The Office Work and Stretch Training (OST) Study: An Individualized and Standardized Approach to Improve the Quality of Life in Office Workers
Abstract
:1. Introduction
2. Methods
2.1. Subjects
2.2. Intervention Program
2.3. Short Form 36
2.4. Measurement Protocol
2.5. Statistical Analysis
2.6. Ethics Approval
3. Results
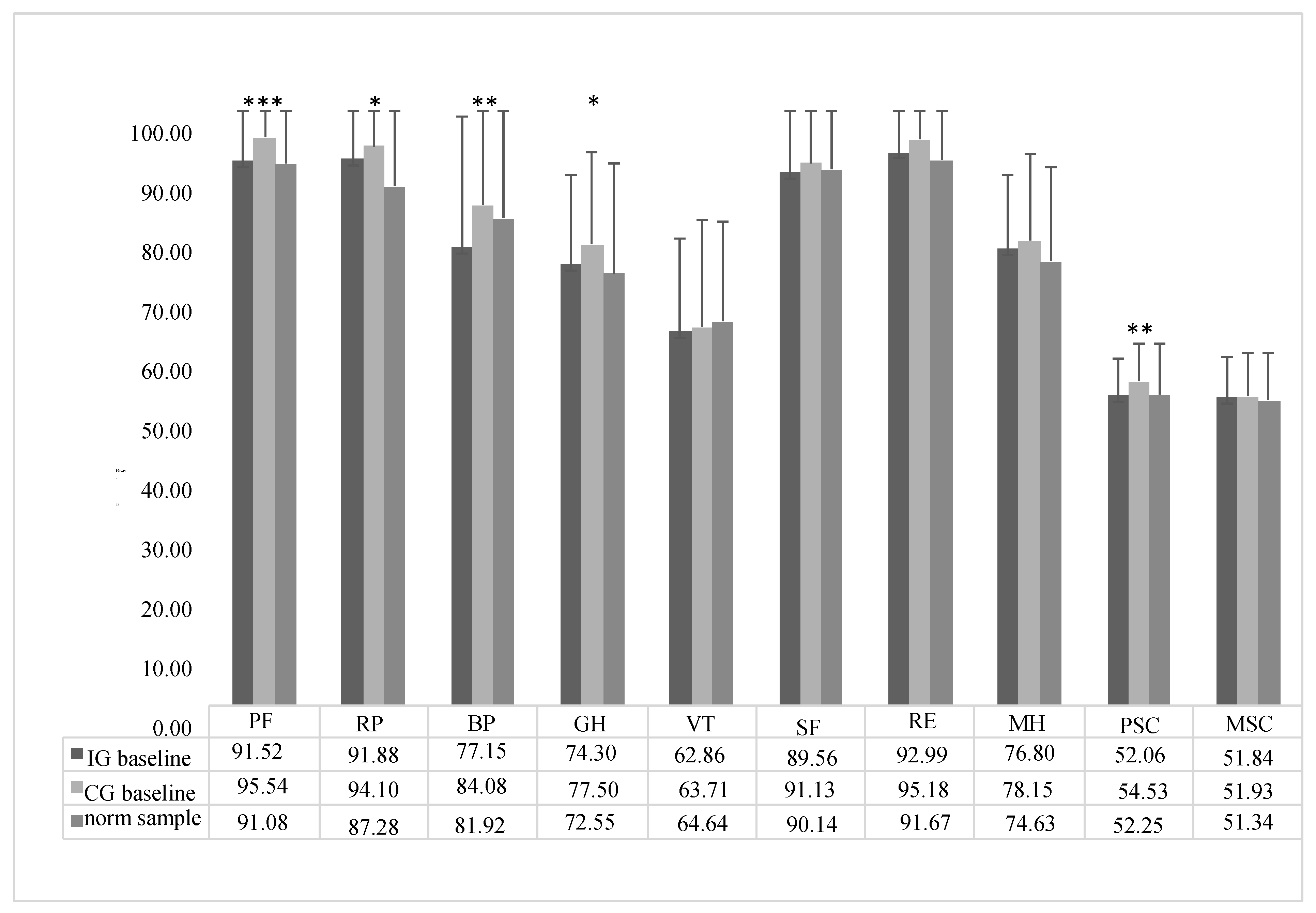
3.1. Comparison of SF-36 Baseline Data
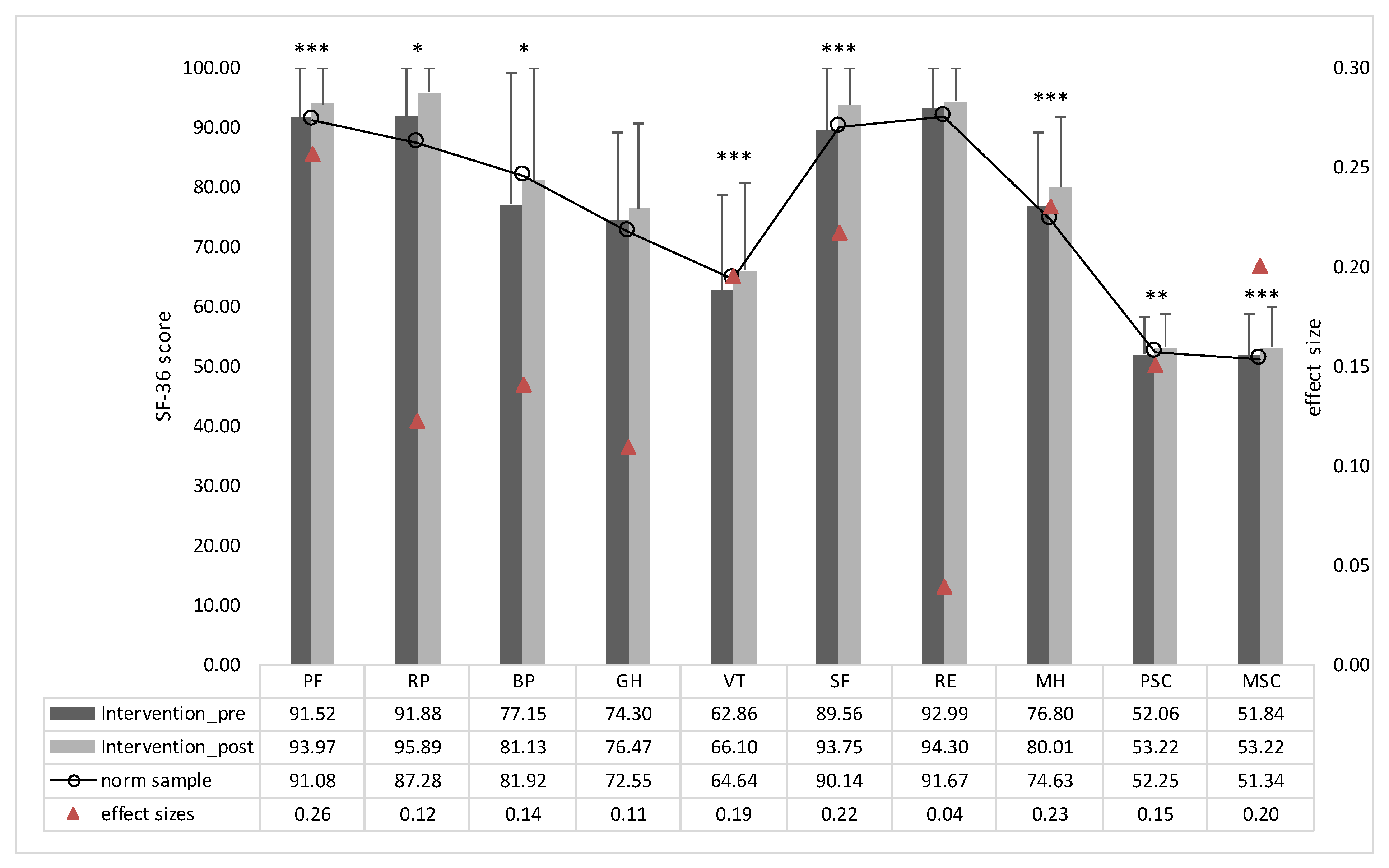
3.2. Examiation of the Effectiveness of the Intervention
3.3. Analysis for Gender Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| SD | standard deviation |
| QoL | quality of life |
| MSD | musculoskeletal disorders |
| WHPPs | workplace health promotion programs |
| IG | intervention group |
| CG | control group |
| PF | physical functioning |
| RP | role limitations due to physical problems |
| BP | bodily pain |
| GH | general health perceptions |
| VT | vitality |
| SF | social functioning |
| RE | role limitations due to emotional problems |
| MH | mental health |
| PSC | physical sum score |
