School-Based Tobacco Control and Smoking in Adolescents: Evidence from Multilevel Analyses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Measures
2.2.1. Smoking
2.2.2. Individual-Level Variables
2.2.3. School-Level Variables
2.3. Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- USDHHS. Preventing Tobacco Use among Youth and Young Adults: A Report of the Surgeon General; US Department of Health and Human Services, Centers for Disease: Atlanta, GA, USA, 2012.
- Bates, C.; Rowell, A. Tobacco Explained… The Truth about the Tobacco Industry… in Its Own Words; UC San Francisco, Center for Tobacco Control Research and Education: San Francisco, CA, USA, 2004. [Google Scholar]
- Thomas, R.E.; McLellan, J.; Perera, R. Effectiveness of school-based smoking prevention curricula: Systematic review and meta-analysis. BMJ Open 2015, 5, e006976. [Google Scholar] [CrossRef]
- Henderson, M.; Ecob, R.; Wight, D.; Abraham, C. What explains between-school differences in rates of smoking? BMC Public Health 2008, 8, 218. [Google Scholar] [CrossRef] [Green Version]
- Mrug, S.; Gaines, J.; Su, W.; Windle, M. School-level substance use: Effects on early adolescents’ alcohol, tobacco, and marijuana use. J. Stud. Alcohol Drugs 2010, 71, 488–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eisenberg, M.E.; Forster, J.L. Adolescent smoking behavior: Measures of social norms. Am. J. Prev. Med. 2003, 25, 122–128. [Google Scholar] [CrossRef]
- Kumar, R.; O’Malley, P.M.; Johnston, L.D.; Schulenberg, J.E.; Bachman, J.G. Effects of school-level norms on student substance use. Prev. Sci. 2002, 3, 105–124. [Google Scholar] [CrossRef]
- Turner, L.; Mermelstein, R.; Flay, B. Individual and contextual influences on adolescent smoking. Ann. N. Y. Acad. Sci. 2004, 1021, 175–197. [Google Scholar] [CrossRef] [PubMed]
- Paek, H.J.; Hove, T.; Oh, H.J. Multilevel analysis of the impact of school-level tobacco policies on adolescent smoking: The case of Michigan. J. Sch. Health 2013, 83, 679–689. [Google Scholar] [CrossRef]
- Lippert, A.M. Association between school-level prevalence of electronic cigarette use and student-level use behaviors, pre-use intentions, and risk perceptions: Evidence from the 2014 US National Youth Tobacco Survey. Nicotine Tob. Res. 2016, 20, 231–238. [Google Scholar] [CrossRef]
- Flay, B.R.; Petraitis, J. A new theory of health behavior with implications for preventive interventions. Adv. Med. Sociol. 1994, 4, 19–44. [Google Scholar]
- Murnaghan, D.; Leatherdale, S.; Sihvonen, M.; Kekki, P. A multilevel analysis examining the association between school-based smoking policies, prevention programs and youth smoking behavior: Evaluating a provincial tobacco control strategy. Health Educ. Res. 2008, 23, 1016–1028. [Google Scholar] [CrossRef]
