Outcomes of the Health Insurance Card Scheme on Migrants’ Use of Health Services in Ranong Province, Thailand
Abstract
:1. Introduction
2. Methods
2.1. Study Site
2.2. Data Sources
2.3. Data Analysis and Variable Management
2.4. Ethical Consideration
3. Results
3.1. Inpatient Care
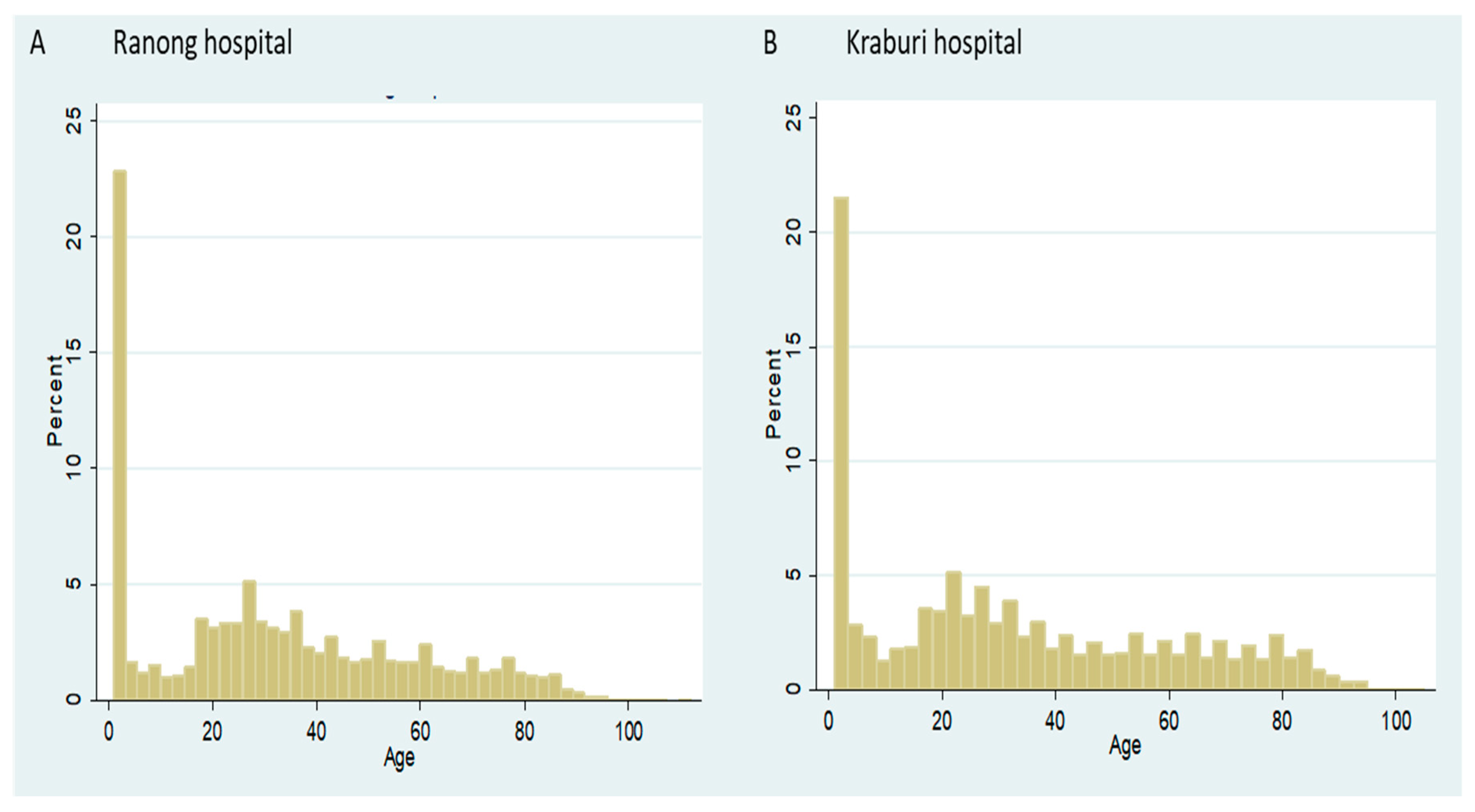
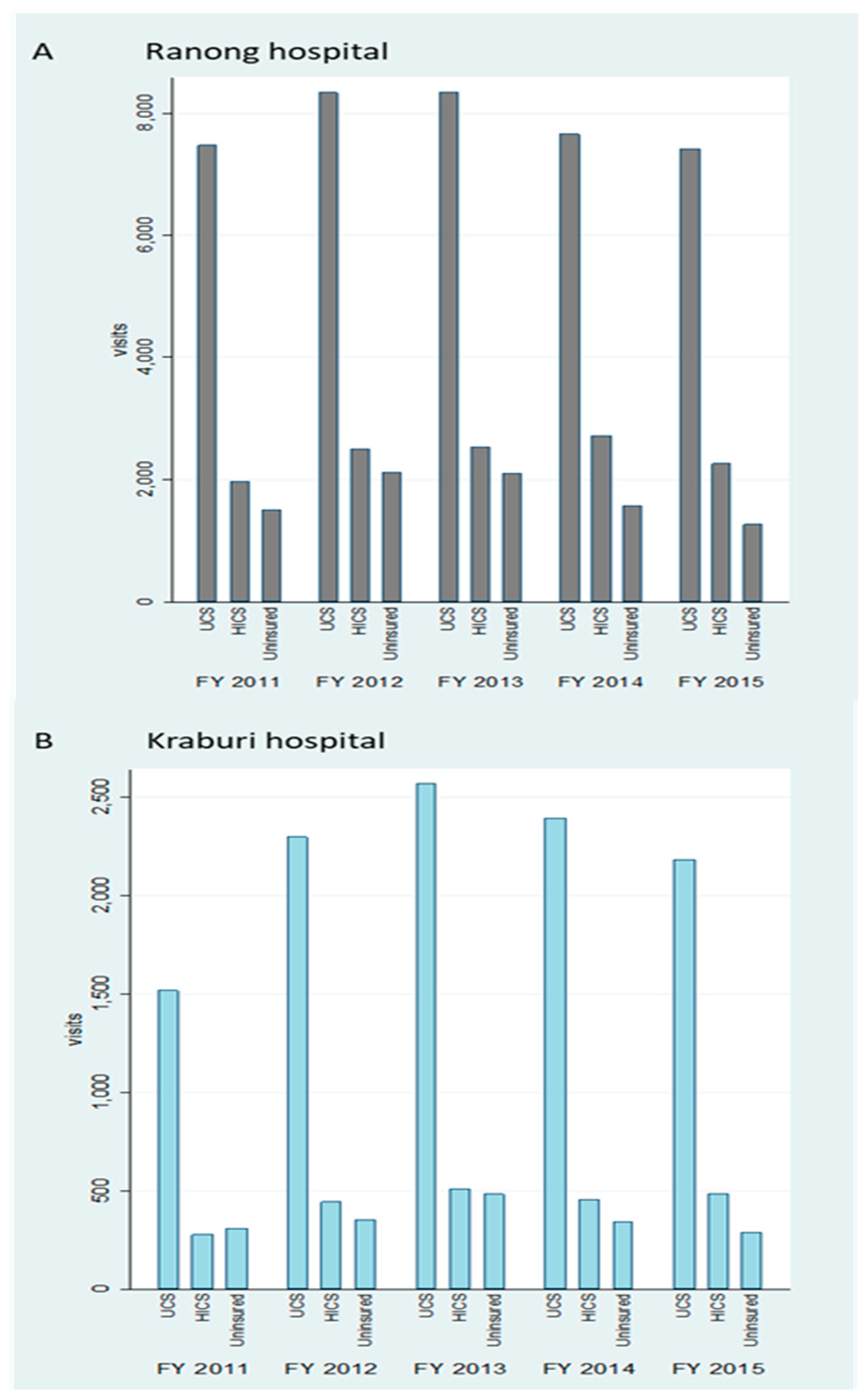
3.1.1. Overview of the Data
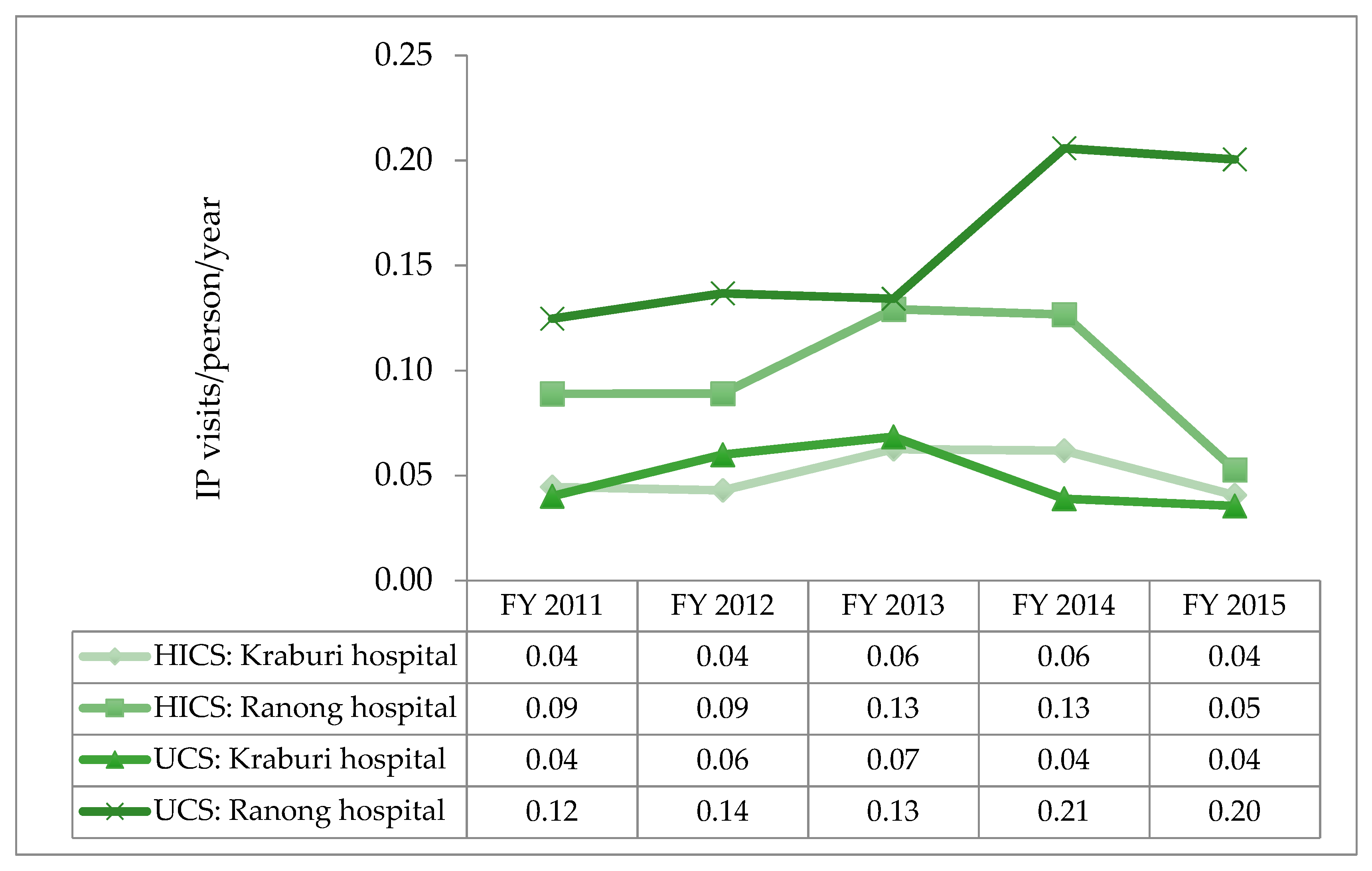
3.1.2. Utilisation Rate
3.1.3. Descriptive Statistics and Univariate Analysis
