Implementation and Long-Term Outcomes of Organisational Health Literacy Interventions in Ireland and The Netherlands: A Longitudinal Mixed-Methods Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Setting and Sample
2.3. Implementation of the OHL-Interventions
2.3.1. Description of the Two OHL-Interventions
- The Irish intervention, “The Literacy Audit for Healthcare Settings” toolkit [31], included guidelines on health literacy friendly communication, and an OHL-assessment tool to assess communication barriers. The core OHL-assessment involves 57 questions, which are completed by professionals on paper about awareness of health literacy, signs and other devices for navigating premises, digital and print materials, and verbal communication. In addition, the OHL-intervention includes references to best practices in health literacy for organisations, such as the use of visuals in written materials and the ways to present numbers. The CDC Clear Communication Index [33] aligned with these requirements and was used to review written materials. In addition, the intervention refers to walking interviews [34] together with service users in order to assess the navigation from their perspective. The intervention was informed by literature for health literacy communication and is freely available online [31].
- In The Netherlands, the Quickscan Health Literacy Toolbox [32] included information on health literacy and organisational change processes, and an OHL-assessment tool to assess the components of navigation, oral communication, written print materials and digital communication, and an action planning format for implementation. Each OHL-assessment component consisted of a self-evaluation checklist for professionals and guides for observing and/or interviewing service users. The intervention was informed by a literature review on health literacy communication and a pilot-test in various Dutch hospitals [32,35,36].
2.3.2. Implementation of OHL-Interventions
Stage 1. Planning and Assessment
- -
- Navigation and signage within health settings
- -
- Interpersonal communication
- -
- Written print material
- -
- Digital content on websites.
Stage 2. Action Planning
Stage 3. Implementation of Actions Planned
2.4. Procedure and Measures
2.4.1. Stage 1
2.4.2. Stage 2
2.4.3. Stage 3
2.5. Analysis
3. Results
3.1. Organisation and Participant Characteristics
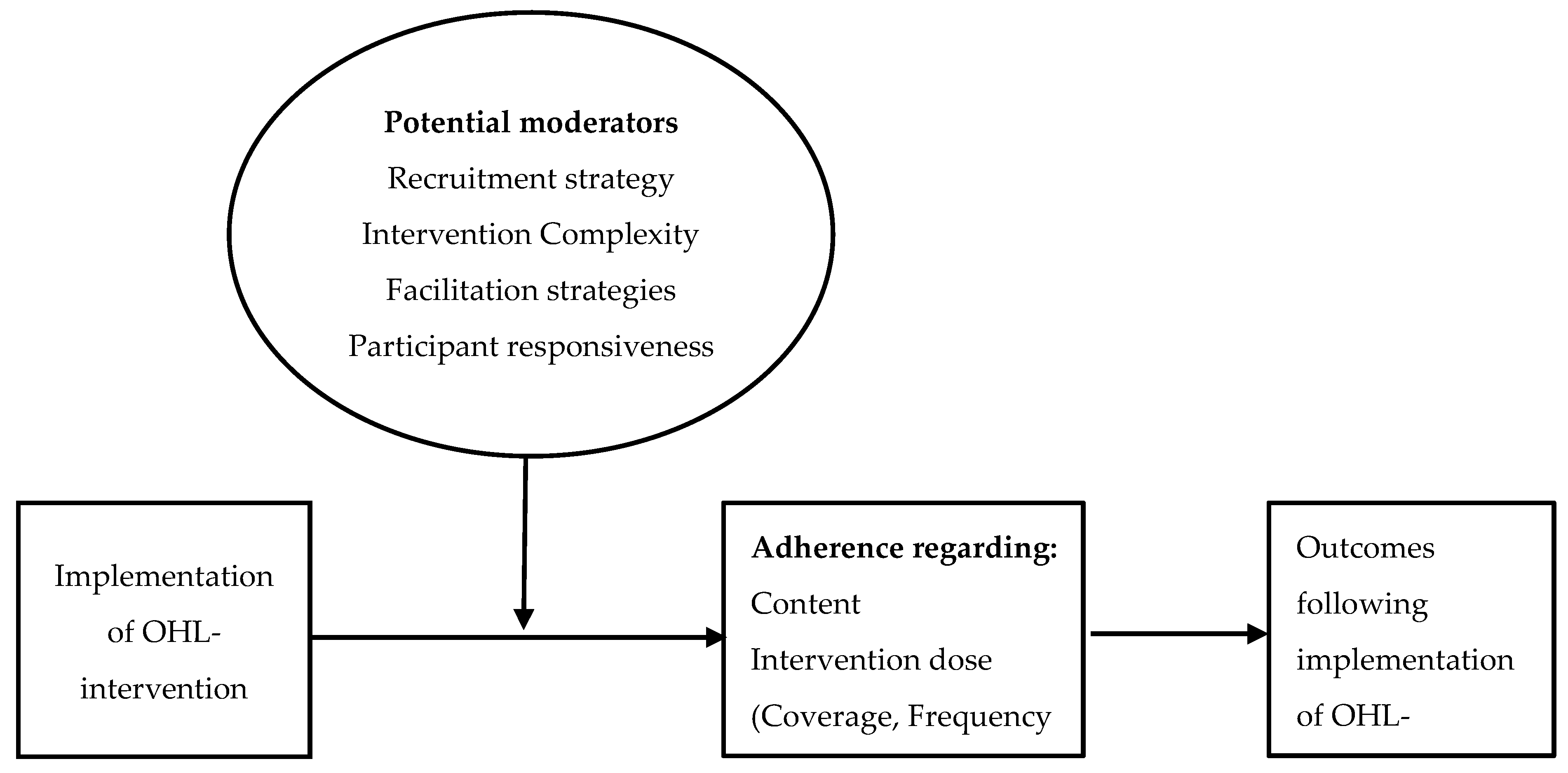
3.2. Implementation Fidelity
3.2.1. Stage 1. OHL Assessment
3.2.2. Stage 2 and 3
3.3. Moderators Influencing Implementation
3.3.1. Stage 1
3.3.2. Stage 2 and 3
3.4. Impact of OHL-Interventions
4. Discussion
4.1. Strengths and Weaknesses
4.2. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Williams, A.M.; Muir, K.W.; Rosdahl, J.A. Readability of Patient Education Materials in Ophthalmology: A Single-Institution Study and Systematic Review. BMC Ophthalmol. 2016, 16, 133. [Google Scholar] [CrossRef] [PubMed]
- Pires, C.; Vigário, M.; Cavaco, A. Readability of Medicinal Package Leaflets: A Systematic Review. Rev. Saude Publica 2015, 49, 4. [Google Scholar] [CrossRef] [PubMed]
- Groene, R.O.; Rudd, R.E. Results of a Feasibility Study to Assess the Health Literacy Environment: Navigation, Written, and Oral Communication in 10 Hospitals in Catalonia, Spain. J. Commun. Healthc. 2011, 4, 227–237. [Google Scholar] [CrossRef]
