Mediating Effect of Social Support in the Relationship Between Childhood Abuse and Non-Suicidal Self-Injury Among Chinese Undergraduates: The Role of Only-Child Status
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Measures
2.2.1. Non-Suicidal Self-Injury
2.2.2. Childhood Abuse
2.2.3. Social Support
2.2.4. Covariates
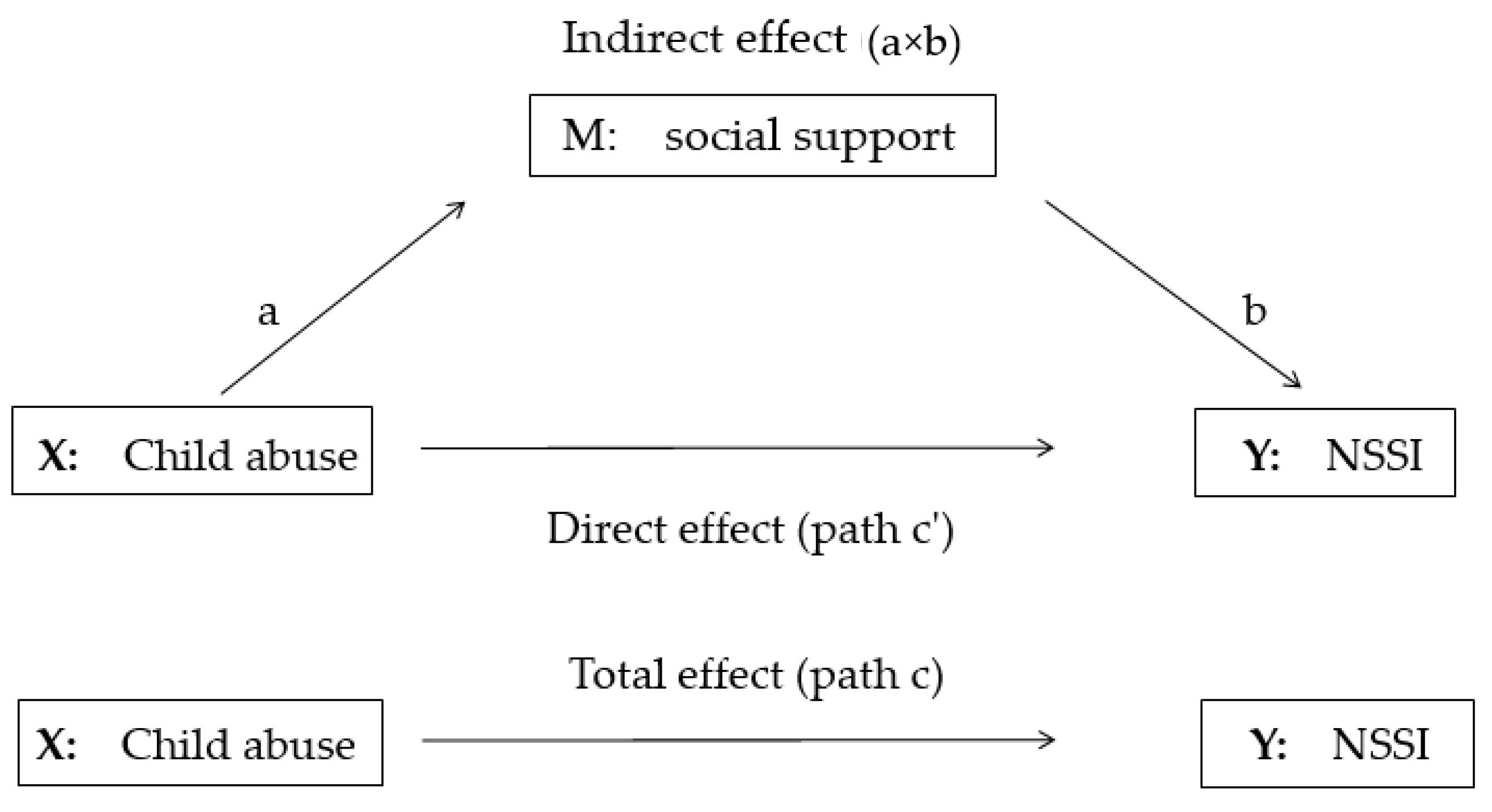
2.3. Data Analysis
3. Results
3.1. Characteristics of Participants
3.2. Correlation Analysis of Child Abuse Score, Social Support Score, and NSSI Frequency
3.3. Testing for Mediation Effects of Social Support in the Relationship Between Childhood Abuse and NSSI
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Types of CA | Only Child | Boot LLCI | Boot ULCI | Indirect Effect a × b | Boot LLCI | Boot ULCI | Direct Effect c’ | Mediation Ratio, % a × b/(a × b + c’) |
|---|---|---|---|---|---|---|---|---|
| Childhood abuse | Yes | 0.0019 | 0.0113 | 0.0053 | 0.0456 | 0.1035 | 0.0745 ** | 6.64% |
| No | −0.0023 | 0.0030 | 0.0003 | 0.1260 | 0.1614 | 0.1437 ** | ND | |
| Physical abuse | Yes | 0.0029 | 0.0175 | 0.0081 | 0.0310 | 0.1242 | 0.0776* | 9.45% |
| No | −0.0014 | 0.0049 | 0.0014 | 0.1608 | 0.2190 | 0.1899 ** | ND | |
| Emotional abuse | Yes | 0.0061 | 0.0301 | 0.0152 | 0.1400 | 0.2679 | 0.2039 ** | 6.94% |
| No | −0.0066 | 0.0060 | −0.0002 | 0.2939 | 0.3743 | 0.3341 ** | ND | |
| Sexual abuse | Yes | −0.0612 | −0.0100 | −0.0290 | −0.0717 | 0.2016 | 0.0650 | ND |
| No | −0.0022 | 0.0248 | 0.0084 | 0.1958 | 0.4441 | 0.3200 ** | ND |
| Types of CA | Only Child | Boot LLCI | Boot ULCI | Indirect Effect a × b | Boot LLCI | Boot ULCI | Direct Effect c’ | Mediation Ratio, % a × b/(a × b + c’) |
|---|---|---|---|---|---|---|---|---|
