Valuing Acute Health Risks of Air Pollution in the Jinchuan Mining Area, China: A Choice Experiment with Perceived Exposure and Hazardousness as Co-Determinants
Abstract
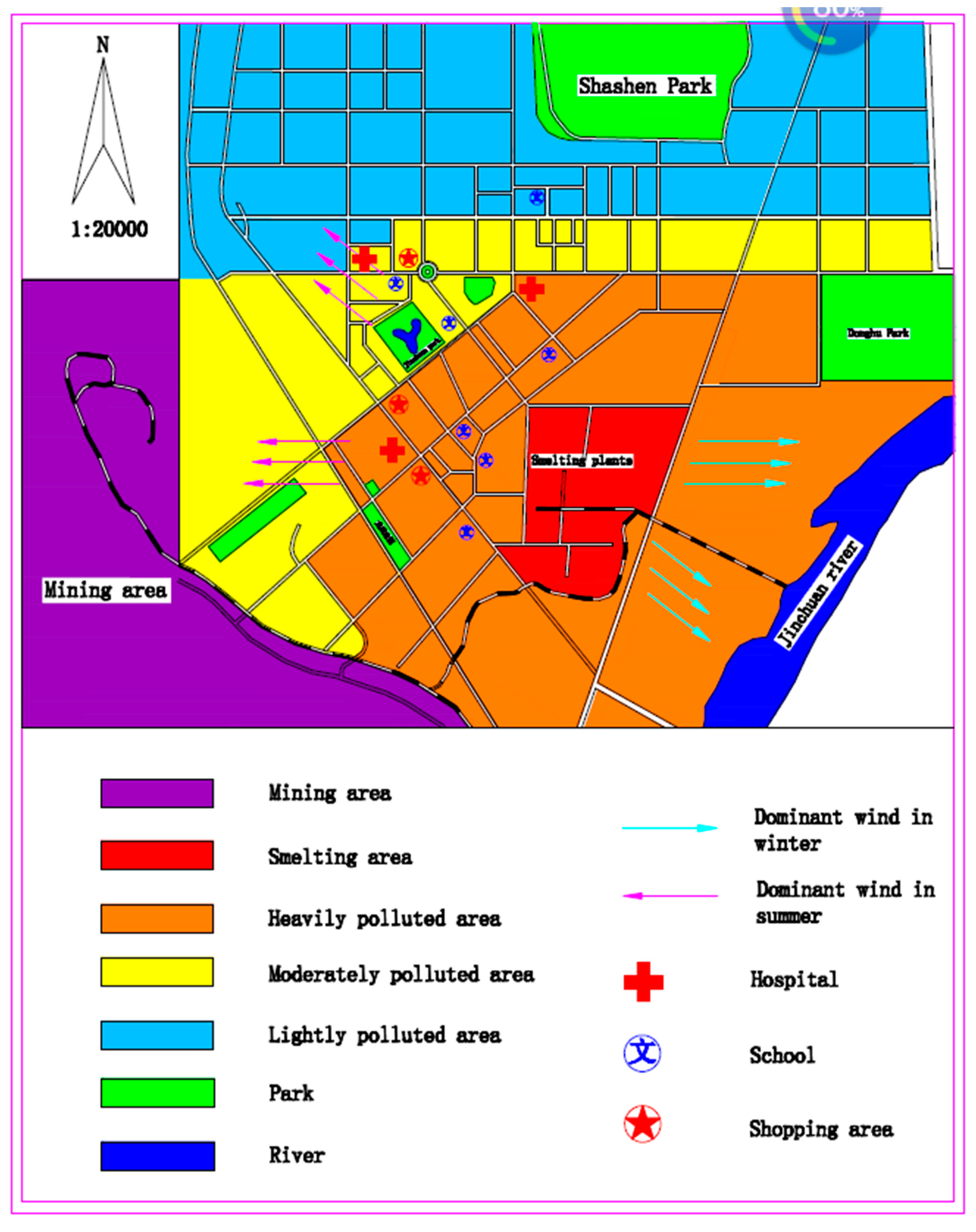
:1. Introduction
2. Conceptual Model and Methods
- (1)
- Illness characteristics: i.e., type of illness, duration, activity restriction, and price of prevention (cure).
