-EU Consortium. Comparative Report of Health Literacy in Eight EU Member States. The European Health Literacy Project 2009–2012; Maastricht University: Maastricht, The Netherlands, 2012; Available online: https://www.healthliteracyeurope.net/hls-eu (accessed on 22 October 2012).
- Kline, R.B. Exploratory and confirmatory factor analysis. In Applied Quantitative Analysis in the Social Sciences; Routledge: New York, NY, USA, 2013; pp. 171–207. [Google Scholar]
- Hays, R.D.; Hayashi, T. Beyond internal consistency reliability: Rationale and user’s guide for multitrait analysis program on the microcomputer. Behav. Res. Methods Instr. Comput. 1990, 22, 167–175. [Google Scholar] [CrossRef]
- Cronbach, L.J.; Shavelson, R.J. My current thoughts on coefficient alpha and successor procedures. Educ. Psychol. Meas. 2004, 64, 391–418. [Google Scholar] [CrossRef]
- Hays, R.D.; Anderson, R.T.; Revicki, D. Assessing reliability and validity of measurement in clinical trials. In Quality of Life Assessment in Clinical Trials: Methods and Practice; Oxford University Press: New York, NY, USA, 1998; pp. 169–182. [Google Scholar]
- Tsai, T.-I.; Lee, S.-Y.D.; Tsai, Y.-W.; Kuo, K.N. Methodology and Validation of health literacy scale development in Taiwan. J. Health. Commun. 2010, 16, 50–61. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [Green Version]
- IBM SPSS. IBM SPSS Statistics for Windows, Version 20.0.; IBM Corp: New York, NY, USA, 2011. [Google Scholar]
- Floyd, F.J.; Widaman, K.F. Factor analysis in the development and refinement of clinical assessment instruments. Psychol. Assess. 1995, 7, 286–299. [Google Scholar] [CrossRef]
- Taylor, R. Interpretation of the correlation coefficient: A basic review. J. Diagn. Med. Sonogr. 1990, 6, 35–39. [Google Scholar] [CrossRef]
- Duong, T.V.; Lin, I.-F.; Sørensen, K.; Pelikan, J.M.; Van den Broucke, S.; Lin, Y.-C.; Chang, P.W. Health literacy in Taiwan: A population-based study. Asia Pac. J. Public Health 2015, 27, 871–880. [Google Scholar] [CrossRef]
- Van der Heide, I.; Rademakers, J.; Schipper, M.; Droomers, M.; Sørensen, K.; Uiters, E. Health literacy of Dutch adults: A cross sectional survey. BMC Public Health 2013, 13, 1–11. [Google Scholar] [CrossRef]
- Paasche-Orlow, M.K.; Parker, R.M.; Gazmararian, J.A.; Nielsen-Bohlman, L.T.; Rudd, R.R. The prevalence of limited health literacy. J. Gen. Intern. Med. 2005, 20, 175–184. [Google Scholar] [CrossRef]
- Rudd, R.E. Health literacy skills of US adults. Am. J. Health Behav. 2007, 31, S8–S18. [Google Scholar] [CrossRef]
- Rootman, I.; Gordon-El-Bihbety, D. A Vision for a Health Literate Canada: Report of the Expert Panel on Health Literacy; Canadian Public Health Association: Ottawa, ON, Canada, 2008; Available online: https://www.cpha.ca/vision-health-literate-canada-report-expert-panel-health-literacy (accessed on 16 June 2017).
- Liu, Y.-B.; Liu, L.; Li, Y.-F.; Chen, Y.-L. Relationship between health literacy, health-related behaviors and health status: A survey of elderly Chinese. Int. J. Environ. Res. Public Health 2015, 12, 9714–9725. [Google Scholar] [CrossRef]
- Kayupova, G.; Turdaliyeva, B.; Tulerayev, K.; Duong, T.V.; Chang, P.W.; Zagulova, D. Health literacy among visitors of district polyclinics in Almaty, Kazakhstan. Iran. J. Public Health 2017, 46, 1062–1070. [Google Scholar]
- Van der Gaag, M.; van der Heide, I.; Spreeuwenberg, P.M.M.; Brabers, A.E.M.; Rademakers, J.J.D.J.M. Health literacy and primary health care use of ethnic minorities in the Netherlands. BMC Health Serv. Res. 2017, 17, 350. [Google Scholar] [CrossRef]
- United Nations. The Sustainable Development Goals Report 2019; United Nations Statistics Division: New York, NY, USA, 2019; Available online: https://unstats.un.org/sdgs/report/2019/The-Sustainable-Development-Goals-Report-2019.pdf (accessed on 30 June 2019).
