The Reciprocal Association between Fitness Indicators and Sleep Quality in the Context of Recent Sport Injury
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.3. Statistical Analysis
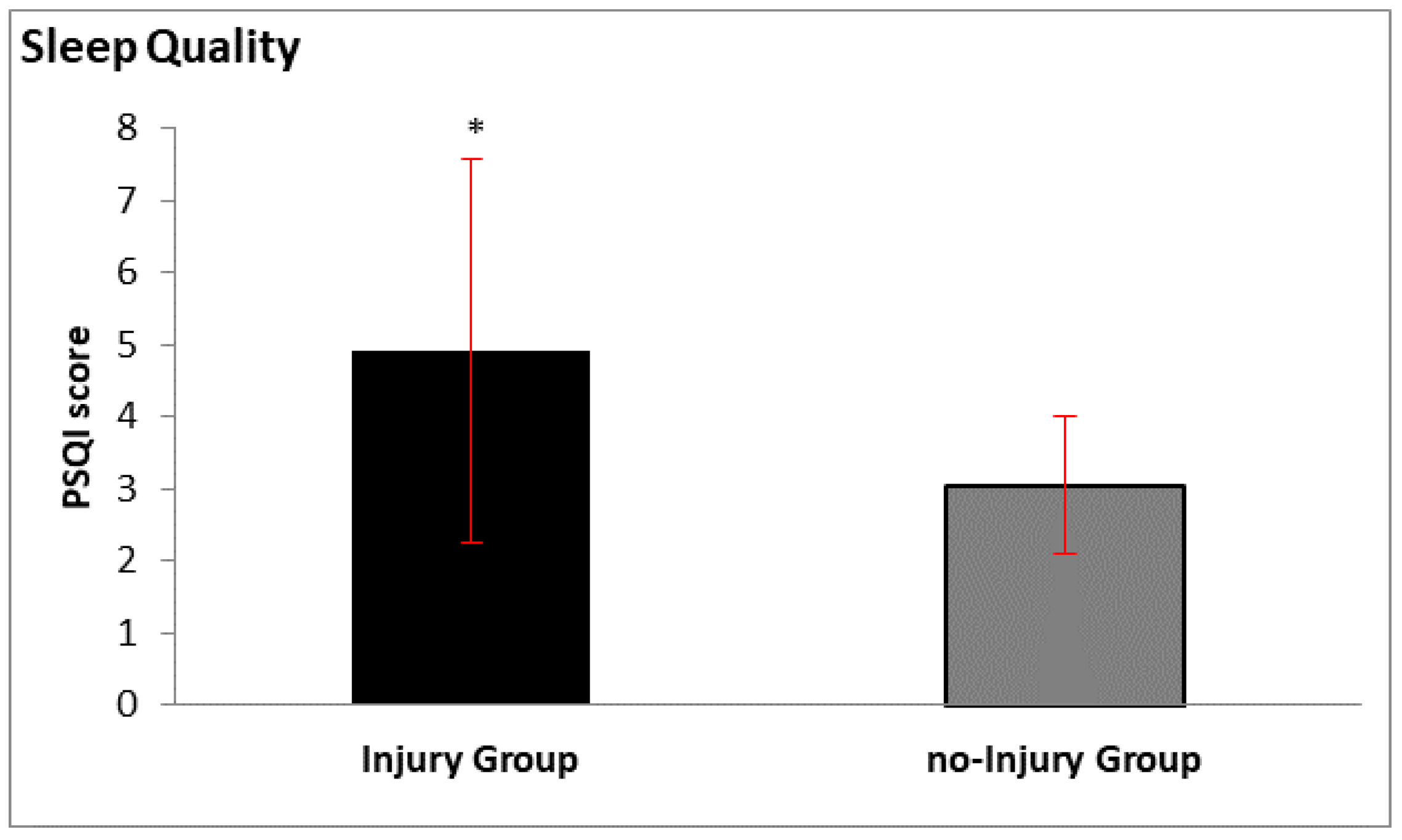
3. Results
4. Discussion
4.1. Cardiopulmonary Changes and Injury
4.2. Sleep Quality and Injury
5. Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Giacchino, M.; Stesina, G. Prevention of Muscle Injuries-The Soccer Mode. In Muscle Injuries in Sport Medicine; IntechOpen Limited: London, UK, 2013; Available online: https://www.intechopen.com/books/muscle-injuries-in-sport-medicine/prevention-of-muscle-injuries-the-soccer-model#B1 (accessed on 26 June 2020).