- Leatherdale, S.T.; Brown, K.S.; Cameron, R.; McDonald, P.W. Social modeling in the school environment, student characteristics, and smoking susceptibility: A multi-level analysis. J. Adolesc. Health 2005, 37, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Maes, L.; Lievens, J. Can the school make a difference? A multilevel analysis of adolescent risk and health behaviour. Soc. Sci. Med. 2003, 56, 517–529. [Google Scholar] [CrossRef]
- USDHHS. Preventing Tobacco Use Among Young People: A Report of the Surgeon General; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 1994. [Google Scholar]
- Flay, B.R. The promise of long-term effectiveness of school-based smoking prevention programs: A critical review of reviews. Tob. Induc. Dis. 2009, 5, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, R.E.; McLellan, J.; Perera, R. School-based programmes for preventing smoking. Evid. Based Child Health 2013, 8, 1616–2040. [Google Scholar] [CrossRef]
- Müller-Riemenschneider, F.; Bockelbrink, A.; Reinhold, T.; Rasch, A.; Greiner, W.; Willich, S.N. Long-term effectiveness of behavioural interventions to prevent smoking among children and youth. Tob. Control 2008, 17, 301–302. [Google Scholar] [CrossRef] [PubMed]
- Galanti, M.R.; Coppo, A.; Jonsson, E.; Bremberg, S.; Faggiano, F. Anti-tobacco policy in schools: Upcoming preventive strategy or prevention myth? A review of 31 studies. Tob. Control 2014, 23, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Coppo, A.; Galanti, M.R.; Giordano, L.; Buscemi, D.; Bremberg, S.; Faggiano, F. School policies for preventing smoking among young people. Cochrane Database. Syst. Rev. 2014, 10, CD009990. [Google Scholar] [CrossRef]
- Schreuders, M.; Nuyts, P.A.; Putte, B. Understanding the impact of school tobacco policies on adolescent smoking behaviour: A realist review. Soc. Sci. Med. 2017, 183, 19–27. [Google Scholar] [CrossRef]
- Lim, M.K.; Cho, H.J. Current status of tobacco control policies in Korea compared with international treaty and its implementation. J. Korean Med. Assoc. 2018, 61, 148–156. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare, Korea Health Promotion Institute. Guidelines for School-Based Tobacco Control Programs; Ministry of Health and Welfare: Sejong, Korea, 2015.
- Korea Centers for Disease Control and Prevention. Statistics on the 14th Korea Youth Risk Behavior Web-based Survey. 2018. Available online: http://yhs.cdc.go.kr/ (accessed on 2 July 2018).
- Bonell, C.P.; Fletcher, A.; Jamal, F.; Wells, H.; Harden, A.; Murphy, S.; Thomas, J. Theories of how the school environment impacts on student health: Systematic review and synthesis. Health Place 2013, 24, 242–249. [Google Scholar] [CrossRef]
