The Perceived Availability of Online Social Support: Exploring the Contributions of Illness and Rural Identities in Adults with Chronic Respiratory Illness
Abstract
:1. Introduction
1.1. Perceived Online Social Support
1.2. Social Identities: Illness and Geographic
2. Materials and Methods
2.1. Measures
2.2. Data Analysis
3. Results
3.1. Research Question 1
3.2. Hypotheses 1–2
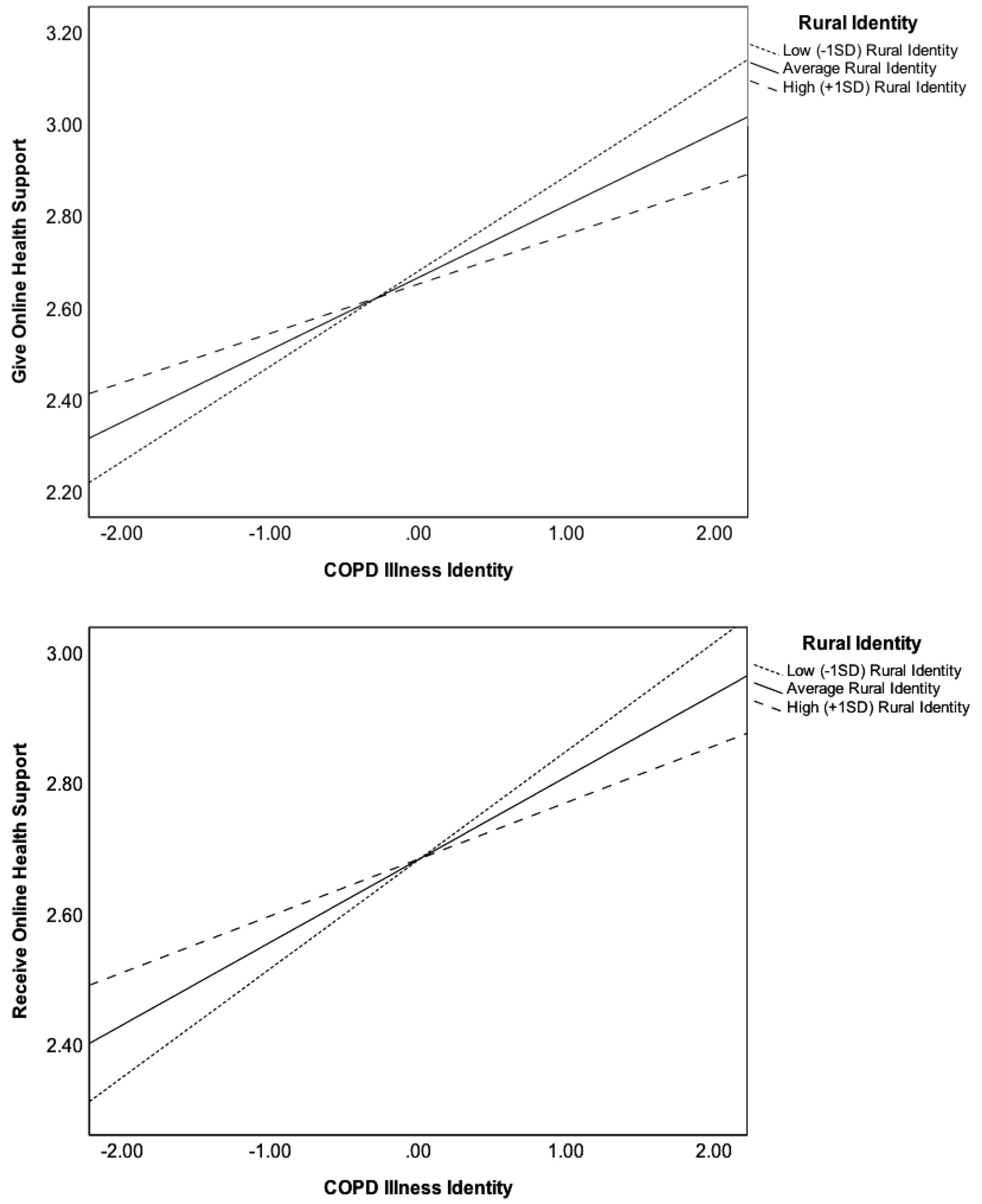
3.3. Research Question 2
4. Discussion
Principal Findings
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lyyra, T.M.; Heikkinen, R.L. Perceived Social Support and Mortality in Older People. J. Gerontol. B Psychol. Sci. Soc. Sci. 2006, 61, S147–S152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinfield, C.; Ellison, N.B.; Lampe, C. Social Capital, Self-Esteem, and Use of Online Social Network Sites: A Longitudinal Analysis. J. Appl. Dev. Psychol. 2008, 29, 434–445. [Google Scholar] [CrossRef]
- Wright, K.B. Communication in Health-Related Online Social Support Groups/Communities: A Review of Research and Predictors of Participation, Applications of Social Support Theory, and Health Outcomes. Rev. Commun. Res. 2016, 4, 65–87. [Google Scholar]
- Shakespeare-Finch, J.; Obst, P.L. The Development of the 2-Way Social Support Scale: A Measure of Giving and Receiving Emotional and Instrumental Support. J. Pers. Assess. 2011, 93, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, T.L.; Adelman, M.B. Communicating Social Support; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1987. [Google Scholar]
- Cutrona, C.E.; Suhr, J.A. Controllability of Stressful Events and Satisfaction with Spouse Support Behaviors. Commun. Res. 1992, 19, 154–174. [Google Scholar] [CrossRef]
