The Effectiveness of Laser-Assisted Surgical Excision of Leukoplakias and Hyperkeratosis of Oral Mucosa: A Case Series in A Group of Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
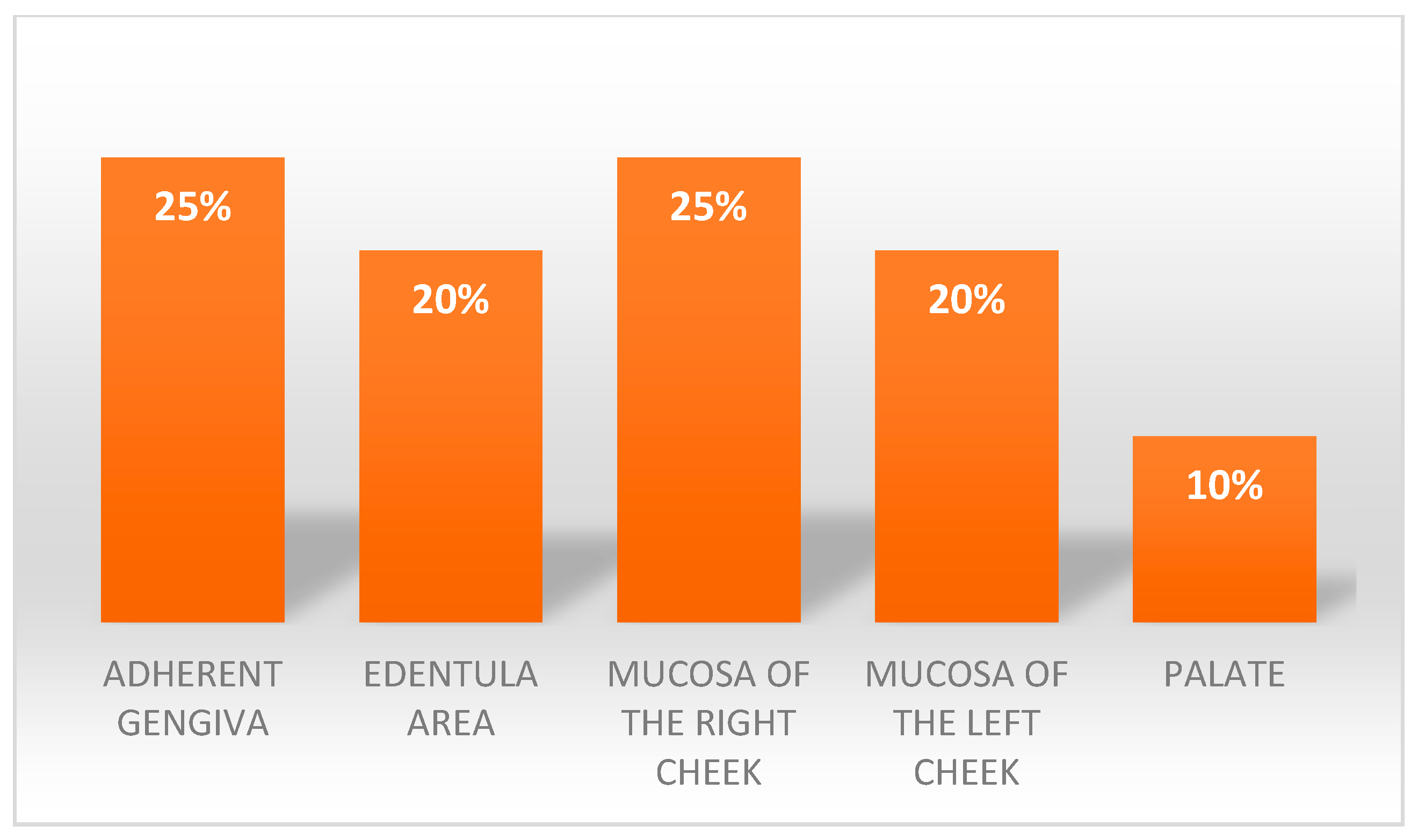
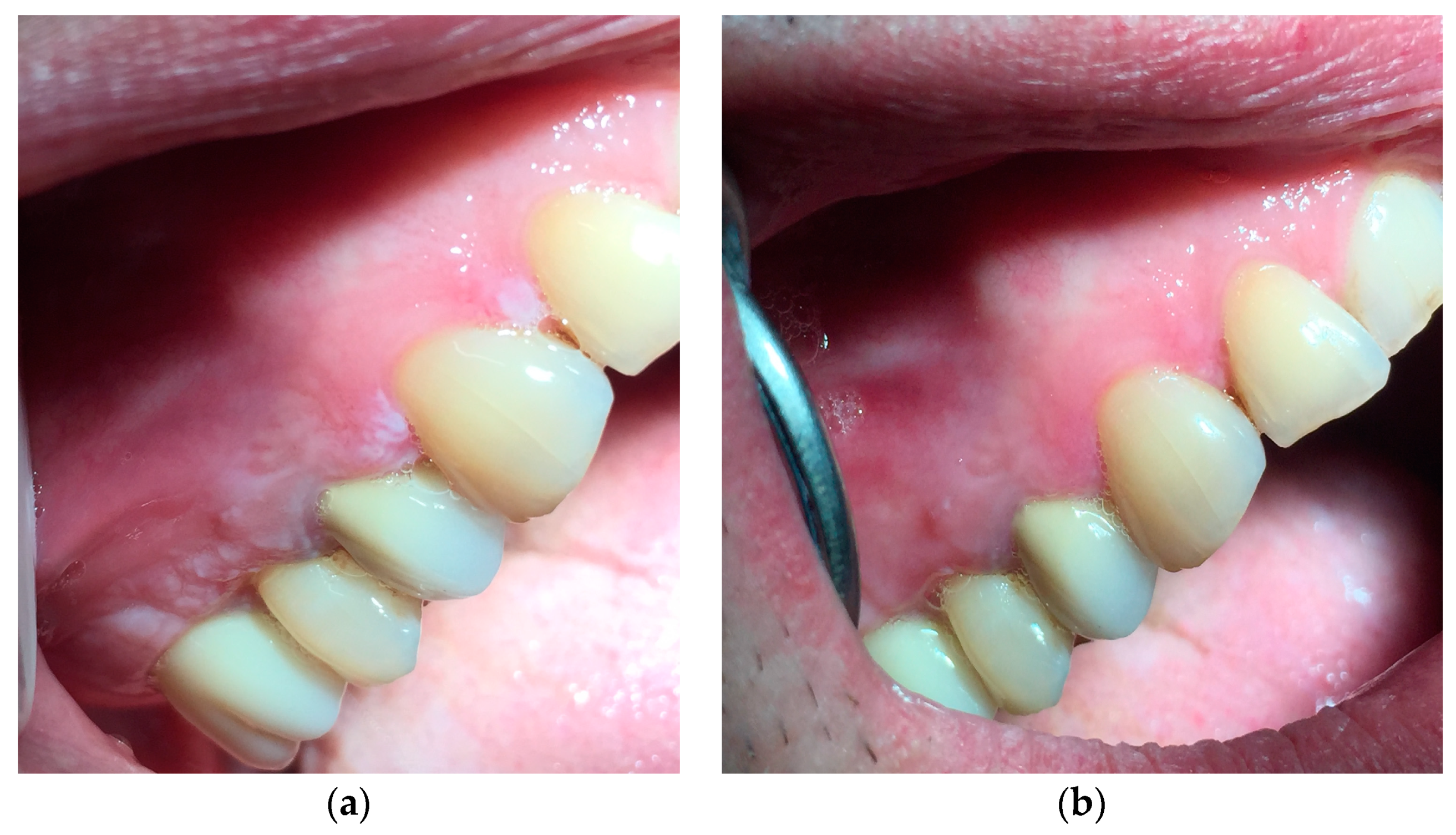
- The site presenting the lesion,
- The histological examination,
- The size of the lesion, in order to have this data, a periodontal probe was used and the greatest distance between the sides of the lesion was measured,
- How long the lesion was present.