- Chung, A.; Rimal, R.N. Social norms: A review. Rev. Commun. Res. 2016, 4, 1–28. [Google Scholar]
- Lapinski, M.K.; Rimal, R.N. An explication of social norms. Commun. Theory 2005, 15, 127–147. [Google Scholar] [CrossRef]
- Schreuders, M.; Klompmaker, L.; van den Putte, B.; Kunst, A.E. Adolescent smoking in secondary schools that have implemented smoke-free policies: In-depth exploration of shared smoking patterns. Int. J. Environ. Res. Public Health 2019, 16, 2100. [Google Scholar] [CrossRef] [Green Version]
- Schreuders, M.; Van Den Putte, B.; Mlinarić, M.; Mélard, N.; Perelman, J.; Richter, M.; Rimpela, A.; Kuipers, M.A.G.; Lorant, V.; Kunst, A.E. The association between smoke-free school policies and adolescents’ perceived anti-smoking norms: Moderation by school connectedness. Nicotine Tob. Res. 2019, 1–9. Available online: https://0-academic-oup-com.brum.beds.ac.uk/ntr/advance-article/doi/10.1093/ntr/ntz212/5625398 (accessed on 13 May 2020). [CrossRef] [PubMed]
- Pokorny, S.B.; Jason, L.A.; Schoeny, M. Current smoking among young adolescents: Assessing school based contextual norms. Tob. Control 2004, 13, 301–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guindon, G.E.; Georgiades, K.; Boyle, M.H. Susceptibility to smoking among South East Asian youth: A multilevel analysis. Tob. Control 2008, 17, 190–197. [Google Scholar] [CrossRef] [Green Version]
- Dedobbeleer, N.; Béland, F.; Contandriopoulos, A.P.; Adrian, M. Gender and the social context of smoking behaviour. Soc. Sci. Med. 2004, 58, 1–12. [Google Scholar] [CrossRef]
- Pförtner, T.K.; Hublet, A.; Schnohr, C.W.; Rathmann, K.; Moor, I.; De Looze, M.; Baška, T.; Molcho, M.; Kannas, L.; Kunst, A.E.; et al. Socioeconomic inequalities in the impact of tobacco control policies on adolescent smoking. A multilevel study in 29 European countries. Addict. Behav. 2016, 53, 58–66. [Google Scholar] [CrossRef]
- Grogan, S.; Conner, M.; Fry, G.; Gough, B.; Higgins, A. Gender differences in smoking: A longitudinal study of beliefs predicting smoking in 11–15 year olds. Psychol. Health 2009, 24, 301–316. [Google Scholar] [CrossRef]
- Grard, A.; Schreuders, M.; Alves, J.; Kinnunen, J.M.; Richter, M.; Federico, B.; Kunst, A.; Clancy, L.; Lorant, V. Smoking beliefs across genders, a comparative analysis of seven European countries. BMC Public Health 2019, 19, 1321. [Google Scholar] [CrossRef]
- Mackie, G.; Moneti, F.; Shakya, H.; Denny, E. What are social norms? How are they measured. In University of California at San Diego-UNICEF Working Paper; University of California: San Diego, CA, USA, 2015. [Google Scholar]
