Adapting Citizen Science to Improve Health in an Occupational Setting: Preliminary Results of a Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
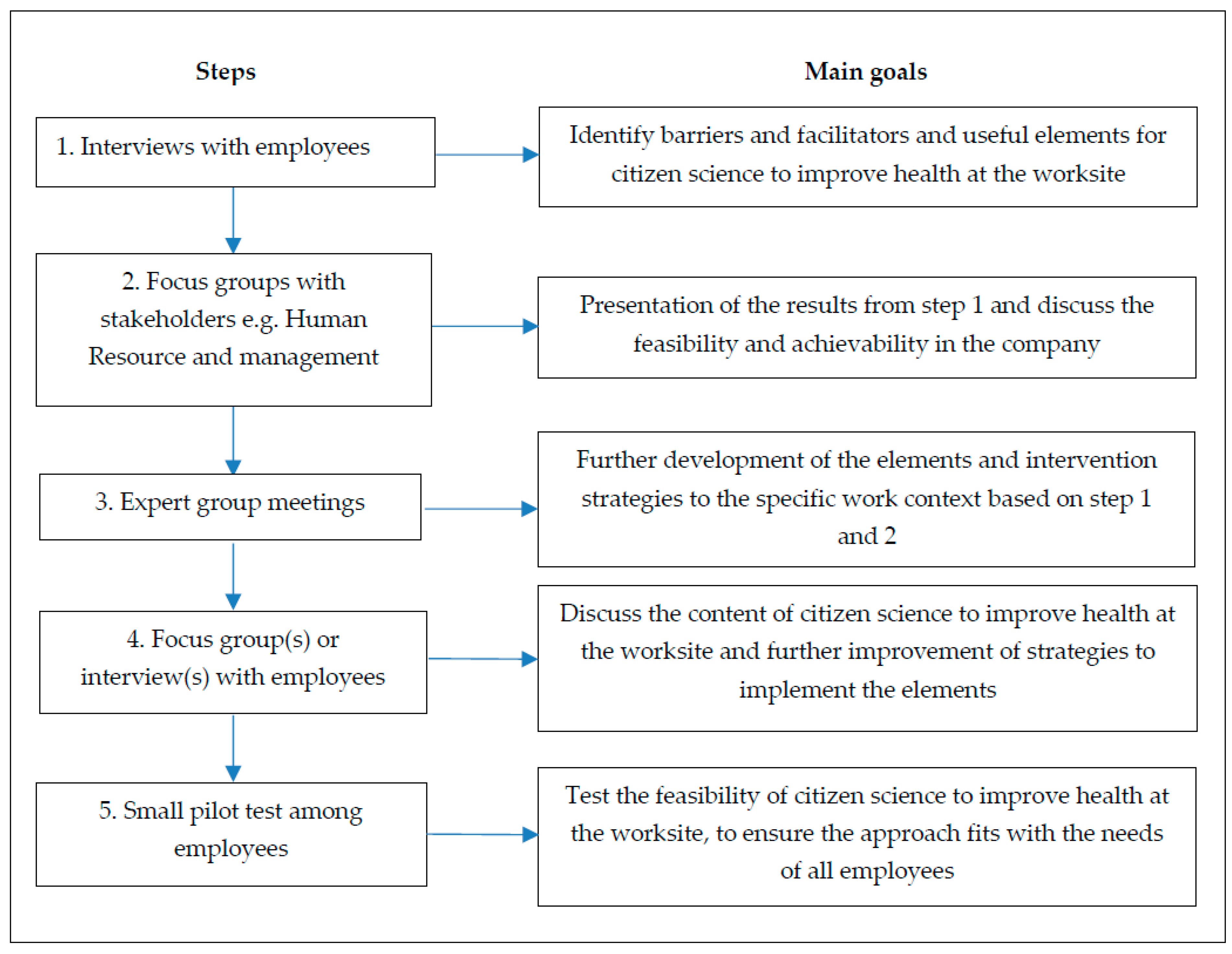
2.1. Study Design
2.2. Participants and Recruitment
2.3. Medical Ethics
2.4. Data Collection
2.4.1. Step 1. Interviews with Employees
2.4.2. Step 2. Focus Groups with Stakeholders
2.4.3. Step 3. Expert Group Meetings
2.4.4. Step 4. Focus Groups with Employees
2.4.5. Step 5. Small Pilot-Tests
2.5. Analysis
3. Results
3.1. Study Population
3.2. Barriers and Facilitating Factors for Citizen Science to Improve Health at the Worksite
3.2.1. Contextual Factors
“As I see it, and speaking from personal experience, construction generally means having to work long hours. The work day starts at 06:45 and often includes a long commute, meaning you have to leave your house at the crack of dawn. The journey back home takes even longer due to traffic jams and the like – it’s exhausting doing that time and time again.”
