Effect of Height of Fall on Mortality in Patients with Fall Accidents: A Retrospective Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
2.1. Ethical Statement
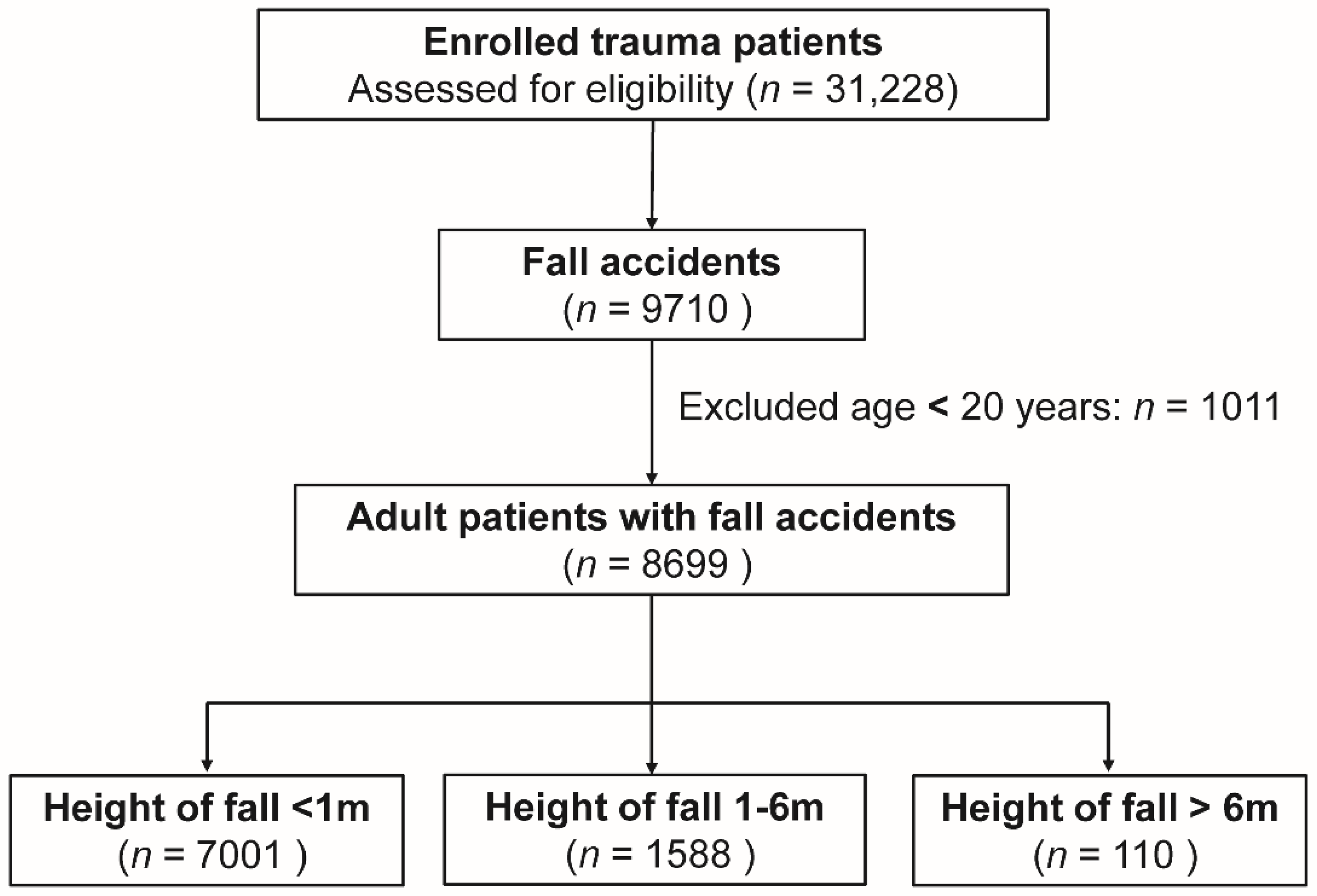
2.2. Study Population
2.3. Data Collection and Outcome Measures
2.4. Statistical Analysis
3. Results
3.1. Study Populations
3.2. Patient and Injury Characteristics
3.3. Physiological Responses and Procedures Performed
3.4. Associated Injuries on Body Regions
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AIS | Abbreviated injury scale |
| AOR | adjusted odds ratio |
| CI | confidence interval |
| CAD | coronary artery disease |
| CHF | congestive heart failure |
| CVA | cerebrovascular accident |
| DM | diabetes mellitus |
| ED | emergency department |
| ESRD | end stage renal disease |
| GCS | Glasgow Coma Scale |
| GLF | ground-level falls |
| HTN | hypertension |
| ICU | intensive care unit |
| ISS | injury severity score |
| LOS | length of stay |
| OR | odds ratio |
| RR | respiratory rate |
| RTS | revised trauma score |
| SBP | systolic blood pressure |
References
- Murray, C.J.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- World Health Organization, Falls, Fact sheet N 344 (2010). Available online: http://www.who.int/ediacentre/factsheets/fs344/en/index.html (accessed on 1 May 2020).
- Kennedy, R.L.; Grant, P.T.; Blackwell, D. Low-impact falls: Demands on a system of trauma management, prediction of outcome, and influence of comorbidities. J. Trauma 2001, 51, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Nakada, T.A.; Nakao, S.; Mizushima, Y.; Matsuoka, T. Association between male sex and increased mortality after falls. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2015, 22, 708–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rau, C.S.; Lin, T.S.; Wu, S.C.; Yang, J.C.; Hsu, S.Y.; Cho, T.Y.; Hsieh, C.H. Geriatric hospitalizations in fall-related injuries. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warner, K.G.; Demling, R.H. The pathophysiology of free-fall injury. Ann. Emerg. Med. 1986, 15, 1088–1093. [Google Scholar] [CrossRef]
- American College of Surgeons Committee on Trauma. Advanced Trauma Life Support for Doctors; American College of Surgeons: Chicago, IL, USA, 2004. [Google Scholar]
- Liu, C.C.; Wang, C.Y.; Shih, H.C.; Wen, Y.S.; Wu, J.J.; Huang, C.I.; Hsu, H.S.; Huang, M.H.; Huang, M.S. Prognostic factors for mortality following falls from height. Injury 2009, 40, 595–597. [Google Scholar] [CrossRef]