3.1.4. Multivariable Analysis
3.2. Outpatient Care
3.2.1. Overview of the Data
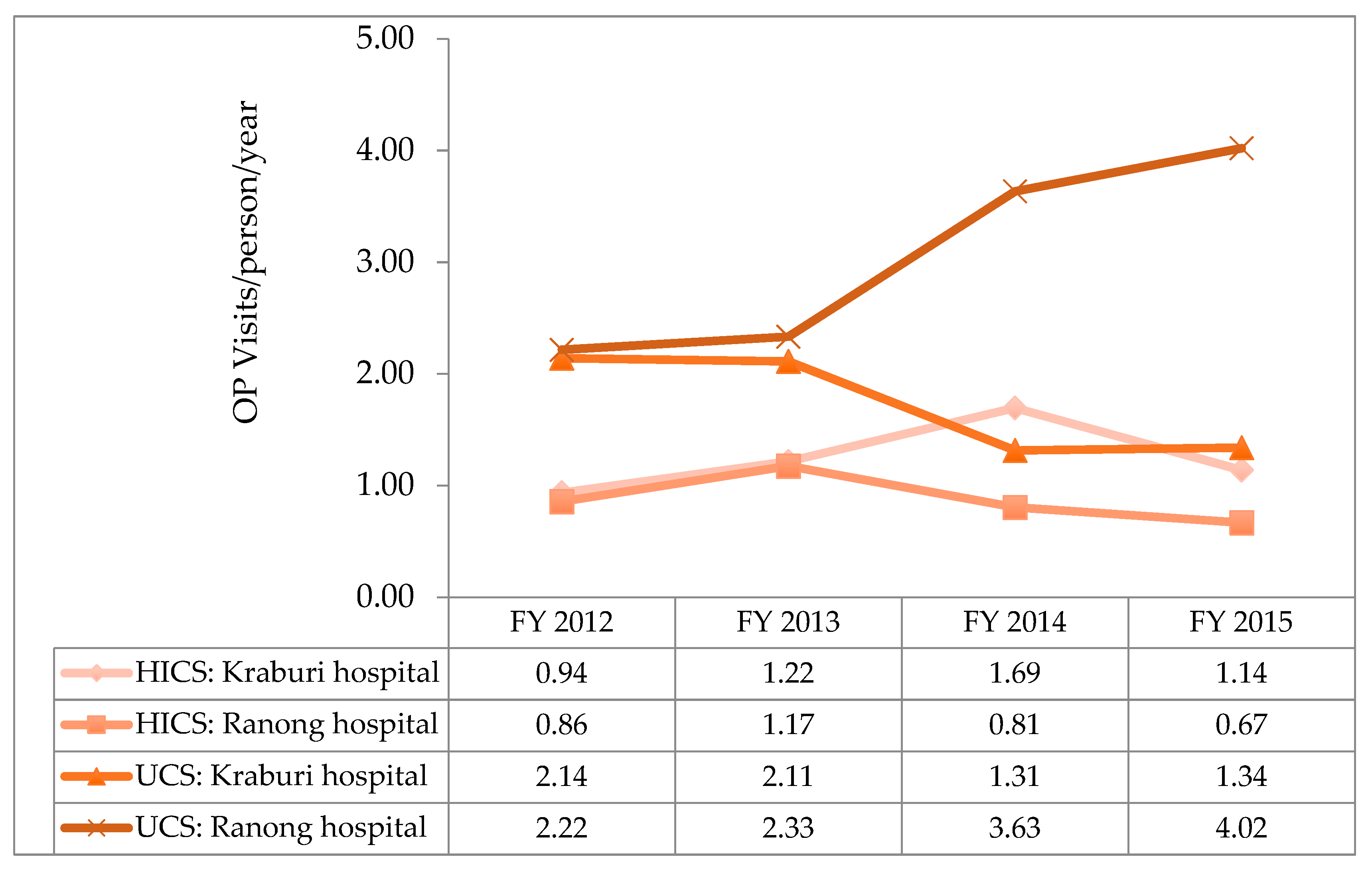
3.2.2. Utilisation Rate
3.2.3. Descriptive Statistics and Univariate Analysis
3.2.4. Multivariable Analysis
4. Discussion
4.1. Result Discussion
4.2. Methodological Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Worldometers. World Population: Dadax. 2019. Available online: https://www.worldometers.info/world-population/ (accessed on 12 December 2019).