“Yes. The workload is heavy, and if you want to work in this industry you need to be able to handle that. There are definitely periods that are incredibly busy. Some projects give you enough time to do everything and allow you to properly plan the work on a ship. But more often than not, you’re in a situation where only half of your plan is complete while the ship is already just around the corner. So you know you only have an hour before the work starts. In other words, go, go, go!”
“Well I guess a lot of the guys here have this mentality of ‘I’m not a wuss, just keep powering on’. But if pressed, they’ll admit that they have a backache or some other ailment.”
“Because we always work on big projects. And don’t forget, you guys [researchers] see each other every day – we don’t. For example, I might be working on a project with my colleagues, let’s say, and then be transferred to this project for four months and then to another project after that. This means I might not see my colleagues for 10 years because we are part of such a large organization.”
“And sometimes we had some very difficult colleagues, who were very inflexible and would say ‘I’m not doing such and such’... I think the key, in such a situation, is to use the group to get these people to cooperate. If you have a group of people and a few enthusiastic people those are your sponsors use them to motivate others.”
“Of course, one of the things people say is ‘we never, or hardly ever, see the executives’. This is a difficult dilemma for everyone – including the executives themselves. I don’t think it’s because it’s not important to them – but rather they lack the time and space for visits. These types of things become more difficult and complicated as an organization grows and even more so when you consider that we have several different locations. It just becomes very tricky.”
3.2.2. Personal Factors
“Food and those kinds of things. It’s just easy - especially if it’s not a priority... I think lots of people don’t realize how unhealthy they are until they stop.”
“Yes I have... quite a lot of inflexible colleagues, who are not open to change. I mean, this is a great organization that takes care of everything. But a lot of people find it hard to adapt – they find change difficult.”
3.3. Feasible Elements for Citizen Science to Improve Health at the Worksite
3.3.1. Improve Knowledge and Skills
“You sometimes see those videos about people breathing in dust and then getting serious illnesses so that they can’t live to see their children grow up. That is... well, I had just become a father and then it hits you hard. It makes you stop and think and makes you aware of the risks involved. I think that’s a good thing, but some people think it’s rubbish. But that’s mainly because a lot of people in this industry tend to be quite nonchalant. I think it’s better to be informed of the facts as they are.”
3.3.2. Social Support and Social Culture
“Talking to others makes you realize they are facing the same issues we are. That can happen when talking to an internal staff member or when talking to someone outside the organization but also when you talk to someone... to two internal staff members or to two people from the outside. Everyone has different sleep habits, some people sleep really well and others have a lot of trouble sleeping. I am a good sleeper so I cannot tell someone who is having trouble sleeping what they should do to sleep better.”
3.3.3. Creating Awareness of Lifestyle Behaviors
“Yes, being confronted with the hard facts is an option—telling someone about the horrible diseases they are at risk of developing. But is that really going to help? You don’t really know. It’s probably more helpful for someone to realize that they are not taking good care of themselves or to recognize their unhealthy behaviors, and then feel they would like to do something about that.”
“I think it is much more effective to write down ‘I ate three frikandels (deep-fried sausages) today’ than to keep track of the calories you consumed in an app. I really believe that. Doing that for four weeks straight will give you a real wake-up call.”
