Exercise, Comorbidities, and Health-Related Quality of Life in People Living with HIV: The HIBES Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Participant and Public Involvement
2.3. Recruitment
2.4. Definitions
2.5. Data Collection and Measures
2.6. Data Analysis
2.7. Statistical Analysis
3. Results
3.1. Exercise Compared to Other Covariates
3.1.1. HRQOL Parameters
3.1.2. Covariates Affecting Each Other
3.1.3. HRQOL Covariates
3.1.4. Exercise and its Effects on HRQOL
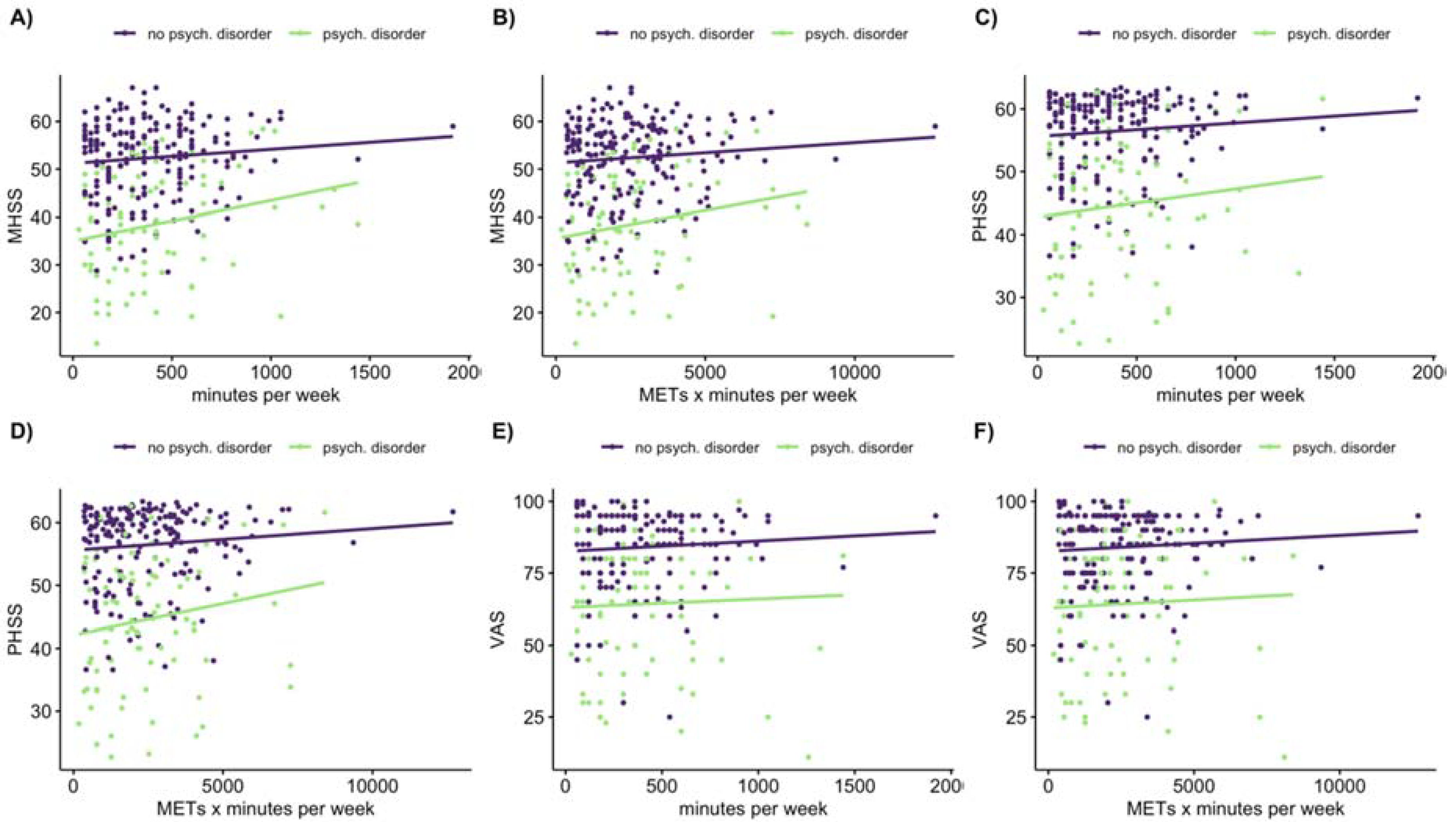
3.2. Linear Regression
4. Discussion
4.1. Comparison of Exercise and No-Exercise on HRQOL
4.2. Association of Exercise and HRQOL
4.3. HRQOL Scales
4.4. Implications
4.5. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Parameter | MHSS | PHSS | Index Value | VAS | ||||
|---|---|---|---|---|---|---|---|---|
| F(df, 448) | Eta Sq. | F(df, 448) | Eta Sq. | F(df, 441) | Eta Sq. | F(df, 443) | Eta Sq. | |
| Exercise (df = 1) | 24.72 * | 0.024 | 38.53 * | 0.034 | 18.35 * | 0.017 | 31.43 * | 0.033 |
| CDC-stage (df = 2) | 19.64 * | 0.004 | 51.78 * | 0.047 | 38.68 * | 0.048 | 34.23 * | 0.035 |
| Psychological (df = 1) | 118.87 * | 0.188 | 93.85 * | 0.1372 | 53.10 * | 0.09 | 63.49 * | 0.105 |
| Parameter | Exercise | CTE | STE | Effect Size |
|---|---|---|---|---|
| n = 288 | n = 147 | n = 141 | ||
| Session/week | 4 (2.3) | 5 (4) * | 3 (2) | 0.613 |
| Minutes/week | 360 (360) | 540 (300) * | 180 (180) | 0.657 |
| METS × minutes/week | 2100 (2193) | 3240 (1950) * | 1170 (1245) | 0.635 |
References
- Deeks, S.G.; Lewin, S.R.; Havlir, D.V. The end of AIDS: HIV infection as a chronic disease. Lancet 2013, 382, 1525–1533. [Google Scholar] [CrossRef] [Green Version]
- Koch-Institut, R. Epidemiologisches Bulletin 46/2019. Available online: https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2019/Ausgaben/46_19.pdf;jsessionid=3149F1E749EEAFD4E5215C4CA1E25C89.internet052?__blob=publicationFile (accessed on 22 November 2019).
- Engelhard, E.A.N.; Smit, C.; van Dijk, P.R.; Kuijper, T.M.; Wermeling, P.R.; Weel, A.E.; de Boer, M.R.; Brinkman, K.; Geerlings, S.E.; Nieuwkerk, P.T. Health-related quality of life of people with HIV: An assessment of patient related factors and comparison with other chronic diseases. AIDS 2018, 32, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Miners, A.; Phillips, A.; Kreif, N.; Rodger, A.; Speakman, A.; Fisher, M.; Anderson, J.; Collins, S.; Hart, G.; Sherr, L.; et al. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: A cross-sectional comparison with the general population. Lancet HIV 2014, 1, e32–e40. [Google Scholar] [CrossRef] [Green Version]