- Corazza, A.; Orlandi, D.; Baldari, A.; Gatto, P.; Stellatelli, M.; Mazzola, C.; Galli, R.; Longo, S.; Sconfienza, L.M.; Silvestri, E. Thigh muscles injuries in professional soccer players: A one year longitudinal study. Muscles Ligaments Tendons J. 2014, 3, 331–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez-Sanz, D.; Losa-Iglesias, M.E.; Becerro de Bengoa-Vallejo, R.; Palomo-Lopez, P.; Beltran-Alacreu, H.; Calvo-Lobo, C.; Navarro-Flores, E.; Lopez-Lopez, D. Skin temperature in youth soccer players with functional equinus and non-equinus condition after running. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 2020–2024. [Google Scholar] [CrossRef] [PubMed]
- Neufer, P.D. The Effect of Detraining and Reduced Training on the Physiological Adaptations to Aerobic Exercise Training. Sports Med. 1989, 8, 302–320. [Google Scholar] [CrossRef] [PubMed]
- Stavrou, V.; Tsarouhas, K.; Karetsi, E.; Michos, P.; Daniil, Z.; Gourgoulianis, K.Ι. Adolescent finswimmers: Early myocardial adaptations in different swimming styles. Sports (Basel) 2018, 6, 78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Godfrey, R.; Ingham, S.; Pedlar, C.; Whyte, G. The detraining and retraining of an elite rower: A case study. J. Sci. Med. Sport 2005, 8, 314–320. [Google Scholar] [CrossRef]
- Almeida, A.M.; Santos Silva, P.R.; Pedrinelli, A.; Hernandez, A.J. Aerobic fitness in professional soccer players after anterior cruciate ligament reconstruction. PLoS ONE 2018, 13, e0194432. [Google Scholar] [CrossRef]
- Waldén, M.; Hägglund, M.; Ekstrand, J. High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br. J. Sports Med. 2006, 40, 158–162. [Google Scholar] [CrossRef] [Green Version]
- Chennaoui, M.; Arnal, P.J.; Sauvet, F.; Léger, D. Sleep and exercise: A reciprocal issue? Sleep Med. Rev. 2015, 20, 59–72. [Google Scholar] [CrossRef]
- Gao, B.; Dwivedi, S.; Milewski, M.D.; Cruz, A.I., Jr. Chronic lack of sleep is associated with increased sports injury in adolescents: A systematic review and meta-analysis. Orthop. J. Sports Med. 2019, 7 (Suppl. S3), 2325967119S00132. [Google Scholar] [CrossRef] [Green Version]
- Burke, T.M.; Lisman, P.J.; Maguire, K.; Skeiky, L.; Choynowski, J.J.; Capaldi, V.F., 2nd; Wilder, J.N.; Brager, A.J.; Dobrosielski, D.A. Examination of Sleep and Injury Among College Football Athletes. J. Strength Cond. Res. 2020, 34, 609–616. [Google Scholar] [CrossRef]
- Sousa, C.V.; Pereira, R.W.; Rosemann, T.; Nikolaidis, P.T.; Knechtle, B. Self-Selected Pacing During a World Record Attempt in 40 Ironman-Distance Triathlons in 40 Days. Int. J. Environ. Res. Public Health 2020, 17, 2390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. STROBE Initiative Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holt, G.R. Declaration of Helsinki—The World’s Document of Conscience and Responsibility. South. Med. J. 2014, 107, 407. [Google Scholar] [CrossRef] [PubMed]
- Norton, K.; Whittingham, N.; Carter, L.; Kerr, D.; Gore, C.; Marfell-Jones, M. Measurement techniques in anthropometry. In Anthropometrica; Norton, K., Olds, T., Eds.; University of New South Wales Press: Sydney, Australia, 1996; pp. 25–44. [Google Scholar]