- Uchino, B.N. Understanding the Links Between Social Support and Physical Health: A Life-Span Perspective with Emphasis on the Separability of Perceived and Received Support. Perspect. Psychol. Sci. J. Assoc. Psychol. Sci. 2009, 4, 236–255. [Google Scholar] [CrossRef] [Green Version]
- Rains, S.A.; Peterson, E.B.; Wright, K.B. Communicating Social Support in Computer-Mediated Contexts: A Meta-Analytic Review of Content Analyses Examining Support Messages Shared Online among Individuals Coping with Illness. Commun. Monogr. 2015, 82, 403–430. [Google Scholar] [CrossRef]
- Walther, J.B.; Loh, T.; Granka, L. Let Me Count the Ways: The Interchange of Verbal and Nonverbal Cues in Computer-Mediated and Face-to-Face Affinity. J. Lang. Soc. Psychol. 2005, 24, 36–65. [Google Scholar] [CrossRef]
- Patel, R.; Chang, T.; Greysen, S.R.; Chopra, V. Social Media Use in Chronic Disease: A Systematic Review and Novel Taxonomy. Am. J. Med. 2015, 128, 1335–1350. [Google Scholar] [CrossRef]
- Allen, C.; Vassilev, I.; Kennedy, A.; Rogers, A. Long-Term Condition Self-Management Support in Online Communities: A Meta-Synthesis of Qualitative Papers. J. Med. Internet Res. 2016, 18, 61. [Google Scholar] [CrossRef]
- Hogg, M.A. Social Identity. In Handbook of Self and Identity; The Guilford Press: New York, NY, USA, 2003; pp. 462–479. [Google Scholar]
- Hecht, M.L.; Lu, Y. Communication Theory of Identity. In Encyclopedia of Health Communication; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2014; pp. 226–227. [Google Scholar] [CrossRef]
- Jung, E.; Hecht, M.L. Elaborating the Communication Theory of Identity: Identity Gaps and Communication Outcomes. Commun. Q. 2004, 52, 265–283. [Google Scholar] [CrossRef]
- Centers for Disease Control & Prevention. CDC–COPD Home Page–Chronic Obstructive Pulmonary Disease (COPD). Available online: https://www.cdc.gov/copd/index.html (accessed on 14 November 2017).
