Feasibility of Ski Mountaineering for Patients Following a Total Knee Arthroplasty: A Descriptive Field Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
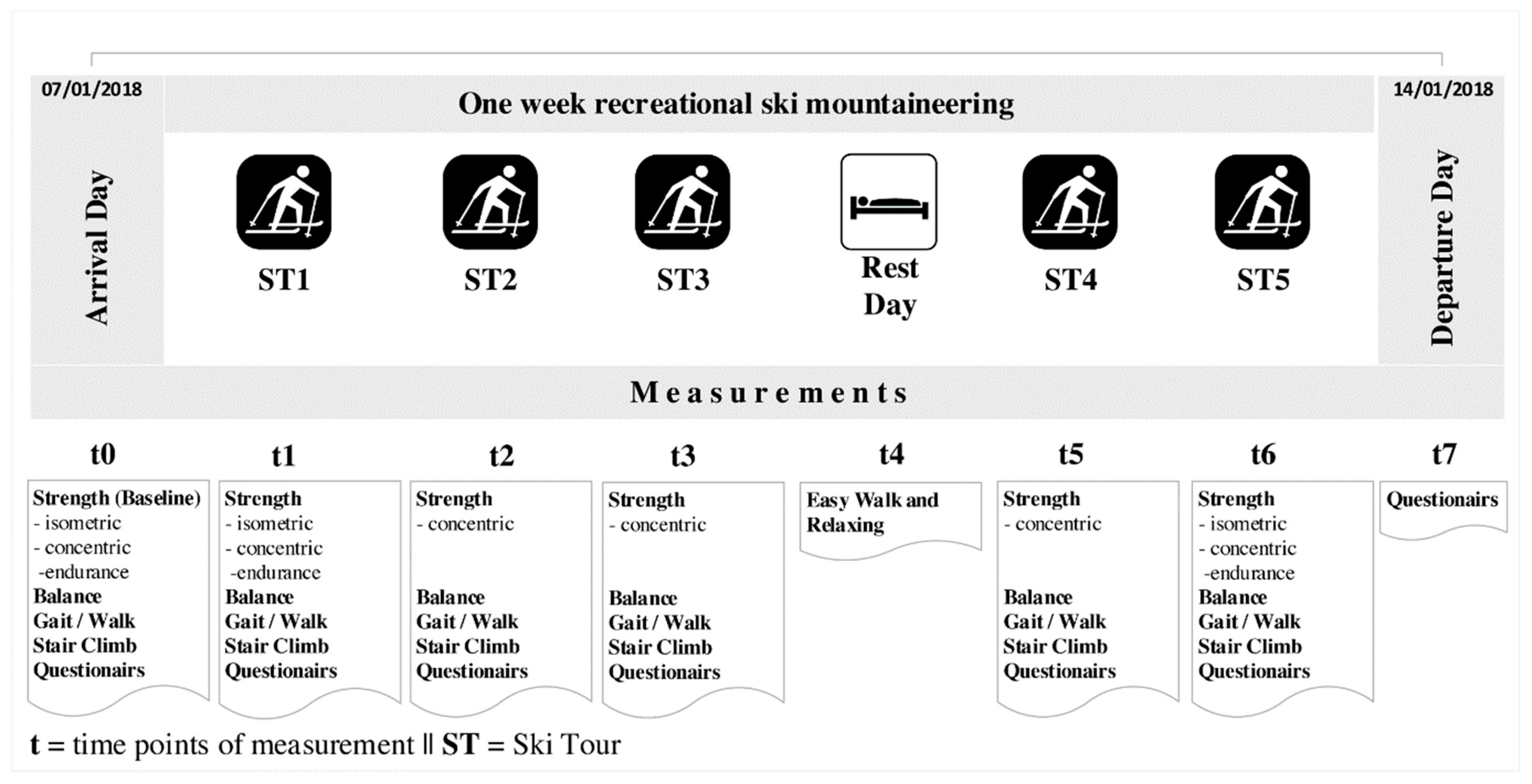
2.2. Study Design
2.3. Environmental Parameters of St. Johann/Tyrol
2.4. Measurements
2.5. Heart Rate Monitoring and Global Positioning System (GPS)-Tracking
2.6. Muscle Strength Measurements (Isokinetic Dynamometry)
2.7. Gait Analysis
2.8. Balance in One- and Two-Legged Stand
2.9. Stair Climb Test
2.10. Borg Scale
2.11. Feeling Scale (FS) and Felt Arousal Scale (FAS)
2.12. Recovery-Stress Questionnaire for Athletes: Shortened German Version (EBF 24)
2.13. Short Form 12 Health Survey (SF-12)
2.14. Mood Scale (Bf-SR)
2.15. Statistical Analysis
3. Results
3.1. Demographics and Patient Characteristics
3.2. Route Information and Exercise Load
3.3. Strength
3.4. Functional Abilities
3.5. Balance
3.6. Mental Health
4. Discussion
4.1. Consequences for Strength, Functional Abilities and Mood
4.2. Feasibility of Recreational Ski Mountaineering after TKA
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| Bf-SR | Mood Scale; German Befindlichkeits-Skala Revidierte Fassung |
| EBF 24 B/3 | Shortened German Version of the Recovery-Stress Questionnaire for athletes |
| FAS | Felt Arousal Scale |
| FS | Feeling Scale |
| MFT | Multifunktionale Trainingsgeräte (Multifunctional Training Equipment) |
| OA | Osteoarthritis |
| RESTQ-Sport | Recovery-Stress Questionnaire for athletes |
| RTE | Relative treatment effect |
| SF12/SF36 | Short form 12/36 Health Survey |
| TKA | Total knee arthroplasty |
Appendix A
| Arrival | Ski Tour 1 | Ski Tour 2 | Ski Tour 3 | Ski Tour 4 | Ski Tour 5 | |
|---|---|---|---|---|---|---|
| Day 1 | Day 2 | Day 3 | Day 4 | Day 6 | Day 7 | |
| Strength | ||||||
| Concentric maximal voluntary contraction | ||||||
| Concentric_Extensor_max (N·m) | 116.00 ± 45.50 | 120.00 ± 57.50 | 117.00 ± 44.50 | 117.50 ± 49.50 | 107.00 ± 38.75 | 119.50 ± 46.75 |
| Concentric_Flexor_max (N·m) | 83.50 ± 43.00 | 81.00 ± 46.00 | 92.50 ± 43.50 | 82.00 ± 41.00 | 78.50 ± 45.75 | 87.50 ± 26.50 |
| Concentric_Extensor_angle (degree) | 58.50 ± 5.00 | 55.50 ± 4.00 | 57.50 ± 11.00 | 59.00 ± 12.00 | 58.00 ± 15.50 | 57.50 ± 4.75 |
| Concentric_Flexor_angle (degree) | 34.50 ± 12.50 | 33.50 ± 5.75 | 34.50 ± 8.75 | 36.00 ± 8.50 | 35.00 ± 7.50 | 35.50 ± 8.00 |
| Isometric maximal voluntary contraction | ||||||
| Isometric_Extensor_max (N·m) | 134.50 ± 76.00 | 128.50 ± 87.00 | 132.00 ± 81.00 | |||
| Isometric_Flexor_max (N·m) | 70.50 ± 32.75 | 67.50 ± 27.75 | 70.00 ± 29.25 | |||
| Strength endurance (SE) | ||||||
| SE_Extensor_work (N·m) | 790.00 ± 571.50 | 666.00 ± 580.50 | 805.50 ± 435.00 | |||
| SE_Flexor_work (N·m) | 724.00 ± 356.50 | 638.50 ± 393.25 | 733.50 ± 335.50 | |||
| SE_Extensor_max (N·m) | 81.50 ± 51.00 | 82.00 ± 54.50 | 85.00 ± 44.00 | |||
| SE_Flexor_max (N·m) | 68.50 ± 35.50 | 71.50 ± 36.50 | 67.00 ± 34.00 | |||