- Wells, K.F.; Dillon, E.K. The Sit and Reach—A Test of Back and Leg Flexibility, Research Quarterly. Am. Assoc. Health Phys. Educ. Recreat. 1952, 23, 115–118. [Google Scholar]
- Mosteller, R.D. Simplified calculate on of body-surface area. N. Engl. J. Med. 1987, 317, 1098. [Google Scholar] [PubMed]
- Boer, P. Estimated lean body mass as an index for normalization of body fluid volumes in man. Am. J. Physiol. 1984, 247, F632–F635. [Google Scholar]
- Wasserman, K.; Hansen, J.E.; Sue, D.Y.; Stringer, W.W.; Whipp, B. Principles of exercise testing and interpretation: Including pathophysiology and clinical applications, 4th ed.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2004; p. 317. [Google Scholar]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef] [Green Version]
- Perantoni, E.; Steiropoulos, P.; Siopi, D.; Amfilochiou, A.; Michailidis, V.; Christoforatou, K.; Tsara, V. Validation of the Greek version of Pittsburg sleep quality questionnaire in a sleep lab population. Eur. Respir. J. 2012, 40, 903. [Google Scholar]
- Stavrou, V.; Vavougios, G.D.; Bardaka, F.; Karetsi, E.; Daniil, Z.; Gourgoulianis, K.I. The effect of exercise training on the quality of sleep in national-level adolescent finswimmers. Sports Med. Open 2019, 5, 34. [Google Scholar] [CrossRef]
- Pfirrmann, D.; Herbst, M.; Ingelfinger, P.; Simon, P.; Tug, S. Analysis of Injury Incidences in Male Professional Adult and Elite Youth Soccer Players: A Systematic Review. J. Athl. Train. 2016, 51, 410–424. [Google Scholar] [CrossRef] [Green Version]
- Tomlinson, R.E.; Silva, M.J. Skeletal blood flow in bone repair and maintenance. Bone Res. 2013, 1, 311–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonnessen, E.; Hem, E.; Leirstein, S.; Haugen, T.; Seiler, S. Maximal aerobic power characteristics of male professional soccer players, 1989–2012. Int. J. Sports Physiol. Perform. 2013, 8, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Kleisouras, V. Exercise Physiology, 11th ed.; Broken Hill Publishers LTD: Nicosia, Cyprus, 2011; pp. 225–226. [Google Scholar]
- Gąsior, J.S.; Sacha, J.; Jeleń, P.J.; Zieliński, J.; Przybylski, J. Heart Rate and Respiratory Rate Influence on Heart Rate Variability Repeatability: Effects of the Correction for the Prevailing Heart Rate. Front. Physiol. 2016, 7, 356. [Google Scholar] [CrossRef] [Green Version]
- Joo, C.H. The effects of short term detraining and retraining on physical fitness in elite soccer players. PLoS ONE 2018, 10, e0196212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogdanis, G.C. Effects of physical activity and inactivity on muscle fatigue. Front. Physiol. 2012, 3, 142. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.H.; Shin, H.W.; Shin, D.G. Impact of oxidative stress on long-term heart rate variability: Linear versus non-linear heart rate dynamics. Heart Lung Circ. 2019, 10, S1443. [Google Scholar] [CrossRef]
- Olivier, N.; Legrand, R.; Rogez, J.; Berthoin, S.; Weissland, T. Effects of knee surgery on cardiac function in soccer players. Am. J. Phys. Med. Rehabil. LWW 2007, 86, 45–49. [Google Scholar] [CrossRef]
- Tan, D.X.; Manchester, L.C.; Terron, M.P.; Flores, L.J.; Reiter, R.J. One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species? J. Pineal Res. 2007, 42, 28–42. [Google Scholar] [CrossRef]
