Environments, Behaviors, and Inequalities: Reflecting on the Impacts of the Influenza and Coronavirus Pandemics in the United States
Abstract
:1. Introduction
Pandemics: Environments, Behaviors, and Inequalities
“An epidemic erodes social cohesiveness because the source of your danger is your fellow human beings, the source of your danger is your wife, children, parents and so on. So, if an epidemic goes on long enough, and the bodies start to pile up and nobody can dig graves fast enough to put the people into them, then morality does start to break down.” [1]Dr. Alfred CrosbyAmerica’s Forgotten Pandemic: The Influenza of 1918
2. The 1918 Influenza Pandemic in the United States
2.1. Influenza Pandemic: An Epidemiological Overview
2.2. Influenza Pandemic: Environments and Behaviors
2.3. Influenza Pandemic: Societal Norms of Inequality
3. The 2019 Coronavirus Pandemic in the United States
3.1. Coronavirus Pandemic: An Epidemiological Overview
3.2. Coronavirus Pandemic: Environments and Behaviors
3.3. Coronavirus Pandemic: Societal Norms of Inequality
4. Creating a Post-COVID-19 New Normal
Reflecting and Reimagining a New Post Pandemic Normal
“This pesky flu’s all over town! And white and black and rich and poor are all included in its tour.” [185]Author UnknownProse Poem on the 1918 Influenza Pandemic
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- PBS. American Experience—Influenza 1918: Dr. Alfred Crosby. Public Broadcasting Service. Available online: https://www.pbs.org/wgbh/americanexperience/features/influenza-author-interview-dr-alfred-crosby/ (accessed on 21 April 2020).
- Cowell, A. Photos from a Century of Epidemics—March 20, 2020. New York Times. Available online: https://www.nytimes.com/2020/03/20/world/europe/coronavirus-aids-spanish-flu-ebola-epidemics.html (accessed on 20 May 2020).
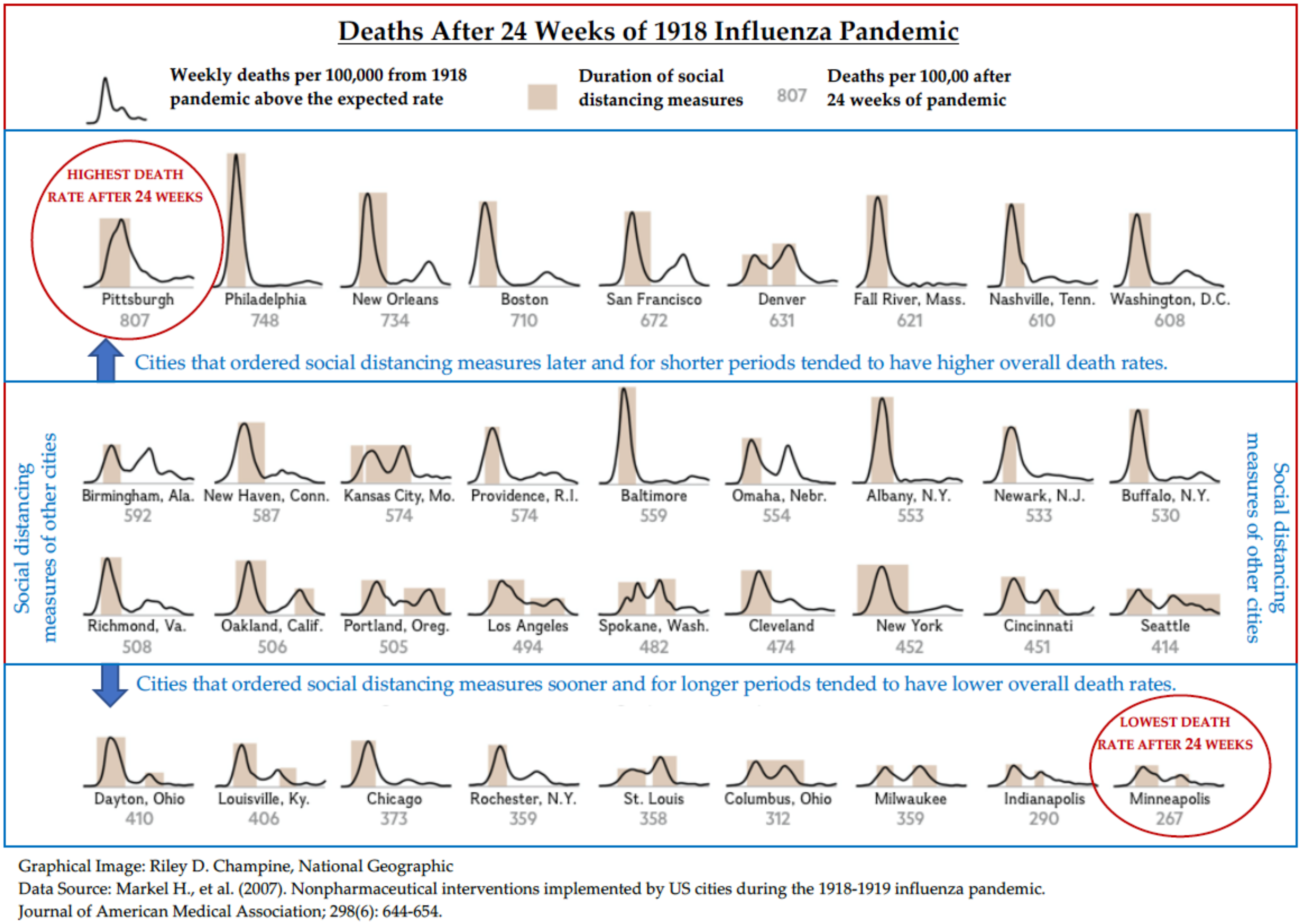
- Strochlic, N.; Champine, R.D. How Some Cities ‘Flattened the Curve’ During the 1918 Flu Pandemic—March 27, 2020. National Geographic. Available online: https://www.nationalgeographic.com/history/2020/03/how-cities-flattened-curve-1918-spanish-flu-pandemic-coronavirus/#close (accessed on 24 April 2020).
- Pinter-Wollman, N.; Jelic, A.; Wells, N.M. The impact of the built environment on health behaviours and disease transmission in social systems. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2018, 373. [Google Scholar] [CrossRef] [PubMed]
- Holtenius, J.; Gillman, A. The Spanish flu in Uppsala, clinical and epidemiological impact of the influenza pandemic 1918–1919 on a Swedish county. Infect. Ecol. Epidemiol. 2014, 4, 21528. [Google Scholar] [CrossRef]
- CDC. 1918 Pandemic (H1N1 virus). U.S. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html (accessed on 20 April 2020).