- Sørensen, K.; Pelikan, J.M.; Rothlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health Literacy in Europe: Comparative Results of the European Health Literacy Survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low Health Literacy and Health Outcomes: An Updated Systematic Review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Koh, H.K.; Baur, C.; Brach, C.; Harris, L.M.; Rowden, J.N. Toward a Systems Approach to Health Literacy Research. J. Health Commun. 2013, 18, 1–5. [Google Scholar] [CrossRef]
- Koh, H.K.; Brach, C.; Harris, L.M.; Parchman, M.L. A Proposed “health Literate Care Model” Would Constitute a Systems Approach to Improving Patients’ Engagement in Care. Health Aff. 2013, 32, 357–367. [Google Scholar] [CrossRef]
- Brach, C.; Keller, D.; Hernandez, L.M.; Baur, C.; Parker, R.; Schyve, P.; Lemerise, A.J.; Schillinger, D. Ten Attributes of Health Literate Health Care Organizations; Institute of Medicine, National Acacemy of Sciences: Washington, DC, USA, 2012. [Google Scholar]
- Annarumma, C.; Palumbo, R. Contextualizing Health Literacy to Health Care Organizations: Exploratory Insights. J. Health Manag. 2016, 18, 611–624. [Google Scholar] [CrossRef]
- Trezona, A.; Dodson, S.; Osborne, R.H. Development of the Organisational Health Literacy Responsiveness (Org-HLR) Framework in Collaboration with Health and Social Services Professionals. BMC Health Serv. Res. 2017, 17, 513. [Google Scholar] [CrossRef]
- Pelikan, J.M.; Dietscher, C. Warum Sollten Und Wie Können Krankenhäuser Ihre Organisationale Gesundheitskompetenz Verbessern? Bundesgesundheitsblatt-Gesundheitsforsch.-Gesundh. 2015, 58, 989–995. [Google Scholar] [CrossRef]
- Farmanova, E.; Bonneville, L.; Bouchard, L. Organizational Health Literacy: Review of Theories, Frameworks, Guides, and Implementation Issues. Inq. J. Health Care Organ. Provis. Financ. 2018, 55. [Google Scholar] [CrossRef]
- Lloyd, J.E.; Song, H.J.; Dennis, S.M.; Dunbar, N.; Harris, E.; Harris, M.F. A Paucity of Strategies for Developing Health Literate Organisations: A Systematic Review. PLoS ONE 2018, 13, e0195018. [Google Scholar] [CrossRef]
- O’Neal, K.S.; Crosby, K.M.; Miller, M.J.; Murray, K.A.; Condren, M.E. Assessing Health Literacy Practices in a Community Pharmacy Environment: Experiences Using the AHRQ Pharmacy Health Literacy Assessment Tool. Res. Soc. Adm. Pharm. 2013, 9, 564–596. [Google Scholar] [CrossRef]
- Gazmararian, J.A.; Beditz, K.; Pisano, S.; Carreón, R. The Development of a Health Literacy Assessment Tool for Health Plans. J. Health Commun. 2010, 15, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Shoemaker, S.J.; Staub-DeLong, L.; Wasserman, M.; Spranca, M. Factors Affecting Adoption and Implementation of AHRQ Health Literacy Tools in Pharmacies. Res. Soc. Adm. Pharm. 2013, 9, 553–563. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, A.; Batterham, R.W.; Dodson, S.; Astbury, B.; Elsworth, G.R.; McPhee, C.; Jacobson, J.; Buchbinder, R.; Osborne, R.H. Systematic Development and Implementation of Interventions to OPtimise Health Literacy and Access (Ophelia). BMC Public Health 2017, 17, 230. [Google Scholar] [CrossRef] [PubMed]
- Weaver, N.L.; Wray, R.J.; Zellin, S.; Gautam, K.; Jupka, K. Advancing Organizational Health Literacy in Health Care Organizations Serving High-Needs Populations: A Case Study. J. Health Commun. 2012, 17, 55–66. [Google Scholar] [CrossRef] [PubMed]