| Balance (one and two legged stance) | ||||||
| S3-Check MFT | ||||||
| Stability Index (score) | 4.85 ± 1.75 | 4.80 ± 1.05 | 5.25 ± 2.20 | 4.75 ± 1.15 | 5.40 ± 1.58 | 5.50 ± 1.75 |
| Stability in relation to standard data (percent) | 93.50 ± 38.25 | 95.50 ± 22.50 | 85.50 ± 49.00 | 95.50 ± 26.00 | 81.50 ± 32.50 | 79.00 ± 37.00 |
| Sensorimotor Index (score) | 4.40 ± 1.50 | 4.00 ± 0.95 | 4.00 ± 1.83 | 4.20 ± 1.50 | 3.60 ± 1.55 | 4.50 ± 1.43 |
| Sensorimotor function in relation to standard data (percent) | 102.00 ± 30.75 | 111.00 ± 20.50 | 112.00 ± 42.75 | 107.50 ± 29.75 | 120.00 ± 34.50 | 101.00 ± 32.25 |
| Symmetry (deviation from horizontal plate position) | 52.00 ± 8.50 | 50.00 ± 9.50 | 47.50 ± 23.00 | 47.00 ± 13.25 | 47.00 ± 22.25 | 51.50 ± 17.75 |
| Deviation of 50 | 5.00 ± 3.75 | 4.00 ± 3.50 | 9.50 ± 14.25 | 5.50 ± 9.50 | 11.00 ± 12.75 | 8.00 ± 8.00 |
| Mobility Lab balance parameter | ||||||
| 95% Ellipse Sway Area (m2/s4) | 9.06 ± 6.07 | 6.23 ± 12.66 | 11.56 ± 12.68 | 10.64 ± 8.45 | 10.49 ± 12.68 | 7.89 ± 10.85 |
| Arrival | Ski Tour 1 | Ski Tour 2 | Ski Tour 3 | Ski Tour 4 | Ski Tour 5 | |
|---|---|---|---|---|---|---|
| Day 1 | Day 2 | Day 3 | Day 4 | Day 6 | Day 7 | |
| Mobility Lab gait parameters | ||||||
| CadenceTKA (steps per minute) | 116.06 ± 9.44 | 120.70 ± 13.52 | 116.44 ± 14.29 | 113.59 ± 9.08 | 118.49 ± 10.20 | 116.82 ± 10.56 |
| Cadence UL (steps per minute) | 114.92 ± 10.06 | 119.36 ± 12.05 | 116.17 ± 16.85 | 117.87 ± 7.98 | 118.14 ± 11.03 | 117.93 ± 11.81 |
| Stride length TKA (meter) | 1.29 ± 0.10 | 1.32 ± 0.15 | 1.31 ± 0.15 | 1.27 ± 0.10 | 1.26 ± 0.09 | 1.26 ± 0.15 |
| Stride length UL (meter) | 1.27 ± 0.09 | 1.32 ± 0.19 | 1.28 ± 0.15 | 1.23 ± 0.12 | 1.27 ± 0.13 | 1.28 ± 0.17 |
| Double support TKA (% of total gait cycle) | 18.59 ± 5.04 | 21.13 ± 14.10 | 24.16 ± 13.16 | 18.89 ± 19.65 | 22.49 ± 11.67 | 20.13 ± 15.49 |
| Double support UL (% of total gait cycle) | 18.32 ± 7.06 | 22.02 ± 15.55 | 25.15 ± 15.12 | 18.67 ± 19.48 | 20.61 ± 15.75 | 20.90 ± 16.40 |
| Single limb support TKA (% of total gait cycle) | 41.50 ± 3.23 | 39.81 ± 3.24 | 39.28 ± 4.13 | 41.11 ± 6.69 | 39.82 ± 5.33 | 40.88 ± 4.36 |
| Single limb support UL (% of total gait cycle) | 41.72 ± 1.86 | 41.22 ± 2.11 | 42.21 ± 4.33 | 40.60 ± 5.63 | 41.50 ± 2.60 | 41.21 ± 3.89 |
| Stance TKA (% of total gait cycle) | 57.74 ± 2.13 | 58.49 ± 2.45 | 57.95 ± 5.52 | 60.89 ± 5.72 | 58.35 ± 3.66 | 58.68 ± 4.73 |
| Stance UL (% of total gait cycle) | 59.38 ± 2.64 | 60.18 ± 2.96 | 60.09 ± 3.51 | 58.74 ± 2.82 | 60.54 ± 4.96 | 58.99 ± 5.37 |
| Swing TKA (% of total gait cycle) | 42.26 ± 2.13 | 41.51 ± 2.45 | 42.05 ± 5.52 | 39.12 ± 5.72 | 40.83 ± 2.94 | 41.32 ± 4.73 |
| Swing UL (% of total gait cycle) | 40.63 ± 2.64 | 39.83 ± 2.96 | 39.91 ± 3.51 | 41.26 ± 2.82 | 39.46 ± 4.96 | 41.02 ± 5.37 |
| Elevation at midswing TKA (centimeter) | 1.72 ± 1.48 | 2.04 ± 2.31 | 2.66 ± 2.82 | 1.95 ± 1.80 | 1.77 ± 0.91 | 1.84 ± 1.59 |