- Taubenberger, K.J.; Morens, D.M. 1918 Influenza: The mother of all pandemics. Emerg. Infect. Dis. 2006, 12, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Taubenberger, J.K. The origin and virulence of the 1918 “Spanish” influenza virus. Proc. Am. Philos. Soc. 2006, 150, 86–112. [Google Scholar] [PubMed]
- Viboud, C.; Eisenstein, J.; Reid, A.H.; Janczewski, T.A.; Morens, D.M.; Taubenberger, J.K. Age- and sex-specific mortality associated with the 1918–1919 influenza pandemic in Kentucky. J. Infect. Dis. 2013, 207, 721–729. [Google Scholar] [CrossRef]
- CDC. The Deadliest Flu: The Complete Story of the Discovery and Reconstruction of the 1918 Pandemic Virus. U.S. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/flu/pandemic-resources/reconstruction-1918-virus.html (accessed on 21 April 2020).
- Crosby, A.W. America’s Forgotten Pandemic: The Influenza of 1918, 2nd ed.; Cambridge University Press: Cambridge, UK, 2003. [Google Scholar]
- Barry, J.M. How the Horrific 1918 Flu Spread Across America—November 2017. Smithsonian Magazine. Available online: https://www.smithsonianmag.com/history/journal-plague-year-180965222/ (accessed on 20 April 2020).
- Martini, M.; Gazzaniga, V.; Bragazzi, N.L.; Barberis, I. The Spanish Influenza Pandemic: A lesson from history 100 years after 1918. J. Prev. Med. Hyg. 2019, 60, E64–E67. [Google Scholar]
- Humphreys, M. The influenza of 1918: Evolutionary perspectives in a historical context. Evol. Med. Public Health 2018, 2018, 219–229. [Google Scholar] [CrossRef]
- Jordan, E. Epidemic Influenza: A Survey; American Medical Association: Chicago, IL, USA, 1927; p. 355. [Google Scholar]
- CDC. 1918 Pandemic Influenza Historic Timeline. U.S. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/flu/pandemic-resources/1918-commemoration/pandemic-timeline-1918.htm (accessed on 20 April 2020).
- Vaughan, W.T. An Epidemiologic Study. Am. J. Hyg. 1921, 7, 65–78. [Google Scholar]
- Roos, D. Why the Second Wave of the 1918 Spanish Flu Was So Deadly. History Channel. Available online: https://www.history.com/news/spanish-flu-second-wave-resurgence (accessed on 20 April 2020).
- Erkoreka, A. The Spanish influenza pandemic in occidental Europe (1918–1920) and victim age. Influenza Other Respir. Viruses 2010, 4, 81–89. [Google Scholar] [CrossRef] [Green Version]
- Trilla, A.; Trilla, G.; Daer, C. The 1918 “Spanish flu” in Spain. Clin. Infect. Dis. 2008, 47, 668–673. [Google Scholar] [CrossRef] [Green Version]
- Nickol, E.M.; Kindrachuk, J. A year of terror and a century of reflection Perspectives on the great influenza pandemic of 1918–1919. BMC Infect. Dis. 2019, 19, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milsten, A. 1918 Influenza Pandemic: A United States Timeline. American College of Emergency Physicians. Available online: https://www.acep.org/how-we-serve/sections/disaster-medicine/news/april-2018/1918-influenza-pandemic-a-united-states-timeline/ (accessed on 20 April 2020).
- UMCHM. Influenza Encyclopedia: The American Influenza Epidemic of 1918–1919—Cambridge, Massachusetts. University of Michigan Center for the History of Medicine, Michigan Publishing. Available online: https://www.influenzaarchive.org/cities/city-cambridge.html# (accessed on 20 April 2020).
- Fighting Influenza with Transit Systems—November 1918. The American City. Available online: https://quod.lib.umich.edu/cgi/t/text/idx/f/flu/0600flu.0016.060/1/--fighting-influenza-with-transit-systems?rgn=full+text;view=image;q1=Place+--+New+York%2C+New+York (accessed on 8 June 2020).
- Sheidlower, N. How NYC Survived the 1918 Spanish Flu Pandemic. Untapped New York. Available online: https://untappedcities.com/2020/03/17/how-nyc-survived-the-1918-spanish-flu-pandemic (accessed on 20 June 2020).
- Poon, L. Remembering the ‘Mother of All Pandemics,’ 100 Years Later. City Lab. Available online: https://www.citylab.com/life/2018/09/spanish-flu-outbreak-1918-new-york-city-public-health-germ-city-museum/569947/ (accessed on 9 June 2020).
- Editorial: Americans Didn’t Like Wearing Masks in 1918—April 7, 2020. The Roanoke Times. Available online: https://www.roanoke.com/opinion/editorials/editorial-americans-didnt-like-wearing-masks-in-1918/article_ce966fa7–2655–53c7-ac37-c97719e985f3.html (accessed on 9 June 2020).
- Taylor, A. Photos of the 1918 Flu Pandemic—April 10, 2018. The Atlantic. Available online: https://www.theatlantic.com/photo/2018/04/photos-the-1918-flu-pandemic/557663/ (accessed on 9 June 2020).
- Poon, L. The Flu Epidemic of 1918. NYC Department of Records and Information Services. Available online: https://www.archives.nyc/blog/2018/3/1/the-flu-epidemic-of-1918 (accessed on 9 June 2020).
- Malewitz, J. The State’s 1918 Pandemic Shutdown Worked—May 1, 2020. Urban Milwaukee. Available online: https://urbanmilwaukee.com/2020/05/01/the-states-1918-pandemic-shutdown-worked/ (accessed on 9 June 2020).
- Marcus, E. Echoes of the Past: The 1918 Influenza Epidemic in Nevada—April 11, 2020. Reno Gazette Journal. Available online: https://www.rgj.com/story/news/2020/04/11/coronavirus-1918-reno-took-similar-quarantine-measures-stem-flu-epidemic/2975837001/ (accessed on 9 June 2020).
- Flynn, M. What Happens if Parades Aren’t Canceled During Pandemics? Philadelphia Found Out in 1918, with Disastrous Results—March 12, 2020. The Washington Post. Available online: https://www.washingtonpost.com/nation/2020/03/12/pandemic-parade-flu-coronavirus/ (accessed on 21 April 2020).
- History.com. Spanish Flu. A&E Television Networks. Available online: https://www.history.com/topics/world-war-i/1918-flu-pandemic (accessed on 21 April 2020).
- Roos, D. How U.S. Cities Tried to Halt the Spread of the 1918 Spanish Flu. History Channel. Available online: https://www.history.com/news/spanish-flu-pandemic-response-cities (accessed on 20 April 2020).