- DeWalt, D.A.; Broucksou, K.A.; Hawk, V.; Brach, C.; Hink, A.; Rudd, R.; Callahan, L. Developing and Testing the Health Literacy Universal Precautions Toolkit. Nurs. Outlook 2011, 59, 85–94. [Google Scholar] [CrossRef]
- Shoemaker, S.J.; Wolf, M.S.; Brach, C. Development of the Patient Education Materials Assessment Tool (PEMAT): A New Measure of Understandability and Actionability for Print and Audiovisual Patient Information. Patient Educ. Couns. 2014, 96, 395–403. [Google Scholar] [CrossRef]
- Weiss, B.D.; Brega, A.G.; LeBlanc, W.G.; Mabachi, N.M.; Barnard, J.; Albright, K.; Cifuentes, M.; Brach, C.; West, D.R. Improving the Effectiveness of Medication Review: Guidance from the Health Literacy Universal Precautions Toolkit. J. Am. Board Fam. Med. 2016, 29, 18–23. [Google Scholar] [CrossRef]
- Kripalani, S.; Robertson, R.; Love-Ghaffari, M.H.; Henderson, L.E.; Praska, J.; Strawder, A.; Katz, M.G.; Jacobson, T.A. Development of an Illustrated Medication Schedule as a Low-Literacy Patient Education Tool. Patient Educ. Couns. 2007, 66, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Mabachi, N.M.; Cifuentes, M.; Barnard, J.; Brega, A.G.; Albright, K.; Weiss, B.D.; Brach, C.; West, D. Demonstration of the Health Literacy Universal Precautions Toolkit. J. Ambul. Care Manag. 2016, 39, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Brega, A.G.; Freedman, M.A.G.; Leblanc, W.G.; Barnard, J.; Mabachi, N.M.; Cifuentes, M.; Albright, K.; Weiss, B.D.; Brach, C.; West, D.R. Using the Health Literacy Universal Precautions Toolkit to Improve the Quality of Patient Materials. J. Health Commun. 2015, 20, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Vellar, L.; Mastroianni, F.; Lambert, K. Embedding Health Literacy into Health Systems: A Case Study of a Regional Health Service. Aust. Heal. Rev. 2016, 41, 621–625. [Google Scholar] [CrossRef]
- Mastroianni, F.; Chen, Y.C.; Vellar, L.; Cvejic, E.; Smith, J.K.; McCaffery, K.J.; Muscat, D.M. Implementation of an Organisation-Wide Health Literacy Approach to Improve the Understandability and Actionability of Patient Information and Education Materials: A Pre-Post Effectiveness Study. Patient Educ. Couns. 2019, 102, 1656–1661. [Google Scholar] [CrossRef]
- Carroll, C.; Patterson, M.; Wood, S.; Booth, A.; Rick, J.; Balain, S. A Conceptual Framework for Implementation Fidelity. Implement. Sci. 2007, 2, 40. [Google Scholar] [CrossRef]
- Hasson, H. Systematic Evaluation of Implementation Fidelity of Complex Interventions in Health and Social Care. Implement. Sci. 2010, 5, 2–9. [Google Scholar] [CrossRef]
- Blankenship, K.M.; Friedman, S.R.; Dworkin, S.; Mantell, J.E. Structural Interventions: Concepts, Challenges and Opportunities for Research. J. Urban Health 2006, 83, 59–72. [Google Scholar] [CrossRef]
- Hawe, P.; Shiell, A.; Riley, T. Complex Interventions: How “out of Control” Can a Randomised Controlled Trial Be? BMJ 2004, 328, 1561–1563. [Google Scholar] [CrossRef]
- Lynch, J. Literacy Audit for Health Care Settings; National Adult Literacy Agency (NALA): Dublin, Ireland, 2009. [Google Scholar]
- Bax, J. Quickscan Health Literacy Toolbox; Dutch Institute for Healthcare Improvement (CBO): Utrecht, The Netherlands, 2014. [Google Scholar]
- Baur, C.; Prue, C. The CDC Clear Communication Index Is a New Evidence-Based Tool to Prepare and Review Health Information. Health Promot. Pract. 2014, 15, 629–637. [Google Scholar] [CrossRef]
- Rudd, R.E. The Health Literacy Environment Activity Packet First Impressions & Walking Interview Eliminating Barriers–Increasing Access; Online Tools: Harvard University: Cambridge, MA, USA, 2010. [Google Scholar]