- Cislaghi, B.; Heise, L. Theory and practice of social norms interventions: Eight common pitfalls. Glob. Health 2018, 14, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikaj, S.; Chaloupka, F. School personnel smoking, school-level policies, and adolescent smoking in low-and middle-income countries. Tob. Control 2016, 25, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Alesci, N.L.; Forster, J.L.; Blaine, T. Smoking visibility, perceived acceptability, and frequency in various locations among youth and adults. Prev. Med. 2003, 36, 272–281. [Google Scholar] [CrossRef]
- Linnansaari, A.; Schreuders, M.; Kunst, A.E.; Rimpelä, A.; Lindfors, P. Understanding school staff members’ enforcement of school tobacco policies to achieve tobacco-free school: A realist review. Syst. Rev. 2019, 8, 177. [Google Scholar] [CrossRef] [PubMed]
- Unger, J.B.; Rohrbach, L.A.; Howard, K.A.; Cruz, T.B.; Johnson, C.A.; Chen, X. Attitudes toward anti-tobacco policy among California youth: Associations with smoking status, psychosocial variables and advocacy actions. Health Educ. Res. 1999, 14, 751–763. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatnagar, A.; Whitsel, L.P.; Blaha, M.J.; Huffman, M.D.; Krishan-Sarin, S.; Maa, J.; Rigotti, N.; Robertson, R.M.; Warner, J.J. New and emerging tobacco products and the nicotine endgame: The role of robust regulation and comprehensive tobacco control and prevention: A presidential advisory from the American Heart Association. Circulation 2019, 139, e937–e958. [Google Scholar] [CrossRef]
- Hansen, W.B.; Graham, J.W. Preventing alcohol, marijuana, and cigarette use among adolescents: Peer pressure resistance training versus establishing conservative norms. Prev. Med. 1991, 20, 414–430. [Google Scholar] [CrossRef]
- Flay, B.R.; Petraitis, J.; Hu, F.B. Psychosocial risk and protective factors for adolescent tobacco use. Nicotine Tob. Res. 1999, 1, s59–s65. [Google Scholar] [CrossRef]
- Simons-Morton, B.G.; Farhat, T. Recent findings on peer group influences on adolescent smoking. J. Prim. Prev. 2010, 31, 191–208. [Google Scholar] [CrossRef] [Green Version]

| Total Sample | Smoking Status | p-Value | ||
|---|---|---|---|---|
| Yes | No | |||
| n (%) | n (%) | n (%) | ||
| All | 4631 (100.0) | 243 (5.2) | 4388 (94.8) | |
| Gender | ||||
| Boys | 2260 (48.8) | 182 (8.0) | 2078 (92.0) | <0.0001 |
| Girls | 2371 (51.2) | 61 (2.6) | 2310 (97.4) | |
| Grade | ||||
| 7 | 945 (20.4) | 14 (1.5) | 931 (98.5) | <0.0001 |
| 8 | 976 (21.1) | 22 (2.2) | 954 (97.8) | |
| 9 | 906 (19.6) | 36 (4.0) | 870 (96.0) | |
| 10 | 737 (15.9) | 68 (9.2) | 669 (90.8) | |
| 11 | 675 (14.6) | 57 (8.4) | 618 (91.6) | |