- Koser, K.; Laczko, F. World Migration Report 2010: The Future of Migration: Building Capacities for Change; International Organization for Migration: Geneva, Switzerland, 2010; p. 115. [Google Scholar]
- World Health Organization. 60th Assembly. Resolution WHA60.26—Workers’ Health: Global Plan of Action; WHO: Geneva, Switzerland, 2007; p. 8. [Google Scholar]
- World Health Organization. 61st Assembly. Resolution WHA61.17—Health of Migrants; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Macpherson, D.W.; Gushulak, B.D.; Macdonald, L. Health and foreign policy: Influences of migration and population mobility. Bull. World Health Organ. 2007, 85, 200–206. [Google Scholar] [CrossRef]
- United Nations. Global Compact for Migration; United Nations: New York, NY, USA, 2018; Available online: https://refugeesmigrants.un.org/migration-compact (accessed on 13 January 2020).
- World Health Organization. 72nd Assembly. Resolution WHA70.15—Promoting the Health of Refugees and Migrants; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Tangcharoensathien, V.; Mills, A.; Palu, T. Accelerating health equity: The key role of universal health coverage in the Sustainable Development Goals. BMC Med. 2015, 13, 101. [Google Scholar] [CrossRef] [Green Version]
- Guinto, R.L.L.R.; Curran, U.Z.; Suphanchaimat, R.; Pocock, N.S. Universal health coverage in ‘One ASEAN’: Are migrants included? Glob. Health Action 2015, 8, 25749. [Google Scholar] [CrossRef] [PubMed]
- Office of Foreign Workers Administration. Statistics of Remaining Cross-Border Migrants Holding Work Permit in Thailand as of October 2018; Department of Employment, Ministry of Labour: Bangkok, Thailand, 2018. Available online: https://www.doe.go.th/prd/assets/upload/files/alien_th/98802fed607243cb1c1afe248b3d29eb.pdf (accessed on 9 August 2019).
- Suphanchaimat, R.; Putthasri, W.; Prakongsai, P.; Tangcharoensathien, V. Evolution and complexity of government policies to protect the health of undocumented/illegal migrants in Thailand—The unsolved challenges. Risk Manag. Healthc. Policy 2017, 10, 49–62. [Google Scholar] [CrossRef] [Green Version]
- National Council for Peace and Order. Temporary Measures to Problems of Migrant Workers and Human Trafficking (Order No.118/2557); Report No.: 118/2557; NCPO: Bangkok, Thailand, 2014. [Google Scholar]
- Health Insurance Group 2013. Health Card for Uninsured Foreigners and Health Card for Mother and Child. In Seminar on Measures and Protocols of Medical Examination, Insuring Migrants and Protecting Maternal and Child Health; 9–10 July 2013; Best Western Grand Howard Hotel; Office of the Permanent Secretary, Ministry of Public Health: Bangkok, Thailand, 2013. [Google Scholar]
- van Enter, B.J.D.; Lau, Y.-L.; Ling, C.L.; Watthanaworawit, W.; Sukthana, Y.; Lee, W.-C.; Nosten, F.; McGready, R. Seroprevalence of Toxoplasma gondii Infection in Refugee and Migrant Pregnant Women along the Thailand-Myanmar Border. Am. J. Trop. Med. Hyg. 2017, 97, 232–235. [Google Scholar] [CrossRef] [Green Version]
- Höglund, R.; Moussavi, Y.; Ruengweerayut, R.; Cheomung, A.; Äbelö, A.; Na-Bangchang, K. Population pharmacokinetics of a three-day chloroquine treatment in patients with Plasmodium vivax infection on the Thai-Myanmar border. Malar. J. 2016, 15, 129. [Google Scholar] [CrossRef] [Green Version]
- Rakprasit, J.; Nakamura, K.; Seino, K.; Morita, A. Healthcare use for communicable diseases among migrant workers in comparison with Thai workers. Ind. Health 2017, 55, 67–75. [Google Scholar] [CrossRef]
- Suphanchaimat, R.; Pudpong, N.; Prakongsai, P.; Putthasri, W.; Hanefeld, J.; Mills, A. The Devil Is in the Detail-Understanding Divergence between Intention and Implementation of Health Policy for Undocumented Migrants in Thailand. Int. J. Environ. Res. Public Health 2019, 16, 1016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Health Security Office (NHSO). National Health Security Act, B.E. 2545 (2002) in the Name of His Mejesty King Bhumibol. Available online: https://bit.ly/2MVAI63 (accessed on 9 February 2019).