| Childhood abuse | Yes | 0.0035 | 0.0176 | 0.0086 | 0.0421 | 0.1004 | 0.0713 ** | 10.78% |
| No | −0.0057 | −0.0001 | −0.0024 | 0.1287 | 0.1641 | 0.1464 ** | ND | |
| Physical abuse | Yes | 0.0059 | 0.0286 | 0.0142 | 0.0247 | 0.1185 | 0.0716* | 16.57% |
| No | −0.0064 | −0.0006 | −0.0021 | 0.1643 | 0.2225 | 0.1934 ** | ND | |
| Emotional abuse | Yes | 0.0068 | 0.0369 | 0.0174 | 0.1377 | 0.2656 | 0.2017 ** | 7.94% |
| No | −0.0136 | −0.0008 | −0.0058 | 0.2997 | 0.3797 | 0.3397 ** | ND | |
| Sexual abuse | Yes | −0.0365 | 0.0192 | −0.0077 | −0.0922 | 0.1797 | 0.0437 | ND |
| No | −0.0173 | 0.0052 | −0.0036 | 0.2078 | 0.4561 | 0.3319 ** | ND |
| Types of CA | Only Child | Boot LLCI | Boot ULCI | Indirect Effect a × b | Boot LLCI | Boot ULCI | Direct Effect c’ | Mediation Ratio, % a × b/(a × b + c’) |
|---|---|---|---|---|---|---|---|---|
| Childhood abuse | Yes | 0.0018 | 0.0134 | 0.0061 | 0.0447 | 0.1028 | 0.0737 ** | 7.64% |
| No | −0.0014 | 0.0016 | 0.0000 | 0.1264 | 0.1616 | 0.1440 ** | ND | |
| Physical abuse | Yes | 0.0034 | 0.0243 | 0.0109 | 0.0279 | 0.1217 | 0.0748* | 12.72% |
| No | −0.0016 | 0.0029 | −0.0003 | 0.1620 | 0.2201 | 0.1910 ** | ND | |
| Emotional abuse | Yes | 0.0042 | 0.0281 | 0.0132 | 0.1420 | 0.2699 | 0.2059 ** | 6.02% |
| No | −0.0038 | 0.0036 | −0.0002 | 0.2942 | 0.3740 | 0.3341 ** | ND | |
| Sexual abuse | Yes | −0.0539 | −0.0036 | −0.0211 | −0.0795 | 0.1937 | 0.0571 | ND |
| No | −0.0050 | 0.0029 | 0.0001 | 0.2047 | 0.4523 | 0.3285 ** | ND |
References
- International Society for the Study of Self-injury. What is Self-Injury? 2018. Available online: https://itriples.org/about-self-injury/what-is-self-injury (accessed on 1 May 2018).