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Themes | Codes | Sub Codes |
|---|---|---|
| Barriers for citizen science | - Work environment | - Different worksites/work location - Working hours - Work pressure - Shift work - Physical workload - Other |
| - Social support and social culture | - Employer (Appreciation) - Colleagues/subcontractors - Masculine culture - Different worksites | |
| - Financial resources | - Employer - Employee | |
| - Private life | ||
| - Personal/behavioral factors | - Age - Distrust - Patronized feeling - Shame - Not open for change - Negative attitude - No interest in lifestyle and health - Lack of awareness - Lack of/incorrect risk perception | |
| Facilitators for citizen science | - Work environment | - Shift work |
| - Social support and social culture | - Group feeling - Be heard - Competition - Employer | |
| - Private life/partner | ||
| - Other | - Rewards | |
| Citizen science elements | - Training | - Knowledge and skills lifestyle and health - Create awareness - Better risk perception - Guidance - More openness to change - Goal setting - Narrative story - Support possibilities in lifestyle change employer |
| - Motivational strategies | ||
| - Social support and culture improvement | - Talk about health with colleagues - Be heard by colleagues and employer - More openness to change | |
| - Active involvement/citizen scientists | - Group-based - Barriers (Masculine culture, work pressure, work location, negative attitude) | |
| - More insight in own lifestyle behavior | - Medical screening - Personal diary - Make pictures - Step counter |
References
- Harris, J.R.; Huang, Y.; Hannon, P.A.; Williams, B. Low–socioeconomic status workers: Their health risks and how to reach them. J. Occup. Environ. Med. 2011, 53, 132–138. [Google Scholar] [CrossRef]
- Schreuder, K.; Roelen, C.; Koopmans, P.; Groothoff, J. Job demands and health complaints in white and blue collar workers. Work 2008, 31, 425–432. [Google Scholar] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Viera, A.; Crotty, K.; Holland, A.; Brasure, M.; Lohr, K.N.; Harden, E. Health literacy interventions and outcomes: An updated systematic review. Evid. Rep. Technol. Assess. 2011, 199, 1–941. [Google Scholar]
- Mackenbach, J.P.; Stirbu, I.; Roskam, A.-J.R.; Schaap, M.M.; Menvielle, G.; Leinsalu, M.; Kunst, A.E. Socioeconomic inequalities in health in 22 European countries. N. Engl. J. Med. 2008, 358, 2468–2481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stringhini, S.; Sabia, S.; Shipley, M.; Brunner, E.; Nabi, H.; Kivimaki, M.; Singh-Manoux, A. Association of socioeconomic position with health behaviors and mortality. Jama 2010, 303, 1159–1166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heide, I.v.d.; Rademakers, J.; Schipper, M.; Droomers, M.; Sørensen, K.; Uiters, E. Health literacy of Dutch adults: A cross sectional survey. BMC Public Health 2013, 13, 179. [Google Scholar]
- Alavinia, S.M.; Van Den Berg, T.I.; Van Duivenbooden, C.; Elders, L.A.; Burdorf, A. Impact of work-related factors, lifestyle, and work ability on sickness absence among Dutch construction workers. Scand. J. Work. Health 2009, 35, 325–333. [Google Scholar] [CrossRef] [Green Version]
- Heikkilä, K.; Fransson, E.I.; Nyberg, S.T.; Zins, M.; Westerlund, H.; Westerholm, P.; Virtanen, M.; Vahtera, J.; Suominen, S.; Steptoe, A. Job strain and health-related lifestyle: Findings from an individual-participant meta-analysis of 118 000 working adults. Am. J. Public Health 2013, 103, 2090–2097. [Google Scholar] [CrossRef]
- Andersen, L.L.; Fallentin, N.; Thorsen, S.V.; Holtermann, A. Physical workload and risk of long-term sickness absence in the general working population and among blue-collar workers: Prospective cohort study with register follow-up. Occup. Env. Med 2016, 73, 246–253. [Google Scholar] [CrossRef]