- (2)
- Perceived health risk: health risk perception on exposure and hazardousness.
- (3)
- Respondent’s external characteristics: including age, family size, income, education, family health experience, work environment and proximity to the pollution source.
2.1. Choice Sets
2.2. Illness Characteristics
2.3. Perceived Health Risk
2.4. Respondent’s External Characteristics
2.5. The Random Parameter Logit Model (RPL)
2.6. Survey and Descriptive Statistics
3. Empirical Results
4. Discussion
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Unordered Choice Sets
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Pneumonia | Acute Pneumonia | I don’t want to purchase either |
| Duration | 9-day episode | 15-day episode | |
| Daily activity | No Limitation | No Limitation | |
| Price | 300 RMB | 500 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Bronchitis | Acute Bronchitis | I don’t want to purchase either |
| Duration | 5-day episode | 5-day episode | |
| Daily activity | At home | In Hospital | |
| Price | 300 RMB | 500 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute upper respiratory tract infection | Acute Pneumonia | I don’t want to purchase either |
| Duration | 9-day episode | 5-day episode | |
| Daily activity | At home | No Limitation | |
| Price | 300 RMB | 100 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute upper respiratory tract infection | Acute Bronchitis | I don’t want to purchase either |
| Duration | 5-day episode | 15-day episode | |
| Daily activity | At home | In Hospital | |
| Price | 300 RMB | 500 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Pneumonia | Acute Bronchitis | I don’t want to purchase either |
| Duration | 9-day episode | 15-day episode | |
| Daily activity | No Limitation | No Limitation | |
| Price | 100 RMB | 300 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Bronchitis | Acute Pneumonia | I don’t want to purchase either |
| Duration | 9-day episode | 5-day episode | |
| Daily activity | At home | At home | |
| Price | 500 RMB | 300 RMB | |
| Which alternative do you prefer to purchase |
Appendix B. Ordered Choice Sets
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Pneumonia | Acute Pneumonia | I don’t want to purchase either |
| Duration | 9-day episode | 15-day episode | |
| Daily activity | No Limitation | No Limitation | |
| Price | 300 RMB | 500 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Bronchitis | Acute Bronchitis | I don’t want to purchase either |
| Duration | 5-day episode | 5-day episode | |
| Daily activity | At home | In Hospital | |
| Price | 300 RMB | 500 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Pneumonia | Acute upper respiratory tract infection | I don’t want to purchase either |
| Duration | 5-day episode | 9-day episode | |
| Daily activity | No Limitation | At home | |
| Price | 100 RMB | 300 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute upper respiratory tract infection | Acute Bronchitis | I don’t want to purchase either |
| Duration | 5-day episode | 15-day episode | |
| Daily activity | At home | In Hospital | |
| Price | 300 RMB | 500 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Pneumonia | Acute Bronchitis | I don’t want to purchase either |
| Duration | 9-day episode | 15-day episode | |
| Daily activity | No Limitation | No Limitation | |
| Price | 100 RMB | 300 RMB | |
| Which alternative do you prefer to purchase |
| Alternative | A | B | C |
|---|---|---|---|
| Disease | Acute Pneumonia | Acute Bronchitis | I don’t want to purchase either |
| Duration | 5-day episode | 9-day episode | |
| Daily activity | At home | At home | |
| Price | 300 RMB | 500 RMB | |
| Which alternative do you prefer to purchase |
References
- Yan, M.; Wilson, A.; Bell, M.L.; Peng, R.D.; Sun, Q.; Pu, W.; Anderson, G.B. The Shape of the Concentration–Response Association between Fine Particulate Matter Pollution and Human Mortality in Beijing, China, and Its Implications for Health Impact Assessment. Environ. Health Perspect. 2019, 127, 067007. [Google Scholar] [CrossRef] [PubMed]
- Wong, E. Air pollution linked to 1.2 million premature deaths in China. New York Times. Available online: https://www.nytimes.com/2013/04/02/world/asia/air-pollution-linked-to-1-2-million-deaths-in-china.html (accessed on 1 April 2013).