| Elevation at midswing UL (centimeter) | 1.86 ± 1.47 | 2.41 ± 0.94 | 2.48 ± 1.02 | 2.22 ± 1.86 | 1.95 ± 1.28 | 2.06 ± 1.53 |
| Lateral step variability TKA (centimeter) | 3.61 ± 0.79 | 0.15 ± 1.29 | 3.29 ± 0.79 | 3.35 ± 1.13 | 3.47 ± 1.48 | 2.87 ± 0.90 |
| Lateral step variability UL (centimeter) | 4.03 ± 1.44 | 3.06 ± 1.14 | 3.35 ± 1.68 | 3.83 ± 0.85 | 3.86 ± 1.14 | 3.53 ± 1.85 |
| Circumduction TKA (centimeter) | 3.49 ± 1.41 | 3.62 ± 2.01 | 3.49 ± 1.88 | 3.20 ± 1.13 | 2.93 ± 2.15 | 3.17 ± 2.14 |
| Circumduction UL (centimeter) | 3.68 ± 1.59 | 3.37 ± 1.59 | 3.27 ± 1.16 | 3.39 ± 2.23 | 3.24 ± 1.59 | 3.27 ± 1.91 |
| Gait Speed TKA (meter/second) | 1.23 ± 0.10 | 1.30 ± 0.15 | 1.27 ± 0.17 | 1.28 ± 0.11 | 1.19 ± 0.14 | 1.18 ± 0.23 |
| Gait Speed UL (meter/second) | 1.23 ± 0.05 | 1.31 ± 0.18 | 1.21 ± 0.17 | 1.23 ± 0.16 | 1.23 ± 0.15 | 1.23 ± 0.23 |
| Stair climb test | ||||||
| Total time (seconds) | 6.20 ± 1.22 | 6.04 ± 1.87 | 6.40 ± 2.35 | 5.99 ± 1.91 | 6.01 ± 1.23 | 6.08 ± 1.81 |
| Arrival | Ski Tour 1 | Ski Tour 2 | Ski Tour 3 | Rest Day | Ski Tour 4 | Ski Tour 5 | Departure | |
|---|---|---|---|---|---|---|---|---|
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Day 8 | |
| VAS Well being | 1.50 ± 3.00 | 3.00 ± 0.00 | 2.50 ± 3.00 | 3.00 ± 4.00 | 1.00 ± 3.00 | 2.00 ± 4.00 | ||
| Feeling Scale | ||||||||
| pre exercise | 3.00 ± 1.00 | 3.00 ± 2.00 | 3.00 ± 2.00 | 2.00 ± 4.00 | 3.00 ± 3.00 | |||
| post exercise | 4.00 ± 2.00 | 4.00 ± 2.00 | 4.00 ± 4.00 | 5.00 ± 2.00 | 4.00 ± 1.00 | |||
| Felt Arousal Scale | ||||||||
| pre exercise | 3.00 ± 2.00 | 3.00 ± 1.00 | 3.00 ± 2.00 | 3.00 ± 1.00 | 3.00 ± 2.00 | |||
| post exercise | 3.00 ± 2.00 | 3.00 ± 1.00 | 3.00 ± 1.00 | 3.00 ± 1.00 | 3.00 ± 2.00 | |||
| Short Form 12 Health Survey | ||||||||
| Physical Subscale | 49.66 ± 7.99 | 49.63 ± 16.07 | ||||||
| Mental Subscale | 54.54 ± 8.98 | 58.46 ± 8.06 | ||||||
| RESTQ-Sport | ||||||||
| Scale 1 General stress | 0.00 ± 1.00 | 0.00 ± 0.50 | ||||||
| Scale 2 Emotional stress | 0.50 ± 1.00 | 0.50 ± 0.50 | ||||||
| Scale 3 Social Stress | 1.00 ± 0.50 | 0.50 ± 1.00 | ||||||
| Scale 4 Conflicts/pressure | 0.50 ± 1.00 | 1.00 ± 0.50 | ||||||
| Scale 5 Fatigue | 0.00 ± 1.00 | 0.00 ± 0.50 | ||||||
| Scale 6 Lack of energy | 1.00 ± 1.00 | 0.50 ± 0.50 | ||||||
| Scale 7 Physical complaints | 1.00 ± 1.00 | 1.50 ± 1.50 | ||||||
| Scale 8 Success | 3.00 ± 3.00 | 3.00 ± 4.00 | ||||||
| Scale 9 Social recovery | 3.50 ± 1.50 | 4.50 ± 3.00 | ||||||
| Scale 10 Physical recovery | 4.00 ± 1.00 | 4.50 ± 1.50 | ||||||
| Scale 11 General well being | 4.00 ± 1.00 | 5.00 ± 1.50 | ||||||
| Scale 12 Sleep Quality | 5.00 ± 2.50 | 5.00 ± 2.50 | ||||||
| Mood Scale | 6.50 ± 7.75 | 3.00 ± 11.00 |
References
- Ethgen, O.; Bruyere, O.; Richy, F.; D’ardennes, C.; Reginster, J. Health-Related Quality of Life in Total Hip and Total Knee Arthroplasty. J. Bone Jt. Surg. 2004, 86, 963–974. [Google Scholar] [CrossRef]
