No Benefit of a Pediatric Screening in Discovering Reduced Visual Acuity in Children: Experiences from a Cross-Sectional Study in Germany
Abstract
:1. Introduction
2. Methods
Setting, Participants, and Study Design
2.1.1. Contents of the PHE
2.1.2. Contents of U7a
2.1.3. Statistical Analyses
3. Results
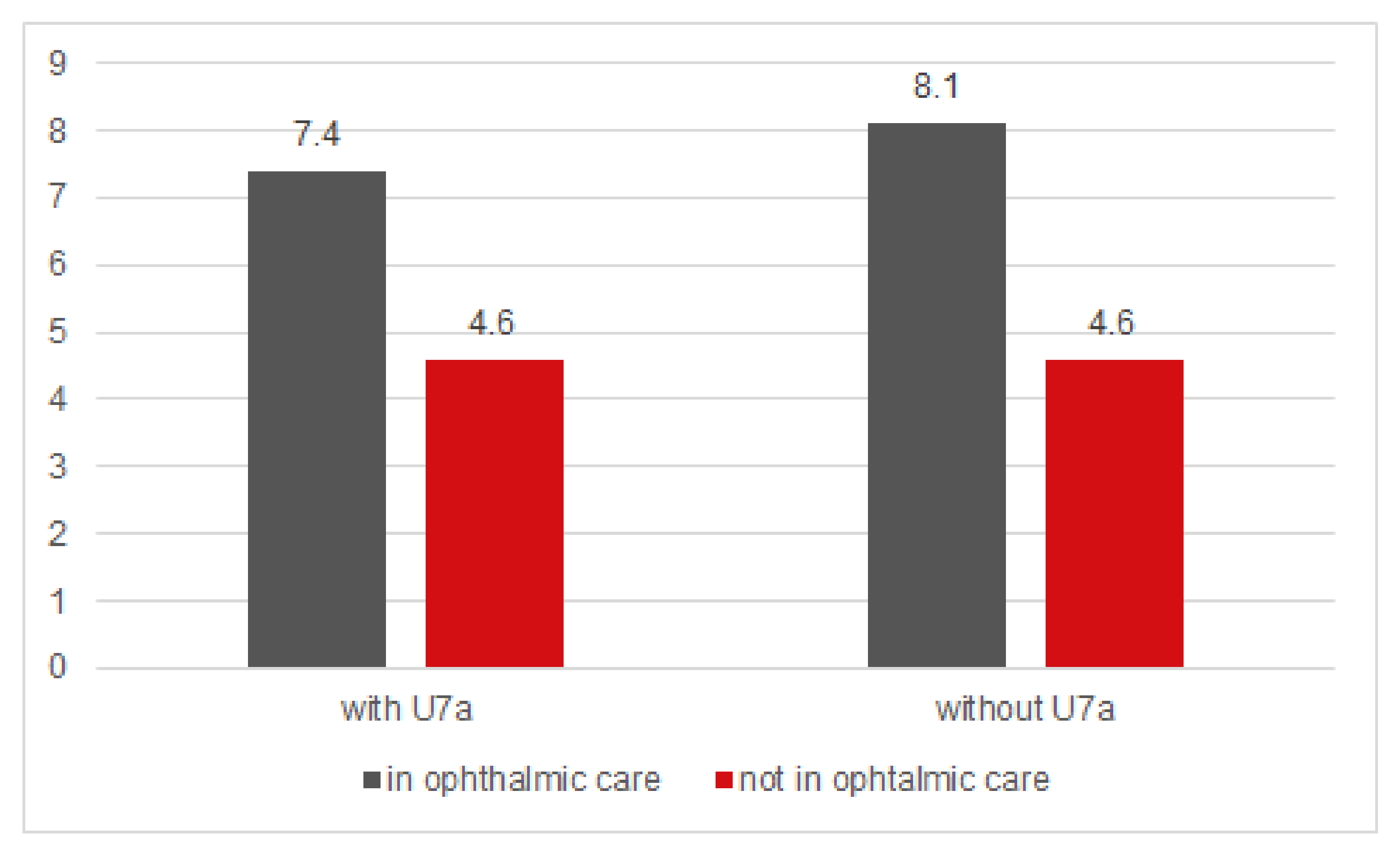
3.1. Unilateral Low Visual Acuity
3.2. Low Visual Acuity in Both Eyes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| VA | visual acuity |
| PHE | preschool health examination |
| U7a | preventive health examination at the end of the third year of life |
| U8 | preventive health examination at the end of the fourth year of life |
| U9 | preventive health examination at the beginning of the sixth year of life |
| IQWIG | German Institute for Quality and Efficiency in Health Care (“Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen”) |
| CI | confidence intervals |
References
- Williams, C.; Northstone, K.; Howard, M.; Harvey, I.; Harrad, R.A.; Sparrow, J.M. Prevalence and risk factors for common vision problems in children: Data from the ALSPAC study. Br. J. Ophthalmol. 2008, 92, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Robaei, D.; Rose, K.; Ojaimi, E.; Kifley, A.; Huynh, S.; Mitchell, P. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology 2005, 112, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Levi, D.M.; Knill, D.C.; Bavelier, D. Stereopsis and amblyopia: A mini-review. Vis. Res. 2015, 114, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Levi, D.M. Visual processing in amblyopia: Human studies. Strabismus 2006, 14, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Elflein, H.M.; Fresenius, S.; Lamparter, J.; Pitz, S.; Pfeiffer, N.; Binder, H.; Wild, P.; Mirshahi, A. The prevalence of amblyopia in Germany: Data from the prospective, population-based Gutenberg Health Study. Deutsch. Arztebl. Int. 2015, 112, 338–344. [Google Scholar]
- Ohlsson, J.; Villarreal, G.; Sjostrom, A.; Abrahamsson, M.; Sjostrand, J. Visual acuity, residual amblyopia and ocular pathology in a screened population of 12-13-year-old children in Sweden. Acta Ophthalmol. Scand. 2001, 79, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Hoeg, T.B.; Moldow, B.; Ellervik, C.; Klemp, K.; Erngaard, D.; la Cour, M.; Buch, H. Danish Rural Eye Study: The association of preschool vision screening with the prevalence of amblyopia. Acta Ophthalmol. 2015, 93, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Long, E.; Lin, H.; Liu, Y. Prevalence and epidemiological characteristics of congenital cataract: A systematic review and meta-analysis. Sci. Rep. 2016, 6, 28564. [Google Scholar] [CrossRef] [PubMed]