- Chen, R.; Yin, P.; Meng, X.; Liu, C.; Wang, L.; Xu, X.; Zhou, M. Fine particulate air pollution and daily mortality. A nationwide analysis in 272 Chinese cities. Am. J. Respir. Crit. Care Med. 2017, 196, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Wei, K. Analysis of Atmosphere Sulfur Dioxide Pollution Control and Countermeasures; Lanzhou University: Lanzhou, China, 2008. [Google Scholar]
- Jinchuan Statistical Yearbook. Jinchuan Statistical Yearbook; Jinchuan Statistic Bureau: Jinchuan, China, 2010. (In Chinese) [Google Scholar]
- Huang, H.; Nan, Z.-R.; Hu, X.; Liu, X.; Li, Y.; Ding, H. Spatial distributions of heavy metals and assessment of potential ecological risk in jinchang urban area. Adm. Tech. Environ. Monit. 2009, 5, 7–10. [Google Scholar]
- Zheng, S.; Liu, X.; Cheng, N.; Dai, M.; Li, H.; Li, J.; Kang, F.; Wang, M.; Ren, X. Association Between Air Pollution and Hospitalization due to Malignant Neoplasms. J. Environ. Occup. Med. 2016, 33, 20–25. (In Chinese) [Google Scholar]
- Rodríguez, M.X.V.; León, C.J. Altruism and the economic values of environmental and social policies. Environ. Resour. Econ. 2004, 28, 233–249. [Google Scholar] [CrossRef]
- Banfi, S.; Filippini, M.; Horehájová, A. Using a choice experiment to estimate the benefits of a reduction of externalities in urban areas with special focus on electro smog. Appl. Econ. 2012, 44, 387–397. [Google Scholar] [CrossRef]
- Yoo, S.-H.; Kwak, S.-J.; Lee, J.-S. Using a choice experiment to measure the environmental costs of air pollution impacts in Seoul. J. Environ. Manag. 2008, 86, 308–318. [Google Scholar] [CrossRef]
- Tsuge, T.; Kishimoto, A.; Takeuchi, K. A choice experiment approach to the valuation of mortality. J. Risk Uncertain. 2005, 31, 73–95. [Google Scholar] [CrossRef]
- Utell, M.J.; Frampton, M.W. Acute Health Effects of Ambient Air Pollution: The Ultrafine Particle Hypothesis. J. Aero. Med. 2000, 13, 355–359. [Google Scholar] [CrossRef]
- Bresnahan, B.W.; Dickie, M.; Gerking, S. Averting behavior and urban air pollution. Land Econ. 1997, 73, 340–357. [Google Scholar] [CrossRef]
- Dickie, M.; Gerking, S. Valuation of Environmental Risks to Children’s Health; Department of Economics, University of Central Florida: Orlando, FL, USA, 2003. [Google Scholar]
- Folmer, H.; Johansson-Stenman, O. Does environmental economics produce aeroplanes without engines? on the need for an environmental social science. Environ. Res. Econ. 2001, 48, 337–361. [Google Scholar] [CrossRef]
- Folmer, H. Why sociology is better conditioned to explain economic behaviour than economics. Kyklos 2009, 62, 258–274. [Google Scholar] [CrossRef]
- Um, M.-J.; Kwak, S.-J.; Kim, T.-Y. Estimating willingness to pay for improved drinking water quality using averting behavior method with perception measure. Environ. Resour. Econ. 2002, 21, 285–300. [Google Scholar] [CrossRef]