- Kösters, A.; Pötzelsberger, B.; Dela, F.; Dorn, U.; Hofstaedter, T.; Fink, C.; Müller, E. Alpine Skiing with total knee ArthroPlasty (ASWAP): Study design and intervention. Scand. J. Med. Sci. Sports 2015, 25, 3–9. [Google Scholar] [CrossRef]
- Jonsson, H.; Olafsdottir, S.; Sigurdardottir, S.; Aspelund, T.; Eiriksdottir, G.; Sigurdsson, S.; Harris, T.B.; Launer, L.; Gudnason, V. Incidence and prevalence of total joint replacements due to osteoarthritis in the elderly: Risk factors and factors associated with late life prevalence in the AGES-Reykjavik Study. BMC Musculoskelet. Disord. 2016, 17, 14. [Google Scholar] [CrossRef]
- OECD/EU. Health at a Glance: Europe 2016—State of Health in the EU Cycle; OECD Publishing: Paris, France, 2016. [Google Scholar]
- Amlani, N.M.; Munir, F. Does physical activity have an impact on sickness absence? A review. Sports Med. 2014, 44, 887–907. [Google Scholar] [CrossRef]
- Kuster, M.S. Exercise Recommendations After Total Joint Replacement. A review of the current literature and proposal of scientifically based guidelines. Sports Med. 2002, 32, 433–455. [Google Scholar] [CrossRef]
- Eigenschenk, B.; Thomann, A.; McClure, M.; Davies, L.; Gregory, M.; Dettweiler, U.; Ingles, E. Benefits of Outdoor Sports for Society. A Systematic Literature Review and Reflections on Evidence. Int. J. Environ. Res. Public Health 2019, 16, 937. [Google Scholar] [CrossRef]
- Dagneaux, L.; Bourlez, J.; Degeorge, B.; Canovas, F. Return to sport after total or unicompartmental knee arthroplasty: An informative guide for residents to patients. EFORT Open Rev. 2017, 2, 496–501. [Google Scholar] [CrossRef]
- Hepperger, C.; Gföller, P.; Abermann, E.; Hoser, C.; Ulmer, H.; Herbst, E.; Fink, C. Sports activity is maintained or increased following total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 26, 1515–1523. [Google Scholar] [CrossRef] [PubMed]
- Paillard, T. Effects of general and local fatigue on postural control: A review. Neurosci. Biobehav. Rev. 2012, 36, 162–176. [Google Scholar] [CrossRef] [PubMed]
- Koller, A.; Fuchs, B.; Leichtfried, V.; Schobersberger, W. Decrease in eccentric quadriceps and hamstring strength in recreational alpine skiers after prolonged skiing. BMJ Open Sport Exerc. Med. 2015, 1. [Google Scholar] [CrossRef]
- Wan, J.; Qin, Z.; Wang, P.; Sun, Y.; Liu, X. Muscle fatigue: General understanding and treatment. Exp. Mol. Med. 2017, 49, e384. [Google Scholar] [CrossRef]
- Pötzelsberger, B.; Stöggl, T.; Lindinger, S.J.; Dirnberger, J.; Stadlmann, M.; Buchecker, M.; Hofstaedter, T.; Gordon, K.; Müller, E. Alpine Skiing With total knee ArthroPlasty (ASWAP): Effects on strength and cardiorespiratory fitness. Scand. J. Med. Sci. Sports 2015, 25, 16–25. [Google Scholar] [CrossRef]
- Pötzelsberger, B.; Lindinger, S.J.; Stöggl, T.; Buchecker, M.; Müller, E. Alpine Skiing With total knee ArthroPlasty (ASWAP): Effects on gait asymmetries. Scand. J. Med. Sci. Sports 2015, 25, 49–59. [Google Scholar] [CrossRef]