- Leer, T.V. Flu Epidemic Hit Utah Hard in 1918, 1919. Deseret News. Available online: https://www.deseret.com/1995/3/28/19166723/flu-epidemic-hit-utah-hard-in-1918–1919 (accessed on 21 April 2020).
- Klein, C. Construction Worker Finds 1918 Flu Pandemic Mass Grave. History.com. A&E Television Networks. Available online: https://www.history.com/news/construction-worker-finds-1918-flu-pandemic-mass-grave (accessed on 24 April 2020).
- Hobday, A.R.; Cason, J.W. The open-air treatment of pandemic influenza. Am. J. Public Health 2009, 99 (Suppl. 2), S236–S242. [Google Scholar] [CrossRef] [PubMed]
- Shipley, A.E. The Open-Air Treatment of the Wounded (The First Eastern General Hospital), 2nd ed.; Country Life Library: London, UK, 1915. [Google Scholar]
- St Clair Strange, F.G. The History of the Royal Sea Bathing Hospital Margate 1791–1991; Meresborough Books: Rainham, UK, 1991. [Google Scholar]
- Jones, E.R. Lettsom and the Royal Sea Bathing Hospital. Trans. Med. Soc. Lond. 1973, 89, 285–287. [Google Scholar]
- Anonymous. Influenza at the Camp Brooks Open Air Hospital. J. Am. Med. Assoc. 1918, 71, 1746–1747. [Google Scholar]
- Hobday, R.A. The open-air factor and infection control. J. Hosp. Infect. 2019, 103, e23–e24. [Google Scholar] [CrossRef] [PubMed]
- Hill, L. The Defence of the Respiratory Membrane against Influenza. Etc. Br. Med. J. 1919, 1, 238–240. [Google Scholar] [CrossRef] [Green Version]
- Editorial. Weapons against Influenza. Am. J. Public Health 1918, 8, 787–788.
- IOM. Modeling Community Containment for Pandemic Influenza: A Letter Report. Committee on Modeling Community Containment for Pandemic Influenza Institute of Medicine of the National Academies. Available online: https://0-doi-org.brum.beds.ac.uk/10.17226/11800 (accessed on 24 April 2020).
- WHOWG. Nonpharmaceutical Interventions for Pandemic Influenza, National and Community Measures. Emerg. Infect. Dis. 2006, 12, 88–94. [Google Scholar]
- Hatchett, R.J.; Mecher, C.E.; Lipsitch, M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc. Natl. Acad. Sci. USA 2007, 104, 7582–7587. [Google Scholar] [CrossRef] [Green Version]
- Markel, H.; Lipman, H.B.; Navarro, J.A.; Sloan, A.; Michalsen, J.R.; Stern, A.M.; Cetron, M.S. Nonpharmaceutical interventions implemented by US cities during the 1918–1919 influenza pandemic. JAMA 2007, 298, 644–654. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J. An Epidemic’s Strawman: Wilmer Krusen, Philadelphia’s 1918–1919 Influenza Epidemic, and Historical Memory. Pa. Mag. Hist. Biogr. 2020, 144, 61–88. [Google Scholar] [CrossRef]
- Bootsma, M.C.; Ferguson, N.M. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc. Natl. Acad. Sci. USA 2007, 104, 7588–7593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wirth, T. Urban Neglect: The Environment, Public Health, and Influenza in Philadelphia, 1915–1919. Pa. Hist. J. Mid Atl. Stud. 2006, 73, 316–342. [Google Scholar]
- Hu, M.; Roberts, J.D. Connections and Divergence between Public Health and Built Environment—A Scoping Review. Urban Sci. 2020, 4, 12. [Google Scholar] [CrossRef] [Green Version]
- Melosi, M.V. The Sanitary City: Urban Infrastructure in America from Colonial Times to the Present; The Johns Hopkins University Press: Baltimore, MD, USA, 1999. [Google Scholar]
- Stern, M.A.; Cetron, M.S.; Markel, H. The 1918–1919 influenza pandemic in the United States: Lessons learned and challenges exposed. Public Health Rep. 2010, 125 (Suppl. 3), 6–8. [Google Scholar] [CrossRef] [Green Version]
- Snowden, F.M. Epidemics and Society: From the Black Death to the Present; Yale University Press: New Haven, CT, USA, 2019. [Google Scholar]
- Gamble, V.N. ”There wasn’t a lot of comforts in those days:” African Americans, public health, and the 1918 influenza epidemic. Public Health Rep. 2010, 125 (Suppl. 3), 114–122. [Google Scholar] [CrossRef] [Green Version]
- Du Bois, W.E.B. The Health and Physique of the Negro American; Atlanta University Press: Atlanta, GA, USA, 1906. [Google Scholar]
- U.S. Census. Urban and Rural Areas. U.S. Census Bureau. Available online: https://www.census.gov/history/www/programs/geography/urban_and_rural_areas.html (accessed on 25 April 2020).
- Garrett, T.A. Pandemic Economics: The 1918 Influenza and Its Modern-Day Implications. Federal Reserve Bank of St. Louis Review. Federal Reserve Bank of St. Louis. Available online: https://files.stlouisfed.org/files/htdocs/publications/review/08/03/Garrett.pdf (accessed on 25 April 2020).
- U.S. Census. We the America: Blacks. U.S. Census Bureau. Available online: https://www.census.gov/prod/cen1990/wepeople/we-1.pdf (accessed on 25 April 2020).
- U.S. Census. The Great Migration, 1910 to 1970. U.S. Census Bureau. Available online: https://www.census.gov/dataviz/visualizations/020/ (accessed on 25 April 2020).
- Hobbs, F.; Stoops, N. Demographic Trends in the 20th Century. U.S. Census Bureau, 2002. Available online: https://www.census.gov/prod/2002pubs/censr-4.pdf (accessed on 25 April 2020).
- Okland, H.; Mamelund, S.E. Race and 1918 Influenza Pandemic in the United States: A Review of the Literature. Int. J. Environ. Res. Public Health 2019, 16, 2487. [Google Scholar]
- Roberts, S.K. Infectious Fear: Politics, Disease, and the Health Effects of Segregation; University of North Carolina Press: Chapel Hill, NC, USA, 2009. [Google Scholar]
- McDonald, S.N. In 1918 and 2020, Race Colors America’s Response to Epidemics: A Look at How Jim Crow Affected the Treatment of African Americans Fighting the Spanish Flu. The Undefeated. Entertainment and Sports Programming Network. Available online: https://theundefeated.com/features/in-1918-and-2020-race-colors-americas-response-to-epidemics/ (accessed on 26 April 2020).