- Temme, D.; Paulssen, M.; Dannewald, T. Incorporating latent variables into discrete choice models: A simultaneous estimation approach using sem software. Bus. Res. 2008, 1, 220–237. [Google Scholar] [CrossRef]
- Johnson, F.R.; Banzhaf, M.R.; Desvousges, W.H. Willingness to pay for improved respiratory and cardiovascular health: A multiple-format, stated-preference approach. Health Econ. 2000, 9, 295–317. [Google Scholar] [CrossRef]
- Sandor, Z.; Wedel, M. Designing conjoint choice experiments using managers’ prior beliefs. J. Mark. Res. 2001, 38, 430–444. [Google Scholar] [CrossRef]
- Costilla-Esquivel, A.; Corona-Villavicencio, F.; Velasco-Castañón, J.G.; Medina-De La Garza, C.E.; Martinez-Villarreal, R.T.; Cortes-Hernandez, D.E.; Gonzalez-Farias, G. A relationship between acute respiratory illnesses and weather. Epidemiol. Infect. 2014, 142, 1375–1383. [Google Scholar] [CrossRef]
- Davis, R.E.; Enfield, K.B. Respiratory hospital admissions and weather changes: A retrospective study in Charlottesville, Virginia, USA. Int. J. Biometeorol. 2018, 62, 1015–1025. [Google Scholar] [CrossRef]
- Dickie, M.; Messman, V.L. Parental altruism and the value of avoiding acute illness: Are kids worth more than parents? J. Environ. Econ. Manag. 2004, 48, 1146–1174. [Google Scholar] [CrossRef]
- Menon, G.; Raghubir, P.; Agrawal, N. Health Risk Perceptions and Consumer Psychology. In Handbook of Consumer Psychology; Haugtvedt, C.P., Herr, P.M., Kardes, F.R., Eds.; Taylaor & Francis Group, LLC: New York, NY, USA, 2008; pp. 981–1010. [Google Scholar]
- Nauges, C.; Van Den Berg, C. Perception of Health Risk and Averting Behavior: An Analysis of Household Water Consumption in Southwest Srilanka; TSE Working Paper; Toulouse School of Economics (TSE): Toulouse, France, 2009. [Google Scholar]
- Ferrer, R.A.; Klein, W.M. Risk perceptions and health behavior. Curr. Opin. Psychol. 2015, 5, 85–89. [Google Scholar] [CrossRef]
- Sjöberg, L.; Moen, B.-E.; Rundmo, T. Explaining Risk Perception; An Evaluation of the Psychometric Paradigm in Risk Perception Research; C Rotunde: Trondheim, Norway, 2004. [Google Scholar]
- El-Toukhy, S. Parsing susceptibility and severity dimensions of health risk perceptions. J. Health Commun. 2015, 20, 499–511. [Google Scholar] [CrossRef] [PubMed]
- Train, K. Halton Sequences for Mixed Logit; UCB: Berkeley, CA, USA, 2000. [Google Scholar]
- McFadden, D.; Train, K. Mixed MNL models for discrete response. J. Appl. Econom. 2000, 15, 447–470. [Google Scholar] [CrossRef]
- Anastasopoulos, P.C.; Mannering, F.L. An empirical assessment of fixed and random parameter logit models using crash- and non-crash-specific injury data. Accid. Anal. Prev. 2011, 43, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- McFadden, D. Conditional Logit Analysis of Qualitative Choice Behavior; UCB: Berkeley, CA, USA, 1973. [Google Scholar]