- Brunner, R.; Kaess, M.; Parzer, P.; Fischer, G.; Carli, V.; Hoven, C.W.; Wasserman, C.; Sarchiapone, M.; Resch, F.; Apter, A.; et al. Life-time prevalence and psychosocial correlates of adolescent direct self-injurious behavior: A comparative study of findings in 11 European countries. J. Child Psychol. Psychiatry 2014, 55, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Gillies, D.; Christou, M.A.; Dixon, A.C.; Featherston, O.J.; Rapti, I.; Garcia-Anguita, A.; Villasis-Keever, M.; Reebye, P.; Christou, E.; Al Kabir, N.; et al. Prevalence and Characteristics of Self-Harm in Adolescents: Meta-Analyses of Community-Based Studies 1990–2015. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 733–741. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.H.; Chen, R.L.; Ma, S.S.; McFeeters, D.; Hao, J.H.; Tao, F.B. Associations of adverse childhood experiences and social support with self-injurious behaviour and suicidality in adolescents. Br. J. Psychiatry 2019, 214, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Doksat, N.G.; Zahmacioglu, O.; Demirci, A.C.; Kocaman, G.M.; Erdogan, A. Association of Suicide Attempts and Non-Suicidal Self-Injury Behaviors With Substance Use and Family Characteristics Among Children and Adolescents Seeking Treatment for Substance Use Disorder. Subst. Use Misuse 2017, 52, 1–10. [Google Scholar]
- Pérez, J.; Venta, A.; Garnaat, S.; Sharp, C. The Difficulties in Emotion Regulation Scale: Factor Structure and Association with Nonsuicidal Self-Injury in Adolescent Inpatients. J. Psychopathol. Behav. Assess. 2012, 34, 393–404. [Google Scholar] [CrossRef]
- Brackman, E.H.; Morris, B.W.; Andover, M.S. Predicting Risk for Suicide: A Preliminary Examination of Non-Suicidal Self-Injury and the Acquired Capability Construct in a College Sample. Arch. Suicide Res. 2016, 20, 663–676. [Google Scholar] [CrossRef]
- Whitlock, J.; Muehlenkamp, J.; Eckenrode, J.; Purington, A.; Baral Abrams, G.; Barreira, P.; Kress, V. Non-suicidal self-injury as a gateway to suicide in adolescents and young adults. J. Adolesc. Health 2013, 52, 486–492. [Google Scholar] [CrossRef]
- Lang, C.M.; Sharma-Patel, K. The Relation between Childhood Maltreatment and Self-Injury: A Review of the Literature on Conceptualization and Intervention. Trauma Violence Abus. 2011, 12, 23–37. [Google Scholar] [CrossRef]
- Taliaferro, L.A.; Muehlenkamp, J.J.; Borowsky, I.W.; McMorris, B.J.; Kugler, K.C. Factors Distinguishing Youth Who Report Self-Injurious Behavior: A Population-Based Sample. Acad. Pediatr. 2012, 12, 205–213. [Google Scholar] [CrossRef]
- Serafini, G.; Canepa, G.; Adavastro, G.; Nebbia, J.; Murri, M.B.; Erbuto, D.; Pocai, B.; Fiorillo, A.; Pompili, M.; Flouri, E.; et al. The Relationship between Childhood Maltreatment and Non-Suicidal Self-Injury: A Systematic Review. Front. Psychol. 2017, 8, 149. [Google Scholar] [CrossRef]
- Martin, J.; Raby, K.L.; Labella, M.H.; Roisman, G.I. Childhood abuse and neglect, attachment states of mind, and non-suicidal self-injury. Attach. Hum. Dev. 2017, 19, 425–446. [Google Scholar] [CrossRef] [PubMed]