- Schlabach, E. The Influenza Epidemic and Jim Crow Public Health Policies and Practices in Chicago, 1917–1921. J. Afr. Am. Hist. 2019, 104, 31–58. [Google Scholar] [CrossRef]
- Starr, I. Influenza in 1918: Recollections of the epidemic in Philadelphia. Ann. Intern. Med. 1976, 85, 516–518. [Google Scholar] [CrossRef]
- Total of 1,000 Patients Expected at Hospital. Richmond Times Dispatch, 25 October 1918.
- Influenza and Pneumonia Claims Many Victims. Baltimore Afro-American, 18 October 1918; 1.
- Washington, S.H. Packing Them In: An Archaeology of Environmental Racism in Chicago, 1865–1954; Lexington Books: Lanham, MD, USA, 2004. [Google Scholar]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Ghinai, I.; McPherson, T.D.; Hunter, J.C.; Kirking, H.L.; Christiansen, D.; Joshi, K.; Rubin, R.; Morales-Estrada, S.; Black, S.R.; Pacilli, M.; et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet 2020, 395, 1137–1144. [Google Scholar] [CrossRef]
- Phan, T.L.; Nguyen, T.V.; Luong, Q.C.; Nguyen, T.V.; Nguyen, H.T.; Le, H.Q.; Nguyen, T.T.; Cao, T.M.; Pham, Q.D. Importation and Human-to-Human Transmission of a Novel Coronavirus in Vietnam. N. Engl. J. Med. 2020, 382, 872–874. [Google Scholar] [CrossRef] [Green Version]
- Holshue, L.M.; DeBolt, C.; Lindquist, S.; Lofy, K.H.; Wiesman, J.; Bruce, H.; Spitters, C.; Ericson, K.; Wilkerson, S.; Tural, A.; et al. Washington State -nCo. First Case of 2019 Novel Coronavirus in the United States. N. Engl. J. Med. 2020, 382, 929–936. [Google Scholar] [PubMed]
- CDC. CDC Confirms Person-to-Person Spread of New Coronavirus in the United States. U.S. Department of Health and Human Service, Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/media/releases/2020/p0130-coronavirus-spread.html (accessed on 5 April 2020).
- Worldometers. Coronavirus Worldwide Graphs. Worldometers. Available online: https://www.worldometers.info/coronavirus/worldwide-graphs/#total-cases (accessed on 27 April 2020).
- NYT. Coronavirus in the U.S.: Latest Map and Case Count—June 21, 2020. New York Times. Available online: https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html (accessed on 21 June 2020).
- CDC. Public Health Responses to COVID-19 Outbreaks on Cruise Ships—Worldwide, February–March 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 347–352. [Google Scholar] [CrossRef] [PubMed]
- CDC. Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19)—United States, February 12–March 16, 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 343–346. [Google Scholar] [CrossRef] [PubMed]
- CDC. Coronavirus Disease 2019 in Children—United States, February 12–April 2, 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 422–426. [Google Scholar] [CrossRef]
- CDC. COVID-19 in a Long-Term Care Facility—King County, Washington, February 27–March 9, 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 339–342. [Google Scholar] [CrossRef] [Green Version]
- CDC. Geographic Differences in COVID-19 Cases, Deaths, and Incidence—United States, February 12–April 7, 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 465–471. [Google Scholar]
- LDH. Coronavirus (COVID-19). Louisiana Department of Health. Available online: http://ldh.la.gov/Coronavirus/ (accessed on 23 April 2020).
- Chandler, C. Mayor Perkins Identifies 5 Hot Spots in Shreveport for Coronavirus—April 2, 2020. KTBS. Available online: https://www.ktbs.com/news/mayor-perkins-identifies-5-hot-spots-in-shreveport-for-coronavirus/article_368892a2–7546–11ea-9a73–7f2a04d71133.html (accessed on 16 May 2020).
- CDC. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019—COVID-NET, 14 States, March 1–30, 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 458–464. [Google Scholar]
- Chotiner, I. How Pandemics Change History. An Interview with Dr. Frank M. Snowden—March 3, 2020. The New Yorker. Available online: https://www.newyorker.com/news/q-and-a/how-pandemics-change-history (accessed on 28 April 2020).
- D’Angelo, M. Tactics for Minimizing COVID-19 Transmission in the Built Environment. Journal of the American Institute of Architects. Architect Magazine. Available online: https://www.architectmagazine.com/practice/tactics-for-minimizing-covid-19-transmission-in-the-built-environment_o (accessed on 30 April 2020).
- Barlow, J. UO’s Indoor Research Center Takes Aim at COVID-19 Risks. University of Oregon. Available online: https://around.uoregon.edu/content/uos-indoor-research-center-takes-aim-covid-19-risks (accessed on 30 April 2020).
- CDC. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019—United States, February 12–March 28, 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 382–386. [Google Scholar] [CrossRef] [PubMed]
- NYT. CDC Gives New Guidelines, New York to Close Restaurants and Schools and Italian Deaths Rise—March 15, 2020. New York Times. Available online: https://www.nytimes.com/2020/03/15/world/coronavirus-live.html (accessed on 5 April 2020).
- Lee, A. These States Have Implemented Stay-at-Home Orders. Here’s What That Means for You—April 7, 2020. CNN. Available online: https://www.cnn.com/2020/03/23/us/coronavirus-which-states-stay-at-home-order-trnd/index.html (accessed on 30 April 2020).
- Gershman, J. A Guide to State Coronavirus Reopenings and Lockdowns—May 20, 2020. The Wall Street Journal. Available online: https://www.wsj.com/articles/a-state-by-state-guide-to-coronavirus-lockdowns-11584749351?mod=theme_coronavirus-ribbon (accessed on 30 April 2020).
- Tyko, K. Starbucks Closing Some Locations and Moving to a ‘To Go’ Model at Other Stores Due to Coronavirus—March 15, 2020. USA Today. Available online: https://www.usatoday.com/story/money/food/2020/03/15/starbucks-coronavirus-changes-mobile-orders-drive-thru-closing-locations/5055192002/ (accessed on 30 April 2020).
- Target, Lowe’s, Home Depot to Limit the Number of Customers Inside to Combat Spread of COVID-19—April 4, 2020. WDRB.com. Available online: https://www.wdrb.com/news/target-lowes-home-depot-to-limit-the-number-of-customers-inside-to-combat-spread-of/article_ac5e4948–761a-11ea-b0ce-47befba7acaa.html (accessed on 30 April 2020).