- Mathauer, I.; Wittenbecher, F. Hospital payment systems based on diagnosis-related groups: Experiences in low- and middle-income countries. Bull. World Health Organ. 2013, 91, 746A–756A. [Google Scholar] [CrossRef] [PubMed]
- Srithamrongsawat, S.; Wisessang, R.; Ratjaroenkhajorn, S. Financing Healthcare for Migrants: A Case Study from Thailand; Health Insurance System Research Office/Health Systems Research Institute: Nonthaburi, Thailand, 2009. [Google Scholar]
- Shanmugasundaram, S.; O’Connor, M. Palliative care services for Indian migrants in australia: Experiences of the family of terminally ill patients. Indian J. Palliat. Care 2009, 15, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Suphanchaimat, R.; Pudpong, N.; Kunpeuk, W.; Julchoo, S.; Phaiyarom, M.; Sinam, P. Health of urban refugees and their healthcare access in Greater Bangkok, Thailand, 2019–2020: Policy analysis and unmet need survey. In Proceedings of the IHPP In-House Conference, Ministry of Public Health, Nonthaburi, Thailand, 16 March 2020. [Google Scholar]
- Thammatacharee, N.; Tisayaticom, K.; Suphanchaimat, R.; Limwattananon, S.; Putthasri, W.; Netsaengtip, R.; Tangcharoensathien, V. Prevalence and profiles of unmet healthcare need in Thailand. BMC Public Health 2012, 12, 923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suphanchaimat, R.; Kunpeuk, W.; Phaiyarom, M.; Nipaporn, S. The Effects of the Health Insurance Card Scheme on Out-of-Pocket Expenditure among Migrants in Ranong Province, Thailand. Risk Manag. Healthc. Policy 2019, 12, 317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomson, E.F.; Nuru-Jeter, A.; Richardson, D.; Raza, F.; Minkler, M. The Hispanic Paradox and older adults’ disabilities: Is there a healthy migrant effect? Int. J. Environ. Res. Public Health 2013, 10, 1786–1814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fennelly, K. The “healthy migrant” effect. Minn. Med. 2007, 90, 51–53. [Google Scholar] [PubMed]
- Hesketh, T.; Ye, X.J.; Li, L.; Wang, H.M. Health status and access to health care of migrant workers in China. Public Health Rep. 2008, 123, 189–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Division of Health Economics and Health Security. Notification of the Ministry of Public Health of Thailand Re: Health Examination and Health Insurance for Migrant Workers 2019. Available online: https://dhes.moph.go.th/?p=4869 (accessed on 28 October 2019).
- Sakworawich, A.P.A. NHSO Will Amend the UHC Act to be Taking for Granted by Immigrants from Neighboring Country. Available online: https://mgronline.com/daily/detail/9600000044667 (accessed on 22 February 2020).
- Thairath. National Health Security Office (NHSO), Free Services for All. Available online: https://www.thairath.co.th/content/936915 (accessed on 22 February 2020).
- Müllerschön, J.; Koschollek, C.; Santos-Hövener, C.; Kuehne, A.; Müller-Nordhorn, J.; Bremer, V. Impact of health insurance status among migrants from sub-Saharan Africa on access to health care and HIV testing in Germany: A participatory cross-sectional survey. BMC Int. Health Hum. Rights 2019, 19, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ledoux, C.; Pilot, E.; Diaz, E.; Krafft, T. Migrants’ access to healthcare services within the European Union: A content analysis of policy documents in Ireland, Portugal and Spain. Glob. Health 2018, 14, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Overcoming migrants’ barriers to health. Bull. World Health Organ. 2008, 86, 583–584. [CrossRef] [PubMed]