- Karatekin, C.; Ahluwalia, R. Effects of Adverse Childhood Experiences, Stress, and Social Support on the Health of College Students. J. Interpers. Violence 2016. [CrossRef] [PubMed]
- Herrenkohl, T.I.; Jung, H.; Klika, J.B.; Mason, W.A.; Brown, E.C.; Leeb, R.T.; Herrenkohl, R.C. Mediating and moderating effects of social support in the study of child abuse and adult physical and mental health. Am. J. Orthopsychiatry 2016, 86, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Baiden, P.; Stewart, S.L.; Fallon, B. The role of adverse childhood experiences as determinants of non-suicidal self-injury among children and adolescents referred to community and inpatient mental health settings. Child Abus. Negl. 2017, 69, 163–176. [Google Scholar] [CrossRef]
- Ditzen, B.; Heinrichs, M. Psychobiology of social support: the social dimension of stress buffering. Restor. Neurol. Neurosci. 2014, 32, 149–162. [Google Scholar]
- Gayer-Anderson, C.; Fisher, H.L.; Fearon, P.; Hutchinson, G.; Morgan, K.; Dazzan, P.; Boydell, J.; Doody, G.A.; Jones, P.B.; Murray, R.M.; et al. Gender differences in the association between childhood physical and sexual abuse, social support and psychosis. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1489–1500. [Google Scholar] [CrossRef] [Green Version]
- Christoffersen, M.N.; Møhl, B.; DePanfilis, D.; Vammen, K.S. Non-Suicidal Self-Injury—Does social support make a difference? An epidemiological investigation of a Danish national sample. Child Abus. Negl. 2015, 44, 106–116. [Google Scholar] [CrossRef]
- Evans, S.E.; Steel, A.L.; DiLillo, D. Child maltreatment severity and adult trauma symptoms: does perceived social support play a buffering role? Child Abus. Negl. 2013, 37, 934–943. [Google Scholar] [CrossRef]
- Zhang, S.; Zhang, Y.; Jin, F. Mediating role of social support in the association among childdood psychological maltreatment neglect and self injury of local normal university students in Liaoning Province. Chin. J. Sch. Health 2017, 38, 1510–1512. [Google Scholar] [CrossRef]
- Xi, M.Y. Research on the differences in social support between only-child and non-only-child undergraduates. J. Nanyang Norm. Univ. 2012, 11, 102–104. [Google Scholar]
- Fletcher, C. Adult Reflections on Being an ‘Only-Child’. Master’s Thesis, University of Chester, Chester, UK, 2014. [Google Scholar]
- Gu, Z.Y. Estimating the quantity of only-child population and the only-child-loss families in China: Based on the analysis of the sixth population census data. J. Chang. Inst. Technol. 2016, 1, 83–89. [Google Scholar] [CrossRef]
- Wan, Y.-H.; Hu, C.L.; Hao, J.H.; Sun, Y.; Tao, F.B. Deliberate self-harm behaviors in Chinese adolescents and young adults. Eur. Child Adolesc. Psychiatry 2011, 20, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Moran, P.; Coffey, C.; Romaniuk, H.; Olsson, C.; Borschmann, R.; Carlin, J.B.; Patton, G.C. The natural history of self-harm from adolescence to young adulthood: a population-based cohort study. Lancet 2012, 379, 236–243. [Google Scholar] [CrossRef] [Green Version]