- Skimo.at. Aktuelle Zahlen, Daten und Fakten des Tourenskisports. Der Aufwärtstrend auf Steigfellen—von der Niesche zum Wirtschaftsfaktor. Available online: http://www.skimo.at/skibergsteigen/185867/skimo-austria-pressekonferenz-aktuelle-zahlen-daten-und-fakten-im-skibergsteigen/ (accessed on 24 April 2019).
- Haslinger, S.; Blank, C.; Morawetz, D.; Koller, A.; Dünnwald, T.; Berger, S.; Schlickum, N.; Schobersberger, W. Effects of Recreational Ski Mountaineering on Cumulative Muscle Fatigue—A Longitudinal Trial. Front. Physiol. 2018, 9, 1687. [Google Scholar] [CrossRef]
- Scuderi, G.R.; Bourne, R.B.; Noble, P.C.; Benjamin, J.B.; Lonner, J.H.; Scott, W.N. The new Knee Society Knee Scoring System. Clin. Orthop. Relat. Res. 2012, 470, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Karvonen, M.; Kentala, K.; Mustala, O. The effects of training heart rate: A longitudinal study. Ann. Med. Exp. Biol. Fenn. 1957, 35, 307–315. [Google Scholar] [PubMed]
- Aquino, M.d.A.; Garces-Leme, L.E. Isokinetik Dynamometry in elderly woman undergoing total knee arthroplasty: A comparative study. Clinics 2006, 61, 215–222. [Google Scholar] [CrossRef]
- Godinho, C.; Domingos, J.; Cunha, G.; Santos, A.T.; Fernandes, R.M.; Abreu, D.; Goncalves, N.; Matthews, H.; Isaacs, T.; Duffen, J.; et al. A systematic review of the characteristics and validity of monitoring technologies to assess Parkinson’s disease. J. Neuroeng. Rehabil. 2016, 13, 24. [Google Scholar] [CrossRef] [PubMed]
- Mancini, M.; King, L.; Salarian, A.; Holmstrom, L.; McNames, J.; Horak, F.B. Mobility Lab to Assess Balance and Gait with Synchronized Body-worn Sensors. J. Bioeng. Biomed. Sci. 2011. [Google Scholar] [CrossRef]
- Raschner, C.; Lembert, S.; Platzer, H.P.; Patterson, C.; Hilden, T.; Lutz, M. S3-Check—Evaluation and generation of normal values of a test for balance ability and postural stability. Sportverletz. Sportschaden 2008, 22, 100–105. [Google Scholar] [CrossRef]
- Bennell, K.; Dobson, F.; Hinman, R. Measures of physical performance assessments: Self-Paced Walk Test (SPWT), Stair Climb Test (SCT), Six-Minute Walk Test (6MWT), Chair Stand Test (CST), Timed Up & Go (TUG), Sock Test, Lift and Carry Test (LCT), and Car Task. Arthritis Care Res. 2011, 63, S350–S370. [Google Scholar] [CrossRef] [Green Version]
- Almeida, G.J.; Schroeder, C.A.; Gil, A.B.; Fitzgerald, G.K.; Piva, S.R. Interrater reliability and validity of the stair ascend/descend test in subjects with total knee arthroplasty. Arch. Phys. Med. Rehabil. 2010, 91, 932–938. [Google Scholar] [CrossRef]
- Borg, G. Anstrengungsempfinden und körperliche Aktivität. Deutsches Ärzteblatt 2004, 101, 1016–1021. [Google Scholar]
- Hardy, C.J.; Rejeski, W.J. Not What, but How One Feels: The Measurement of Affect during Exercise. J. Sport Exerc. Psychol. 1989, 11, 304–317. [Google Scholar] [CrossRef]
- Svebak, S.; Murgatroyd, S. Metamotivational dominance: A multimethod validation of reversal theory constructs. J. Personal. Soc. Psychol. 1985, 48, 107–116. [Google Scholar] [CrossRef]