- Lapostolle, F.; Gere, C.; Borron, S.W.; Petrovic, T.; Dallemagne, F.; Beruben, A.; Lapandry, C.; Adnet, F. Prognostic factors in victims of falls from height. Crit. Care Med. 2005, 33, 1239–1242. [Google Scholar] [CrossRef]
- Dickinson, A.; Roberts, M.; Kumar, A.; Weaver, A.; Lockey, D.J. Falls from height: Injury and mortality. J. R. Army Med. Corps 2012, 158, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Icer, M.; Guloglu, C.; Orak, M.; Ustundag, M. Factors affecting mortality caused by falls from height. Ulus. Travma Acil. Cerrahi. Derg. 2013, 19, 529–535. [Google Scholar] [CrossRef] [Green Version]
- Katz, K.; Gonen, N.; Goldberg, I.; Mizrahi, J.; Radwan, M.; Yosipovitch, Z. Injuries in attempted suicide by jumping from a height. Injury 1988, 19, 371–374. [Google Scholar] [CrossRef]
- Agalar, F.; Cakmakci, M.; Sayek, I. Factors effecting mortality in urban vertical free falls: Evaluation of 180 cases. Int. Surg. 1999, 84, 271–274. [Google Scholar] [PubMed]
- Goodacre, S.; Than, M.; Goyder, E.C.; Joseph, A.P. Can the distance fallen predict serious injury after a fall from a height? J. Trauma 1999, 46, 1055–1058. [Google Scholar] [CrossRef] [PubMed]
- Beale, J.P.; Wyatt, J.P.; Beard, D.; Busuttil, A.; Graham, C.A. A five year study of high falls in Edinburgh. Injury 2000, 31, 503–508. [Google Scholar] [CrossRef]
- Spaniolas, K.; Cheng, J.D.; Gestring, M.L.; Sangosanya, A.; Stassen, N.A.; Bankey, P.E. Ground level falls are associated with significant mortality in elderly patients. J. Trauma 2010, 69, 821–825. [Google Scholar] [CrossRef] [PubMed]
- Helling, T.S.; Watkins, M.; Evans, L.L.; Nelson, P.W.; Shook, J.W.; Van Way, C.W. Low falls: An underappreciated mechanism of injury. J. Trauma 1999, 46, 453–456. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.H.; Nguyen, H.V.; Chiu, M.T.; Chow, K.Y.; Ong, M.E.; Lim, G.H.; Nadkarni, N.V.; Bautista, D.C.; Cheng, J.Y.; Loo, L.M.; et al. The Low Fall as a Surrogate Marker of Frailty Predicts Long-Term Mortality in Older Trauma Patients. PLoS ONE 2015, 10, e0137127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.; Bein, K.J.; Ivers, R.; Dinh, M.M. Changing patterns of injury associated with low-energy falls in the elderly: A 10-year analysis at an Australian Major Trauma Centre. ANZ J. Surg. 2015, 85, 230–234. [Google Scholar] [CrossRef]