- Maciel, R.A.; Klück, H.M.; Durand, M.; Sprinz, E. Comorbidity is more common and occurs earlier in persons living with HIV than in HIV-uninfected matched controls, aged 50 years and older: A cross-sectional study. Int. J. Infect. Dis. 2018, 70, 30–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christensen, S.; Wolf, E.; Altevers, J.; Diaz-Cuervo, H. Comorbidities and costs in HIV patients: A retrospective claims database analysis in Germany. PLoS ONE 2019, 14, e0224279. [Google Scholar] [CrossRef] [PubMed]
- Gallant, J.; Hsue, P.Y.; Shreay, S.; Meyer, N. Comorbidities among US patients with prevalent HIV infection—A trend analysis. J. Infect. Dis. 2017. [Google Scholar] [CrossRef]
- O’Brien, K.K.; Tynan, A.-M.; Nixon, S.A.; Glazier, R.H. Effectiveness of Progressive Resistive Exercise (PRE) in the context of HIV: Systematic review and meta-analysis using the Cochrane Collaboration protocol. BMC Infect. Dis. 2017, 17. [Google Scholar] [CrossRef]
- Poton, R.; Polito, M.; Farinatti, P. Effects of resistance training in HIV-infected patients: A meta-analysis of randomised controlled trials. J. Sports Sci. 2017, 35, 2380–2389. [Google Scholar] [CrossRef]
- Gomes Neto, M.; Conceição, C.S.; Carvalho, V.O.; Brites, C. Effects of combined aerobic and resistance exercise on exercise capacity, muscle strength and quality of life in HIV-infected patients: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0138066. [Google Scholar] [CrossRef] [Green Version]
- Pérez Chaparro, C.G.A.; Zech, P.; Schuch, F.; Wolfarth, B.; Rapp, M.; Heiβel, A. Effects of aerobic and resistance exercise alone or combined on strength and hormone outcomes for people living with HIV. A meta-analysis. PLoS ONE 2018, 13, e0203384. [Google Scholar] [CrossRef]
- Zech, P.; Pérez-Chaparro, C.; Schuch, F.; Wolfarth, B.; Rapp, M.; Heissel, A. Effects of aerobic and resistance exercise on cardiovascular parameters for people living with HIV. J. Assoc. Nurses AIDS Care 2019, 30, 186–205. [Google Scholar] [CrossRef]
- Fillipas, S.; Cherry, C.L.; Cicuttini, F.; Smirneos, L.; Holland, A.E. The effects of exercise training on metabolic and morphological outcomes for people living with HIV: A systematic review of randomised controlled trials. HIV Clin. Trials 2010, 11, 270–282. [Google Scholar] [CrossRef] [PubMed]