- Tijhuis, K. Een Evaluatie van Het Friese Pilotproject ‘Quickscan Gezondheidsvaardigheden’; Wageningen University & Research: Wageningen, The Netherlands, 2014. [Google Scholar]
- De Bresser, A. Zelfevaluatie of Observatie: Een Meetinstrument Voor de Mondelinge Communicatie in de Spreekkamer; Utrecht University: Utrecht, The Netherlands, 2013. [Google Scholar]
- Chew, L.D.; Griffin, J.M.; Partin, M.R.; Noorbaloochi, S.; Grill, J.P.; Snyder, A.; Bradley, K.A.; Nugent, S.M.; Baines, A.D.; VanRyn, M. Validation of Screening Questions for Limited Health Literacy in a Large VA Outpatient Population. J. Gen. Intern. Med. 2008, 23, 561–566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durlak, J.A.; DuPre, E.P. Implementation Matters: A Review of Research on the Influence of Implementation on Program Outcomes and the Factors Affecting Implementation. Am. J. Community Psychol. 2008, 41, 327–350. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Hasson, H.; Blomberg, S.; Duner, A. Fidelity and Moderating Factors in Complex Interventions: A Case Study of a Continuum of Care Program for Frail Elderly People in Health and Social Care. Implement. Sci. 2012, 7, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schinckus, L.; Van den Broucke, S.; Housiaux, M. Assessment of Implementation Fidelity in Diabetes Self-Management Education Programs: A Systematic Review. Patient Educ. Couns. 2014, 96, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Willis, C.D.; Saul, J.E.; Bitz, J.; Pompu, K.; Best, A.; Jackson, B. Improving Organizational Capacity to Address Health Literacy in Public Health: A Rapid Realist Review. Public Health 2014, 128, 515–524. [Google Scholar] [CrossRef]
| Implementation Stage | Implementation Activities of OHL-Intervention in Hospitals | Research Measurements |
|---|---|---|
| 1. Planning and assessment (month 0–6) | 1. Project planning and conducting of OHL-assessment | 1. Questionnaire (after 6 months) |
| 2. Action planning(month 7–8) | 2. Action planning based on OHL-assessment outcomes | 2. Questionnaire and interviews with project committees(after 8 months) |
| 3. Implementation of actions (month 9–18) | 3. Implementation of the actions to improve communication | 3. Interviews with implementation coordinators (after 18 months) |
| Characteristics of the Hospital Setting | Setting 1 (IRL 1) Teaching Hospital | Setting 2 (NLD 2) Academic Rehabilitation Centre | Setting 3 (NLD) General Hospital | Setting 4 (NLD) General Hospital |
|---|---|---|---|---|
| Number of professionals (fulltime equivalent) | 2500 | 450 | 680 | 2670 |
| Number of beds | 540 | 120 | 313 | 468 |
| Questionnaire N in stage 1 (professionals involved in OHL-assessment) | 7 | 5 | 8 | 1 |
| Questionnaire N in stage 2 (project committee). | 5 | 4 | 3 | 1 |
| Interviews N in stage 2 (project committee) | 10 | 5 | 5 | 1 |
| Interviews N in stage 3 (implementation coordinators) | 2 | 2 | 1 | 1 |
| Professional disciplines (project committee) | ||||
| 1 | 1 | 2 | - |
| 4 | - | 3 | - |
| 3 | - | 1 | - |
| 1 | 2 | 1 | 1 |
| 1 | 2 | 1 | - |
| Navigation and Signage | Interpersonal Communication | Written Print Material | Digital Content | |||||
|---|---|---|---|---|---|---|---|---|
| Assessment | Actions | Assessment | Actions | Assessment | Actions | Assessment | Actions | |