- Han, M.L.K.; Martinez, C.H.; Au, D.H.; Bourbeau, J.; Boyd, C.M.; Branson, R.; Criner, G.J.; Kalhan, R.; Kallstrom, T.J.; King, A.; et al. Meeting the Challenge of COPD Care Delivery in the USA: A Multiprovider Perspective. Lancet Respir. Med. 2016, 4, 473–526. [Google Scholar] [CrossRef]
- Pleasants, R.A.; Riley, I.L.; Mannino, D.M. Defining and Targeting Health Disparities in Chronic Obstructive Pulmonary Disease. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 2475–2496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gardener, A.C.; Ewing, G.; Kuhn, I.; Farquhar, M. Support Needs of Patients with COPD: A Systematic Literature Search and Narrative Review. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 1021–1035. [Google Scholar] [CrossRef] [Green Version]
- Kiley, J.P.; Gibbons, G.H. COPD National Action Plan: Addressing a Public Health Need Together. Chest 2017, 152, 698–699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paige, S.R.; Stellefson, M.; Krieger, J.L.; Alber, J.M. Computer-Mediated Experiences of Patients with Chronic Obstructive Pulmonary Disease. Am. J. Health Educ. 2019, 50, 127–134. [Google Scholar] [CrossRef]
- Barton, C.; Effing, T.W.; Cafarella, P. Social Support and Social Networks in COPD: A Scoping Review. J. Chronic Obstr. Pulm. Dis. 2015, 12, 690–702. [Google Scholar] [CrossRef]
- Reblin, M.; Uchino, B.N. Social and Emotional Support and Its Implication for Health. Curr. Opin. Psychiatry 2008, 21, 201–205. [Google Scholar] [CrossRef] [Green Version]
- Göz, F.; Karaoz, S.; Goz, M.; Ekiz, S.; Cetin, I. Effects of the Diabetic Patients’ Perceived Social Support on Their Quality-of-Life. J. Clin. Nurs. 2007, 16, 1353–1360. [Google Scholar] [CrossRef]
- Prati, G.; Pietrantoni, L. Optimism, Social Support, and Coping Strategies As Factors Contributing to Posttraumatic Growth: A Meta-Analysis. J. Loss Trauma 2009, 14, 364–388. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Fan, V.S.; Belza, B.; Pike, K.; Nguyen, H.Q. Association between Social Support and Self-Care Behaviors in Adults with Chronic Obstructive Pulmonary Disease. Ann. Am. Thorac. Soc. 2017, 14, 1419–1427. [Google Scholar] [CrossRef] [PubMed]
- Lenferink, A.; van der Palen, J.; Effing, T. The Role of Social Support in Improving Chronic Obstructive Pulmonary Disease Self-Management. Expert Rev. Respir. Med. 2018, 12, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Stellefson, M.L.; Shuster, J.J.; Chaney, B.H.; Paige, S.R.; Alber, J.M.; Chaney, J.D.; Sriram, P.S. Web-Based Health Information Seeking and EHealth Literacy among Patients Living with Chronic Obstructive Pulmonary Disease (COPD). Health Commun. 2018, 33, 1410–1424. [Google Scholar] [CrossRef]
- Fox, S. The Social Life of Health Information; Pew Res. Center: Washington, DC, USA, 2014; Available online: https://www.pewresearch.org/fact-tank/2014/01/15/the-social-life-of-health-information/ (accessed on 28 December 2019).