| MSC | mental sum score |
References
- Marschall, J.; Hildebrandt, S.; Nolting, H.D. Gesundheitsreport 2019: Analyse der Arbeitsunfähigkeitsdaten Alte und neue Süchte im Betrieb; DAK Gesundheit: Hamburg, Germany, 2019. [Google Scholar]
- Burton, W.N.; Conti, D.J.; Chen, C.Y.; Schultz, A.B.; Edington, D.W. The role of health risk factors and disease on worker productivity. J. Occup. Environ. Med. 1999, 41, 863–877. [Google Scholar] [CrossRef] [PubMed]
- Loeppke, R.; Edington, D.; Bender, J.; Reynolds, A. The association of technology in a workplace wellness program with health risk factor reduction. J. Occup. Environ. Med. 2013, 55, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Leite, W.K.D.S.; Silva, L.B.D.; Souza, E.L.D.; Fernandes, J.G.B.; Colaco, G.A. Risk of WMSDs in monofuntional and multifunctional workers in a Brazilian footwear company. Production 2017, 27. [Google Scholar] [CrossRef] [Green Version]
- Vieira, E.R.; Serra, M.V.G.B.; de Almeida, L.B.; Villela, W.V.; Scalon, J.D.; Quemelo, P.R.V. Symptoms and risks for musculoskeletal disorders among male and female footwear industry workers. Int. J. Ind. Ergon. 2015, 48, 110–116. [Google Scholar] [CrossRef]
- Rutanen, R.; Nygård, C.-H.; Moilanen, J.; Mikkola, T.; Raitanen, J.; Tomas, E.; Luoto, R. Effect of physical exercise on work ability and daily strain in symptomatic menopausal women: A randomized controlled trial. Work 2014, 47, 281–286. [Google Scholar] [CrossRef]
- Lamb, S.; Kwok, K.C. A longitudinal investigation of work environment stressors on the performance and wellbeing of office workers. Appl. Ergon. 2016, 52, 104–111. [Google Scholar] [CrossRef]
- Da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am. J. Ind. Med. 2010, 53, 285–323. [Google Scholar] [CrossRef]
- Mazda Adli, B.B.; Birner, U.; Bogert, B. BKK Gesundheitsreport 2019; Medizinisch Wissenschaftliche Verlagsgesellschaft: Berlin, Germany, 2019. [Google Scholar]
- Brenscheidt, S.S.A.; Hinnenkamp, H.; Hünefeld, L. Arbeitswelt im Wandel: Zahlen—Daten—Fakten (2019). Ausgabe 2019; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin (BAuA): Dortmund, Germany, 2019.