| Total (N = 440) | GHL Index | ||
|---|---|---|---|
| Frequency (%) | Mean ± SD | p-Value 1 | |
| Age | 0.007 | ||
| 18–39 | 223 (50.7) | 25.0 ± 9.0 | |
| 40–59 | 179 (40.7) | 24.1 ± 8.6 | |
| ≥60 | 38 (8.6) | 20.1 ± 10.1 | |
| Gender | <0.001 | ||
| Women | 248 (56.4) | 22.5 ± 9.3 | |
| Men | 192 (43.6) | 26.4 ± 8.2 | |
| Ethnicity attainment | 0.376 | ||
| Kinh (Vietnamese) | 62 (14.1) | 23.3 ± 9.5 | |
| Ethnic minority | 378 (85.9) | 24.4 ± 8.9 | |
| Marital status | <0.001 | ||
| Never married | 54 (12.3) | 31.7 ± 8.2 | |
| Married | 386 (87.7) | 23.2 ± 8.6 | |
| Education | 0.004 | ||
| Illiterate | 84 (19.1) | 17.2 ± 8.8 | |
| Elementary School | 102 (23.2) | 20.9 ± 8.7 | |
| Secondary School | 128 (29.1) | 26.1 ± 7.1 | |
| High School | 102 (23.2) | 29.0 ± 7.1 | |
| Vocational/University | 24 (5.5) | 32.6 ± 5.4 | |
| Occupation | 0.002 | ||
| Agroforestry | 342 (77.7) | 23.5 ± 8.8 | |
| Others (Officers/Small trade/Craft/Housework) | 98 (22.3) | 26.7 ± 9.3 | |
| Ability to pay for medication | <0.001 | ||
| Very difficult | 143 (32.5) | 19.2 ± 8.4 | |
| Fairly difficult | 178 (40.5) | 24.8 ± 8.2 | |
| Fairly easy | 87 (19.8) | 28.9 ± 7.3 | |
| Very easy | 32 (7.3) | 30.7 ± 8.8 | |
| Social status | <0.001 | ||
| Low | 167 (38.1) | 21.5 ± 8.9 | |
| Middle or High | 271 (61.9) | 26.0 ± 8.7 | |
| Tendency to view health-related TV/radio | <0.001 | ||
| Never | 67 (15.2) | 19.1 ± 9.8 | |
| Rarely | 110 (25.0) | 25.3 ± 7.3 | |
| Sometimes | 192 (43.6) | 24.9 ± 9.0 | |
| Often | 71 (16.1) | 25.7 ± 9.3 | |
| Community involvement | 0.003 | ||
| Never | 148 (33.6) | 23.2 ± 9.0 | |
| Rarely | 84 (19.1) | 22.3 ± 9.8 | |
| Sometimes | 157 (35.7) | 25.2 ± 8.1 | |
| Often | 51 (11.6) | 27.4 ± 9.6 |
| Total Sample (N = 440) | |
|---|---|
| Absolute model fit 1 | |
| RMSEA | 0.09 |
| GFI | 0.94 |
| Incremental fit 1 | |
| AGFI | 0.89 |
| CFI | 0.85 |
| IFI | 0.86 |
| NFI | 0.82 |
| Parsimonious fit 1 | |
| χ2/df | 4.34 |
| Item-scale convergent validity, range of correlations (rho) | |
| GHL | 0.49–0.64 |
| HC-HL | 0.66–0.74 |
| DP-HL | 0.62–0.73 |
| HP-HL | 0.63–0.73 |
| Reliability, Cronbach’s alpha | |
| GHL | 0.79 |
| HC-HL | 0.65 |
| DP-HL | 0.56 |
| HP-HL | 0.60 |
| Floor effects, % | |
| GHL | 0.50 |
| HC-HL | 7.70 |
| DP-HL | 1.40 |
| HP-HL | 1.80 |
| Ceiling effect, % | |
| GHL | 0.00 |
| HC-HL | 1.40 |
| DP-HL | 1.40 |
| HP-HL | 5.00 |
| Bivariate Model | Multivariate Model | |||
|---|---|---|---|---|
| B (95% CI) | p-Value | B (95% CI) | p-Value | |
| Age | ||||
| 18–39 | Reference | Reference | ||
| 40−59 | −0.92 (−2.68, 0.84) | 0.306 | 0.82 (−0.61, 2.25) | 0.259 |
| ≥60 | −4.98 (−8.06, −1.89) | 0.002 | −2.31 (−4.89, 0.28) | 0.080 |
| Gender | ||||
| Women | Reference | Reference | ||
| Men | 3.90 (2.24, 5.57) | <0.001 | 0.14 (−1.40, 1.67) | 0.860 |
| Ethnicity | ||||
| Kinh (Vietnamese) | Reference | Reference | ||
| Ethnic minority | 1.10 (−1.33, 3.53) | 0.376 | 1.43 (−0.51, 3.37) | 0.148 |
| Marital status | ||||