- The lesion was measured with periodontal probe and the results were reported in mm,
- The appearance of the lesion was reported,
- The discomfort was measured with an arbitrary numerical scale from 0 to 5 and the type of discomfort that the patient perceived was noted,
- The pain caused by the lesion was measured, with an NRS scale (Numerical Rating Scale) [19],
- The tactile perception was evaluated, that is the sensation of roughness that the patient felt passing the tongue on the area where the lesion was present, with an arbitrary numerical scale from 0 to 5.
- Discomfort measured with an arbitrary numerical scale from 0 to 5.
- Pain caused by the lesion, measured with the NRS scale [19].
- Tactile perception, measured with an arbitrary numerical scale from 0 to 5.
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Analysis of the Lesion Size
3.3. Discomfort Analysis
3.4. Tactile Perception
3.5. Pain: Not Perceived
4. Discussion
- ○
- Size of the lesion.
- ○
- Tactile perception.
- ○
- Discomfort.
- ○
- Pain.
4.1. Effectiveness
4.2. Efficiency
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bokor-Bratić, M. Prevalence of oral leucoplakia. Med. Pregl. 2003, 56, 552–555. [Google Scholar] [CrossRef]
- Gönen, Z.; Asan, C.Y.; Etöz, O.; Alkan, A. Oral leucoplakia associated with amalgam restorations. J. Oral Sci. 2016, 58, 445–448. [Google Scholar] [CrossRef]
- Kazanowska-Dygdala, M.; Dus, I.; Radwan-oczko, M. The presence of Helicobacter pylori in oral cavities of patients with leucoplakia and oral lichen planus. J. Appl. Oral Sci. 2016, 24, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Chaves, A.L.F.; Silva, A.G.; Maia, F.M.; Lopes, G.F.M.; de Paulo, L.F.B.; Muniz, L.V.; Dos Santos, H.B.; Soares, J.M.A.; Souza, A.A.; de Oliveira Barbosa, L.A.; et al. Reduced CD8+ T cells infiltration can be associated with a malignant transformation in potentially malignant oral epithelial lesions. Clin. Oral Investig. 2018. [Google Scholar] [CrossRef] [PubMed]
- Ardiuno, P.G.; Bagan, J.; El-Naggar, A.K.; Carrozzo, M. Urban legends series: Oral Leucoplakia. Oral Dis. 2013, 19, 642–659. [Google Scholar] [CrossRef]
- Kumar, A.; McCaul, L.C.J.; Kerawala, C.J.; Coombed, D.; Godden, D.; Brennan, P.A. How should we manage oral leucoplakia? Br. J. Oral Maxillofac. Surg. 2013, 51, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, L.; Barbieri, C.; Martins, M.; Salazar, F.; Vescovi, P.; Meleti, M.; Pacheco, J. Type of surgical treatment and recurrence of oral leucoplakia: A retrospective clinical study. Oral Med. Pathol. 2017, 22, 520–526. [Google Scholar]
- Modegas-Vegara, A.; Hueto-Madrid, J.; Chimenos-Küstner, E.; Bescos-Atin, C. The treatment of oral leucoplakia with the CO2 laser: A retrospective study of 65 patients. J. Cranio-Maxillo-Fac. Surg. 2015, 43, 677–681. [Google Scholar] [CrossRef]
- Del Corso, G.; Gissi, D.B.; Tarsitano, A.; Costabile, E.; Marchetti, C.; Foschini, L.M. Laser evaporation versus laser excision of oral leucoplakia: A retrospective study with long-term follow-up. J. Cranio-Maxillo-Fac. Surg. 2015, 43, 763–768. [Google Scholar] [CrossRef]