- Rongen, A.; Robroek, S.J.; van Lenthe, F.J.; Burdorf, A. Workplace health promotion: A meta-analysis of effectiveness. Am. J. Prev. Med. 2013, 44, 406–415. [Google Scholar] [CrossRef]
- Robroek, S.J.; Polinder, S.; Bredt, F.J.; Burdorf, A. Cost-effectiveness of a long-term Internet-delivered worksite health promotion programme on physical activity and nutrition: A cluster randomized controlled trial. Health Educ. Res. 2012, 27, 399–410. [Google Scholar] [CrossRef] [Green Version]
- Terry, P.E.; Fowles, J.B.; Xi, M.; Harvey, L. The ACTIVATE study: Results from a group-randomized controlled trial comparing a traditional worksite health promotion program with an activated consumer program. Am. J. Health Promot. 2011, 26, e64–e73. [Google Scholar] [CrossRef]
- Groeneveld, I.F.; van Wier, M.F.; Proper, K.I.; Bosmans, J.E.; van Mechelen, W.; van der Beek, A.J. Cost-effectiveness and cost-benefit of a lifestyle intervention for workers in the construction industry at risk for cardiovascular disease. J. Occup. Environ. Med. 2011, 53, 610–617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tunwattanapong, P.; Kongkasuwan, R.; Kuptniratsaikul, V. The effectiveness of a neck and shoulder stretching exercise program among office workers with neck pain: A randomized controlled trial. Clin. Rehabil. 2016, 30, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Zavanela, P.M.; Crewther, B.T.; Lodo, L.; Florindo, A.A.; Miyabara, E.H.; Aoki, M.S. Health and fitness benefits of a resistance training intervention performed in the workplace. J. Strength Cond. Res. 2012, 26, 811–817. [Google Scholar] [CrossRef]
- Shariat, A.; Mohd Tamrin, S.B.; Arumugam, M.; Danaee, M.; Ramasamy, R. Office Exercise Training to Reduce and Prevent the Occurrence of Musculoskeletal Disorders among Office Workers: A Hypothesis. MJMS 2016, 23, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Marker, A.M.; Steele, R.G.; Noser, A.E. Physical activity and health-related quality of life in children and adolescents: A systematic review and meta-analysis. Health Psychol. 2018, 37, 893–903. [Google Scholar] [CrossRef]
- Puciato, D.; Borysiuk, Z.; Rozpara, M. Quality of life and physical activity in an older working-age population. Clin. Interv. Aging 2017, 12, 1627–1634. [Google Scholar] [CrossRef] [Green Version]
- Vagetti, G.C.; Barbosa Filho, V.C.; Moreira, N.B.; Oliveira, V.; Mazzardo, O.; Campos, W. Association between physical activity and quality of life in the elderly: A systematic review, 2000–2012. Rev. Bras. Psiquiatr. 2014, 36, 76–88. [Google Scholar] [CrossRef] [Green Version]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar] [CrossRef] [Green Version]
- Perez-Cruzado, D.; Cuesta-Vargas, A.; Vera-Garcia, E.; Mayoral-Cleries, F. The relationship between quality of life and physical fitness in people with severe mental illness. Health Qual. Life Outcomes 2018, 16, 82. [Google Scholar] [CrossRef] [Green Version]
- Rosenbaum, S.; Tiedemann, A.; Ward, P.B. Meta-analysis physical activity interventions for people with mental illness: A systematic review and meta-analysis. J. Clin. Psychiatry 2014, 75, 1–11. [Google Scholar] [CrossRef]
- Sihawong, R.; Janwantanakul, P.; Sitthipornvorakul, E.; Pensri, P. Exercise therapy for office workers with nonspecific neck pain: A systematic review. J. Manip. Physiol. Ther. 2011, 34, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Louw, S.; Makwela, S.; Manas, L.; Meyer, L.; Terblanche, D.; Brink, Y. Effectiveness of exercise in office workers with neck pain: A systematic review and meta-analysis. South Afr. J. Physiother. 2017, 73, 392. [Google Scholar] [CrossRef] [PubMed]
- Van Eerd, D.; Munhall, C.; Irvin, E.; Rempel, D.; Brewer, S.; Van Der Beek, A.; Dennerlein, J.; Tullar, J.; Skivington, K.; Pinion, C. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: An update of the evidence. Occup. Environ. Med. 2016, 73, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Page, P. Current concepts in muscle stretching for exercise and rehabilitation. Int. J. Sports Phys. Ther. 2012, 7, 109. [Google Scholar]
- Marangoni, A.H. Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcomes. Work 2010, 36, 27–37. [Google Scholar] [CrossRef]
- Bracke, P.E. Progressive muscle relaxation. Corsini Encycl. Psychol. 2010. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1002/9780470479216.corpsy0712. (accessed on 15 February 2020).