- Paige, S.R.; Stellefson, M.; Chaney, B.H.; Alber, J.M. Pinterest as a Resource for Health Information on Chronic Obstructive Pulmonary Disease (COPD): A Social Media Content Analysis. Am. J. Health Educ. 2015, 46, 241–251. [Google Scholar] [CrossRef]
- Stellefson, M.; Chaney, B.; Ochipa, K.; Chaney, D.; Haider, Z.; Hanik, B.; Chavarria, E.; Bernhardt, J.M. YouTube as a Source of COPD Patient Education: A Social Media Content Analysis. Chron. Respir. Dis. 2014, 11, 61–71. [Google Scholar] [CrossRef] [Green Version]
- Cook, N.S.; Kostikas, K.; Gruenberger, J.B.; Shah, B.; Pathak, P.; Kaur, V.P.; Mudumby, A.; Sharma, R.; Gutzwiller, F.S. Patients’ Perspectives on COPD: Findings from a Social Media Listening Study. ERJ Open Res. 2019, 5, 00128–02018. [Google Scholar] [CrossRef]
- Martinez, C.H.; St. Jean, B.L.; Plauschinat, C.A.; Rogers, B.; Beresford, J.; Martinez, F.J.; Richardson, C.; Han, M.K. Internet Access and Use by COPD Patients in the National Emphysema/COPD Association Survey. BMC Pulm. Med. 2014, 14, 66. [Google Scholar] [CrossRef] [Green Version]
- Preece, J. Sociability and Usability in Online Communities: Determining and Measuring Success. Behav. Inf. Technol. 2001, 20, 347–356. [Google Scholar] [CrossRef]
- Charmaz, K. Stories of Suffering: Subjective Tales and Research Narratives. Qual. Health Res. 1999, 9, 362–382. [Google Scholar] [CrossRef]
- Yanos, P.T.; Roe, D.; Lysaker, P.H. The Impact of Illness Identity on Recovery from Severe Mental Illness. Am. J. Psychiatr. Rehabil. 2010, 13, 73–93. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. Tips From Former Smokers® Campaign. Available online: https://www.cdc.gov/tobacco/campaign/tips/index.html (accessed on 6 April 2019).
- Pederson, A.P.; Hoyak, K.A.K.; Mills, S.; Camp, P.G. Reflecting the Changing Face of Chronic Obstructive Pulmonary Disease: Sex and Gender in Public Education Materials on COPD. Proc. Am. Thorac. Soc. 2007, 4, 683–685. [Google Scholar] [CrossRef] [PubMed]
- Stellefson, M.; Paige, S.R.; Alber, J.M.; Stewart, M. COPD360social Online Community: A Social Media Review. Health Promot. Pract. 2018, 19, 489–491. [Google Scholar] [CrossRef] [PubMed]
- Apperson, A.; Stellefson, M.; Paige, S.R.; Chaney, B.H.; Chaney, J.D.; Wang, M.Q.; Mohan, A. Facebook Groups on Chronic Obstructive Pulmonary Disease: Social Media Content Analysis. Int. J. Environ. Res. Public Health 2019, 16, 3789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Proshansky, H.M.; Fabian, A.K.; Kaminoff, R. Place-Identity: Physical World Socialization of the Self. J. Environ. Psychol. 1983, 3, 57–83. [Google Scholar] [CrossRef]
- Rakauskas, M.E.; Ward, N.J.; Gerberich, S.G. Identification of Differences between Rural and Urban Safety Cultures. Accid. Anal. Prev. 2009, 41, 931–937. [Google Scholar] [CrossRef]
- Slama, K. Rural Culture Is a Diversity Issue. Minn. Psychol. 2004, 53, 9–12. [Google Scholar]
- Parker, K.; Horowitz, J.M.; Brown, A.; Fry, R.; Cohn, D.; Igielnik, R. Similarities and Differences between Urban, Suburban and Rural Communities in America; Pew Research Center: Washington, DC, USA, 2018; Available online: https://www.pewsocialtrends.org/2018/05/22/what-unites-and-divides-urban-suburban-and-rural-communities/ (accessed on 28 December 2019).