- Hsieh, C.H.; Chen, Y.C.; Hsu, S.Y.; Hsieh, H.Y.; Chien, P.C. Defining polytrauma by abbreviated injury scale >/= 3 for a least two body regions is insufficient in terms of short-term outcome: A cross-sectional study at a level I trauma center. Biomed J. 2018, 41, 321–327. [Google Scholar] [CrossRef]
- Hsieh, C.H.; Hsu, S.Y.; Hsieh, H.Y.; Chen, Y.C. Differences between the sexes in motorcycle-related injuries and fatalities at a Taiwanese level I trauma center. Biomed. J. 2017, 40, 113–120. [Google Scholar] [CrossRef]
- Hsieh, C.H.; Liu, H.T.; Hsu, S.Y.; Hsieh, H.Y.; Chen, Y.C. Motorcycle-related hospitalizations of the elderly. Biomed. J. 2017, 40, 121–128. [Google Scholar] [CrossRef]
- Son, H.M.; Kim, S.H.; Shin, S.D.; Ryoo, H.W.; Ryu, H.H.; Lee, J.H. Occupational fall injuries presenting to the emergency department. Emerg. Med. Australas 2014, 26, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Jagnoor, J.; Keay, L.; Ganguli, A.; Dandona, R.; Thakur, J.S.; Boufous, S.; Cumming, R.; Ivers, R.Q. Fall related injuries: A retrospective medical review study in North India. Injury 2012, 43, 1996–2000. [Google Scholar] [CrossRef] [PubMed]
- Taira, T.; Morita, S.; Umebachi, R.; Miura, N.; Icimura, A.; Inoue, S.; Nakagawa, Y.; Inokuchi, S. Risk factors for ground-level falls differ by sex. Am. J. Emerg. Med. 2015, 33, 640–644. [Google Scholar] [CrossRef]
- Reginster, J.Y.; Kaufman, J.M.; Goemaere, S.; Devogelaer, J.P.; Benhamou, C.L.; Felsenberg, D.; Diaz-Curiel, M.; Brandi, M.L.; Badurski, J.; Wark, J.; et al. Maintenance of antifracture efficacy over 10 years with strontium ranelate in postmenopausal osteoporosis. Osteoporos. Int. 2012, 23, 1115–1122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menz, H.B.; Lord, S.R. Footwear and postural stability in older people. J. Am. Podiatr. Med. Assoc. 1999, 89, 346–357. [Google Scholar] [CrossRef]
- Hannan, E.L.; Mendeloff, J.; Farrell, L.S.; Cayten, C.G.; Murphy, J.G. Multivariate models for predicting survival of patients with trauma from low falls: The impact of gender and pre-existing conditions. J. Trauma 1995, 38, 697–704. [Google Scholar] [CrossRef]
- Velmahos, G.C.; Jindal, A.; Chan, L.S.; Murray, J.A.; Vassiliu, P.; Berne, T.V.; Asensio, J.; Demetriades, D. “Insignificant” mechanism of injury: Not to be taken lightly. J. Am. Coll. Surg. 2001, 192, 147–152. [Google Scholar] [CrossRef]