| 12 | 392 (8.5) | 46 (11.7) | 346 (88.3) | |
| # of programs participated in | ||||
| 0–1 | 1602 (34.6) | 139 (8.7) | 1463 (91.3) | <0.0001 |
| 2–3 | 1696 (36.6) | 71 (4.2) | 1625 (95.8) | |
| ≥4 | 1333 (28.8) | 33 (2.5) | 1300 (97.5) | |
| Witnessed teachers smoking | ||||
| Yes | 1289 (27.8) | 144 (11.2) | 1145 (88.8) | <0.0001 |
| No | 3342 (72.2) | 99 (3.0) | 3243 (97.0) | |
| Attitudes toward tobacco use [Mean (SD)] | 27.5 (4.2) | 21.6 (5.1) | 27.9 (3.9) | <0.0001 |
| Attitudes regarding tobacco control regulations [Mean (SD)] | 11.9 (4.0) | 9.5 (3.3) | 12.0 (4.0) | <0.0001 |
| Distribution of School Characteristics | Distribution of Smoking Prevalence in School | ||
|---|---|---|---|
| n (%) | Mean | SD | |
| All | 62 (100.0) | 5.80 | 9.43 |
| School type | |||
| Boys-only | 5 (8.0) | 10.66 | 5.02 |
| Girls-only | 13 (21.0) | 2.22 | 3.53 |
| Co-education | 44 (71.0) | 6.30 | 10.65 |
| Tobacco-free school declaration | |||
| Yes | 26 (41.9) | 5.55 | 7.15 |
| No | 36 (58.1) | 5.98 | 10.88 |
| # of staff | |||
| 1–3 | 38 (61.3) | 6.35 | 11.41 |
| ≥4 | 24 (38.7) | 4.91 | 5.01 |
| Years as a tobacco-free school | |||
| 0 | 43 (69.4) | 6.75 | 11.05 |
| 1 | 11 (17.7) | 3.86 | 3.91 |
| ≥2 | 8 (12.9) | 3.35 | 1.52 |
| School smoking rates | |||
| 0–5% | 41 (66.1) | 1.57 | 1.57 |
| 5–10% | 11 (17.7) | 6.96 | 1.41 |
| >10% | 10 (16.1) | 21.83 | 14.87 |
| School norm towards tobacco use 1 | |||
| Quartile 1 | 17 (27.4) | 14.94 | 14.08 |
| Quartile 2 | 15 (24.2) | 3.41 | 3.27 |
| Quartile 3 | 14 (22.6) | 2.94 | 2.29 |
| Quartile 4 | 16 (25.8) | 0.83 | 1.14 |
| School norm regarding tobacco control regulations 2 | |||
| Quartile 1 | 17 (27.4) | 12.11 | 15.24 |
| Quartile 2 | 16 (25.8) | 5.25 | 4.98 |
| Quartile 3 | 13 (21.0) | 3.75 | 3.37 |
| Quartile 4 | 16 (25.8) | 1.30 | 3.03 |
| Current Smoking | |||||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Intercept | 0.03 (0.02–0.04) * | 0.01 (0.01–0.02) * | 0.04 (0.02–0.08) * | 0.01 (0.01–0.04) * | 0.00 (0.00–0.01) * |
| Student level | |||||
| Gender | |||||
| Boys | 1.00 | 1.00 | 1.00 | ||
| Girls | 0.42 (0.27–0.66) * | 0.71 (0.44–1.14) | 0.81 (0.50–1.32) | ||
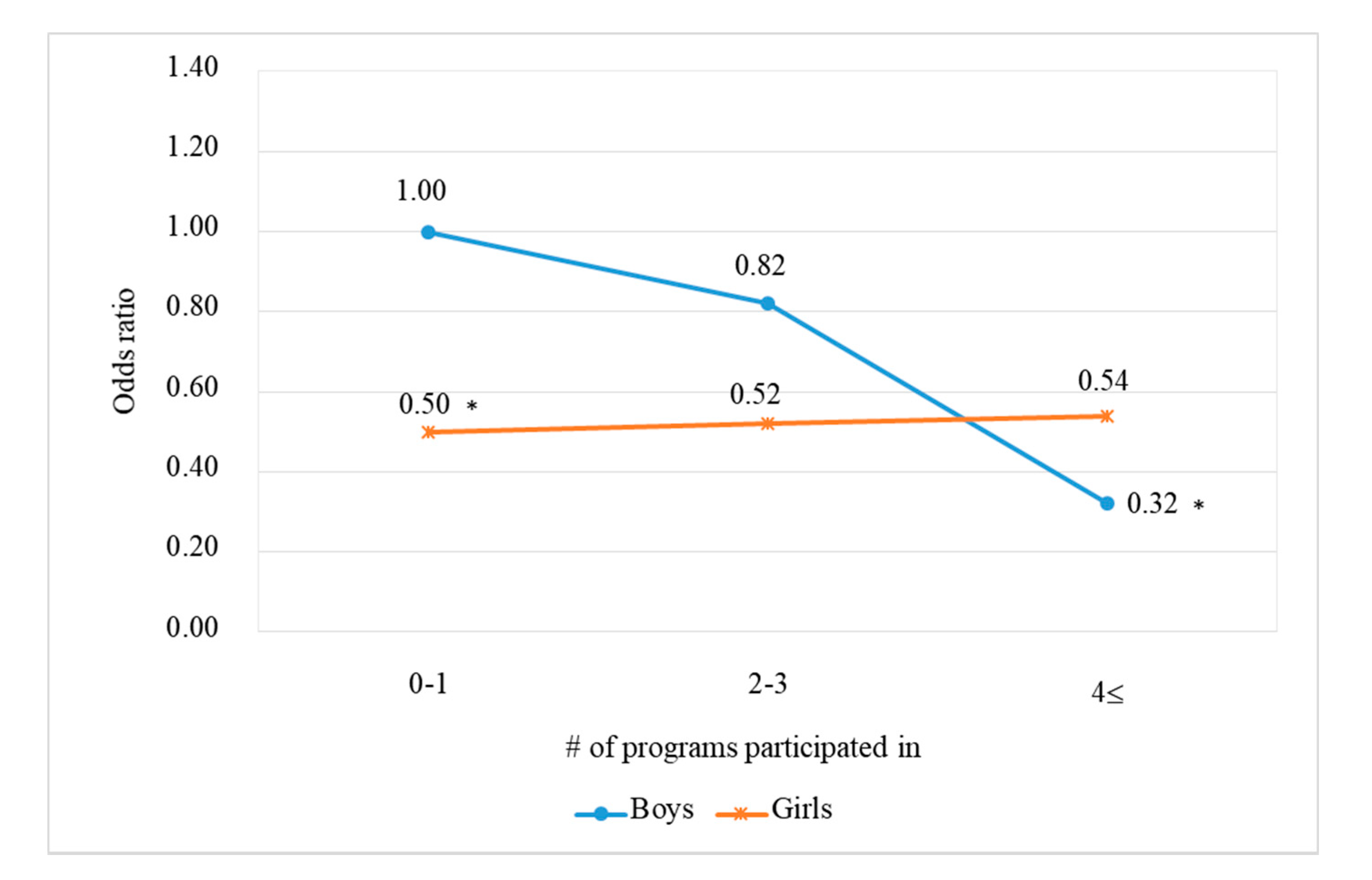
| # of programs participated in | |||||
| 0–1 | 1.00 | 1.00 | 1.00 | ||
| 2–3 | 0.85 (0.59–1.22) | 0.85 (0.60–1.22) | 1.70 (1.06–2.75) * | ||
| ≥4 | 0.46 (0.29–0.73) * | 0.47 (0.30–0.74) * | 1.58 (0.97–2.58) | ||
| Witnessed teachers smoking | |||||
| No | 1.00 | 1.00 | 1.00 | ||
| Yes | 2.91 (2.12–4.00) * | 2.57 (1.88–3.51) * | 2.56 (1.87–3.50) * | ||
| Attitudes toward tobacco use | 0.57 (0.51–0.63) * | 0.56 (0.51–0.63) * | 0.56 (0.50–0.62) * | ||
| Attitudes regarding tobacco control regulations | 0.56 (0.47–0.66) * | 0.54 (0.46–0.64) * | 0.54 (0.46–0.65) * | ||