| Variable | Uninsured N = 10,382 | HICS N = 14,165 | UCS N = 50,175 | Test (p-Value) |
|---|---|---|---|---|
| Age—mean (SD) | 26.2 (18.7) | 30.9 (13.7) | 39.2 (26.5) | ANOVA (<0.001) |
| Age group—n (%) | Chi-square (<0.001) | |||
| • =<7 y | 2327 (22.4) | 841 (5.9) | 8302 (16.6) | |
| • 8–15 y | 578 (5.6) | 109 (0.8) | 3468 (6.9) | |
| • 16–30 y | 3700 (35.6) | 6830 (48.2) | 9651 (19.2) | |
| • 31–60 y | 3215 (31.0) | 5963 (42.1) | 15,597 (31.1) | |
| • >60 y | 560 (5.4) | 422 (3.0) | 13,156 (26.2) | |
| Female—n (%) | 5935 (57.7) | 9766 (68.9) | 26,596 (53.0) | Chi-square (<0.001) |
| Female (non-delivery)—n (%) | 4478 (51.7) | 6612 (60.1) | 24,466 (50.9) | Chi-square (<0.001) |
| Catastrophic illness—n (%) | 1411 (15.4) | 1722 (13.7) | 10,392 (23.6) | Chi-square (<0.001) |
| Proximity to a facility—n (%) | 6376 (63.4) | 11,051 (83.6) | 35,648 (71.1) | Chi-square (<0.001) |
| Facility level—n (% in a row) | Chi-square (<0.001) | |||
| • District hospital | 1782 (11.9) | 2172 (14.6) | 10,974 (73.5) | |
| • Provincial hospital | 8600 (14.4) | 11,993 (20.1) | 39,201 (65.5) |
| Variable | IRR | Std. Err. | p-Value | [95% Conf. | Interval] |
|---|---|---|---|---|---|
| Insurance (v uninsured) | |||||
| • HICS | 1.017 | 0.005 | 0.001 | 1.007 | 1.026 |
| • UCS | 1.087 | 0.005 | <0.001 | 1.077 | 1.096 |
| Ever had catastrophic illness (v never) | 1.057 | 0.012 | <0.001 | 1.034 | 1.080 |
| Insurance##Catastrophic illness | |||||
| • HICS##Ever had catastrophic illness | 1.193 | 0.028 | <0.001 | 1.140 | 1.249 |
| • UCS##Ever had catastrophic illness | 1.336 | 0.021 | <0.001 | 1.295 | 1.379 |
| Age group (v ≤ 7 yr) | |||||
| • 8–15 | 0.930 | 0.008 | <0.001 | 0.914 | 0.945 |
| • 16–30 | 0.965 | 0.006 | <0.001 | 0.952 | 0.977 |
| • 31–60 | 1.026 | 0.008 | 0.002 | 1.009 | 1.042 |
| • >60 | 1.118 | 0.014 | <0.001 | 1.092 | 1.145 |
| Female (v male) | 0.993 | 0.007 | 0.327 | 0.981 | 1.007 |
| Proximity (v non-proximity) | 1.106 | 0.007 | <0.001 | 1.092 | 1.119 |
| Post-OSS (v pre-OSS) | 0.982 | 0.007 | 0.006 | 0.969 | 0.995 |
| Insurance##OSS | |||||
| • HICS##Post-OSS | 1.001 | 0.011 | 0.961 | 0.980 | 1.022 |
| • UCS##Post-OSS | 0.988 | 0.011 | 0.268 | 0.968 | 1.009 |
| Provincial hospital (v district hospital) | 0.997 | 0.009 | 0.711 | 0.980 | 1.014 |
| Variable | Uninsured N = 99,119 | HICS N = 172,463 | UCS N = 908,215 | Test (p-Value) |
|---|---|---|---|---|
| Age—mean (SD) | 28.1 (17.9) | 37.1 (17.4) | 45.1 (23.9) | ANOVA (<0.001) |
| Age group—n (%) | Chi-square (<0.001) | |||
| • ≤7 y | 17,560 (17.7) | 8640 (5.0) | 99,480 (10.1) | |
| • 8–15 y | 4867 (4.9) | 2967 (1.7) | 62,978 (6.4) | |
| • 16–30 y | 35,155 (35.5) | 54,459 (31.6) | 116,252 (11.9) | |
| • 31–60 y | 36,865 (37.2) | 89,975 (52.2) | 405,526 (41.4) | |
| • >60 y | 4668 (4.7) | 16,421 (9.5) | 295,974 (30.2) | |