- Wan, Y.; Chen, J.; Sun, Y.; Tao, F. Impact of Childhood Abuse on the Risk of Non-Suicidal Self-Injury in Mainland Chinese Adolescents. PLoS ONE 2015, 10, e0131239. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.M.; Dai, X.Y. Development of social support scale for university students. Chin. J. Clin. Psychol. 2008, 16, 456–458. [Google Scholar]
- Xing, C.; Tao, F.B.; Yuan, C.J.; Wan, Y.H.; Qi, X.Y.; Hu, C.L.; Hao, J.H.; Yao, R.Y. Evaluation of reliability and validity of the multidimensional sub-health questionnaire of adolescents. Chin. J. Public Health 2008, 24, 1031–1033. [Google Scholar]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef] [Green Version]
- Wu, J.; Liu, H. Features of non suicidal self-injury and relationships with coping methods among college students. Iran J. Public Health 2019, 48, 270–277. [Google Scholar]
- Kiekens, G.; Hasking, P.; Claes, L.; Boyes, M.; Mortier, P.; Auerbach, R.; Cuijpers, P.; Demyttenaere, K.; Green, J.; Kessler, R.; et al. Predicting the incidence of non-suicidal self-injury in college students. Eur. Psychiatry 2019, 59, 44–51. [Google Scholar] [CrossRef]
- Taliaferro, L.A.; Muehlenkamp, J.J. Risk factors associated with self-injurious behavior among a national sample of undergraduate college students. J. Am. Coll. Health 2015, 63, 40–48. [Google Scholar] [CrossRef]
- Mars, B.; Heron, J.; Klonsky, E.D.; Moran, P.; O’Connor, R.C.; Tilling, K.; Wilkinson, P.; Gunnell, D. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiatry 2019, 6, 327–337. [Google Scholar] [CrossRef] [Green Version]
- Andrewes, H.E.; Hulbert, C.; Cotton, S.M.; Betts, J.; Chanen, A.M. Relationships between the frequency and severity of non-suicidal self-injury and suicide attempts in youth with borderline personality disorder. Early Interv. Psychiatry 2019, 13, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Zubrick, S.R.; Hafekost, J.; Johnson, S.E.; Sawyer, M.G.; Patton, G.; Lawrence, D. The continuity and duration of depression and its relationship to non-suicidal self-harm and suicidal ideation and behavior in adolescents 12–17. J. Affect. Disord. 2017, 220, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.L.; Clum, G.A. Social support and problem-solving as moderators of the relationship between childhood abuse and suicidality: Applications to a delinquent population. J. Trauma. Stress 2002, 15, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Sperry, D.M.; Widom, C.S. Child abuse and neglect, social support, and psychopathology in adulthood: a prospective investigation. Child Abus. Negl. 2013, 37, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, M.A. Childhood physical maltreatment, perceived social isolation, and internalizing symptoms: A longitudinal, three-wave, population-based study. Eur. Child Adolesc. Psychiatry 2018, 27, 481–491. [Google Scholar] [CrossRef]