| Setting 1 | X 1 | - | X | - | X | X | X | - |
| Setting 2 | - | - | X | X | X | X | - | - |
| Setting 3 | X | - | - | - | X | X | X | X |
| Setting 4 | - | - | - | - | - | - | X | X |
| Moderators | Illustrative Quotes from Study Respondents |
|---|---|
| Stage 1 Recruitment | “Ehm what applies to us is that it is filled in by very different people, from very different functions. And that you just do not have the opportunity in your daily work to get these people together in this way about one and the same subject”. (NLD 1 setting 2, participant 5, interview) |
| Facilitation strategies | “… and if you want you can get everything from there (from the internet) and implement it yourself but in practice it is much more awkward. Of course, it often does not work that way. And that is purely because you need a coordinator, and sometimes you will need an authority that is qualified, shall we say. Ehm that guides you or assigns the right people”. (NLD setting 3, participant 12, interview). |
| Intervention complexity | “Well, my experience is that it is a lot. That I, well yeah, that it would be nicer if it [the tool] were digitally better available. And those questionnaires were more simplified and a final results tool was added so that you could process your results more easily”. (NLD setting 3, participant 13, interview) |
| Participant responsiveness | “I think it’s been very useful, great to focus our attention on health literacy even though we knew there was work needed to be done about it. I suppose it kind of focused us and gave us a bit of momentum to get working on it. It was very practical and very clear. Everybody is very interested in it”. (IRL 2, setting 1, participant 21, interview) |
| Stage 2 and 3 Quality of delivery | “Of course we have the results from the Quickscan. And if you approach that very narrowly, you look very closely at the three leaflets we have scanned and the two letters and the oral checklists […]. But the effect of applying the Quickscan is that we simply see what is actually needed. We see that many things are going well, but that there are also points for improvement in this area. In fact, we want to embed that within the center”. (NLD, setting 2, participant 1, interview) |
| Contextual moderators: | |
| (1) Different organisational structures and procedures | “We are a centre but we have different departments. All different departments have different methods. So when we say this must be done differently, that could affect all kinds of different working systems. […] Sometimes it is bound to a computer system that we use”. (NLD, setting 2, participant 1, interview) |
| (2) Limited resources | “So this area of stuff is seen to be like that, it will cost money and it’s letting the dust settle, letting the sun dawn on that last chapter and that we can go at it again but it really has put projects like this, stopped them in their tracks. But I think if it’s done on a phased basis where it’s broken up into smaller mini projects I think it has a lot better chance of seeing the light of day again”. (IRL, setting 1, participant 18, interview) |
| (3) Embedding OHL-interventions into ongoing activities | “See where you can reinforce each other in this area. If you are going to do something as a stand-alone project, it can be done of course, but I think that has less chance of success. I think it is nice that you link it to, there is of course a lot of attention for self-management, of course, and it links to patient-centeredness. Hospitality, so it links to so many parts. And whatever you link it to; it will give you more opportunities to implement”. (NLD, setting 2, participant 1, follow up interview) |