- Tyko, K. Dollar General Cuts Store Hours, Dedicates Hour to Senior Shoppers During Coronavirus Pandemic—March 16, 2020. USA Today. Available online: https://www.usatoday.com/story/money/2020/03/16/coronavirus-seniors-dollar-general-dedicates-hour-senior-shoppers/5065594002/ (accessed on 30 April 2020).
- Giacobbe, A. How the COVID-19 Pandemic Will Change the Built Environment. Architectural Digest. Available online: https://www.architecturaldigest.com/story/covid-19-design (accessed on 30 April 2020).
- MTA. MTA Essential Service During the Coronavirus Pandemic. Metropolitan Transportation Authority. Available online: https://new.mta.info/precautions-against-coronavirus (accessed on 13 April 2020).
- NORTA. Coronavirus (COVID-19) Service Reduction. New Orleans Regional Transit Authority. Available online: https://www.norta.com/About/Coronavirus-Response (accessed on 13 April 2020).
- CTA. CTA: Coronavirus Info (COVID-19). Chicago Transit Authority. Available online: https://www.transitchicago.com/coronavirus/ (accessed on 13 April 2020).
- Levenson, M. 11 Days After Fuming About a Coughing Passenger, a Bus Driver Died From the Coronavirus—April 4, 2020. New York Times. Available online: https://www.nytimes.com/2020/04/04/us/detroit-bus-driver-coronavirus.html (accessed on 9 June 2020).
- Caswell, M. Coronavirus: Amtrak to reduce Northeast Corridor services by 60 per cent—March 16, 2020. Business Traveller. Available online: https://www.businesstraveller.com/business-travel/2020/03/16/coronavirus-amtrak-to-reduce-northeast-corridor-services-by-60-per-cent/ (accessed on 9 June 2020).
- Clabaugh, J. Amtrak Now Requires Passengers to Wear Face Masks–May 7, 2020. WTOP News. Available online: https://wtop.com/business-finance/2020/05/amtrak-now-requires-passengers-to-wear-face-masks/ (accessed on 9 June 2020).
- DHS. Fact Sheet: DHS Notice of Arrival Restrictions on China, Iran and Certain Countries of Europe. Department of Homeland Security. Available online: https://www.dhs.gov/news/2020/03/17/fact-sheet-dhs-notice-arrival-restrictions-china-iran-and-certain-countries-europe (accessed on 9 June 2020).
- DOS. Global Level 4 Health Advisory—Do Not Travel. U.S. Department of State. Available online: https://travel.state.gov/content/travel/en/traveladvisories/ea/travel-advisory-alert-global-level-4-health-advisory-issue.html (accessed on 9 June 2020).
- Bolashikov, D.Z.; Melikov, A.K. Methods for air cleaning and protection of building occupants from airborne pathogens. Build. Environ. 2009, 44, 1378–1385. [Google Scholar] [CrossRef] [PubMed]
- Neal, T. COVID-19 and the Built Environment. Colin, Biggers and Paisley Lawyers. Available online: https://www.cbp.com.au/insights/insights/2020/march/covid-19-and-the-built-environment (accessed on 30 April 2020).
- LaForce, F.M. Airborne infections and modern building technology. In Proceedings of the 3rd International Conference on Indoor Air Quality and Climate, Stockholm, Sweden, 20–24 August 1984; pp. 109–127. [Google Scholar]
- Kowalski, J.W.; Bahnfleth, W.P. Immune-Building Technology, and Bioterrorism Defense. HPAC Eng. 2003, 75, 57–62. [Google Scholar]
- Li, Y.; Leung, G.M.; Tang, J.W.; Yang, X.; Chao, C.Y.; Lin, J.Z.; Lu, J.W.; Nielsen, P.V.; Niu, J.; Qian, H.; et al. Role of ventilation in airborne transmission of infectious agents in the built environment—a multidisciplinary systematic review. Indoor Air 2007, 17, 2–18. [Google Scholar] [CrossRef] [PubMed]
- ASHRAE. Method of Testing General Ventilation Air-Cleaning Devices for Removal Efficiency by Particle Size; ANSI/ASHRAE Standard 52.2–1999; American Society of Heating, Refrigerating and Air-Conditioning Engineers: Atlanta, GA, USA, 1999. [Google Scholar]
- ISO. Clean Rooms and Associated Controlled Environment—Part 1: Classification of Air Cleanliness, 1st ed.; ISO 14644–1; International Organization for Standardization: Geneva, Switzerland, 1999. [Google Scholar]
- Kowalski, J.W.; Bahnfleth, W.P. Airborne Respiratory Diseases and Mechanical Systems for Control of Microbes. HPAC Eng. 1998, 70, 34–48. [Google Scholar]
- Luckiesh, M. Applications of Germicidal, Erythemal and Infrared Energy; D. Van Nostrand Company: New York, NY, USA, 1946. [Google Scholar]
- Ko, G.; First, M.W.; Burge, H.A. The characterization of upper-room ultraviolet germicidal irradiation in inactivating airborne microorganisms. Environ. Health. Perspect. 2002, 110, 95–101. [Google Scholar]
- Xu, P.; Kujundzic, E.; Peccia, J.; Schafer, M.P.; Moss, G.; Hernandez, M.; Miller, S.L. Impact of environmental factors on efficacy of upper-room air ultraviolet germicidal irradiation for inactivating airborne mycobacteria. Environ. Sci. Technol. 2005, 39, 9656–9664. [Google Scholar] [CrossRef]
- Jensen, M.M. Inactivation of Airborne Viruses by Ultraviolet Irradiation. Appl. Microbiol. 1964, 12, 418–420. [Google Scholar] [CrossRef] [Green Version]
- Scott, D. Coronavirus is Exposing All of the Weaknesses in the US Health System—March 16, 2020. Vox. Available online: https://www.vox.com/policy-and-politics/2020/3/16/21173766/coronavirus-covid-19-us-cases-health-care-system (accessed on 30 April 2020).
- AHA. Fast Facts on U.S. Hospitals, 2020. American Hospital Association. Available online: https://www.aha.org/statistics/fast-facts-us-hospitals (accessed on 30 April 2020).
- Ellison, A. Cash-Strapped Rural Hospitals Brace for Surge of COVID-19 Patients. Becker’s Hospital Review. Available online: https://www.beckershospitalreview.com/finance/cash-strapped-rural-hospitals-brace-for-surge-of-covid-19-patients.html (accessed on 30 April 2020).
- Post, N.M. Health Care Designers Educate, Advise, Warn During COVID-19 Crisis. Engineering News Record. Available online: https://www.enr.com/articles/48999-health-care-designers-educate-advise-warn-during-covid-19-crisis (accessed on 16 May 2020).