- Hanley, N.; Mourato, S.; Wright, R.E. Choice modelling approaches: A superior alternative for environmental valuatioin? J. Econ. Surv. 2001, 15, 435–462. [Google Scholar] [CrossRef]
- Revelt, D.; Train, K. Mixed logit with repeated choices: Households’ choices of appliance efficiency level. Rev. Econ. Stat. 1998, 80, 647–657. [Google Scholar] [CrossRef]
- Hajivassiliou, V.; McFadden, D.; Ruud, P. Simulation of multivariate normal rectangle probabilities and their derivatives theoretical and computational results. J. Econom. 1996, 72, 85–134. [Google Scholar] [CrossRef]
- Lusk, J.L.; Schroeder, T.C. Are choice experiments incentive compatible? A test with quality differentiated beef steaks. Am. J. Agric. Econ. 2004, 86, 467–482. [Google Scholar] [CrossRef]
- Bech, M.; Gyrd-Hansen, D. Effects coding in discrete choice experiments. Health Econ. 2005, 14, 1079–1083. [Google Scholar] [CrossRef]
- Pedhazur, E.J. Multiple Regression in Behavioral Research, 3rd ed.; Holt: New York, NY, USA, 1997. [Google Scholar]
- Scarpa, R.; Rose, J.M. Design efficiency for non-market valuation with choice modelling: How to measure it, what to report and why. Aust. J. Agric. Resour. Econ. 2008, 52, 253–282. [Google Scholar] [CrossRef]
- JEQMR. Jinchuan Environmental Quality Monitoring Report; Jinchuan Environmental Protection Bureau: Jinchuan, China, 2011. (In Chinese) [Google Scholar]
- Li, Z.; Folmer, H.; Xue, J. To what extent does air pollution affect happiness? The case of the Jinchuan mining area, China. Ecol. Econ. 2014, 99, 88–99. [Google Scholar] [CrossRef]
- Fox, J.T.; Il Kim, K.; Ryan, S.P.; Bajari, P. The random coefficients logit model is identified. J. Econom. 2012, 166, 204–212. [Google Scholar] [CrossRef]
- Fox, J.T. Semiparametric estimation of multinomial discrete-choice models using a subset of choices. RAND J. Econ. 2007, 38, 1002–1019. [Google Scholar] [CrossRef]
- Abdel-Aty, M. Analysis of driver injury severity levels at multiple locations using ordered probit models. J. Saf. Res. 2003, 34, 597–603. [Google Scholar] [CrossRef] [PubMed]
- O’donnell, C.J.; Connor, D.H. Predicting the severity of motor vehicle accident injuries using models of ordered multiple choice. Accid. Anal. Prev. 1996, 28, 739–753. [Google Scholar] [CrossRef]
- O’Neal, P.W. Motivation of Health Behavior; Nova Publishers: New York, NY, USA, 2007. [Google Scholar]
| Attribute | Levels of Attributes | Description |
|---|---|---|
| Illness | (1) Acute upper respiratory tract infection | Sneezing, a runny nose, cough and fever |
| (2) Acute Bronchitis | Cough, fever, burning or dull pain in the chest, wheezing. | |
| (3) Acute Pneumonia | Chest pain, fever, and difficulty breathing. | |
| Duration (days) | (1) 5 | 5-day episode |
| (2) 9 | 9-day episode | |
| (3) 15 | 15-day episode | |
| Activity Restriction | (1) No Limitation | No physical limitations nor restrictions of activities |