- Chainani-Wu, N.; Madden, E.; Sim, C.; Collins, K.; Silverman, S. Clinical predictors of oral leucoplakia recurrence following CO2 laser vaporization. J. Cranio-Maxillo-Fac. Surg. 2015, 43, 1875–1879. [Google Scholar] [CrossRef]
- Grammer, R.; Lerman, M.A. Keratosis of unknown significance and leucoplakia: A preliminary study. Oral Maxillofac. Pathol. 2014, 118, 713–724. [Google Scholar]
- Bellato, L.; Martinelli, P.; Lombardi, T. Alveolar ridge keratosis—A retrospective clinicopathological study. Head Face Med. 2013, 9, 2–5. [Google Scholar] [CrossRef] [PubMed]
- Matarese, G.; Ramaglia, L.; Cicciù, M.; Cordasco, G.; Isola, G. The Effects of Diode Laser Therapy as an Adjunct to Scaling and Root Planing in the Treatment of Aggressive Periodontitis: A 1-Year Randomized Controlled Clinical Trial. Photomed. Laser Surg. 2017, 35, 702–709. [Google Scholar] [CrossRef] [PubMed]
- Caccianiga, G.; Rey, G.; Paiusco, A.; Lauritano, D.; Cura, F.; Ormianer, Z.; Carinci, F. Oxygen high level laser therapy is efficient in treatment of chronic periodontitis: A clinical and microbiological study using PCR analysis. J. Biol. Regul. Homeost. Agents 2016, 30 (Suppl. 1), 87–97. [Google Scholar] [PubMed]
- Yadwad, K.; Veena, H.R.; Patil, S.; Shivaprasad, B.M. Diode laser therapy in the management of chronic periodontitis—A clinico-microbiological study. Int. Med. Appl. Sci. 2017, 9, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Meimandi, M.; Ardakani, M.; Nejad, A.; Yousefnejad, P.; Saebi, K.; Tayeed, M. The Effect of Photodynamic Therapy in the Treatment of Chronic Periodontitis: A Review of Literature. J. Lasers Med. Sci. 2017, 8 (Suppl. 1), S7–S11. [Google Scholar] [CrossRef]
- Roncati, M.; Lauritano, D.; Cura, F.; Carinci, F. Evaluation of light-emitting diode (LED-835 NM) application over human gingival fibroblast: An in vitro study. J. Biol. Regul. Homeost. Agents 2016, 30 (Suppl. 1), 161–167. [Google Scholar]
- Isola, G.; Matarese, G.; Williams, R.C.; Siciliano, V.I.; Alibrandi, A.; Cordasco, G.; Ramaglia, L. The effects of a desiccant agent in the treatment of chronic periodontitis: A randomized, controlled clinical trial. Clin. Oral Investig. 2018, 22, 791–800. [Google Scholar] [CrossRef]
- Sirintawat, N.; Sawang, K.; Chaiyasamut, T.; Wongsirichat, N. Pain measurement in oral and maxillofacial surgery. J. Dent. Anesth. Pain Med. 2017, 17, 253–263. [Google Scholar] [CrossRef]
- Usama, R.K.; Onkar, S.; Birangane, R.; Chaudhari, S.; Kulkarni, A. Treatment of oral leucoplakia with diode laser: A pilot study on Indian subjects. Asian Pac. J. Cancer Prev. 2015, 16, 8383–8386. [Google Scholar]
- Kuribayashi, Y.; Tsushima, F.; Morita, K.; Matsumoto, K.; Sakurai, J.; Uesugi, A.; Sato, K.; Oda, S. Long-term outcome of non-surgical treatment in patients with oral leucoplakia. J. Cranio-Maxillo-Fac. Surg. 2015, 51, 1020–1025. [Google Scholar]