- Meyer, G.; Schwenn, O.; Pfeiffer, N.; Grehn, F. Trabeculotomy in congenital glaucoma. Graefes Arch. Clin. Exp. Ophthalmol. 2000, 238, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Lambert, S.R. The timing of surgery for congenital cataracts: Minimizing the risk of glaucoma following cataract surgery while optimizing the visual outcome. J. AAPOS 2016, 20, 191–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. Früherkennungsuntersuchung von Sehstörungen bei Kindern bis zur Vollendung des 6. Lebensjahres, Abschlussbericht S05-02, Version 1.0; IQWIG: Köln, Germany, 2008. [Google Scholar]
- Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. Früherkennung von Seh-störungen bei Kindern bis zur Vollendung des 6, Lebensjahres (Folgeauftrag zu Auftrag S05-02), Rapid Report S14-01; IQWIG: Köln, Germany, 2015. [Google Scholar]
- Jonas, D.E.; Amick, H.R.; Wallace, I.F.; Feltner, C.; Vander Schaaf, E.B.; Brown, C.L.; Baker, C. Vision Screening in Children Aged 6 Months to 5 Years: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2017, 318, 845–858. [Google Scholar] [CrossRef] [PubMed]
- Kasmann-Kellner, B.; Heine, M.; Pfau, B.; Singer, A.; Ruprecht, K.W. Screening for amblyopia, strabismus and refractive abnormalities in 1,030 kindergarten children. Klin. Monbl. Augenheilkd. 1998, 213, 166–173. [Google Scholar] [PubMed]
- Friedman, D.S.; Repka, M.X.; Katz, J.; Giordano, L.; Ibironke, J.; Hawes, P.; Burkom, D.; Tielsch, J.M. Prevalence of decreased visual acuity among preschool-aged children in an American urban population: The Baltimore Pediatric Eye Disease Study, methods, and results. Ophthalmology 2008, 115, 1786–1795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cotter, S.A.; Tarczy-Hornoch, K.; Wang, Y.; Azen, S.P.; Dilauro, A.; Borchert, M.; Varma, R.; Multi-Ethnic Pediatric Eye Disease Study Group. Visual acuity testability in African-American and Hispanic children: The multi-ethnic pediatric eye disease study. Am. J. Ophthalmol. 2007, 144, 663–667. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, C.; Northstone, K.; Harrad, R.A.; Sparrow, J.M.; Harvey, I.; Team, A.S. Amblyopia treatment outcomes after preschool screening v school entry screening: Observational data from a prospective cohort study. Br. J. Ophthalmol. 2003, 87, 988–993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Donoghue, L.; McClelland, J.F.; Logan, N.S.; Rudnicka, A.R.; Owen, C.G.; Saunders, K.J. Refractive error and visual impairment in school children in Northern Ireland. Br. J. Ophthalmol. 2010, 94, 1155–1159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandfeld, L.; Weihrauch, H.; Tubaek, G.; Mortzos, P. Ophthalmological data on 4.5- to 7-year-old Danish children. Acta Ophthalmol. 2018, 96, 379–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gronlund, M.A.; Andersson, S.; Aring, E.; Hard, A.L.; Hellstrom, A. Ophthalmological findings in a sample of Swedish children aged 4-15 years. Acta Ophthalmol. Scand. 2006, 84, 169–176. [Google Scholar] [CrossRef] [PubMed]