- Heissel, A.; Zech, P.; Rapp, M.A.; Schuch, F.B.; Lawrence, J.B.; Kangas, M.; Heinzel, S. Effects of exercise on depression and anxiety in persons living with HIV: A meta-analysis. J. Psychosom. Res. 2019, 126, 109823. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Recommendations on Physical Activity for Health; WHO: Geneva, Switzerland, 2010; pp. 24–27. ISBN 978-92-4-159997-9. [Google Scholar]
- Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short and Long Forms 2005. Available online: www.ipaq.ki.se (accessed on 28 May 2020).
- Leavitt, M.O. 2008 U.S. Department of Health and Human Services, Physical Activity Guidelines for Americans. 2008; p. 55. Available online: www.health.gov/paguidlines (accessed on 28 May 2020).
- George, S.; Bergin, C.; Clarke, S.; Courtney, G.; Codd, M.B. Health-related quality of life and associated factors in people with HIV: An Irish cohort study. Health Qual. Life Outcomes 2016, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghiasvand, H.; Waye, K.M.; Noroozi, M.; Harouni, G.G.; Armoon, B.; Bayani, A. Clinical determinants associated with quality of life for people who live with HIV/AIDS: A Meta-analysis. BMC Health Serv. Res. 2019, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rugg, C.; Kadoor, A.; Feeley, B.T.; Pandya, N.K. The effects of playing multiple high school sports on national basketball association players’ propensity for injury and athletic performance. Am. J. Sports Med. 2018, 46, 402–408. [Google Scholar] [CrossRef]
- Buckley, P.S.; Bishop, M.; Kane, P.; Ciccotti, M.C.; Selverian, S.; Exume, D.; Emper, W.; Freedman, K.B.; Hammoud, S.; Cohen, S.B.; et al. Early single-sport specialization: A survey of 3090 high school, collegiate, and professional athletes. Orthop. J. Sports Med. 2017, 5, 232596711770394. [Google Scholar] [CrossRef] [Green Version]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126. [Google Scholar] [PubMed]
- Pollock, M.L.; Gaesser, G.A.; Butcher, J.D.; Després, J.P.; Dishman, R.K.; Franklin, B.A.; Garber, C.E. ACSM position stand: The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med. Sci. Sports Exerc. 1998, 30, 975–991. [Google Scholar] [CrossRef]
- Wu, A.W. MOS-HIV Health Survey Users Manual. Available online: https://eprovide.mapi-trust.org/instruments/medical-outcome-study-hiv-health-survey, (accessed on 10 June 2019).