- Li, S.; Zhao, F.; Yu, G. Childhood maltreatment and intimate partner violence victimization: A meta-analysis. Child Abus. Negl. 2019, 88, 212–224. [Google Scholar] [CrossRef]
- Swannell, S.; Martin, G.; Page, A.; Hasking, P.; Hazell, P.; Taylor, A.; Protani, M. Child maltreatment, subsequent non-suicidal self-injury and the mediating roles of dissociation, alexithymia and self-blame. Child Abus. Negl. 2012, 36, 572–584. [Google Scholar] [CrossRef]
- Ma, S.; Wan, Y.; Zhang, S.; Xu, S.; Liu, W.; Xu, L.; Zhai, L.; Zhang, H.; Hao, J.; Tao, F. Mediating effect of psychological symptoms, coping styles and impulsiveness on the relationship between childhood abuses and non-suicidal self-injuries among middle school students. Wei Sheng Yan Jiu J. Hyg. Res. 2018, 47, 530–535. [Google Scholar]
- Liu, N.; Chen, Y.; Yang, X.; Hu, Y. Do Demographic characteristics make differences? Demographic characteristics as moderators in the associations between only child status and cognitive/non-cognitive outcomes in China. Front. Psychol. 2017, 8, 3. [Google Scholar] [CrossRef]
- Paivio, S.C.; McCulloch, C.R. Alexithymia as a mediator between childhood trauma and self-injurious behaviors. Child Abus. Negl. 2004, 28, 339–354. [Google Scholar] [CrossRef] [PubMed]
- Falbo, T.; Hooper, S.Y. China’s only children and psychopathology: A quantitative synthesis. Am. J. Orthopsychiatry 2015, 85, 259–274. [Google Scholar] [CrossRef] [PubMed]
- Chen, K. A Study of Current Only-Child Families in China: Asurvey of 1180 Families in the Urban and Suburban Areas of Beijing; International Sociological Association: Madrid, Spain, 1986. [Google Scholar]
- Feng, X. Bias and reality: A survey analysis of issues on only children’s education. Sociol. Stud. 1993, 1, 90–96. [Google Scholar]
- Liu, R.X.; Lin, W.; Chen, Z.-Y. School performance, peer association, psychological and behavioral adjustments: A comparison between Chinese adolescents with and without siblings. J. Adolesc. 2010, 33, 411–417. [Google Scholar] [CrossRef]
- Liu, X.; Huang, X.T. Social support and its mechanism for mental health. Psychol. Res. 2010, 3, 3–8. [Google Scholar]
| Variable | Total (n = 4799) | Only Child (n = 1577) | Non-Only Child (n = 3222) | p-Value |
|---|---|---|---|---|
| Age (mean, s.d) | 20.51 (1.02) | 20.24 (0.87) | 20.64 (1.06) | p < 0.001 |
| Gender (n (%)) | ||||
| boy | 2011 (41.9) | 903 (57.3) | 1108 (34.4) | p < 0.001 |
| girl | 2788 (58.1) | 674 (42.7) | 2114 (65.6) | |
| Urban/rural | ||||
| rural | 3139 (65.4) | 532 (33.7) | 2607 (80.9) | p < 0.001 |
| urban | 1660 (34.6) | 1045 (66.3) | 615 (19.1) | |
| Father’s education level | ||||
| Less than junior middle school | 936 (19.5) | 229 (14.5) | 707 (21.9) | p < 0.001 |
| Junior middle school | 2184 (45.5) | 464 (29.4) | 1720 (53.4) | |
| Senior middle school | 1051 (21.9) | 412 (26.1) | 639 (19.8) | |
| College or more | 628 (13.1) | 472 (29.9) | 156 (4.8) | |
| Mother’s education level | ||||
| Less than junior middle school | 2179 (45.4) | 362 (23.0) | 1817 (56.4) | p < 0.001 |