- Raju, S.; Keet, C.A.; Matsui, E.C.; Drummond, M.B.; Hansel, N.N.; Wise, R.A.; Peng, R.D.; McCormack, M.C. The Impact of Poverty and Rural Residence on Chronic Obstructive Pulmonary Disease (COPD) Prevalence: A Nationwide Analysis. In C15. Novel Epidemiology of Asthma and Copd (American Thoracic Society International Conference Abstracts); American Thoracic Society: Denver, CO, USA, 2015; p. A3904. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. BRFSS Survey Data and Documentation. Available online: https://www.cdc.gov/brfss/annual_data/annual_2017.html (accessed on 11 March 2019).
- Oris, L.; Luyckx, K.; Rassart, J.; Goubert, L.; Goossens, E.; Apers, S.; Arat, S.; Vandenberghe, J.; Westhovens, R.; Moons, P. Illness Identity in Adults with a Chronic Illness. J. Clin. Psychol. Med. Settings 2018, 25, 429–440. [Google Scholar] [CrossRef] [Green Version]
- Maples, P.; Franks, A.; Ray, S.; Stevens, A.B.; Wallace, L.S. Development and Validation of a Low-Literacy Chronic Obstructive Pulmonary Disease Knowledge Questionnaire (COPD-Q). Patient Educ. Couns. 2010, 81, 19–22. [Google Scholar] [CrossRef]
- The Benefits of Quitting Smoking Over Time; American Cancer Society: New York, NY, USA, 2018; Available online: https://www.cancer.org/healthy/stay-away-from-tobacco/benefits-of-quitting-smoking-over-time.html (accessed on 22 December 2019).
- Final Recommendation Statement: Lung Cancer Screening; US Preventive Services Task Force: Rockville, MD, USA, 2013; Available online: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/lung-cancer-screening (accessed on 22 December 2019).
- Cohen, J.; Cohen, P.; West, S.; Aiken, L. Applied Multiple Regression/Correlation Analysis for Behavioral Sciences, 3rd ed.; Routledge; Taylor & Francis Group: New York, NY, USA, 2003. [Google Scholar]
- Sinclair, C. Effectiveness and User Acceptance of Online Chronic Disease Management Interventions in Rural and Remote Settings: Systematic Review and Narrative Synthesis. Clin. Med. Insights Ther. 2015, 7. [Google Scholar] [CrossRef]

| Predictor | Descriptive Statistics |
|---|---|
| Socio-Demographics | |
| Age, M (SD) | 55.14 (12.62) |
| Gender, n (%) | |
| Female | 256 (44.50) |
| Male | 298 (51.80) |
| Missing | 21 (3.70) |
| Race, n (%) | |
| White | 474 (82.4) |
| Black/African American | 54 (9.4) |
| Asian American | 12 (2.1) |
| Native American | 13 (2.3) |
| Other/Multi-Racial | 19 (3.3) |
| Missing | 1 (0.7) |
| Ethnicity, n (%) | |
| Hispanic | 108 (18.8) |
| Non-Hispanic | 433 (75.3) |
| Missing | 34 (5.9) |
| Income, n (%) | |
| $24,999 or less | 70 (12.2) |
| $25K–$34,999 | 60 (10.4) |
| $35K–$49,999 | 124 (21.6) |
| $50K–$74,999 | 147 (25.6) |
| $75K or more | 156 (27.1) |
| Missing | 18 (3.1) |
| Education, n (%) | |
| Less than High School | 37 (12.7) |
| High School or Equivalent | 66 (11.5) |
| College 1–3 Years | 180 (31.3) |
| College 4 or More Years | 288 (50.1) |
| Missing | 4 (0.7) |