- Gross, D.P.; Algarni, F.S.; Niemelainen, R. Reference values for the SF-36 in Canadian injured workers undergoing rehabilitation. J. Occup. Rehabil. 2015, 25, 116–126. [Google Scholar] [CrossRef]
- Leone, M.A.; Beghi, E.; Righini, C.; Apolone, G.; Mosconi, P. Epilepsy and quality of life in adults: A review of instruments. Epilepsy Res. 2005, 66, 23–44. [Google Scholar] [CrossRef]
- Graves, J.M.; Fulton-Kehoe, D.; Jarvik, J.G.; Franklin, G.M. Early imaging for acute low back pain: One-year health and disability outcomes among Washington State workers. Spine 2012, 37, 1617–1627. [Google Scholar] [CrossRef]
- Newnham, E.A.; Harwood, K.E.; Page, A.C. Evaluating the clinical significance of responses by psychiatric inpatients to the mental health subscales of the SF-36. J. Affect. Disord. 2007, 98, 91–97. [Google Scholar] [CrossRef]
- Nishiyama, T.; Ozaki, N. Measurement limit of quality-of-life questionnaires in psychiatric settings. Qual. Life Res. 2010, 19, 25–30. [Google Scholar] [CrossRef]
- Holzgreve, F.; Maltry, L.; Lampe, J.; Schmidt, H.; Bader, A.; Rey, J.; Groneberg, D.A.; van Mark, A.; Ohlendorf, D. The office work and stretch training (OST) study: An individualized and standardized approach for reducing musculoskeletal disorders in office workers. J. Occup. Med. Toxicol. 2018, 13, 37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Myers, T.W. Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists; Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- McKenzie, R.; May, S. The Lumbar Spine Mechanical Diagnosis & Therapy; Spinal Publications New Zealand: Waikanae, New Zealand, 2003. [Google Scholar]
- Saner-Bissig, J. McKenzie—Mechanische Diagnose und Therapie: 3 Tabellen; Thieme Georg Verlag: Stuttgart, Germany, 2007. [Google Scholar]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Morfeld, M.; Kirchberger, I.; Bullinger, M. SF-36 Fragebogen Zum Gesundheitszustand: Deutsche Version Des Short Form-36 Health Survey; Hogrefe: Göttingen, Germany, 2011. [Google Scholar]
- Rippentrop, A.E.; Altmaier, E.M.; Chen, J.J.; Found, E.M.; Keffala, V.J. The relationship between religion/spirituality and physical health, mental health, and pain in a chronic pain population. Pain 2005, 116, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Glombiewski, J.A.; Hartwich-Tersek, J.; Rief, W. Depression in chronic back pain patients: Prediction of pain intensity and pain disability in cognitive-behavioral treatment. Psychosomatics 2010, 51, 130–136. [Google Scholar] [CrossRef]
- Goncalves, T.R.; Mediano, M.F.F.; Sichieri, R.; Cunha, D.B. Is Health-related Quality of Life Decreased in Adolescents with Back Pain? Spine 2018, 43, E822–E829. [Google Scholar] [CrossRef]
- Rudy, T.E.; Weiner, D.K.; Lieber, S.J.; Slaboda, J.; Boston, J.R. The impact of chronic low back pain on older adults: A comparative study of patients and controls. Pain 2007, 131, 293–301. [Google Scholar] [CrossRef]
- Halbertsma, J.P.; Göeken, L.N.; Hof, A.L.; Groothoff, J.W.; Eisma, W.H. Extensibility and stiffness of the hamstrings in patients with nonspecific low back pain. Arch. Phys. Med. Rehabil. 2001, 82, 232–238. [Google Scholar] [CrossRef]