| (2) At home | Stay in the house, without social or recreational activities | |
| (3) In Hospital | In hospital and help needed to take care of oneself | |
| Price of cure (annual) | (1) 100 RMB | |
| (2) 300 RMB | ||
| (3) 500 RMB |
| Alternatives | A | B | C | |
|---|---|---|---|---|
| Attributes | ||||
| Disease | Acute Pneumonia | Acute Bronchitis | I don’t want to purchase either | |
| Duration | 5-day episode | 9-day episode | ||
| Daily activity restriction | At home | At home | ||
| Price of cure (annual) | 300 RMB | 500 RMB | ||
| Which alternative do you prefer to purchase | ||||
| Variables | Min | Max | Mean | S.D. |
|---|---|---|---|---|
| Age | 21 | 78 | 44.11 | 11.4 |
| Family size | 1 | 6 | 3 | 0.78 |
| Family health experience | 0 | 1 | 0.33 | 0.48 |
| Exposure | 0 | 7 | 2 | 1.53 |
| Hazardousness | 1 | 10 | 7.46 | 1.51 |
| Education | % | Work environment | % | |
| Primary school | 6.30% | Non-JMC employee (reference case) | 59.55% | |
| Middle school | 23.60% | Miners and smelter workers of JMC (MS) | 18.18% | |
| High school | 25.30% | JMC employee, but not miner or smelter worker (NMS) | 22.27% | |
| Vocational school | 25.30% | Household Income (RMB per month) | % | |
| Bachelor’s degree | 19.10% | 1000–2000 | 4.70% | |
| Master’s degree | 0.40% | 2000–3000 | 15.30% | |
| 3000–4000 | 18.30% | |||
| Proximity to the pollution source | % | 4000–5000 | 19.10% | |
| Nearby smelting plants, severe air pollution (SAP) | 29.60% | 5000–6000 | 20.90% | |
| Medium distance, medium air pollution (MAP) | 29.80% | 6000–7000 | 13.00% | |
| Far away from smelting plants, light air pollution (LAP) | 40.60% | More than 7000 | 8.60% | |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|
| Ordered-RPL Model with Exposure and Hazardousness | Ordered-RPL Model without Exposure and Hazardousness | Unordered-RPL Model with Exposure and Hazardousness | ||||
| Variables | Coefficient | T-Value | Coefficient | T-Value | Coefficient | T-Value |
| Acute upper respiratory tract infection * ln(duration + 1) (AI*LD) | 0.106 | - | 0.101 | - | −0.047 | - |
| S.D. | - | - | - | - | - | - |
| Acute Bronchitis * ln(Duration + 1) (AB*LD) | −0.057 ** | −2.067 | −0.061 ** | −2.205 | −0.038 | −1.381 |
| S.D. | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Acute Pneumonia * ln(Duration + 1) (AP*LD) | −0.049 * | −1.722 | −0.050 * | −1.757 | 0.009 | 0.354 |
| S.D. | 0.489 *** | 13.788 | 0.481 *** | 13.508 | 0.445 *** | 12.720 |
| No Limitation (NL) | 0.661 | - | 0.715 | - | 0.698 | - |
| S.D. | - | - | - | - | - | - |
| At home (AH) | −0.040 | −0.069 | −0.040 | −0.073 | 0.087 | 0.151 |
| S.D. | 0.000 | 0.000 | 0.000 | 0.000 | −0.002 | 0.000 |
| In hospital (IH) | −0.621 *** | −5.874 | −0.675 *** | −6.098 | −0.611 *** | −5.605 |
| S.D. | 1.545 *** | 8.618 | 1.607 *** | 8.889 | 1.622 *** | 9.551 |