- Dieker, A.C.; IJzelenberg, W.; Proper, K.I.; Burdorf, A.; Ket, J.C.; van der Beek, A.J.; Hulsegge, G. The contribution of work and lifestyle factors to socioeconomic inequalities in self-rated health‒a systematic review. Scand. J. Work. Health 2019, 45, 114–125. [Google Scholar] [CrossRef] [Green Version]
- Coenen, P.; Huysmans, M.A.; Holtermann, A.; Krause, N.; van Mechelen, W.; Straker, L.M.; van der Beek, A.J. Do highly physically active workers die early? A systematic review with meta-analysis of data from 193 696 participants. Br. J. Sports Med. 2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hämmig, O.; Bauer, G.F. The social gradient in work and health: A cross-sectional study exploring the relationship between working conditions and health inequalities. BMC Public Health 2013, 13, 1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mente, A.; de Koning, L.; Shannon, H.S.; Anand, S.S. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch. Intern. Med. 2009, 169, 659–669. [Google Scholar] [CrossRef] [Green Version]
- Goetzel, R.Z.; Henke, R.M.; Tabrizi, M.; Pelletier, K.R.; Loeppke, R.; Ballard, D.W.; Grossmeier, J.; Anderson, D.R.; Yach, D.; Kelly, R.K. Do workplace health promotion (wellness) programs work? J. Occup. Environ. Med. 2014, 56, 927–934. [Google Scholar] [CrossRef] [Green Version]
- Stiehl, E.; Shivaprakash, N.; Thatcher, E.; Ornelas, I.J.; Kneipp, S.; Baron, S.L.; Muramatsu, N. Worksite Health Promotion for Low-Wage Workers: A Scoping Literature Review. Am. J. Health Promot. 2018, 32, 359–373. [Google Scholar] [CrossRef] [Green Version]
- White, M.; Adams, J.; Heywood, P. How and why do interventions that increase health overall widen inequalities within populations. Soc. Inequal. Public Health 2009, 65, 82. [Google Scholar]
- Magnée, T.; Burdorf, A.; Brug, J.; Kremers, S.P.; Oenema, A.; van Assema, P.; Ezendam, N.P.; van Genugten, L.; Hendriksen, I.J.; Hopman-Rock, M. Equity-specific effects of 26 Dutch obesity-related lifestyle interventions. Am. J. Prev. Med. 2013, 44, e61–e70. [Google Scholar] [CrossRef]
- Tonnon, S.C.; Proper, K.I.; van der Ploeg, H.P.; Westerman, M.J.; Sijbesma, E.; van der Beek, A.J. A qualitative study of the anticipated barriers and facilitators to the implementation of a lifestyle intervention in the dutch construction industry. BMC Public Health 2014, 14, 1317. [Google Scholar] [CrossRef]
- Stuber, J.M.; Middel, C.N.; Mackenbach, J.D.; Beulens, J.W.; Lakerveld, J. Successfully Recruiting Adults with a Low Socioeconomic Position into Community-Based Lifestyle Programs: A Qualitative Study on Expert Opinions. Int. J. Environ. Res. Public Health 2020, 17, 2764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van de Ven, D.; Robroek, S.J.; Burdorf, A. Are workplace health promotion programmes effective for all socioeconomic groups? A systematic review. Occup. Environ. Med. 2020. [Google Scholar] [CrossRef]
- Den Broeder, L.; Uiters, E.; Ten Have, W.; Wagemakers, A.; Schuit, A.J. Community participation in Health Impact Assessment. A scoping review of the literature. Environ. Impact Assess. Rev. 2017, 66, 33–42. [Google Scholar] [CrossRef]
- Lingard, H.; Turner, M. Improving the health of male, blue collar construction workers: A social ecological perspective. Constr. Manag. Econ. 2015, 33, 18–34. [Google Scholar] [CrossRef]
- Tsutsumi, A.; Nagami, M.; Yoshikawa, T.; Kogi, K.; Kawakami, N. Participatory intervention for workplace improvements on mental health and job performance among blue-collar workers: A cluster randomized controlled trial. J. Occup. Environ. Med. 2009, 51, 554–563. [Google Scholar] [CrossRef] [PubMed]
- Follett, R.; Strezov, V. An analysis of citizen science based research: Usage and publication patterns. PLoS ONE 2015, 10, e0143687. [Google Scholar] [CrossRef] [Green Version]