| Chronic Obstructive Pulmonary Disease (COPD)-Specific Factors | |
| COPD Illness Identity, M (SD) | 3.16 (1.77) |
| Respiratory Symptom Severity, M (SD) | 2.81 (0.96) |
| Disease Knowledge, M (SD) | 6.45 (2.74) |
| Smoker (Current, Quit within 15 years), n (%) | 242 (42.2) |
| Reported COPD Diagnosis, n (%) | 407 (70.8) |
| Rural-Specific Factors | |
| Rural Identity, M (SD) | 3.01 (1.22) |
| Perceived Rural Residence, M (SD) | 2.98 (1.29) |
| Online Activity and Support Behaviors | |
| Give Online Health Support, M (SD) | 2.57 (1.15) |
| Receive Online Health Support, M (SD) | 2.58 (1.16) |
| Weekly Social Media Use, n (%) | |
| 0–1 h | 119 (20.7) |
| 2–4 h | 99 (17.2) |
| 5–9 h | 63 (11) |
| 10+ h | 289 (50.3) |
| Missing | 5 (0.9) |
| 95% CI | |||||
|---|---|---|---|---|---|
| Regression Steps | R2 Change | b | SE b | Lower Bound | Upper Bound |
| Step 1: Socio-Demographics | 0.05 ** | ||||
| Age | −0.01 | 0.01 | −0.02 | 0.01 | |
| Gender a | −0.25 | 0.15 | −0.56 | 0.05 | |
| Race b | 0.31 | 0.23 | −0.15 | 0.77 | |
| Ethnicity c | 0.37 | 0.22 | −0.05 | 0.79 | |
| Income d | −0.60 ** | 0.16 | −0.91 | −0.29 | |
| Education e | 0.57 * | 0.23 | 0.12 | 1.03 | |
| Rural Identity | 0.06 | 0.10 | −0.13 | 0.25 | |
| Perceived Rural Residence | −0.02 | 0.10 | −0.21 | 0.16 | |
| Step 2: COPD Experiences | 0.22 ** | ||||
| COPD Diagnosis | 0.79 ** | 0.19 | 0.42 | 1.15 | |
| Respiratory Symptoms | 0.54 ** | 0.09 | 0.37 | 0.71 | |
| Smoker f | 0.32 * | 0.15 | 0.01 | 0.62 | |
| Step 3: COPD Awareness | 0.28 ** | ||||
| COPD Knowledge | 0.18 ** | 0.03 | 0.12 | 0.23 | |
| Regression Models, b (SE) [95% CI] | ||
|---|---|---|
| Regression Steps | Outcome 1: Perceived Availability to Give Online Support | Outcome 2: Perceived Availability to Receive Online Support |
| Step 1: COPD Illness Identity | ||
| n(df) | 501(8) | 504(8) |
| F Statistic | 20.15 *** | 21.05 *** |
| R2 Value | 0.24 | 0.25 |
| COPD Status | 0.61 (0.17) [0.28, 0.95] *** | 0.62 (0.17) [0.29, 0.96] *** |
| Symptom Severity | 0.55 (0.08) [0.39, 0.71] *** | 0.54 (0.08) [0.38, 0.69] *** |
| COPD Knowledge | 0.17 (0.03) [0.11, 0.22] *** | 0.17 (0.03) [0.12, 0.22] *** |
| Smoker | 0.12 (0.15) [−0.16, 0.41] | 0.11 (0.15) [−0.18, 0.40] |
| Perceived Rural Residence | −0.05 (0.06) [−0.02, 0.01] | −0.05 (0.05) [−0.15, 0.06] |
| Age | −0.01 (0.01) [−0.02, 0.01] | −0.01 (0.01) [−0.02, 0.01] |
| Income | −0.24 (0.14) [−0.52, 0.03] | −0.24 (0.14) [−0.51, 0.03] |
| Education | 0.40 (0.19) [0.04, 0.77] * | 0.35 (0.19) [−0.02, 0.71] |
| Step 2: Online Support Outcome | ||
| n(df) | 497(12) | 500(12) |
| F Statistic | 39.57 *** | 37.50 *** |
| R2 Value | 0.49 | 0.47 |
| COPD Status | 0.76 (0.09) [0.57, 0.94] *** | 0.72 (0.10) [0.52, 0.91] *** |
| COPD Illness Identity | 0.16 (0.02) [0.11, 0.21] *** | 0.13 (0.02) [0.08, 0.18] *** |
| Rural Identity | −0.01 (0.04) [−0.10, 0.07] | 0.01 (0.05) [−0.09, 0.09] |