| Price | 0.037 *** | 5.383 | 0.037 *** | 5.490 | 0.007 ** | 2.130 |
| 0.226 *** | 4.934 | 0.218 *** | 4.623 | |||
| 0.175 **** | 4.238 | 0.190 *** | 4.520 | |||
| −0.147 *** | −9.583 | −0.148 *** | −9.289 | |||
| −0.085 *** | −6.079 | −0.125 *** | −8.857 | |||
| −0.134 **** | −3.623 | −0.108 *** | −2.865 | |||
| −0.086 *** | −2.580 | −0.091 *** | −2.726 | |||
| −0.044 *** | −3.178 | −0.030 ** | −2.144 | |||
| −0.017 | −1.327 | −0.024 * | −1.853 | |||
| 0.139 *** | 6.251 | 0.087 *** | 3.961 | |||
| 0.086 *** | 4.406 | 0.046 ** | 2.465 | |||
| 0.161 | 1.503 | 0.117 | 1.096 | 0.308 *** | 2.882 | |
| 0.563 *** | 5.613 | 0.533 *** | 5.352 | 0.434 *** | 4.438 | |
| −0.342 *** | −5.039 | −0.296 *** | −4.346 | −0.357 *** | −5.200 | |
| −0.294 *** | −4.583 | −0.256 *** | −4.016 | −0.333 *** | −5.340 | |
| −0.056 | −1.123 | −0.077 | −1.553 | −0.012 | −0.243 | |
| 0.097 ** | 2.152 | 0.082 * | 1.842 | 0.030 | 0.682 | |
| 0.259 *** | 7.207 | 0.243 *** | 6.968 | 0.305 *** | 8.605 | |
| 0.396 *** | 11.557 | 0.386 *** | 11.522 | 0.355 *** | 10.706 | |
| −0.267 *** | −5.341 | −0.250 *** | −5.182 | −0.315 *** | −6.345 | |
| −0.352 *** | −7.654 | −0.338 *** | −7.610 | −0.333 *** | −7.363 | |
| 0.309 *** | 2.032 | 0.221 | 1.512 | 0.291 * | 1.921 | |
| 0.275 ** | 1.993 | 0.221 * | 1.657 | 0.236 * | 1.709 | |
| −0.031 | −0.237 | −0.010 | −0.078 | −0.153 | −1.170 | |
| −0.441 *** | −3.491 | −0.422 *** | −3.342 | −0.304 ** | −2.504 | |
| −0.081 | −0.713 | −0.036 | −0.325 | 0.072 | 0.647 | |
| 0.278 *** | 2.630 | 0.328 *** | 3.208 | 0.184 * | 1.797 | |
| N | 759 | 759 | 759 | |||
| Log-likelihood | −4139 | −4195.7 | −4206.7 | |||
| McFadden R square | 0.106 | 0.094 | 0.091 | |||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|
| Variables | Lightly Polluted Areas | T-Value | Moderate Polluted Areas | T-Value | Severely Polluted Areas | T-Value |
| Acute upper respiratory tract infection * ln(duration + 1) (AI*LD) | 0.091 | - | 0.175 | - | 0.087 | - |
| Acute Bronchitis * ln(Duration + 1) (AB*LD) | −0.051 | −1.4435 | −0.069 | −1.0497 | −0.055 | −0.8611 |
| SD | 0.000 | 0.0000 | 0.001 | 0.0002 | 0.000 | 0.0001 |
| Acute Pneumonia * ln(Duration + 1) (AP*LD) | −0.040 | −1.0864 | −0.106 | −1.5615 | −0.032 | −0.4920 |
| S.D | 0.478 ** | 10.7158 | 0.589 *** | 6.6072 | 0.462 *** | 5.9455 |
| No Limitation (NL) | 0.582 | - | 0.683 | - | 0.918 | - |
| At home (AH) | −0.007 | −0.0091 | −0.087 | −0.0639 | −0.073 | −0.0578 |
| S.D | 0.000 | 0.0001 | 0.003 | 0.0004 | 0.007 | 0.0009 |
| In hospital (IH) | −0.575 *** | −4.3801 | −0.596 *** | −2.7580 | −0.845 *** | −3.0156 |
| S.D | 1.441 *** | 6.1734 | 1.667 *** | 4.2456 | 2.051 *** | 5.2880 |
| Price | 0.033 *** | 3.8242 | 0.046 *** | 2.5976 | 0.034 ** | 2.1298 |
| 0.338 *** | 5.3933 | 0.472 *** | 3.5962 | −0.138 | −0.9936 | |
| 0.188 *** | 3.5165 | 0.492 *** | 4.6626 | −0.072 | −0.5175 | |
| −0.174 *** | −7.5286 | −0.208 *** | −5.4870 | −0.028 | −0.3514 | |