- Guerrini, C.J.; Majumder, M.A.; Lewellyn, M.J.; McGuire, A.L. Citizen science, public policy. Science 2018, 361, 134–136. [Google Scholar] [CrossRef]
- Chrisinger, B.W.; Ramos, A.; Shaykis, F.; Martinez, T.; Banchoff, A.W.; Winter, S.J.; King, A.C. Leveraging citizen science for healthier food environments: A pilot study to evaluate corner stores in Camden, New Jersey. Front. Public Health 2018, 6, 89. [Google Scholar] [CrossRef] [Green Version]
- Katapally, T.R.; Bhawra, J.; Leatherdale, S.T.; Ferguson, L.; Longo, J.; Rainham, D.; Larouche, R.; Osgood, N. The SMART study, a mobile health and citizen science methodological platform for active living surveillance, integrated knowledge translation, and policy interventions: Longitudinal study. Jmir Public Health Surveill. 2018, 4, e31. [Google Scholar] [CrossRef]
- Den Broeder, L.; Devilee, J.; Van Oers, H.; Schuit, A.J.; Wagemakers, A. Citizen Science for public health. Health Promot. Int. 2016, 33, 505–514. [Google Scholar] [CrossRef]
- Den Broeder, L.; Lemmens, L.; Uysal, S.; Kauw, K.; Weekenborg, J.; Schönenberger, M.; Klooster-Kwakkelstein, S.; Schoenmakers, M.; Scharwächter, W.; Van de Weerd, A. Public health citizen science; perceived impacts on citizen scientists: A case study in a low-income neighbourhood in the Netherlands. Citiz. Sci. Theory Pract. 2017, 2, 7. [Google Scholar] [CrossRef] [Green Version]
- Winter, S.J.; Rosas, L.G.; Romero, P.P.; Sheats, J.L.; Buman, M.P.; Baker, C.; King, A.C. Using citizen scientists to gather, analyze, and disseminate information about neighborhood features that affect active living. J. Immigr. Minority Health 2016, 18, 1126–1138. [Google Scholar] [CrossRef] [Green Version]
- King, A.C.; Winter, S.J.; Sheats, J.L.; Rosas, L.G.; Buman, M.P.; Salvo, D.; Rodriguez, N.M.; Seguin, R.A.; Moran, M.; Garber, R. Leveraging citizen science and information technology for population physical activity promotion. Transl. J. Am. Coll. Sports Med. 2016, 1, 30. [Google Scholar]
- Consortium, S. Green Paper on Citizen Science: Towards a better Society of Empowered Citizens and Enhanced Research. Brussels: European Commission. 2014. Available online: https://ec.europa.eu/digital-single-market/en/news/green-paper-citizen-science-europe-towards-society-empowered-citizens-and-enhanced-research (accessed on 6 July 2020).
- Hinckson, E.; Schneider, M.; Winter, S.J.; Stone, E.; Puhan, M.; Stathi, A.; Porter, M.M.; Gardiner, P.A.; Dos Santos, D.L.; Wolff, A. Citizen science applied to building healthier community environments: Advancing the field through shared construct and measurement development. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 133. [Google Scholar] [CrossRef] [Green Version]
- Wiggins, A.; Wilbanks, J. The rise of citizen science in health and biomedical research. Am. J. Bioeth. 2019, 19, 3–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shirk, J.L.; Ballard, H.L.; Wilderman, C.C.; Phillips, T.; Wiggins, A.; Jordan, R.; McCallie, E.; Minarchek, M.; Lewenstein, B.V.; Krasny, M.E. Public participation in scientific research: A framework for deliberate design. Ecol. Soc. 2012, 17, 29. [Google Scholar] [CrossRef] [Green Version]
- Wandersman, A. Community science: Bridging the gap between science and practice with community-centered models. Am. J. Community Psychol. 2003, 31, 227–242. [Google Scholar] [CrossRef] [PubMed]
- Du Plessis, K.; Cronin, D.; Corney, T.; Green, E. Australian blue-collar men’s health and well-being: Contextual issues for workplace health promotion interventions. Health Promot. Pract. 2013, 14, 715–720. [Google Scholar] [CrossRef]
- Campbell, N.; Gaston, A.; Gray, C.; Rush, E.; Maddison, R.; Prapavessis, H. The Short QUestionnaire to ASsess Health-enhancing (SQUASH) physical activity in adolescents: A validation using doubly labeled water. J. Phys. Act. Health 2016, 13, 154–158. [Google Scholar] [CrossRef]