| (4) Obtaining leadership support | “It’s very good! The general manager, the director of nursing, they are very ehm, you know, they are committed to this. They really are! Ehm, they feel it’s very worthwhile and like that it’s ehm, it’s a patient experience initiative as well”. (IRL, setting 1, participant 23, follow up interview) |
| Stage 1. Outcomes of the OHL-Intervention Assessment | Illustrative Quotes |
| Awareness of health literacy and related communication barriers (all settings). | “So it has made me stop, take off my work hat and […] look at it from a patient’s perspective. So it’s made me more aware and it’s made me very anxious to try and be part of doing something about it”. (IRL 1, setting 1, participant 22, interview) |
Written communication (settings 1, 2, and 3):
| “Well they (service users) were so clear about it. That they get far too much information, too many letters. And according to me, the letters also very often (contain) information that does not reach the customer at the right time, and contradictory messages in a letter and ehm well all sorts of things”. (NLD 2, setting 2, participant 2, interview) |
Navigation (settings 1 and 3):
| “I mean, if you were able to come to the hospital and walk around. It can be very confusing for people. And it’s quite a large building with a lot of different areas and no two signs are the same”. (IRL, setting 1, participant 23, follow up interview) |
Oral communication (settings 1 and 2):
| “If we use jargon, if we choose this, you also create a distance with the patient. Besides that, it is ineffective, because he does not always understand it”. (NLD, setting 2, participant 3, interview) |
Website (settings 1, 3 and 4):
| “Yes, because I also know that we said in advance, everyone scrolls, when you go to the website. […] Well not really. […] I saw this with those low-literate people, nobody scrolls. Everyone thinks this is it. And then there is a lot of information underneath”. (NLD, setting 4, participant 6, interview) |
| Stage 2 and 3. Organisational Changes Undertaken Following Action Plan | Illustrative Quotes |
| Organisation wide health literacy committee established (settings 1 and 2). | “Establishing the Health Literacy Committee was a big step. And then spreading the word about it. […] And all the hospitals in our group are very interested in it as well, ehm, because people do realise that it is very difficult for patients”. (IRL, setting 1, participant 23, follow up interview) |
| Extra employee to facilitate the embedding of health literacy in working procedures and professionals’ practice (settings 2). | “We have at least one employee for a year, so there is also a limitation in terms of employability. Hence, we also want to see as much as possible, which tools for example, we can already use for staff and administration, to train these people and provide them with skills. So that they can continue with it independently”. (NLD, setting 2, participant 1, follow up interview) |
| Health literacy policy and more user-friendly checklist to assess leaflets or letters (settings 1). | “The health literacy policy for the hospital, okay? So that people have a process to follow when they are developing not only information leaflets but I suppose any kind of (patient) information”. (IRL, setting 1, participant 21, follow up interview) |