- Kallus, K.W. Erholungs-Belastungs-Fragebogen (EBF). Handanweisung; Pearson Assessment: Frankfurt am Main, Germany, 2011. [Google Scholar]
- Kellmann, M. Preventing overtraining in athletes in high-intensity sports and stress/recovery monitoring. Scand. J. Med. Sci. Sports 2010, 20, 95–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bullinger, M.; Kirchberger, I. SF-36 Fragegbogen zum Gesundheitszustand Handanweisung; Hogrefe Verlag für Psychologie: Göttingen, Germany, 1998; p. 155. [Google Scholar]
- Ware, J.; Kosinski, M.; Keller, S. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Abele-Brehm, A.; Brehm, W. Zur Konzeptionalisierung und Messung von Befindlichkeit. Die Entwicklung der “Befindlichkeitsskalen (BFS)”. Diagnostica 1986, 32, 209–228. [Google Scholar]
- Von Zerssen, D.; Petermann, F. Die Befindlichkeits-Skala, Revidierte Fassung, Manual; Hogrefe Verlag GmbH & Co.KG: Göttingen, Germany, 2011. [Google Scholar]
- Noguchi, K.; Gel, Y.R.; Brunner, E.; Konietschke, F. nparLD: An R Software Package for the Nonparametric Analysis of Longitudinal Data in Factorial Experiments. J. Stat. Softw. 2012, 50. [Google Scholar] [CrossRef]
- Brunner, E. Nichtparametrische Analyse Longitudinaler Daten; Walter de Gruyter GmbH & Co KG: München, Germany; Wien, Austria; Oldenburg, Germany, 2014; p. 256. [Google Scholar]
- Haber, P. Lungenfunktion und Spiroergometrie. Interpretaion und Befunderstellung, 2nd ed.; Springer: Wien, Austria, 2007; p. 141. [Google Scholar]
- Wonisch, M.; Berent, R.; Klicpera, M.; Laimer, H.; Marko, C.; Schwann, H.; Schmid, P. Praxisleitlinien Ergometrie. J. Kardiol. 2008, 15, 3–17. [Google Scholar] [CrossRef]
- Pretty, J.; Peacock, J.; Sellens, M.; Griffin, M. The mental and physical health outcomes of green exercise. Int. J. Environ. Health Res. 2005, 15, 319–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowler, D.E.; Buyung-Ali, L.M.; Knight, T.M.; Pullin, A.S. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health 2010, 10, 456. [Google Scholar] [CrossRef] [PubMed]
- Thompson Coon, J.; Boddy, K.; Stein, K.; Whear, R.; Barton, J.; Depledge, M.H. Does Participating in Physical Activity in Outdoor Natural Environments Have a Greater Effect on Physical and Mental Wellbeing than Physical Activity Indoors? A Systematic Review. Environ. Sci. Technol. 2011, 45, 1761–1772. [Google Scholar] [CrossRef] [PubMed]
- Akers, A.; Barton, J.; Cossey, R.; Gainsford, P.; Griffin, M.; Micklewright, D. Visual color perception in green exercise: Positive effects on mood and perceived exertion. Environ. Sci. Technol. 2012, 46, 8661–8666. [Google Scholar] [CrossRef] [PubMed]
- Wooller, J.-J.; Barton, J.; Gladwell, V.F.; Micklewright, D. Occlusion of sight, sound and smell during Green Exercise influences mood, perceived exertion and heart rate. Int. J. Environ. Health Res. 2015, 26, 267–280. [Google Scholar] [CrossRef]