- Tan, D.X.; Reiter, R.J.; Manchester, L.C.; Yan, M.T.; El-Sawi, M.; Sainz, R.M.; Mayo, J.C.; Kohen, R.; Allegra, M.; Hardeland, R. Chemical and physical properties and potential mechanisms: Melatonin as a broad spectrum antioxidant and free radical scavenger. Curr. Top. Med. Chem. 2002, 2, 181–197. [Google Scholar] [CrossRef] [Green Version]
- Huston, J.M.; Tracey, K.J. The pulse of inflammation: Heart rate variability, the cholinergic anti-inflammatory pathway and implications for therapy. J. Intern. Med. 2011, 269, 45–53. [Google Scholar] [CrossRef]
- Clark, A.; Mach, N. Exercise-induced stress behavior, gut-microbiota-brain axis and diet: A systematic review for athletes. J. Int. Soc. Sports Nutr. 2016, 13, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sloan, R.P.; McCreath, H.; Tracey, K.J.; Sidney, S.; Liu, K.; Seeman, T. RR interval variability is inversely related to inflammatory markers: The CARDIA study. Mol. Med. 2007, 13, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Eaton, D.K.; McKnight-Eily, L.R.; Lowry, R.; Perry, G.S.; Presley-Cantrell, L.; Croft, J.B. Prevalence of insufficient, borderline, and optimal hours of sleep among high school students-United States. J. Adolesc. Health 2010, 46, 399–401. [Google Scholar] [CrossRef] [PubMed]
- Nedelec, M.; Aloulou, A.; Duforez, F.; Meyer, T.; Dupont, G. The variability of sleep among elite athletes. Sports Med. Open 2018, 4, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vitale, J.A.; Weydahl, A. Chronotype, physical activity, and sport performance: A systematic review. Sports Med. 2017, 47, 1859–1868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weger, M.; Diotel, N.; Dorsemans, A.C.; Dickmeis, T.; Weger, B.D. Stem cells and the circadian clock. Dev. Biol. 2017, 431, 111–123. [Google Scholar] [CrossRef]
- Dolezal, B.A.; Neufeld, E.V.; Boland, D.M.; Martin, J.L.; Cooper, C.B. Interrelationship between Sleep and Exercise: A Systematic Review. Adv. Prev. Med. 2017, 2017, 1364387. [Google Scholar]
- Delahanty, D.L. Toward the Predeployment Detection of Risk for PTSD. Am. J. Psychiatry 2011, 168, 9–11. [Google Scholar] [CrossRef]
- Slavich, G.M.; Irwin, M.R. From stress to inflammation and major depressive disorder: A social signal transduction theory of depression. Psychol. Bull. 2014, 140, 774–815. [Google Scholar] [CrossRef]
- Campbell, C.M.; Edwards, R.R. Mind-body interactions in pain: The neurophysiology of anxious and catastrophic pain-related thoughts. Transl. Res. 2009, 153, 97–101. [Google Scholar] [CrossRef] [Green Version]
| Injurygroup (n = 22) | No-Injurygroup (n = 20) | p Value | ||
|---|---|---|---|---|
| Age | years | 21.6 ± 5.4 | 24.2 ± 5.6 | 0.145 |
| Body mass index | kg/m2 | 22.9 ± 1.5 | 22.9 ± 1.7 | 0.947 |
| Body surface area | m2 | 1.8 ± 0.2 | 1.9 ± 0.2 | 0.667 |
| Lean body mass | kg | 58.5 ± 3.8 | 58.9 ± 3.7 | 0.753 |
| Body fat | % | 11.0 ± 3.9 | 10.1 ± 2.8 | 0.415 |
| Total body water | % | 64.0 ± 2.5 | 64.3 ± 1.8 | 0.712 |
| Injuries | ||||
| Lateral/medial of thigh muscles | % | 27 | ||
| Hamstrings muscles | % | 36 | ||
| Dorsal muscles | % | 18 | ||
| Abdominal muscles | % | 18 | ||
| Sit and Reach Test | cm | 44.2 ± 5.0 | 48.2 ± 6.1 | 0.031 |