- Nourbakhsh, M.R.; Arab, A.M. Relationship between mechanical factors and incidence of low back pain. J. Orthop. Sports Phys. Ther. 2002, 32, 447–460. [Google Scholar] [CrossRef]
- Lawand, P.; Júnior, I.L.; Jones, A.; Sardim, C.; Ribeiro, L.H.; Natour, J. Effect of a muscle stretching program using the global postural reeducation method for patients with chronic low back pain: A randomized controlled trial. Jt. Bone Spine 2015, 82, 272–277. [Google Scholar] [CrossRef]
- Hartfiel, N.; Burton, C.; Rycroft-Malone, J.; Clarke, G.; Havenhand, J.; Khalsa, S.B.; Edwards, R.T. Yoga for reducing perceived stress and back pain at work. Occup. Med. 2012, 62, 606–612. [Google Scholar] [CrossRef] [Green Version]
- Morimoto, T.; Oguma, Y.; Yamazaki, S.; Sokejima, S.; Nakayama, T.; Fukuhara, S. Gender differences in effects of physical activity on quality of life and resource utilization. Qual. Life Res. 2006, 15, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Sundelin, G. Patterns of electromyographic shoulder muscle fatigue during MTM-paced repetitive arm work with and without pauses. Int. Arch. Occup. Environ. Health 1993, 64, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Samani, A.; Holtermann, A.; Søgaard, K.; Madeleine, P. Active pauses induce more variable electromyographic pattern of the trapezius muscle activity during computer work. J. Electromyogr. Kinesiol. 2009, 19, e430–e437. [Google Scholar] [CrossRef] [PubMed]
- Richter, J.M.; Slijper, H.P.; Over, E.A.; Frens, M.A. Computer work duration and its dependence on the used pause definition. Appl. Ergon. 2008, 39, 772–778. [Google Scholar] [CrossRef] [PubMed]



| Entire Sample [Mean (SD) or %] | Intervention Group [Mean (SD) or %] | Control Group [Mean (SD) or %] | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | ||||
| Initial participants | n = 313 | n = 172 | n = 137 | n = 216 | n = 135 | n = 78 | n = 97 | n = 38 | n = 59 |
| Dropouts | n = 60 | n = 35 | n = 22 | n = 58 | n = 33 | n = 22 | n = 2 | n = 2 | n = 0 |
| Final participants | n = 253 | n = 138 | n = 115 | n = 158 | n = 102 | n = 56 | n = 95 | n = 36 | n = 59 |
| Age (years) ** | 43.37 (11.24) | 46.74 (10.21) | 39.32 (11.11) | 44.94 (10.56) | 47.42 (9.52) | 40.33 (10.84) | 40.83 (11.92) | 44.86 (11.86) | 38.37 (11.37) |
| Height (cm) | 175.37 (9.35) | 180.34 (7.18) | 169.41 (8.10) | 176.21 (8.76) | 180.78 (6.24) | 167.89 (6.21) | 173.98 (10.15) | 179.11 (9.36) | 170.85 (9.38) |
| Weight (kg) *** | 75.76 (15.23) | 82.90 (13.51) | 67.12 (12.52) | 78.15 (15.02) | 83.83 (13.19) | 67.43 (12.49) | 71.97 (14.74) | 80.25 (14.23) | 66.83 (12.64) |
| BMI (kg/m2) ** | 24.50 (3.81) | 25.45 (3.64) | 23.35 (3.71) | 25.03 (3.97) | 25.64 (3.74) | 23.90 (4.18) | 23.61 (3.35) | 24.89 (3.34) | 22.81 (3.13) |
| Handedness (% right) | 94.90 | 94.20 | 95.70 | 93.70 | 94.10 | 92.90 | 96.80 | 94.20 | 98.30 |
| Doing sports (% yes) | 72.70 | 72.50 | 73.00 | 70.90 | 70.60 | 71.40 | 75.80 | 77.80 | 74.60 |
| Smoking (% non-smoker) | 88.90 | 90.60 | 87.00 | 89.90 | 92.20 | 85.70 | 96.80 | 86.10 | 88.10 |
| h/sports/week *** | 3.13 (3.01) | 3.2 (3.17) | 3.04 (2.80) | 2.77 (3.17) | 2.97 (3.29) | 2.41 (2.92) | 3.96 (2.45) | 4.04 (2.56) | 3.90 (2.40) |
| IG-CG | IG-Norm Sample | CG-Norm Sample | |
|---|---|---|---|