- Defuentes-Merillas, L.; Dejong, C.; Schippers, G. Reliability and validity of the Dutch version of the Readiness to Change Questionnaire. Alcohol Alcohol. 2002, 37, 93–99. [Google Scholar] [CrossRef] [Green Version]
- Oenema, A.; Brug, J.; Lechner, L. Web-based tailored nutrition education: Results of a randomized controlled trial. Health Educ. Res. 2001, 16, 647–660. [Google Scholar] [CrossRef] [Green Version]
- Partinen, M.; Gislason, T. Basic Nordic Sleep Questionnaire (BNSQ): A quantitated measure of subjective sleep complaints. J. Sleep Res. 1995, 4, 150–155. [Google Scholar] [CrossRef]
- Van Assema, P.; Brug, J.; Ronda, G.; Steenhuis, I. The relative validity of a short Dutch questionnaire as a means to categorize adults and adolescents to total and saturated fat intake. J. Hum. Nutr. Diet. 2001, 14, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Van den Brink, C.; Ocké, M.; Houben, A.; Van Nierop, P.; Droomers, M. Validering van standaardvraagstelling voeding voor Lokale en Nationale Monitor Volksgezondheid. 2005. Available online: https://www.rivm.nl/publicaties/validering-van-standaardvraagstelling-voeding-voor-lokale-en-nationale-monitor (accessed on 6 July 2020).
- Van der Zee, K.; Sanderman, R. RAND-36. 2012. Available online: https://www.umcg.nl/SiteCollectionDocuments/research/institutes/SHARE/assessment%20tools/handleiding_rand36_2e_druk.pdf (accessed on 6 July 2020).
- Weinstein, N.D.; Rothman, A.J.; Sutton, S.R. Stage theories of health behavior: Conceptual and methodological issues. Health Psychol. 1998, 17, 290. [Google Scholar] [CrossRef] [PubMed]
- Kolmet, M.; Marino, R.; Plummer, D. Anglo-Australian male blue-collar workers discuss gender and health issues. Int. J. Men’s Health 2006, 5, 81–92. [Google Scholar] [CrossRef]
- Michie, S.; Jochelson, K.; Markham, W.A.; Bridle, C. Low-income groups and behaviour change interventions: A review of intervention content, effectiveness and theoretical frameworks. J. Epidemiol. Community Health 2009, 63, 610–622. [Google Scholar] [CrossRef] [Green Version]
- Verdonk, P.; Seesing, H.; De Rijk, A. Doing masculinity, not doing health? A qualitative study among Dutch male employees about health beliefs and workplace physical activity. BMC Public Health 2010, 10, 712. [Google Scholar] [CrossRef] [Green Version]
- Malik, S.H.; Blake, H.; Suggs, L.S. A systematic review of workplace health promotion interventions for increasing physical activity. Br. J. Health Psychol. 2014, 19, 149–180. [Google Scholar] [CrossRef]
- Soler, R.E.; Leeks, K.D.; Razi, S.; Hopkins, D.P.; Griffith, M.; Aten, A.; Chattopadhyay, S.K.; Smith, S.C.; Habarta, N.; Goetzel, R.Z. A systematic review of selected interventions for worksite health promotion: The assessment of health risks with feedback. Am. J. Prev. Med. 2010, 38, S237–S262. [Google Scholar] [CrossRef]
- Nielsen, K.; Fredslund, H.; Christensen, K.B.; Albertsen, K. Success or failure? Interpreting and understanding the impact of interventions in four similar worksites. Work Stress 2006, 20, 272–287. [Google Scholar] [CrossRef]
- Goldgruber, J.; Ahrens, D. Effectiveness of workplace health promotion and primary prevention interventions: A review. J. Public Health 2010, 18, 75–88. [Google Scholar] [CrossRef] [Green Version]

| Category | Factors | Construction Company | Terminal Company |
|---|---|---|---|
| Context | Work location | Barrier | Barrier |
| Work pressure | Barrier | Barrier | |
| Shift work | Not applicable | Barrier/Facilitator | |
| (Lack of) social support and (negative) social culture | Barrier/Facilitator | Barrier/Facilitator | |
| Personal | Lack of openness for change | Barrier | Barrier |
| Lack of/incorrect risk perception | Barrier | Barrier | |