- Atanasijevic, T.C.; Savic, S.N.; Nikolic, S.D.; Djoki, V.M. Frequency and severity of injuries in correlation with the height of fall. J. Forensic Sci. 2005, 50, 608–612. [Google Scholar] [CrossRef]
- Petaros, A.; Slaus, M.; Coklo, M.; Sosa, I.; Cengija, M.; Bosnar, A. Retrospective analysis of free-fall fractures with regard to height and cause of fall. Forensic Sci. Int. 2013, 226, 290–295. [Google Scholar] [CrossRef]
- Lau, G.; Ooi, P.L.; Phoon, B. Fatal falls from a height: The use of mathematical models to estimate the height of fall from the injuries sustained. Forensic Sci. Int. 1998, 93, 33–44. [Google Scholar] [CrossRef]
- Champion, H.R.; Sacco, W.J.; Copes, W.S.; Gann, D.S.; Gennarelli, T.A.; Flanagan, M.E. A revision of the Trauma Score. J. Trauma 1989, 29, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Akkoca, M.; Tokgoz, S.; Yilmaz, K.B.; Guler, S.; Akinci, M.; Balas, S.; Karabacak, H.; Saydam, M. Mortality determiners for fall from height cases. Ulus. Travma Acil. Cerrahi. Derg. 2018, 24, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Casali, M.B.; Battistini, A.; Blandino, A.; Cattaneo, C. The injury pattern in fatal suicidal falls from a height: An examination of 307 cases. Forensic Sci. Int. 2014, 244, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Nadhim, E.A.; Hon, C.; Xia, B.; Stewart, I.; Fang, D. Falls from Height in the Construction Industry: A Critical Review of the Scientific Literature. Int. J. Environ. Res. Public Health 2016, 13, 638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variables | <1 m | 1–6 m | >6 m | 1–6 m vs. <1 m | >6 m vs. <1 m | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 7001) | (n = 1588) | (n = 110) | OR (95% CI) | p | OR (95% CI) | p | ||||||
| Age, (years) | 68.7 | ±15.6 | 53.1 | ±15.3 | 42.2 | ±14.7 | - | <0.001 | - | <0.001 | ||
| Gender, n (%) | <0.001 | <0.001 | ||||||||||
| Male | 2533 | (36.2) | 1241 | (78.1) | 83 | (75.5) | 6.3 | (5.55–7.17) | 5.4 | (3.50–8.39) | ||
| Female | 4468 | (63.8) | 347 | (21.9) | 27 | (24.5) | 0.2 | (0.14–0.18) | 0.2 | (0.12–0.29) | ||
| Intention, n (%) | 0 | (0.0) | 15 | (0.9) | 33 | (30.0) | - | <0.001 | - | <0.001 | ||
| Non-intention, n (%) | 6975 | (99.6) | 1564 | (98.5) | 74 | (67.3) | 0.2 | (0.14–0.42) | <0.001 | 0.01 | (0.00–0.01) | <0.001 |
| Comorbidities, n (%) | ||||||||||||