- Rogerson, M.; Gladwell, V.F.; Gallagher, D.J.; Barton, J.L. Influences of Green Outdoors versus Indoors Environmental Settings on Psychological and Social Outcomes of Controlled Exercise. Int. J. Environ. Res. Public Health 2016, 13, 363. [Google Scholar] [CrossRef]
- Gladwell, V.; Kuoppa, P.; Tarvainen, M.; Rogerson, M. A Lunchtime Walk in Nature Enhances Restoration of Autonomic Control during Night-Time Sleep: Results from a Preliminary Study. Int. J. Environ. Res. Public Health 2016, 13, 280. [Google Scholar] [CrossRef]
- Röijezon, U.; Clark, N.C.; Treleaven, J. Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Manual Ther. 2015, 20, 368–377. [Google Scholar] [CrossRef]
- Hofstaedter, T.; Fink, C.; Dorn, U.; Pötzelsberger, B.; Hepperger, C.; Gordon, K.; Müller, E. Alpine Skiing With total knee ArthroPlasty (ASWAP): Clinical and radiographic outcomes. Scand. J. Med. Sci. Sports 2015, 25, 10–15. [Google Scholar] [CrossRef]
- Burtscher, M.; Gatterer, H.; Flatz, M.; Sommersacher, R.; Woldrich, T.; Ruedl, G.; Hotter, B.; Lee, A.; Nachbauer, W. Effects of Modern Ski Equipment on the Overall Injury Rate and the Pattern of Injury Location in Alpine Skiing. Clin. J. Sport Med. 2008, 18, 355–357. [Google Scholar] [CrossRef]
| Ski Tour 1 | Ski Tour 2 | Ski Tour 3 | Ski Tour 4 | Ski Tour 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| t1 | t2 | t3 | t5 | t6 | ||||||
| median | IQR | median | IQR | median | IQR | median | IQR | median | IQR | |
| HR (bpm) | 123.00 | 13.00 | 121.00 | 18.00 | 128.50 | 18.00 | 119.00 | 26.00 | 114.50 | 12.00 |
| Time (min) | 129.00 | 30.00 | 102.50 | 15.00 | 160.00 | 11.00 | 201.00 | 31.00 | 189.00 | 0.00 |
| Ascent (m) | 780.00 # | - | 715.00# | - | 953.00 | 200.00 | 1037.00 | 35.00 | 998.00 | 0.00 |
| Distance (m) | 4400.00 | 200.00 | 3600.00# | - | 4513.00 | 573.00 | 5380.00 | 373.00 | 5430.00 | 0.00 |
| Borg Scale score | 11.00 | 3.00 | 10.50 | 2.00 | 12.5 | 3.00 | 12.00 | 4.00 | 11.00 | 1.00 |
| Mobility LabGait Parameters | F1-LD-F1 | Relative Treatment Effects (RTEs) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| F | p | UL | TKA | UL | TKA | ||||
| Cadence | leg | 0.03(1,∞) | 0.87 | leg × t1 | 0.41 | 0.44 | leg × t4 | 0.52 | 0.41 |
| time | 1.53(2.34,∞) | 0.21 | leg × t2 | 0.58 | 0.6 | leg × t5 | 0.56 | 0.52 | |
| leg × time | 0.34(2.34,∞) | 0.75 | Leg × t3 | 0.49 | 0.45 | leg × t6 | 0.5 | 0.51 | |
| Stride length | leg | 0.02(1,∞) | 0.88 | leg × t1 | 0.5 | 0.54 | leg × t4 | 0.41 | 0.45 |
| time | 1.56(2.39,∞) | 0.21 | leg × t2 | 0.57 | 0.61 | leg × t5 | 0.49 | 0.45 | |
| leg × time | 0.21(2.39,∞) | 0.85 | leg × t3 | 0.47 | 0.54 | leg × t6 | 0.48 | 0.47 | |
| Double support time | leg | 0.02(1,∞) | 0.88 | leg × t1 | 0.39 | 0.39 | leg × t4 | 0.5 | 0.5 |
| time | 0.9(2.78,∞) | 0.44 | leg × t2 | 0.51 | 0.5 | leg × t5 | 0.53 | 0.5 | |
| leg × time | 0.01(2.78,∞) | 1 | leg × t3 | 0.58 | 0.56 | leg × t6 | 0.53 | 0.5 | |
| Single limb support time | leg | 1.12(1,∞) | 0.29 | leg × t1 | 0.64 | 0.59 | leg × t4 | 0.47 | 0.51 |