| Negative attitude | Barrier | Barrier | |
| Lack of awareness | Barrier | Barrier |
| Citizen Science Element | Targeted Barriers/Facilitators | Strategies to Implement the Element | Included in |
|---|---|---|---|
| Improve knowledge and skills to improve lifestyle and health | Lack of/incorrect risk perception, lack of openness for change, lack of awareness, negative attitude | Content focused on lifestyle factors, mainly physical activity and dietary behavior, during shift work | T 1 |
| Content focused on physical activity during work and leisure time and dietary behavior in a physically demanding job | C 2 | ||
| Information provided on employee specific factsheets | C | ||
| Information provided in a booklet | T | ||
| Work location, work pressure | Short, repetitive meetings during working hours | C/T | |
| Lack of/incorrect risk perception, lack of openness for change, lack of awareness, negative attitude, work location, work pressure | Recurrent reminders of health messages via screens at the worksite | C | |
| Recurrent and reminder of health messages via e-mail or SMS | T | ||
| (Lack of) social support and negative social culture | Interactive meetings | C/T | |
| Lack of/incorrect risk perception, lack of awareness, negative attitude, lack of openness for change | Narrative storytelling (a short video of an employee telling his personal story) | C | |
| Lack of/incorrect risk perception, lack of openness for change, lack of awareness | Personal goal setting | C/T | |
| (Lack of) social support and negative social culture, lack of awareness, negative attitude | Performing exercises during meetings | C | |
| Improve social support and social culture | (Lack of) social support employees and negative social culture | Interactive, small group meetings with employees | C/T |
| (Lack of) social support from the employer | Meetings facilitated by the prevention team and management of the company | C | |
| Providing a step counter | T | ||
| (Lack of) social support, negative attitude, lack of openness for change, lack of awareness | Collect and discuss ideas on how to improve health at the worksite | C/T | |
| Active role in the decision-making process | C/T | ||
| (Lack of) social support employees | Additional training of citizen scientists | T | |
| Create awareness of lifestyle behavior | Lack of awareness, lack of/incorrect risk perception, negative attitude | Collect personal data on lifestyles (photos/videos) | C |
| Collect personal data on lifestyle by keeping a diary and a step counter | T |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van den Berge, M.; Hulsegge, G.; van der Molen, H.F.; Proper, K.I.; Pasman, H.R.W.; den Broeder, L.; Tamminga, S.J.; Hulshof, C.T.J.; van der Beek, A.J. Adapting Citizen Science to Improve Health in an Occupational Setting: Preliminary Results of a Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 4917. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17144917
van den Berge M, Hulsegge G, van der Molen HF, Proper KI, Pasman HRW, den Broeder L, Tamminga SJ, Hulshof CTJ, van der Beek AJ. Adapting Citizen Science to Improve Health in an Occupational Setting: Preliminary Results of a Qualitative Study. International Journal of Environmental Research and Public Health. 2020; 17(14):4917. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17144917
Chicago/Turabian Stylevan den Berge, Mandy, Gerben Hulsegge, Henk F. van der Molen, Karin I. Proper, H. Roeline W. Pasman, Lea den Broeder, Sietske J. Tamminga, Carel T. J. Hulshof, and Allard J. van der Beek. 2020. "Adapting Citizen Science to Improve Health in an Occupational Setting: Preliminary Results of a Qualitative Study" International Journal of Environmental Research and Public Health 17, no. 14: 4917. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17144917