| CVA | 794 | (11.3) | 39 | (2.5) | 1 | (0.9) | 0.2 | (0.14–0.27) | <0.001 | 0.1 | (0.01–0.51) | 0.001 |
| HTN | 3658 | (52.2) | 377 | (23.7) | 8 | (7.3) | 0.3 | (0.25–0.32) | <0.001 | 0.1 | (0.04–0.15) | <0.001 |
| CAD | 569 | (8.1) | 52 | (3.3) | 1 | (0.9) | 0.4 | (0.29–0.51) | <0.001 | 0.1 | (0.01–0.74) | 0.006 |
| CHF | 141 | (2.0) | 9 | (0.6) | 0 | (0.0) | 0.3 | (0.14–0.55) | <0.001 | - | 0.133 | |
| DM | 1930 | (27.6) | 230 | (14.5) | 6 | (5.5) | 0.4 | (0.38–0.52) | <0.001 | 0.2 | (0.07–0.35) | <0.001 |
| ESRD | 355 | (5.1) | 20 | (1.3) | 0 | (0.0) | 0.2 | (0.15–0.38) | <0.001 | - | 0.015 | |
| Variables | <1 m | 1–6 m | >6 m | 1–6 m vs. <1 m | >6 m vs. <1 m | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 7001) | (n = 1588) | (n = 110) | OR (95% CI) | p | OR (95% CI) | p | ||||||
| GCS (median, IQR) | 15.0 | (15.0–15.0) | 15.0 | (15.0–15.0) | 15 | (12.8–15.0) | - | <0.001 | - | <0.001 | ||
| 3–8 | 164 | (2.3) | 94 | (5.9) | 14 | (12.7) | 2.6 | (2.02–3.40) | <0.001 | 6.1 | (3.40–10.88) | <0.001 |
| 9–12 | 203 | (2.9) | 67 | (4.2) | 13 | (11.8) | 1.5 | (1.11–1.96) | 0.007 | 4.5 | (2.47–8.14) | <0.001 |
| 13–15 | 6634 | (94.8) | 1427 | (89.9) | 83 | (75.5) | 0.5 | (0.40–0.60) | <0.001 | 0.2 | (0.11–0.27) | <0.001 |
| ISS (median, IQR) | 9.0 | (4.0–9.0) | 9.0 | (4.0–14.0) | 17.5 | (9.0–25.0) | - | <0.001 | - | <0.001 | ||
| 1–15 | 6189 | (88.4) | 1197 | (75.4) | 46 | (41.8) | 0.4 | (0.35–0.46) | <0.001 | 0.1 | (0.06–0.14) | <0.001 |
| 16–24 | 659 | (9.4) | 267 | (16.8) | 35 | (31.8) | 1.9 | (1.67–2.27) | <0.001 | 4.5 | (2.98–6.76) | <0.001 |
| ≥25 | 153 | (2.2) | 124 | (7.8) | 29 | (26.4) | 3.8 | (2.97–4.84) | <0.001 | 16.0 | (10.18–25.22) | <0.001 |
| AIS ≥ 2 | ||||||||||||
| Head/Neck, n (%) | 1098 | (15.7) | 437 | (27.5) | 39 | (35.5) | 2.0 | (1.80–2.32) | <0.001 | 3.0 | (1.99–4.39) | <0.001 |
| Face, n (%) | 185 | (2.6) | 122 | (7.7) | 25 | (22.7) | 3.1 | (2.42–3.88) | <0.001 | 10.8 | (6.78–17.33) | <0.001 |
| Thorax, n (%) | 253 | (3.6) | 289 | (18.2) | 52 | (47.3) | 5.9 | (4.96–7.10) | <0.001 | 23.9 | (16.11–35.49) | <0.001 |
| Abdomen, n (%) | 159 | (2.3) | 187 | (11.8) | 50 | (45.5) | 5.7 | (4.61–7.15) | <0.001 | 35.9 | (23.87–53.87) | <0.001 |
| Extremity, n (%) | 5394 | (77.0) | 1003 | (63.2) | 85 | (77.3) | 0.5 | (0.46–0.57) | <0.001 | 1.0 | (0.65–1.59) | 0.955 |
| LOS in hospital, (days) | 8.2 | ±8.2 | 10.6 | ±11.1 | 21.2 | ±16.0 | - | <0.001 | - | <0.001 | ||