| Female—n (%) | 51,882 (52.4) | 104,343 (60.5) | 561,184 (57.6) | Chi-square (<0.001) |
| Disease status —n (%) | Chi-square (<0.001) | |||
| • ACSC | 8266 (8.3) | 33,313 (19.3) | 254,508 (26.0) | |
| • Z group | 58,901 (59.4) | 56,412 (32.7) | 267,653 (27.3) | |
| Proximity to a facility—n (%) | 57,020 (61.5) | 132,567 (80.6) | 791,155 (82.8) | Chi-square (<0.001) |
| Facility level—n (row %) | Chi-square (<0.001) | |||
| • Health centres | 5465 (5.1) | 7913 (7.4) | 93,973 (87.5) | |
| • District hospital | 40,856 (9.9) | 45,693 (11.1) | 324,362 (78.9) | |
| • Provincial hospital | 52,798 (7.2) | 118,857 (16.2) | 561,880 (76.6) |
| Variable | IRR | Std. Err. | p-Value | [95% Conf. | Interval] |
|---|---|---|---|---|---|
| Insurance (v uninsured) | |||||
| • HICS | 1.099 | 0.016 | <0.001 | 1.068 | 1.130 |
| • UCS | 1.336 | 0.014 | <0.001 | 1.309 | 1.364 |
| Ever had ACSC (v never) | 1.569 | 0.031 | <0.001 | 1.510 | 1.630 |
| Insurance##ACSC | |||||
| • HICS##Ever had ACSC | 1.118 | 0.031 | <0.001 | 1.060 | 1.179 |
| • UCS##Ever had ACSC | 1.285 | 0.027 | <0.001 | 1.234 | 1.339 |
| Ever had Z group (v never) | 1.389 | 0.018 | <0.001 | 1.355 | 1.423 |
| Insurance##Z group | |||||
| • HICS##Ever had Z group | 1.908 | 0.039 | <0.001 | 1.832 | 1.987 |
| • UCS##Ever had Z group | 1.606 | 0.024 | <0.001 | 1.560 | 1.653 |
| Age group (v ≤ 7 yr) | |||||
| • 8–15 | 0.953 | 0.008 | <0.001 | 0.936 | 0.969 |
| • 16–30 | 1.017 | 0.009 | 0.043 | 1.001 | 1.034 |
| • 31–60 | 1.471 | 0.013 | <0.001 | 1.445 | 1.497 |
| • >60 | 2.164 | 0.026 | <0.001 | 2.114 | 2.216 |
| Female (v male) | 1.011 | 0.007 | 0.140 | 0.996 | 1.026 |
| Proximity (v non-proximity) | 1.200 | 0.012 | <0.001 | 1.177 | 1.223 |
| Post-OSS (v pre-OSS) | 1.165 | 0.021 | <0.001 | 1.126 | 1.206 |
| Insurance##OSS | |||||
| • HICS##Post-OSS | 0.864 | 0.019 | <0.001 | 0.828 | 0.902 |
| • UCS##Post-OSS | 0.841 | 0.016 | <0.001 | 0.811 | 0.872 |
| Facility level (v health centre) | |||||
| • District hospital | 1.528 | 0.015 | <0.001 | 1.498 | 1.558 |
| • Provincial hospital | 1.455 | 0.014 | <0.001 | 1.428 | 1.483 |
| Alpha | 0.438 | 0.005 | - | 0.428 | 0.448 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Phaiyarom, M.; Pudpong, N.; Suphanchaimat, R.; Kunpeuk, W.; Julchoo, S.; Sinam, P. Outcomes of the Health Insurance Card Scheme on Migrants’ Use of Health Services in Ranong Province, Thailand. Int. J. Environ. Res. Public Health 2020, 17, 4431. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124431
Phaiyarom M, Pudpong N, Suphanchaimat R, Kunpeuk W, Julchoo S, Sinam P. Outcomes of the Health Insurance Card Scheme on Migrants’ Use of Health Services in Ranong Province, Thailand. International Journal of Environmental Research and Public Health. 2020; 17(12):4431. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124431
Chicago/Turabian StylePhaiyarom, Mathudara, Nareerut Pudpong, Rapeepong Suphanchaimat, Watinee Kunpeuk, Sataporn Julchoo, and Pigunkaew Sinam. 2020. "Outcomes of the Health Insurance Card Scheme on Migrants’ Use of Health Services in Ranong Province, Thailand" International Journal of Environmental Research and Public Health 17, no. 12: 4431. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124431