| Never married | Reference | Reference | ||
| Married | −8.52 (−10.97, −6.07) | <0.001 | −3.12 (−5.69, −0.56) | 0.017 |
| Education attainment | ||||
| Illiterate | Reference | Reference | ||
| Elementary School | 3.73 (1.49, 5.97) | 0.001 | 3.41 (1.33, 5.49) | 0.001 |
| Secondary School | 8.89 (6.76, 11.03) | <0.001 | 7.11 (5.07, 9.15) | <0.001 |
| High School | 11.79 (9.55, 14.03) | <0.001 | 7.64 (5.31, 9.97) | <0.001 |
| Vocational/University | 15.43 (11.91, 18.95) | <0.001 | 10.44 (6.67, 14.22) | <0.001 |
| Occupation | ||||
| Agroforestry | Reference | Reference | ||
| Others (Officers/Small trade/Craft/Housework) | 3.13 (1.12, 5.14) | 0.002 | −1.21 (−3.10, 0.68) | 0.209 |
| Ability to pay for medication | ||||
| Very difficult | Reference | Reference | ||
| Fairly difficult | 5.55 (3.75, 7.34) | <0.001 | 4.17 (2.51, 5.83) | <0.001 |
| Fairly easy | 9.70 (7.53, 11.88) | <0.001 | 5.64 (3.57, 7.72) | <0.001 |
| Very easy | 11.49 (8.36, 14.62) | <0.001 | 9.89 (6.97, 12.80) | <0.001 |
| Social status | ||||
| Low | Reference | Reference | ||
| Middle or High | 4.53 (2.84, 6.22) | <0.001 | 1.37 (−0.13, 2.87) | 0.073 |
| Tendency to view health-related TV/radio | ||||
| Never | Reference | Reference | ||
| Rarely | 6.19 (3.52, 8.87) | <0.001 | 5.23 (2.97, 7.49) | <0.001 |
| Sometimes | 5.75 (3.30, 8.20) | <0.001 | 4.13 (2.10, 6.16) | <0.001 |
| Often | 6.63 (3.69, 9.57) | <0.001 | 6.15 (3.70, 8.60) | <0.001 |
| Community involvement | ||||
| Never | Reference | Reference | ||
| Rarely | −0.91 (−3.30, 1.48) | 0.454 | −0.43 (−2.38, 1.51) | 0.662 |
| Sometimes | 1.99 (−0.02, 3.99) | 0.052 | −0.63 (−2.31, 1.05) | 0.460 |
| Often | 4.21 (1.36, 7.05) | 0.004 | 2.05 (−0.43, 4.53) | 0.105 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duong, T.V.; Nguyen, T.T.P.; Pham, K.M.; Nguyen, K.T.; Giap, M.H.; Tran, T.D.X.; Nguyen, C.X.; Yang, S.-H.; Su, C.-T. Validation of the Short-Form Health Literacy Questionnaire (HLS-SF12) and Its Determinants among People Living in Rural Areas in Vietnam. Int. J. Environ. Res. Public Health 2019, 16, 3346. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16183346
Duong TV, Nguyen TTP, Pham KM, Nguyen KT, Giap MH, Tran TDX, Nguyen CX, Yang S-H, Su C-T. Validation of the Short-Form Health Literacy Questionnaire (HLS-SF12) and Its Determinants among People Living in Rural Areas in Vietnam. International Journal of Environmental Research and Public Health. 2019; 16(18):3346. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16183346
Chicago/Turabian StyleDuong, Tuyen Van, Thao T. P. Nguyen, Khue M. Pham, Kien T. Nguyen, Manh H. Giap, Tung D. X. Tran, Chi X. Nguyen, Shwu-Huey Yang, and Chien-Tien Su. 2019. "Validation of the Short-Form Health Literacy Questionnaire (HLS-SF12) and Its Determinants among People Living in Rural Areas in Vietnam" International Journal of Environmental Research and Public Health 16, no. 18: 3346. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16183346