| ICU admission, n (%) | 1027 | (14.7) | 368 | (23.2) | 64 | (58.2) | 1.8 | (1.53–2.01) | <0.001 | 8.1 | (5.51–11.89) | <0.001 |
| Mortality, n (%) | 178 | (2.5) | 56 | (3.5) | 6 | (5.5) | 1.4 | (1.03–1.90) | 0.033 | 2.2 | (0.96–5.10) | 0.056 |
| AOR of mortality | - | - | - | 2.2 | (1.64–2.89) | <0.001 | 2.5 | (1.84–3.38) | 0.001 | |||
| AOR of mortality (ISS) | - | - | - | 1.4 | (0.95–2.22) | 0.082 | 10.0 | (2.22–33.33) | 0.002 | |||
| Variables | <1 m | 1–6 m | >6 m | 1–6 m vs. < 1 m | >6 m vs. <1 m | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 7001) | (n = 1588) | (n = 110) | OR (95% CI) | p | OR (95% CI) | p | ||||||
| Physiological response at ED, n (%) | ||||||||||||
| GCS < 13 | 367 | (5.2) | 161 | (10.1) | 27 | (24.5) | 2.0 | (1.68–2.48) | <0.001 | 5.9 | (3.76–9.19) | <0.001 |
| SBP < 90 mmHg | 57 | (0.8) | 29 | (1.8) | 7 | (6.4) | 2.3 | (1.44–3.56) | 0.001 | 8.3 | (3.69–18.59) | <0.001 |
| RR< 10 or > 29 beats/min | 5 | (0.1) | 12 | (0.8) | 4 | (3.6) | 10.7 | (3.75–30.28) | <0.001 | 52.8 | (13.98–199.38) | <0.001 |
| Procedures performed at ED, n (%) | ||||||||||||
| Endotracheal intubation | 90 | (1.3) | 67 | (4.2) | 16 | (14.5) | 3.4 | (2.45–4.66) | <0.001 | 13.1 | (7.40–23.10) | <0.001 |
| Chest tube insertion | 27 | (0.4) | 35 | (2.2) | 14 | (12.7) | 5.8 | (3.51–9.65) | <0.001 | 37.7 | (19.16–74.07) | <0.001 |
| Blood transfusion | 144 | (2.1) | 58 | (3.7) | 27 | (24.5) | 1.8 | (1.32–2.46) | <0.001 | 15.5 | (9.73–24.65) | <0.001 |
| (n = 7001) | (n = 1588) | (n = 110) | OR (95% CI) | p | OR (95% CI) | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Head trauma, n (%) | ||||||||||||
| Cranial fracture | 130 | (1.9) | 131 | (8.2) | 12 | (10.9) | 4.8 | (3.70–6.10) | <0.001 | 6.5 | (3.47–12.08) | <0.001 |
| Epidural hematoma (EDH) | 81 | (1.2) | 87 | (5.5) | 10 | (9.1) | 5.0 | (3.64–6.74) | <0.001 | 8.5 | (4.30–16.96) | <0.001 |
| Subdural hematoma (SDH) | 654 | (9.3) | 245 | (15.4) | 18 | (16.4) | 1.8 | (1.51–2.07) | <0.001 | 1.9 | (1.14–3.17) | 0.016 |
| Subarachnoid hemorrhage (SAH) | 291 | (4.2) | 175 | (11.0) | 19 | (17.3) | 2.9 | (2.35–3.47) | <0.001 | 4.8 | (2.90–8.00) | <0.001 |
| Intracerebral hematoma (ICH) | 124 | (1.8) | 50 | (3.1) | 5 | (4.5) | 1.8 | (1.29–2.52) | 0.001 | 2.6 | (1.06–6.59) | 0.049 |
| Cerebral contusion | 245 | (3.5) | 114 | (7.2) | 7 | (6.4) | 2.1 | (1.70–2.68) | <0.001 | 1.9 | (0.86–4.07) | 0.113 |