- CDC. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. U.S. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Finfection-control%2Fcontrol-recommendations.html#collection (accessed on 20 April 2020).
- Stevens, P. Studio Prototype Designs Prefabricated ‘Vital House’ to Combat COVID-19. Designboom. Available online: https://www.designboom.com/architecture/studio-prototype-vital-house-virus-hotel-covid-19–03–25–2020/ (accessed on 16 May 2020).
- Loehrke, J.; Petras, G. Coronavirus Hospitals in the Field: How the Army Corps of Engineers Fights COVID-19 with Tents—April 17, 2020. USA Today. Available online: https://www.usatoday.com/in-depth/news/2020/04/16/coronavirus-covid-19-field-hospital-army-corps-of-engineers-samaritans-purse-central-park-tcf-center/5119808002/ (accessed on 30 April 2020).
- Black, J. Duke Health Triage Tents Provide COVID-19 Care—April 8, 2020. Duke Today. Available online: https://today.duke.edu/2020/04/duke-health-triage-tents-provide-covid-19-care (accessed on 30 April 2020).
- Brown, E.N. 3 Things Hospitals Can Do Right Now to Prepare for COVID-19. Fast Company. Available online: https://www.fastcompany.com/90480139/3-things-hospitals-can-do-right-now-to-prepare-for-covid-19 (accessed on 16 May 2020).
- McMichael, M.T.; Currie, D.W.; Clark, S.; Pogosjans, S.; Kay, M.; Schwartz, N.G.; Lewis, J.; Baer, A.; Kawakami, V.; Lukoff, M.D.; et al. Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. N. Engl. J. Med. 2020, 382. [Google Scholar] [CrossRef]
- CDC. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility—King County, Washington, March 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 377–381. [Google Scholar] [CrossRef] [Green Version]
- Spolidoro, B. How Architecture Can Defend Us from Germs, Bacteria, and Viruses Like COVID-19. Fisher Architecture. Available online: https://fisherarch.com/healthy-buildings-well/ (accessed on 16 May 2020).
- Kearney, A.; Muñana, C. Taking Stock of Essential Workers. Kaiser Family Foundation. Available online: https://www.kff.org/coronavirus-policy-watch/taking-stock-of-essential-workers/ (accessed on 14 May 2020).
- Cooper, D. Balancing Paychecks and Public Assistance: How Higher Wages Would Strengthen What Government Can Do. Economic Policy Institute. Available online: https://www.epi.org/publication/wages-and-transfers/ (accessed on 14 May 2020).
- Lowrey, A. Don’t Blame Econ 101 for the Plight of Essential Workers—May 13, 2020. The Atlantic. Available online: https://www.theatlantic.com/ideas/archive/2020/05/why-are-americas-most-essential-workers-so-poorly-treated/611575/ (accessed on 14 May 2020).
- Watkins, S. Kroger Ranks Among Top Employers of Workers on Food Stamps—September 12, 2018. Biz Journals. Available online: https://www.bizjournals.com/cincinnati/news/2018/09/12/kroger-ranks-among-top-employers-of-workers-on.html (accessed on 14 May 2020).
- CDC. COVID-19 Among Workers in Meat and Poultry Processing Facilities—19 States, April 2020. Centers for Disease Control and Prevention. Morb. Mortal. Wkly. Rep. 2020, 69, 557–561. [Google Scholar]
- Undetected: Lack of Access to Testing Among Minorities Keeps Virus Alive—May 10, 2020. Tampa Bay Times. Available online: https://www.tampabay.com/news/health/2020/05/10/undetected-lack-of-access-to-testing-among-minorities-keeps-virus-alive/ (accessed on 10 June 2020).
- Farmer, B. Long-Standing Racial And Income Disparities Seen Creeping Into COVID-19 Care. Kaiser Health News. Available online: https://khn.org/news/covid-19-treatment-racial-income-health-disparities/ (accessed on 10 June 2020).
- Livingston, D. Coronavirus Testing Is Lacking in Black Ohio Communities—May 11, 2020. Akron Beacon Journal. Available online: https://www.governing.com/now/Coronavirus-Testing-Is-Lacking-in-Black-Ohio-Communities.html (accessed on 10 June 2020).
- Coronavirus in Texas: Testing Sites Lacking in Black and Hispanic Neighborhoods, NPR finds—May 27, 2020. Eagle Pass Business Journal. Available online: https://www.epbusinessjournal.com/2020/05/coronavirus-in-texas-testing-sites-lacking-in-black-and-hispanic-neighborhoods-npr-finds/ (accessed on 10 June 2020).
- Mtshali, M. How Medical Bias Against Black People is Shaping Covid-19 Treatment and Care. Vox. Available online: https://www.vox.com/2020/6/2/21277987/coronavirus-in-black-people-covid-19-testing-treatment-medical-racism (accessed on 10 June 2020).
- Frye, J. On the Frontlines at Work and at Home: The Disproportionate Economic Effects of the Coronavirus Pandemic on Women of Color. Center for American Progress. Available online: https://www.americanprogress.org/issues/women/reports/2020/04/23/483846/frontlines-work-home/ (accessed on 15 May 2020).
- Quick Facts About the Gender Wage Gap. Center for American Progress. Available online: https://www.americanprogress.org/issues/women/reports/2020/03/24/482141/quick-facts-gender-wage-gap/ (accessed on 15 May 2020).
- IPUMS. Center for American Progress Calculations are Based on an Analysis of Employed Workers by Sex, Race, Ethnicity, and Occupation Using Data From Steven Ruggles and Others, “Integrated Public Use Microdata Series U.S. Census Data for Social, Economic, and Health Research, 2014–2018 American Community Survey: 5-Year Estimates: Version 10.0” (Minneapolis: Minnesota Population Center, 2020). IPUMS USA. University of Minnesota. Available online: https://usa.ipums.org/usa/ (accessed on 15 May 2020).
- DOL. U.S. Bureau of Labor Statistics, “News Release: Unemployment Insurance Weekly Claims”. U.S. Department of Labor. Available online: https://www.dol.gov/ui/data.pdf (accessed on 15 May 2020).
- Elflein, J. Death Rates from Coronavirus (COVID-19) in the United States as of May 13, 2020, by State. Statista. Available online: https://0-www-statista-com.brum.beds.ac.uk/statistics/1109011/coronavirus-covid19-death-rates-us-by-state/ (accessed on 16 May 2020).
- Tehrani, O.S.; Wu, S.J.; Roberts, J.D. The Color of Health: Residential Segregation, Light Rail Transit Developments, and Gentrification in the United States. Int. J. Environ. Res. Public Health 2019, 16, 3683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Census Reporter. Louisiana. U.S. Census Bureau. Available online: https://censusreporter.org/profiles/04000US22-louisiana/ (accessed on 13 April 2020).