- Natekar, M.; Raghuveer, H.; Rayapati, D.; Shobha, E.; Prashanth, N.; Rangan, V. A comparative evaluation: Oral leukoplakia surgical management using diode laser, CO2 laser and cryosurgery. Oral Surg. 2017, 9, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Brouns, E.R.E.A.; Baart, J.A.; van der Waal, I.; Karagozoglu, K.H.; Aartman, I.H.A. Treatment results of CO2 laser vaporisation in a cohort of 35 patients with oral leukoplakia. Oral Dis. 2013, 19, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Maloth, K.; Velpula, N.; Kodangal, S.; Sangmesh, M.; Meka, S.U. Photodynamic Therapy—A Non-invasive Treatment Modality for Precancerous Lesions. J. Lasers Med. Sci. 2016, 7, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Van der Hem, P.S.; van der Wal, J.E.; Nauta, J.M.; Roodenburg, J.L.N. The results of CO2 laser surgery in patients with oral leukoplakia: A 25 year follow up. Oral Oncol. 2005, 41, 31–47. [Google Scholar] [CrossRef] [PubMed]
- Vivek, V.; Balan, A.; Jayasree, R.S.; Sreelatha, K.T.; Gupta, A.K. Three-year follow-up of oral leukoplakia after neodymium: Yttrium aluminum garnet (Nd:YAG) laser surgery. Laser Med. Sci. 2008, 23, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Comacho-Alonso, L.J. Comparison of pain and swelling after removal of oral leukoplakia with CO2 laser and cold knife: A randomized clinical trial. Med. Oral 2013, 18, 38–44. [Google Scholar]
- Tambuwala, A.; Sangle, A.; Khan, A.; Sayed, A. Excision of Oral Leukoplakia by CO2 Lasers Versus Traditional Scalpel: A Comparative Study. J. Maxillofac. Oral Surg. 2014, 13, 320–327. [Google Scholar] [CrossRef]
- Romeo, U.; Russo, N.; Palaia, G.; Tenore, G.; Del Vecchio, A. Oral proliferative verrucous leukoplakia treated with the photodynamic therapy: A case report. Ann. Stomatol. 2014, 2, 77–80. [Google Scholar] [CrossRef]





| Regression: Lesion Dimension T1 | ||
|---|---|---|
| Constant | Lesion Dimension T0 | |
| Coefficient | −8.5327 | 0.814990 |
| Std error of coef | 11.7132 | 0.03492 |
| t-ratio | −0.7285 | 23.3347 |
| Significance | 4756.97% | 0.0000 % |
| Beta-weight | 0.9839 | |
| Standard error of regression | 42.4721 | |
| Coefficient of determination | 96.80% | |
| Adjusted coef of determination | 96.62% | |
| Number of observation | 20 | |
| Residual degrees of freedom | 18 | |
| t-statistic for computing | ||
| 95% confidence intervals | 2.1009 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lauritano, D.; Lucchese, A.; Gabrione, F.; Di Stasio, D.; Silvestre Rangil, J.; Carinci, F. The Effectiveness of Laser-Assisted Surgical Excision of Leukoplakias and Hyperkeratosis of Oral Mucosa: A Case Series in A Group of Patients. Int. J. Environ. Res. Public Health 2019, 16, 210. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16020210
Lauritano D, Lucchese A, Gabrione F, Di Stasio D, Silvestre Rangil J, Carinci F. The Effectiveness of Laser-Assisted Surgical Excision of Leukoplakias and Hyperkeratosis of Oral Mucosa: A Case Series in A Group of Patients. International Journal of Environmental Research and Public Health. 2019; 16(2):210. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16020210
Chicago/Turabian StyleLauritano, Dorina, Alberta Lucchese, Federica Gabrione, Dario Di Stasio, Javier Silvestre Rangil, and Francesco Carinci. 2019. "The Effectiveness of Laser-Assisted Surgical Excision of Leukoplakias and Hyperkeratosis of Oral Mucosa: A Case Series in A Group of Patients" International Journal of Environmental Research and Public Health 16, no. 2: 210. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16020210