| −0.068 *** | −3.4167 | −0.185 *** | −5.7982 | 0.046 | 0.5995 | |
| −0.208 *** | −4.2627 | −0.245 * | 1.6711 | 0.150 | 1.2373 | |
| −0.065 | −1.5533 | −0.332 ** | −2.4187 | 0.108 | 0.9257 | |
| −0.065 *** | −4.0336 | −0.050 | −0.6199 | 0.077 | 1.0756 | |
| −0.013 | −0.9055 | −0.051 | −0.6646 | 0.051 | 0.7804 | |
| 0.230 *** | 6.1769 | 0.103 | 1.6321 | −0.163 | −1.5038 | |
| 0.138 *** | 4.6727 | −0.007 | −0.1060 | −0.136 | −1.2492 | |
| −0.079 | −0.5857 | −0.616 * | −1.7600 | 1.745 *** | 5.0478 | |
| 0.268 ** | 2.1420 | −0.275 | −0.8729 | 2.626 *** | 7.5509 | |
| −0.312 *** | −3.8581 | 0.151 | 0.5283 | −0.902 *** | −3.4883 | |
| −0.242 *** | −3.2633 | 0.148 | 0.5275 | −0.887 *** | −3.1262 | |
| 0.002 | 0.0319 | −0.352 ** | −2.1124 | −0.314 ** | −2.2428 | |
| 0.151 ** | 2.6563 | −0.242 * | −1.6921 | −0.153 | −1.1751 | |
| 0.269 *** | 6.0633 | 0.395 *** | 3.5805 | 0.349 *** | 3.4411 | |
| 0.392 *** | 9.3348 | 0.422 *** | 4.0159 | 0.836 *** | 8.1224 | |
| −0.264 *** | −4.4248 | −0.396 *** | −2.6258 | −0.083 | −0.4215 | |
| −0.310 *** | −5.6574 | −0.434 *** | −2.9395 | −0.353 ** | −2.0753 | |
| −0.20321 | −1.3685 | −1.357 *** | −3.4844 | 1.415 *** | 5.0928 | |
| 0.230096 * | 1.6857 | −1.083 *** | −2.9658 | 2.034 *** | 7.1594 | |
| N | 220 | 221 | 318 | |||
| Log-likelihood | −2488.4 | −773.87 | −743.78 | |||
| McFadden R square | 0.110 | 0.140 | 0.184 |
| 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| Disease | Duration | Activity Restriction Level | ||
| No Limitation | At Home | In Hospital | ||
| Acute upper respiratory tract infection (AI) | 5 | 0 | 0 | - |
| 9 | 0 | 0 | - | |
| 15 | 0 | 0 | - | |
| Acute bronchitis (AB) | 5 | 0 | 3.833 | 19.551 |
| 9 | 0 | 4.619 | 20.337 | |
| 15 | 0 | 5.342 | 21.060 | |
| Acute pneumonia (AP) | 5 | 0 | 3.468 | 19.186 |
| 9 | 0 | 4.150 | 19.868 | |
| 15 | 0 | 4.778 | 20.495 | |
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z. Valuing Acute Health Risks of Air Pollution in the Jinchuan Mining Area, China: A Choice Experiment with Perceived Exposure and Hazardousness as Co-Determinants. Int. J. Environ. Res. Public Health 2019, 16, 4563. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16224563
Li Z. Valuing Acute Health Risks of Air Pollution in the Jinchuan Mining Area, China: A Choice Experiment with Perceived Exposure and Hazardousness as Co-Determinants. International Journal of Environmental Research and Public Health. 2019; 16(22):4563. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16224563
Chicago/Turabian StyleLi, Zhengtao. 2019. "Valuing Acute Health Risks of Air Pollution in the Jinchuan Mining Area, China: A Choice Experiment with Perceived Exposure and Hazardousness as Co-Determinants" International Journal of Environmental Research and Public Health 16, no. 22: 4563. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16224563