- Zanolli, L. Data from US South Shows African Americans Hit Hardest by Covid-19—April 8, 2020. The Guardian. Available online: https://www.theguardian.com/world/2020/apr/08/black-americans-coronavirus-us-south-data (accessed on 16 May 2020).
- APM. The Color of Coronavirus: COVID-19 Deaths by Rave and Ethnicity in the U.S. APM Research Lab. Available online: https://www.apmresearchlab.org/covid/deaths-by-race (accessed on 21 June 2020).
- Moore, N. In Chicago, COVID-19 Is Hitting The Black Community Hard—April 6, 2020. NPR. Available online: https://www.npr.org/sections/coronavirus-live-updates/2020/04/06/828303894/in-chicago-covid-19-is-hitting-the-black-community-hard (accessed on 7 April 2020).
- Williams, J.P. Black People Are Disproportionately Getting and Dying From COVID-19—April 7, 2020. U.S. News. Available online: https://www.usnews.com/news/healthiest-communities/articles/2020–04–07/black-people-are-disproportionately-dying-from-coronavirus (accessed on 7 April 2020).
- CDC. COVID-19 in Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html (accessed on 16 May 2020).
- Swalec, A. Black DC Residents Make Up Most Coronavirus Deaths Thus Far—April 8, 2020. NBC Washington. Available online: https://www.nbcwashington.com/news/local/black-dc-residents-make-up-most-coronavirus-deaths-thus-far/2267854/ (accessed on 16 May 2020).
- DHHS. Obesity and African Americans. U.S. Department of Health and Human Services. Office of Minority Health. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=25 (accessed on 7 April 2020).
- DHHS. Diabetes and African Americans. U.S. Department of Health and Human Services. Office of Minority Health. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=18 (accessed on 7 April 2020).
- DHHS. Asthma and African Americans. U.S. Department of Health and Human Services. Office of Minority Health. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=15 (accessed on 7 April 2020).
- Nicholas, B.S.; Kalantar-Zadeh, K.; Norris, K.C. Racial disparities in kidney disease outcomes. Semin. Nephrol. 2013, 33, 409–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Covert, B. Race Best Predicts Whether You Live Near Pollution Environmental Racism Extends far Beyond Flint—May 15, 2020. The Nation. Available online: https://www.thenation.com/article/politics/trump-gop-coronavirus-fascism/ (accessed on 16 May 2020).
- Thibodeaux, J. City racial composition as a predictor of African American food deserts. Urban Stud. 2016, 53, 2238–2252. [Google Scholar] [CrossRef]
- Williams, D.R.; Collins, C. Racial Residential Segregation a Fundamental Cause of Racial Disparities in Health. Public Health Rep. 2001, 116, 404–416. [Google Scholar] [CrossRef]
- Allen, D.J. Lost in the Transit Desert: Race, Transit Access, and Suburban Form; Routledge: New York, NY, USA, 2017. [Google Scholar]
- Austin, A. African Americans are Still Concentrated in Neighborhoods with High Poverty and Still Lack Full Access to Decent Housing. Economic Policy Institute. Available online: https://www.epi.org/publication/african-americans-concentrated-neighborhoods/ (accessed on 16 May 2020).
- Livingston, G. About One-Third of U.S. Children are Living with an Unmarried Parent. Pew Research Center. Available online: https://www.pewresearch.org/fact-tank/2018/04/27/about-one-third-of-u-s-children-are-living-with-an-unmarried-parent/ (accessed on 16 May 2020).
- Ellis, E.G. Covid-19 Is Killing Black People Unequally—Don’t Be Surprised—May 2, 2020. Wired. Available online: https://www.wired.com/story/covid-19-coronavirus-racial-disparities/ (accessed on 16 May 2020).
- Watson, B.; Robinson, D.H.; Harker, L.; Arriola, K.R. The Inclusion of African-American Study Participants in Web-Based Research Studies: Viewpoint. J. Med. Internet Res. 2016, 18, e168. [Google Scholar] [CrossRef]
- National Institutes of Health. Pathways to Prevention Workshop: Methods for Evaluating Natural Experiments in Obesity. December 5–6, 2017 in Natcher Conference Center, NIH Campus, Bethesda, Maryland. Available online: https://prevention.nih.gov/p2p-workshop/2017/methods-evaluating-natural-experiments-obesity (accessed on 11 November 2017).
- Terrell, F.; Moseley, K.L.; Terrell, A.S.; Nickerson, K.J. The relationship between motivation to volunteer, gender, cultural mistrust, and willingness to donate organs among Blacks. J. Natl. Med. Assoc. 2004, 96, 53–60. [Google Scholar]
- Richardson, A.; Allen, J.A.; Xiao, H.; Vallone, D. Effects of race/ethnicity and socioeconomic status on health information-seeking, confidence, and trust. J. Health Care Poor Underserved 2012, 23, 1477–1493. [Google Scholar] [CrossRef]
- Harmon, B.E.; Kim, S.H.; Blake, C.E.; Hebert, J.R. Health care information in African American churches. J. Health Care Poor Underserved 2014, 25, 242–256. [Google Scholar] [CrossRef] [Green Version]
- CDC. Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html (accessed on 7 April 2020).
- Alfonso, F., III. Why Some People of Color Say They Won’t Wear Homemade Masks—April 7, 2020. CNN. Available online: https://www.cnn.com/2020/04/07/us/face-masks-ethnicity-coronavirus-cdc-trnd/index.html (accessed on 7 April 2020).
- Stephens, J. Video: Wood River Officer Made Black Men Leave Walmart Because they Wore Masks—March 24, 2020. The Telegraph. Available online: https://www.thetelegraph.com/news/article/Video-Wood-River-officer-has-men-leave-Walmart-15154393.php (accessed on 7 April 2020).
- Thomas, A. I’m a Black Man in America. Entering a Shop With a Face Mask Might Get Me Killed—April 7, 2020. The Guardian. Available online: https://www.theguardian.com/commentisfree/2020/apr/07/black-men-coronavirus-masks-safety (accessed on 7 April 2020).
- Park, E. Confronting Anti-Asian Discrimination During the Coronavirus Crisis—March 17, 2020. The New Yorker. Available online: https://www.newyorker.com/culture/culture-desk/confronting-anti-asian-discrimination-during-the-coronavirus-crisis (accessed on 17 May 2020).