Written communication (settings 1, 2, and 3):
| “Ehm, yes, they obviously cannot copy sentences, because every brochure is different. But (they can take over) the tone in which a brochure is written or the layout of a text on the website. […] So that there are a number of examples that people can continue with”. (NLD, Setting 2, Participant 5, follow up interview) |
| “So they did either four hours or half a day of plain English training. […] Yeah, I think I’d say 64 or 65 people at this stage that have been trained in plain English”. (IRL, setting 1, participant 21, follow up interview) |
| “So, what we looked at was our outpatients’ letters […] we revised those letters. Now that was a process of itself and we went, we passed them with some low literacy level groups and also high literacy level groups and we’ve kind of come back to the basics of who, what, why, where and when. Yes! So we changed about three or four letters. We have over 30 letters, okay?” (IRL, setting 1, participant 21, follow up interview) |
Digital communication (websites) (settings 3 and 4):
| “When people looked at the left in the navigation structure and when they were (looking at) a condition, they did not know exactly which treatment and what examination belonged to it. In terms of image, we made some adjustments. Another font and a different color, now it is clearer what belongs together”. (NLD, setting 4, participant 6, follow up interview) |
| Navigation (settings 1 and 3) | “Ehm, another thing we hoped to do but we didn’t get the money this time for it was a site map. You know, a simple map with all, we have quite a big site here and a lot of different buildings”. (IRL, setting 1, participant 23, follow up interview) |
| Oral communication (setting 2) | “I’m sure it will come in time […] But we definitely will look at the oral communication, but we’re not there or near to it”. (IRL, setting 1, participant 21, follow up interview) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaper, M.; Sixsmith, J.; Meijering, L.; Vervoordeldonk, J.; Doyle, P.; Barry, M.M.; de Winter, A.F.; Reijneveld, S.A. Implementation and Long-Term Outcomes of Organisational Health Literacy Interventions in Ireland and The Netherlands: A Longitudinal Mixed-Methods Study. Int. J. Environ. Res. Public Health 2019, 16, 4812. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16234812
Kaper M, Sixsmith J, Meijering L, Vervoordeldonk J, Doyle P, Barry MM, de Winter AF, Reijneveld SA. Implementation and Long-Term Outcomes of Organisational Health Literacy Interventions in Ireland and The Netherlands: A Longitudinal Mixed-Methods Study. International Journal of Environmental Research and Public Health. 2019; 16(23):4812. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16234812
Chicago/Turabian StyleKaper, Marise, Jane Sixsmith, Louise Meijering, Janine Vervoordeldonk, Priscilla Doyle, Margaret M. Barry, Andrea F. de Winter, and Sijmen A. Reijneveld. 2019. "Implementation and Long-Term Outcomes of Organisational Health Literacy Interventions in Ireland and The Netherlands: A Longitudinal Mixed-Methods Study" International Journal of Environmental Research and Public Health 16, no. 23: 4812. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16234812