| Injurygroup (n = 22) | No-Injurygroup (n = 20) | % Differences | p Value | ||
|---|---|---|---|---|---|
| O2 uptake | mL/min/kg | 7.5 ± 1.4 | 5.5 ± 1.2 | 26.3 | <0.001 |
| O2 uptake predicted | mL/min/kg | 8.1 ± 0.2 | 8.0 ± 0.2 | 0.2 | 0.772 |
| O2 uptake | % of predicted | 92.5 ± 17.2 | 68.3 ± 14.6 | 26.2 | <0.001 |
| Heart rate | bpm | 100.6 ± 12.8 | 93.1 ± 4.6 | 10.6 | 0.001 |
| Heart rate | % of predicted | 50.7 ± 6.4 | 47.6 ± 2.8 | 9.3 | 0.003 |
| Injurygroup (n = 22) | no-Injurygroup (n = 20) | p Value | ||
|---|---|---|---|---|
| 1 | When have you usually gone to bed? | 11.4 ± 8.2 | 11.3 ± 9.3 | 0.542 |
| 2 | How long has it taken you to fall asleep each night? | 14.9 ± 10.7 | 15.9 ± 8.9 | 0.748 |
| 3 | What time have you usually gotten up in the morning? | 9.3 ± 1.9 | 9.0 ± 3.3 | 0.719 |
| 4 | How many hours of actual sleep did you get at night? | 7.5 ± 1.2 | 7.5 ± 1.5 | 0.954 |
| 5 | Cannot get to sleep within 30 min | 0.8 ± 1.0 | 1.2 ± 1.1 | 0.322 |
| 6 | Wake up in the middle of the night or early morning | 1.2 ± 0.6 | 0.9 ± 0.4 | 0.091 |
| 7 | Have to get up to use the bathroom | 0.6 ± 0.8 | 0.5 ± 0.8 | 0.588 |
| 8 | Cannot breathe comfortably | 0.5 ± 0.5 | 0.2 ± 0.4 | 0.063 |
| 9 | Cough or snore loudly | 0.3 ± 0.5 | 0.0 ± / | 0.018 |
| 10 | Feel too cold | 0.0 ± 0.2 | 0.0 ± / | 0.013 |
| 11 | Feel too hot | 0.7 ± 1.0 | 0.4 ± 0.8 | 0.199 |
| 12 | Have bad dreams | 0.7 ± 0.7 | 0.0 ± / | <0.001 |
| 13 | Have pain | 0.0 ± 0.2 | 0.1 ± 0.2 | 0.947 |
| 14 | During the past month, how often have you taken medicine to help you sleep? | 0.0 ± 0.0 | 0.1 ± 0.2 | 0.300 |
| 15 | During the past month, how often have you had trouble staying awake while driving, eating meals, or engaging in social activity? | 0.3 ± 0.6 | 0.2 ± 0.4 | 0.405 |
| 16 | During the past month, how much of a problem has it been for you to keep up enthusiasm to get things done? | 0.2 ± 0.4 | 0.5 ± 0.8 | 0.092 |
| 17 | During the past month, how would you rate your sleep quality overall? | 0.9 ± 0.7 | 1.0 ± 0.8 | 0.717 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stavrou, V.T.; Astara, K.; Daniil, Z.; Gourgoulianis, K.I.; Kalabakas, K.; Karagiannis, D.; Basdekis, G. The Reciprocal Association between Fitness Indicators and Sleep Quality in the Context of Recent Sport Injury. Int. J. Environ. Res. Public Health 2020, 17, 4810. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17134810
Stavrou VT, Astara K, Daniil Z, Gourgoulianis KI, Kalabakas K, Karagiannis D, Basdekis G. The Reciprocal Association between Fitness Indicators and Sleep Quality in the Context of Recent Sport Injury. International Journal of Environmental Research and Public Health. 2020; 17(13):4810. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17134810
Chicago/Turabian StyleStavrou, Vasileios T., Kyriaki Astara, Zoe Daniil, Konstantinos I. Gourgoulianis, Konstantinos Kalabakas, Dimitrios Karagiannis, and George Basdekis. 2020. "The Reciprocal Association between Fitness Indicators and Sleep Quality in the Context of Recent Sport Injury" International Journal of Environmental Research and Public Health 17, no. 13: 4810. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17134810