| time | 0.89(2.58,∞) | 0.43 | leg × t2 | 0.54 | 0.41 | leg × t5 | 0.6 | 0.4 | |
| leg × time | 0.68(2.58,∞) | 0.54 | leg × t3 | 0.57 | 0.35 | leg × t6 | 0.48 | 0.44 | |
| Stance | leg | 0.58(1,∞) | 0.44 | leg × t1 | 0.46 | 0.28 | leg × t4 | 0.45 | 0.63 |
| time | 1.57(2.56,∞) | 0.20 | leg × t2 | 0.56 | 0.46 | leg × t5 | 0.63 | 0.42 | |
| leg × time | 1.58(2.56,∞) | 0.20 | leg × t3 | 0.54 | 0.44 | leg × t6 | 0.59 | 0.52 | |
| Swing | leg | 0.32(1,∞) | 0.57 | leg × t1 | 0.56 | 0.73 | leg × t4 | 0.56 | 0.38 |
| time | 2.14(2.69,∞) | 0.1 | leg × t2 | 0.45 | 0.56 | leg × t5 | 0.37 | 0.45 | |
| leg × time | 1.27(2.69,∞) | 0.28 | leg × t3 | 0.47 | 0.57 | leg × t6 | 0.42 | 0.49 | |
| Elevation at midswing | leg | 0.32(1,∞) | 1 | leg × t1 | 0.43 | 0.41 | leg × t4 | 0.53 | 0.47 |
| time | 1.6(3.93,∞) | 0.17 | leg × t2 | 0.56 | 0.48 | leg × t5 | 0.54 | 0.44 | |
| leg × time | 0.1(3.93,∞) | 0.98 | leg × t3 | 0.66 | 0.57 | leg × t6 | 0.48 | 0.44 | |
| Lateral step variability | leg | 1.66(1,∞) | 0.20 | leg × t1 | 0.7 | 0.55 | leg × t4 | 0.58 | 0.39 |
| time | 1.64(3.57,∞) | 0.17 | leg × t2 | 0.38 | 0.55 | leg × t5 | 0.59 | 0.54 | |
| leg × time | 1.41(3.57,∞) | 0.23 | leg × t3 | 0.49 | 0.38 | leg × t6 | 0.56 | 0.28 | |
| Circumduction | leg | 0(1,∞) | 0.95 | leg × t1 | 0.46 | 0.54 | leg × t4 | 0.49 | 0.45 |
| time | 1.31(2.84,∞) | 0.27 | leg × t2 | 0.59 | 0.56 | leg × t5 | 0.5 | 0.42 | |
| leg × time | 0.53(2.84,∞) | 0.65 | leg × t3 | 0.51 | 0.51 | leg × t6 | 0.48 | 0.5 | |
| Gait speed | leg | 0.01(1,∞) | 0.92 | leg × t1 | 0.43 | 0.41 | leg × t4 | 0.48 | 0.56 |
| time | 2.01(2.12,∞) | 0.13 | leg × t2 | 0.66 | 0.66 | leg × t5 | 0.5 | 0.42 | |
| leg × time | 0.39(2.12,∞) | 0.69 | leg × t3 | 0.45 | 0.57 | Leg × t6 | 0.46 | 0.41 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haslinger, S.; Huber, D.; Morawetz, D.; Blank, C.; Prossegger, J.; Dünnwald, T.; Koller, A.; Fink, C.; Hartl, A.; Schobersberger, W. Feasibility of Ski Mountaineering for Patients Following a Total Knee Arthroplasty: A Descriptive Field Study. Int. J. Environ. Res. Public Health 2019, 16, 1582. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16091582
Haslinger S, Huber D, Morawetz D, Blank C, Prossegger J, Dünnwald T, Koller A, Fink C, Hartl A, Schobersberger W. Feasibility of Ski Mountaineering for Patients Following a Total Knee Arthroplasty: A Descriptive Field Study. International Journal of Environmental Research and Public Health. 2019; 16(9):1582. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16091582
Chicago/Turabian StyleHaslinger, Simon, Daniela Huber, David Morawetz, Cornelia Blank, Johanna Prossegger, Tobias Dünnwald, Arnold Koller, Christian Fink, Arnulf Hartl, and Wolfgang Schobersberger. 2019. "Feasibility of Ski Mountaineering for Patients Following a Total Knee Arthroplasty: A Descriptive Field Study" International Journal of Environmental Research and Public Health 16, no. 9: 1582. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16091582