| PF | < 0.001 | 0.005 | 0.001 |
| RP | > 0.05 | > 0.05 | 0.023 |
| BP | 0.049 | < 0.000 | > 0.05 |
| GH | > 0.05 | > 0.05 | 0.039 |
| PSC | 0.021 | 0.021 | > 0.05 |
| Intervention Group | Control Group | Intervention–Control Study | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||||||||||
| Pre | Post | p Value a | Effect Size r b | Pre | Post | p Value a | Effect Size r b | diff. IG | diff. CG | p Value c | Effect Size r b | |
| PF | 91.52 (10.38) | 93.97 (10.17) | <0.001 | 0.26 | 96.51 (6.92) | 97.22 (6.79) | 0.056 | 0.19 | 2.45 (8.09) | 0.70 (5.18) | <0.001 | 0.21 |
| RP | 91.88 (21.97) | 95.89 (14.07) | 0.030 | 0.12 | 94.15 (18.85) | 97.19 (11.51) | 0.053 | 0.01 | 3.98 (23.09) | 3.28 (17.29) | >0.2 | 0.01 |
| BP | 77.15 (21.97) | 81.13 (19.62) | 0.013 | 0.14 | 83.68 (20.61) | 81.76 (17.98) | >0.2 | 0.15 | 4.04 (18.69) | −1.93 (18.55) | 0.01 | 0.16 |
| GH | 74.30 (14.88) | 76.47 (14.04) | 0.053 | 0.11 | 77.61 (15.35) | 77.67 (13.41) | >0.2 | 0.08 | 2.17 (12.08) | 0.02 (12.24) | 0.154 | 0.09 |
| VT | 62.86 (15.77) | 66.10 (14.67) | <0.001 | 0.19 | 63.74 (17.91) | 63.96 (16.45) | >0.2 | 0.13 | 3.24 (11.88) | 0.23 (13.94) | 0.025 | 0.14 |
| SF | 89.56 (15.32) | 93.75 (12.03) | <0.001 | 0.22 | 91.13 (14.70) | 92.63 (13.08) | >0.2 | 0.10 | 4.19 (13.21) | 1.34 (14.57) | 0.080 | 0.11 |
| RE | 92.99 (19.26) | 94.30 (19.25) | >0.2 | 0.04 | 95.44 (16.57) | 92.28 (21.44) | 0.090 | 0.13 | 1.27 (22.61) | −3.16 (19.49) | 0.018 | 0.15 |
| MH | 76.80 (12.39) | 80.01 (11.85) | <0.001 | 0.23 | 78.02 (14.34) | 78.75 (13.27) | >0.2 | 0.14 | 3.21 (10.27) | 0.72 (10.70) | 0.012 | 0.16 |
| PSC | 52.06 (6.19) | 53.22 (5.46) | 0.009 | 0.15 | 54.11 (5.24) | 54.42 (4.18) | >0.2 | 0.09 | 1.20 (5.24) | 0.33 (4.64) | 0.103 | 0.10 |
| MSC | 51.84 (6.84) | 53.22 (6.62) | <0.001 | 0.20 | 52.00 (7.37) | 51.75 (7.32) | >0.2 | 0.15 | 1.37 (5.86) | −0.13 (5.59) | 0.008 | 0.17 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holzgreve, F.; Maltry, L.; Hänel, J.; Schmidt, H.; Bader, A.; Frei, M.; Filmann, N.; Groneberg, D.A.; Ohlendorf, D.; van Mark, A. The Office Work and Stretch Training (OST) Study: An Individualized and Standardized Approach to Improve the Quality of Life in Office Workers. Int. J. Environ. Res. Public Health 2020, 17, 4522. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124522
Holzgreve F, Maltry L, Hänel J, Schmidt H, Bader A, Frei M, Filmann N, Groneberg DA, Ohlendorf D, van Mark A. The Office Work and Stretch Training (OST) Study: An Individualized and Standardized Approach to Improve the Quality of Life in Office Workers. International Journal of Environmental Research and Public Health. 2020; 17(12):4522. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124522
Chicago/Turabian StyleHolzgreve, Fabian, Laura Maltry, Jasmin Hänel, Helmut Schmidt, Andreas Bader, Markus Frei, Natalie Filmann, David Alexander Groneberg, Daniela Ohlendorf, and Anke van Mark. 2020. "The Office Work and Stretch Training (OST) Study: An Individualized and Standardized Approach to Improve the Quality of Life in Office Workers" International Journal of Environmental Research and Public Health 17, no. 12: 4522. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17124522