| Junior middle school | 1630 (34.0) | 530 (33.6) | 1100 (34.1) | |
| Senior middle school | 655 (13.6) | 414 (26.2) | 241 (7.5) | |
| College or more | 335 (7.0) | 271 (17.2) | 64 (2.0) | |
| Economic status of family | ||||
| poor | 1339 (27.9) | 240 (15.2) | 1099 (34.1) | p < 0.001 |
| moderate | 3181 (66.3) | 1169 (74.1) | 2012 (62.4) | |
| good | 279 (5.8) | 168 (10.7) | 111 (3.4) | |
| Non-suicidal self-injury # | ||||
| Yes | 568 (11.8) | 211 (13.4) | 357 (11.1) | 0.021 |
| No | 4231 (88.2) | 1366 (86.6) | 2865 (88.9) | |
| Psychological symptoms (mean, s.d) | 3.69 (6.61) | 3.963 (7.10) | 3.58 (6.35) | 0.086 |
| Childhood abuse (mean, s.d) | ||||
| Total | 17.12 (5.26) | 17.08 (5.02) | 17.13 (5.37) | 0.767 |
| Physical abuse | 7.21 (3.19) | 7.25 (3.07) | 7.19 (3.25) | 0.524 |
| Emotional abuse | 5.64 (2.32) | 5.53 (2.25) | 5.69 (2.35) | 0.024 |
| Sexual abuse | 4.27 (0.87) | 4.30 (1.05) | 4.25 (0.77) | 0.060 |
| Social support (mean, s.d) | ||||
| Total | 32.10 (13.49) | 30.86 (13.43) | 32.70 (13.48) | p < 0.001 |
| Classmates and friends | 11.88 (5.34) | 11.38 (5.31) | 12.12 (5.34) | p < 0.001 |
| Family and relatives | 12.32 (5.57) | 11.88 (5.64) | 12.53 (5.52) | p < 0.001 |
| Others | 8.36 (4.01) | 8.11 (3.95) | 8.48 (4.03) | 0.003 |
| Category | Variable | CA | PA | 3. EA | 4. SA | 5. SS | 6. NSSI |
|---|---|---|---|---|---|---|---|
| Total | 1. Childhood abuse | 1.00 | |||||
| 2. Physical abuse | 0.92 * | 1.00 | |||||
| 3. Emotional abuse | 0.86 * | 0.63 * | 1.00 | ||||
| 4. Sexual abuse | 0.39 * | 0.19 * | 0.25 * | 1.00 | |||
| 5. Social support | −0.20 * | −0.17 * | −0.20 * | −0.08 * | 1.00 | ||
| 6. NSSI | 0.27 * | 0.22 * | 0.28 * | 0.11 * | −0.11 * | 1.00 | |
| Only child | 1. Childhood abuse | 1.00 | |||||
| 2. Physical abuse | 0.90 * | 1.00 | |||||
| 3. Emotional abuse | 0.83 * | 0.59 * | 1.00 | ||||
| 4. Sexual abuse | 0.36 * | 0.14 * | 0.14 * | 1.00 | |||
| 5. Social support | −0.19 * | −0.17 * | −0.18 * | −0.003 | 1.00 | ||
| 6. NSSI | 0.19 * | 0.13 * | 0.22 * | 0.07 * | −0.16 * | 1.00 | |
| Non-only child | 1.Childhood abuse | 1.00 | |||||
| 2. Physical abuse | 0.92 * | 1.00 | |||||
| 3. Emotional abuse | 0.88 * | 0.65 * | 1.00 | ||||
| 4. Sexual abuse | 0.43 * | 0.23 * | 0.33 * | 1.00 | |||
| 5. Social support | −0.21 * | −0.17 * | −0.21 * | −0.13 * | 1.00 | ||
| 6. NSSI | 0.31 * | 0.26 * | 0.32 * | 0.13 * | −0.08 * | 1.00 |
| Types of CA | Model | Boot LLCI | Boot ULCI | Indirect Effect a × b | Boot LLCI | Boot ULCI | Direct Effect c’ | Mediation Ratio, % a × b/(a × b + c’) |
|---|---|---|---|---|---|---|---|---|
| Childhood abuse | 1 | 0.0022 | 0.0097 | 0.0057 | 0.1254 | 0.1550 | 0.1402 ** | 3.91% |
| 2 | −0.0009 | 0.0037 | 0.0012 | 0.1088 | 0.1393 | 0.1241 ** | ND | |
| Physical abuse | 1 | 0.0055 | 0.0164 | 0.0104 | 0.1555 | 0.2047 | 0.1801 ** | 5.46% |
| 2 | −0.0003 | 0.0061 | 0.0025 | 0.1302 | 0.1800 | 0.1551 ** | ND | |
| Emotional abuse | 1 | 0.0054 | 0.0206 | 0.0124 | 0.2963 | 0.3634 | 0.3298 ** | 3.62% |
| 2 | −0.0028 | 0.0078 | 0.0023 | 0.2636 | 0.3318 | 0.2977 ** | ND | |