| COPD Status * Rural Identity | −0.03 (0.07) [−0.16, 0.11] | −0.01 (0.07) [−0.15, 0.12] |
| COPD Identity * Rural Identity | −0.04 (0.02) [−0.07, −0.01] * | −0.03 (0.02) [−0.07, 0.00] * |
| Symptom Severity | −0.05 (0.04) [−0.14, 0.04] | −0.03 (0.04) [−0.12, 0.06] |
| COPD Knowledge | −0.04 (0.02) [−0.07, −0.01] ** | −0.06 (0.02) [−0.09, −0.03] *** |
| Smoker a | 0.07 (0.08) [−0.08, 0.23] | 0.04 (0.08) [−0.12, 0.20] |
| Perceived Rural Residence | −0.22 (0.04) [−0.30, −0.13] *** | −0.19 (0.04) [−0.27, −0.10] *** |
| Age | −0.03 (0.01) [−0.04, −0.03] *** | −0.04 (0.01) [−0.04, −0.03] *** |
| Income | −0.07 (0.08) [−0.21, 0.08] | −0.14 (0.07) [−0.29, 0.01] |
| Education | 0.16 (0.10) [−0.04, 0.37] | 0.19 (0.10) [−0.01, 0.40] |
| 95% Confidence Interval | |||
|---|---|---|---|
| Direct/Indirect Pathway | Effect (Std. Error) | Lower Level | Upper Level |
| Direct Effect COPD Diagnosis -> Give Online Support | |||
| Low Rural Identity | 0.79 (0.13) | 0.54 | 1.05 |
| Average Rural Identity | 0.76 (0.09) | 0.57 | 0.94 |
| High Rural Identity | 0.72 (0.12) | 0.49 | 0.96 |
| COPD Diagnosis -> Receive Online Support | |||
| Low Rural Identity | 0.74 (0.13) | 0.48 | 1.00 |
| Average Rural Identity | 0.72 (0.10) | 0.53 | 0.91 |
| High Rural Identity | 0.71 (0.12) | 0.47 | 0.94 |
| Indirect Effect COPD Diagnosis -> COPD Illness Identity -> Give Online Support | |||
| Low Rural Identity | 0.13 (0.05) | 0.04 | 0.24 |
| Average Rural Identity | 0.10 (0.04) | 0.03 | 0.18 |
| High Rural Identity | 0.07 (0.03) | 0.02 | 0.13 |
| COPD Diagnosis –> COPD Illness Identity -> Receive Online Support | |||
| Low Rural Identity | 0.10 (0.04) | 0.03 | 0.20 |
| Average Rural Identity | 0.08 (0.03) | 0.02 | 0.15 |
| High Rural Identity | 0.05 (0.03) | 0.01 | 0.12 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paige, S.R.; Damiani, R.E.; Flood-Grady, E.; Krieger, J.L.; Stellefson, M. The Perceived Availability of Online Social Support: Exploring the Contributions of Illness and Rural Identities in Adults with Chronic Respiratory Illness. Int. J. Environ. Res. Public Health 2020, 17, 242. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17010242
Paige SR, Damiani RE, Flood-Grady E, Krieger JL, Stellefson M. The Perceived Availability of Online Social Support: Exploring the Contributions of Illness and Rural Identities in Adults with Chronic Respiratory Illness. International Journal of Environmental Research and Public Health. 2020; 17(1):242. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17010242
Chicago/Turabian StylePaige, Samantha R., Rachel E. Damiani, Elizabeth Flood-Grady, Janice L. Krieger, and Michael Stellefson. 2020. "The Perceived Availability of Online Social Support: Exploring the Contributions of Illness and Rural Identities in Adults with Chronic Respiratory Illness" International Journal of Environmental Research and Public Health 17, no. 1: 242. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17010242