| Cervical vertebral fracture | 35 | (0.5) | 55 | (3.5) | 4 | (3.6) | 7.1 | (4.66–10.95) | <0.001 | 7.5 | (2.62–21.51) | 0.003 |
| Maxillofacial trauma, n (%) | ||||||||||||
| Orbital fracture | 37 | (0.5) | 23 | (1.4) | 3 | (2.7) | 2.8 | (1.64–4.67) | <0.001 | 5.3 | (1.60–17.38) | 0.024 |
| Nasal fracture | 14 | (0.2) | 18 | (1.1) | 1 | (0.9) | 5.7 | (2.84–11.53) | <0.001 | 4.6 | (0.60–35.13) | 0.209 |
| Maxillary fracture | 77 | (1.1) | 68 | (4.3) | 11 | (10.0) | 4.0 | (2.89–5.60) | <0.001 | 10.0 | (5.15–19.37) | <0.001 |
| Mandibular fracture | 37 | (0.5) | 20 | (1.3) | 6 | (5.5) | 2.4 | (1.39–4.15) | 0.002 | 10.9 | (4.49–26.29) | <0.001 |
| Thoracic trauma, n (%) | ||||||||||||
| Rib fracture | 200 | (2.9) | 247 | (15.6) | 34 | (30.9) | 6.3 | (5.15–7.62) | <0.001 | 15.2 | (9.91–23.34) | <0.001 |
| Sternal fracture | 1 | (0.0) | 5 | (0.3) | 1 | (0.9) | 22.1 | (2.58–189.38) | 0.001 | 64.2 | (3.99–1033.36) | 0.031 |
| Hemothorax | 7 | (0.1) | 14 | (0.9) | 7 | (6.4) | 8.9 | (3.58–22.05) | <0.001 | 67.9 | (23.40–197.09) | <0.001 |
| Pneumothorax | 24 | (0.3) | 36 | (2.3) | 9 | (8.2) | 6.7 | (4.01–11.34) | <0.001 | 25.9 | (11.75–57.13) | <0.001 |
| Hemopneumothorax | 23 | (0.3) | 40 | (2.5) | 14 | (12.7) | 7.8 | (4.68–13.13) | <0.001 | 44.2 | (22.10–88.59) | <0.001 |
| Lung contusion | 7 | (0.1) | 21 | (1.3) | 4 | (3.6) | 13.4 | (5.68–31.55) | <0.001 | 37.7 | (10.87–130.73) | <0.001 |
| Thoracic vertebral fracture | 67 | (1.0) | 68 | (4.3) | 22 | (20.0) | 4.6 | (3.29–6.52) | <0.001 | 25.9 | (15.30–43.76) | <0.001 |
| Abdominal trauma, n (%) | ||||||||||||
| Hepatic injury | 6 | (0.1) | 21 | (1.3) | 12 | (10.9) | 15.6 | (6.30–38.77) | <0.001 | 142.8 | (52.51–388.07) | <0.001 |
| Splenic injury | 4 | (0.1) | 11 | (0.7) | 2 | (1.8) | 12.2 | (3.88–38.37) | <0.001 | 32.4 | (5.87–178.74) | 0.003 |
| Retroperitoneal injury | 2 | (0.0) | 7 | (0.4) | 4 | (3.6) | 15.5 | (3.22–74.66) | <0.001 | 132.1 | (23.93–728.81) | <0.001 |
| Renal injury | 6 | (0.1) | 9 | (0.6) | 2 | (1.8) | 6.6 | (2.36–18.70) | <0.001 | 21.6 | (4.31–108.18) | 0.006 |
| Lumbar vertebral fracture | 111 | (1.6) | 150 | (9.4) | 37 | (33.6) | 6.5 | (5.03–8.33) | <0.001 | 31.5 | (20.31–48.74) | <0.001 |
| Sacral vertebral fracture | 11 | (0.2) | 28 | (1.8) | 13 | (11.8) | 11.4 | (5.67–22.96) | <0.001 | 85.2 | (37.23–194.83) | <0.001 |
| Extremity trauma, n (%) | ||||||||||||