| Sexual abuse | 1 | 0.0115 | 0.0408 | 0.0237 | 0.2263 | 0.4066 | 0.3164 ** | 6.97% |
| 2 | −0.0046 | 0.0081 | 0.0010 | 0.1139 | 0.2960 | 0.2049 ** | ND |
| Types of CA | Model | Boot LLCI | Boot ULCI | Indirect effect a × b | Boot LLCI | Boot ULCI | Direct Effect c’ | Mediation Ratio, % a × b/(a × b + c’) |
|---|---|---|---|---|---|---|---|---|
| Childhood abuse | 1 | 0.0067 | 0.0248 | 0.0138 | 0.0691 | 0.1257 | 0.0974 ** | 12.41% |
| 2 | 0.0032 | 0.0152 | 0.0077 | 0.0431 | 0.1012 | 0.0721 ** | 9.65% | |
| Physical abuse | 1 | 0.0113 | 0.0409 | 0.0226 | 0.0541 | 0.1471 | 0.1006 ** | 18.34% |
| 2 | 0.0053 | 0.0251 | 0.0127 | 0.0262 | 0.1198 | 0.0730* | 14.82% | |
| Emotional abuse | 1 | 0.0150 | 0.0512 | 0.0294 | 0.1890 | 0.3148 | 0.2519 ** | 10.45% |
| 2 | 0.0075 | 0.0342 | 0.0178 | 0.1373 | 0.2653 | 0.2013 ** | 8.12% | |
| Sexual abuse | 1 | −0.0281 | 0.0373 | 0.0013 | 0.0648 | 0.3327 | 0.1988* | ND |
| 2 | −0.0554 | 0.0009 | −0.0218 | −0.0784 | 0.1941 | 0.0578 | ND |
| Types of CA | Model | Boot LLCI | Boot ULCI | Indirect Effect a × b | Boot LLCI | Boot ULCI | Direct Effect c’ | Mediation ratio, % a × b/(a × b + c’) |
|---|---|---|---|---|---|---|---|---|
| Childhood abuse | 1 | −0.0021 | 0.0056 | 0.0016 | 0.1420 | 0.1764 | 0.1592 ** | ND |
| 2 | −0.0043 | −0.0011 | −0.0013 | 0.1276 | 0.1630 | 0.1453 ** | ND | |
| Physical abuse | 1 | 0.0007 | 0.0110 | 0.0054 | 0.1858 | 0.2432 | 0.2145 ** | 2.46% |
| 2 | −0.0043 | 0.0024 | −0.0006 | 0.1628 | 0.2211 | 0.1920 ** | ND | |
| Emotional abuse | 1 | −0.0046 | 0.0120 | 0.0036 | 0.3281 | 0.4068 | 0.3674 ** | ND |
| 2 | −0.0105 | 0.0020 | −0.0036 | 0.2974 | 0.3775 | 0.3374 ** | ND | |
| Sexual abuse | 1 | 0.0132 | 0.0535 | 0.0295 | 0.3133 | 0.5601 | 0.4367 ** | 6.33% |
| 2 | −0.0090 | 0.0123 | 0.0011 | 0.2032 | 0.4514 | 0.3273 ** | ND |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, H.; Song, X.; Wang, S.; Zhang, S.; Xu, S.; Wan, Y. Mediating Effect of Social Support in the Relationship Between Childhood Abuse and Non-Suicidal Self-Injury Among Chinese Undergraduates: The Role of Only-Child Status. Int. J. Environ. Res. Public Health 2019, 16, 4023. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16204023
Xu H, Song X, Wang S, Zhang S, Xu S, Wan Y. Mediating Effect of Social Support in the Relationship Between Childhood Abuse and Non-Suicidal Self-Injury Among Chinese Undergraduates: The Role of Only-Child Status. International Journal of Environmental Research and Public Health. 2019; 16(20):4023. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16204023
Chicago/Turabian StyleXu, Huiqiong, Xianbing Song, Shanshan Wang, Shichen Zhang, Shaojun Xu, and Yuhui Wan. 2019. "Mediating Effect of Social Support in the Relationship Between Childhood Abuse and Non-Suicidal Self-Injury Among Chinese Undergraduates: The Role of Only-Child Status" International Journal of Environmental Research and Public Health 16, no. 20: 4023. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16204023