| Year | 2009/2010 | 2010/2011 | 2011/2012 | 2012/2013 | 2013/2014 | 2014/2015 | Total |
|---|---|---|---|---|---|---|---|
| N | 28,454 | 27,687 | 22,403 | 26,955 | 27,587 | 27,036 | 160,122 |
| Female (%) | 13,584 (47.8) | 13,165 (47.5) | 10,859 (48.5) | 12,855 (47.7) | 13,256 (48.1) | 13,002 (48.1) | 76,721 (47.9) |
| Average age (years) at PHE | 5.8 ± 0.4 | 5.8 ± 0.4 | 5.8 ± 0.3 | 5.8 ± 0.4 | 5.8 ± 0.4 | 5.8 ± 0.4 | 5.8 ± 0.4 |
| Proportion (%) PHE VA <0, 7 (monocular) | 679 (2.39) | 653 (2.35) | 511 (2.28) | 602 (2.23) | 708 (2.56) | 796 (2.94) | 3949 (2.46) |
| Proportion (%) PHE VA <0, 7 (binocular) | 794 (2.79) | 713 (2.57) | 507 (2.26) | 634 (2.35) | 778 (2.82) | 810 (2.99) | 4236 (2.65) |
| U7a participation rate (%) | - | - | 38.46 | 75.97 | 89.18 | 91.69 | 49.02 |
| Proportion (%) of children participating in all screening examinations (U1–U9 without U7a) | 74.04 | 77.98 | 82.59 | 85.56 | 87.41 | 89.72 | 82.8 |
| Total Number of Participants (N) | 160,122 |
|---|---|
| Number of participants with U7a (N) | 78,491 |
| proportion (%) of children with PHE VA <0.7 (mon- or binocular) | 5.02 |
| proportion (%) of children with PHE VA <0.7 (monocular) | 2.48 |
| proportion (%) of children with PHE VA <0.7 (binocular) | 2.54 |
| Number of Participants without U7a (N) | 81,631 |
| proportion (%) of children with PHE VA <0.7 (mon- or binocular) | 5.20 |
| proportion (%) of children with PHE VA <0.7 (monocular) | 2.46 |
| proportion (%) of children with PHE VA <0.7 (binocular) | 2.74 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elflein, H.M.; Pokora, R.; Müller, D.F.; Jahn, K.; Ponto, K.A.; Pitz, S.; Pfeiffer, N.; Schuster, A.K.; Urschitz, M.S. No Benefit of a Pediatric Screening in Discovering Reduced Visual Acuity in Children: Experiences from a Cross-Sectional Study in Germany. Int. J. Environ. Res. Public Health 2020, 17, 3419. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103419
Elflein HM, Pokora R, Müller DF, Jahn K, Ponto KA, Pitz S, Pfeiffer N, Schuster AK, Urschitz MS. No Benefit of a Pediatric Screening in Discovering Reduced Visual Acuity in Children: Experiences from a Cross-Sectional Study in Germany. International Journal of Environmental Research and Public Health. 2020; 17(10):3419. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103419
Chicago/Turabian StyleElflein, Heike M., Roman Pokora, Denis F. Müller, Klaus Jahn, Katharina A. Ponto, Susanne Pitz, Norbert Pfeiffer, Alexander K. Schuster, and Michael S. Urschitz. 2020. "No Benefit of a Pediatric Screening in Discovering Reduced Visual Acuity in Children: Experiences from a Cross-Sectional Study in Germany" International Journal of Environmental Research and Public Health 17, no. 10: 3419. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103419