- Connolly, G. Coronavirus: FBI Director Warns of Potential for Spike in Hate Crimes as Anti-Asian Incidents Surge. The Independent. Available online: https://www.independent.co.uk/news/world/americas/us-politics/coronavirus-hate-crimes-anti-asian-attacks-fbi-us-cases-a9479191.html (accessed on 17 May 2020).
- Liu, E. Covid-19 Has Inflamed Racism Against Asian-Americans. Here’s How to Fight Back—April 11, 2020. CNN. Available online: https://www.cnn.com/2020/04/10/opinions/how-to-fight-bias-against-asian-americans-covid-19-liu/index.html (accessed on 17 May 2020).
- Quinn, S.C.; Kumar, S. Health Inequalities and Infectious Disease Epidemics: A Challenge for Global Health Security. Biosecur. Bioterror. 2014, 12, 263–273. [Google Scholar] [CrossRef] [Green Version]
- Harmon, A.; Rojas, R. A Delicate Balance: Weighing Protest Against the Risks of the Coronavirus—June 7, 2020. New York Times. Available online: https://www.nytimes.com/2020/06/07/us/Protest-coronavirus-george-floyd.html (accessed on 8 June 2020).
- Taylor, A. Images From a Worldwide Protest Movement—June 8, 2020. The Atlantic. Available online: https://www.theatlantic.com/photo/2020/06/images-worldwide-protest-movement/612811/ (accessed on 11 June 2020).
- Frieden, T. A New Normal With COVID-19: The Next Steps We Must Take. Think Global Health. Council on Foreign Relations. Available online: https://www.thinkglobalhealth.org/article/new-normal-covid-19-next-steps-we-must-take (accessed on 17 May 2020).
- RTSL. When and How to Reopen After COVID-19. Resolve to Save Lives. Vital Strategies. Available online: https://preventepidemics.org/wp-content/uploads/2020/04/COV020_WhenHowLoosenFaucet_v4.pdf (accessed on 17 May 2020).
- Guidelines for Opening Up America Again. U.S. Centers for Disease Control. Available online: https://www.whitehouse.gov/openingamerica/ (accessed on 11 June 2020).
- Guterres, A. We are all in this Together: Human Rights and COVID-19 Response and Recovery. United Nations. Available online: https://www.un.org/en/un-coronavirus-communications-team/we-are-all-together-human-rights-and-covid-19-response-and (accessed on 11 June 2020).
- Dietz, L.; Horve, P.F.; Coil, D.A.; Fretz, M.; Eisen, J.A.; van den Wymelenberg, K. 2019 Novel Coronavirus (COVID-19) Pandemic: Built Environment Considerations To Reduce Transmission. mSystems 2020, 5. [Google Scholar] [CrossRef] [Green Version]
- EYQ. While Addressing the Now and Planning the Next, Organizations Must Also Consider the Lasting Shifts That Could Be the Legacy of COVID-19. Ernst & Young Global Limited. Available online: https://www.ey.com/en_gl/covid-19/will-you-define-the-new-normal-or-watch-it-unfold (accessed on 17 May 2020).
- Hlavinka, E. COVID-19 Killing African Americans at Shocking Rates—Wildly Disproportionate Mortality Highlights Need to Address Longstanding Inequities. Medpage Today. Available online: https://www.medpagetoday.com/infectiousdisease/covid19/86266 (accessed on 17 May 2020).
- Anonymous. A Prose Poem on the Epidemic. Am. J. Nurs. 1919, 19, 718. [Google Scholar]

| African American Women | Hispanic Women | Asian American Women | American Indian Women | Other Non-White Women | Two or More Races Women | |
|---|---|---|---|---|---|---|
| 1 | nursing assistants | maids/housekeeping cleaners | registered nurses | cashiers | maids/housekeeping cleaners | cashiers |
| 2 | cashiers | cashiers | accountants/auditors | secretaries/administrative assistants | cashiers | registered nurses |
| 3 | customer service representatives | customer service representatives | cashiers | maids/housekeeping cleaners | nursing assistants | waitresses |
| 4 | registered nurses | secretaries/administrative assistants | manicurists/pedicurists | elementary/middle school teachers | registered nurses | elementary/middle school teachers |
| 5 | personal care aides | janitors/building cleaners | personal care aides | personal care aides | child care workers | customer service representatives |
| 6 | elementary/middle school teachers | retail salespeople | retail salespeople | registered nurses | retail salespeople | secretaries/administrative assistants |
| Pandemic Characteristics | 1918 Influenza Pandemic | 2019 Coronavirus Pandemic |
|---|---|---|
| Epidemiology | ||
| Disease Pathogen | Influenza A (H1N1) | SARS-CoV-2 |
| Pandemic Origin | Fort Riley, Kansas, USA | Wuhan, China |
| Pandemic Waves | 3 | 1 as of June 21, 2020 |
| At Risk Population (Age) | 15–34 years | 65+ years |
| Life Expectancy Reduction | yes | no |
| Overall Mortality | 675,000 | 119,810 as of June 21, 2020 |
| Environment | ||
| Hospital Environments | open-air | airborne infection isolation |
| Quarantine Measures | yes | yes |
| Military Environmental Risk | yes | no |
| Airplane Environment Risk | no | yes |
| Reduced Public Transit | yes | yes |
| Urban Environment Deficiencies | yes | yes |
| Behavior | ||
| Social Distancing | yes | yes |
| Cloth Face Mask | yes | yes |
| Racial Profiling | yes | yes |
| Public Gatherings | no | no |
| Political Resistance | yes | yes |
| Widespread Protests | no | yes |
| Inequalities | ||
| Healthcare Discrimination | yes (sanctioned) | yes |
| Health Provider Discrimination | yes (sanctioned) | yes |
| Economic Inequalities | yes | yes |
| Rural vs. Urban Inequalities | yes | yes |
| Preexisting Health Risks | yes | yes |
| Mortality Disparities (Race) | White Americans | African Americans |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roberts, J.D.; Tehrani, S.O. Environments, Behaviors, and Inequalities: Reflecting on the Impacts of the Influenza and Coronavirus Pandemics in the United States. Int. J. Environ. Res. Public Health 2020, 17, 4484. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124484
Roberts JD, Tehrani SO. Environments, Behaviors, and Inequalities: Reflecting on the Impacts of the Influenza and Coronavirus Pandemics in the United States. International Journal of Environmental Research and Public Health. 2020; 17(12):4484. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124484
Chicago/Turabian StyleRoberts, Jennifer D., and Shadi O. Tehrani. 2020. "Environments, Behaviors, and Inequalities: Reflecting on the Impacts of the Influenza and Coronavirus Pandemics in the United States" International Journal of Environmental Research and Public Health 17, no. 12: 4484. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124484