| Clavicle fracture | 101 | (1.4) | 78 | (4.9) | 7 | (6.4) | 3.5 | (2.61–4.77) | <0.001 | 4.6 | (2.11–10.23) | 0.001 |
| Humeral fracture | 407 | (5.8) | 80 | (5.0) | 9 | (8.2) | 0.9 | (0.67–1.10) | 0.230 | 1.4 | (0.73–2.88) | 0.301 |
| Radial fracture | 952 | (13.6) | 282 | (17.8) | 17 | (15.5) | 1.4 | (1.19–1.59) | <0.001 | 1.2 | (0.69–1.96) | 0.575 |
| Ulnar fracture | 331 | (4.7) | 95 | (6.0) | 10 | (9.1) | 1.3 | (1.01–1.62) | 0.040 | 2.0 | (1.04–3.90) | 0.034 |
| Metacarpal fracture | 58 | (0.8) | 31 | (2.0) | 5 | (4.5) | 2.4 | (1.54–3.70) | <0.001 | 5.7 | (2.24–14.50) | 0.003 |
| Pelvic fracture | 53 | (0.8) | 90 | (5.7) | 30 | (27.3) | 7.9 | (5.58–11.11) | <0.001 | 49.2 | (29.84–80.98) | <0.001 |
| Femoral fracture | 2777 | (39.7) | 173 | (10.9) | 18 | (16.4) | 0.2 | (0.16–0.22) | <0.001 | 0.3 | (0.18–0.49) | <0.001 |
| Tibia fracture | 168 | (2.4) | 81 | (5.1) | 11 | (10.0) | 2.2 | (1.67–2.87) | <0.001 | 4.5 | (2.38–8.58) | <0.001 |
| Fibular fracture | 106 | (1.5) | 49 | (3.1) | 8 | (7.3) | 2.1 | (1.47–2.92) | <0.001 | 5.1 | (2.42–10.74) | <0.001 |
| Calcaneal fracture | 324 | (4.6) | 103 | (6.5) | 12 | (10.9) | 1.4 | (1.14–1.80) | 0.002 | 2.5 | (1.37–4.64) | 0.006 |
| Metatarsal fracture | 89 | (1.3) | 138 | (8.7) | 20 | (18.2) | 7.4 | (5.63–9.71) | <0.001 | 17.3 | (10.18–29.25) | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, T.-M.; Tsai, C.-H.; Liu, H.-T.; Huang, C.-Y.; Chou, S.-E.; Su, W.-T.; Hsu, S.-Y.; Hsieh, C.-H. Effect of Height of Fall on Mortality in Patients with Fall Accidents: A Retrospective Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 4163. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17114163
Hsieh T-M, Tsai C-H, Liu H-T, Huang C-Y, Chou S-E, Su W-T, Hsu S-Y, Hsieh C-H. Effect of Height of Fall on Mortality in Patients with Fall Accidents: A Retrospective Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2020; 17(11):4163. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17114163
Chicago/Turabian StyleHsieh, Ting-Min, Ching-Hua Tsai, Hang-Tsung Liu, Chun-Ying Huang, Sheng-En Chou, Wei-Ti Su, Shiun-Yuan Hsu, and Ching-Hua Hsieh. 2020. "Effect of Height of Fall on Mortality in Patients with Fall Accidents: A Retrospective Cross-Sectional Study" International Journal of Environmental Research and Public Health 17, no. 11: 4163. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17114163