| School level | |||||
| School type | |||||
| Coeducation | 1.00 | 1.00 | 1.00 | ||
| Boys only | 0.91 (0.48–1.71) | 0.72 (0.32–1.60) | 0.64 (0.29–1.39) | ||
| Girls only | 1.00 (0.49–2.04) | 1.20 (0.45–3.22) | 1.18 (0.46–3.00) | ||
| Tobacco-free school declaration | |||||
| No | 1.00 | 1.00 | 1.00 | ||
| Yes | 1.06 (0.68–1.65) | 0.94 (0.54–1.61) | 0.99 (0.58–1.68) | ||
| # of staff | |||||
| 1–3 | 1.00 | 1.00 | 1.00 | ||
| ≥4 | 0.67 (0.41–1.09) | 0.69 (0.38–1.24) | 0.76 (0.42–1.36) | ||
| Years as a tobacco-free school | |||||
| 0 | 1.00 | 1.00 | 1.00 | ||
| 1 | 1.34 (0.80–2.27) | 1.53 (0.80–2.95) | 1.52 (0.80–2.89) | ||
| ≥2 | 1.85 (1.01–3.39) * | 2.01 (0.99–4.09) | 2.15 (1.06–4.34) * | ||
| School smoking rates | |||||
| 0–5% | 1.00 | 1.00 | 1.00 | ||
| 5–10% | 3.20 (1.90–5.41) * | 3.84 (2.00–7.39) * | 4.16 (2.18–7.95) * | ||
| >10% | 9.71 (5.03–18.73) * | 9.29 (3.57–24.19) * | 9.95 (3.91–25.31) * | ||
| School norm towards tobacco use 1 | |||||
| Q1 | 1.00 | 1.00 | 1.00 | ||
| Q2–Q3 | 0.68 (0.36–1.27) | 0.83 (0.38–1.80) | 0.87 (0.41–1.86) | ||
| Q4 | 0.36 (0.14–0.90) * | 0.50 (0.17–1.46) | 0.45 (0.16–1.25) | ||
| School norm regarding tobacco control regulations 2 | |||||
| Q1 | 1.00 | 1.00 | |||
| Q2–Q3 | 0.71 (0.47–1.07) | 0.65 (0.39–1.08) | |||
| Q4 | 0.32 (0.13–0.75) * | 0.28 (0.11–0.76) * | |||
| Interactions | |||||
| # of programs (2–3) × Gender | 1.27 (0.57–2.82) | ||||
| # of programs (≥4) × Gender | 3.33 (1.31–8.48) * | ||||
| School norm regarding tobacco control regulations2 × Gender | 0.28 (0.12–0.65) * | ||||
| School–level random variance | 1.8368 * | 1.0204 * | 0.0739 | 0.1839 | 0.1644 |
| AIC | 1673.37 | 1394.18 | 1593.07 | 1354.04 | 1346.81 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Jang, M.; Yoo, S.; JeKarl, J.; Chung, J.Y.; Cho, S.-i. School-Based Tobacco Control and Smoking in Adolescents: Evidence from Multilevel Analyses. Int. J. Environ. Res. Public Health 2020, 17, 3422. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103422
Kim SY, Jang M, Yoo S, JeKarl J, Chung JY, Cho S-i. School-Based Tobacco Control and Smoking in Adolescents: Evidence from Multilevel Analyses. International Journal of Environmental Research and Public Health. 2020; 17(10):3422. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103422
Chicago/Turabian StyleKim, Seong Yeon, Myungwha Jang, Seunghyun Yoo, Jung JeKarl, Joo Youn Chung, and Sung-il Cho. 2020. "School-Based Tobacco Control and Smoking in Adolescents: Evidence from Multilevel Analyses" International Journal of Environmental Research and Public Health 17, no. 10: 3422. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17103422