- Revicki, D.A.; Sorensen, S.; Wu, A.W. Reliability and validity of physical and mental health summary scores from the medical outcomes study HIV health survey. Med. Care 1998, 36, 126–137. [Google Scholar] [CrossRef]
- Tran, B.; Ohinmaa, A.; Nguyen, L. Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. Health Qual. Life Outcomes 2012, 10, 132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Reene, M.; Janssen, B. EQ-5D-5L User Guide, Basic Information on How to Use the EQ-5D-5L Instrument, Version 2.1; EuroQol Research Foundation: Rotterdam, The Netherlands, 2015. [Google Scholar]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.F.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahriar, J.; Delate, T.; Hays, R.D.; Coons, S.J. Commentary on using the SF-36 or MOS-HIV in studies of persons with HIV disease. Health Qual. Life Outcomes 2003, 7, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinz, A.; Kohlmann, T.; Stöbel-Richter, Y.; Zenger, M.; Brähler, E. The quality of life questionnaire EQ-5D-5L: Psychometric properties and normative values for the general German population. Qual. Life Res. 2014, 23, 443–447. [Google Scholar] [CrossRef]
- Ainsworth, B.; Haskell, W.; Herrmann, S.; Meckes, N.; Basset Jr., D.; Tudor-Locke, C.; Greer, J.; Vezina, J.; Whitt-Glover, M.; Leon, A. 2011 compendium of physical activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef] [Green Version]
- Revelle, W. Procedures for Psychological, Psychometric, and Personality Research. 2018. Available online: https://CRAN.R-project.org/package=psych (accessed on 15 May 2020).
- R Core Team. R: A Language and Environment for Statistical Computing. 2019. Available online: https://www.gbif.org/tool/81287/r-a-language-and-environment-for-statistical-computing (accessed on 15 May 2020).
- Wickham, H.; Francois, R.; Henry, B.L.; Müller, K. DPLYR: A Grammar of Data Manipulation. 2019. Available online: https://CRAN.R-project.org/package=dplyr (accessed on 15 May 2020).
- Fox, J.; Weisberg, S. An R Companion to Applied Regression; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2019. [Google Scholar]
- Venables, W.N.; Ripley, B.D. Modern Applied Statistics with S, 4th ed.; Springer: New York, NY, USA, 2002; ISBN 0-387-95457-0. [Google Scholar]
- Kassambara, A. GGPUBR: “GGPLOT’’ Based Publication Ready Plots. R Package Version 0.3.0. Available online: https://CRAN.R-project.org/package=ggpubr (accessed on 15 May 2020).
- European Commission. Special Eurobarometer 412 “Sport and Physical Activity”; European Commission: Brussels, Belgium, 2014; ISBN 978-92-79-36836-3. [Google Scholar]
- Stein, L.; Hechler, D.; Jessen, A.B.; Neumann, K.; Jessen, H.; Beneke, R. Sports behaviour among HIV-infected versus non-infected individuals in a Berlin cohort. Int. J. STD AIDS 2012, 23, 25–29. [Google Scholar] [CrossRef]
- Dufour, C.A.; Marquine, M.J.; Fazeli, P.L.; Umlauf, A.; Henry, B.L.; Zlatar, Z.; Montoya, J.L.; Ellis, R.J.; Grant, I.; Moore, D.J. A longitudinal analysis of the impact of physical activity on neurocognitive functioning among HIV-infected adults. AIDS Behav. 2018, 22, 1562–1572. [Google Scholar] [CrossRef]
- Fillipas, S.; Cicuttini, F.; Holland, A.; Cherry, C. Physical activity particpation and cardiovascular fitness in people leaving with HIV. A one-year longitudinal study. Retrovirology 2012, 9. [Google Scholar] [CrossRef] [Green Version]
- Kiloor, A.; Sonykumari, A.K.; Metri, K. Impact of yoga on psychopathologies and QoLin persons with HIV: A randomized controlled study. J. Bodyw. Mov. Ther. 2018. [Google Scholar] [CrossRef]
- Anandh, V.; Alagesan, J. Effect of aerobicand progressive resistance training on functional capacity, quality of life and CD4 count in people with HIV/AIDS. Glob. J. Res. Anal. 2014, 3, 226–231. [Google Scholar] [CrossRef]
- Agin, D.; Gallagher, D.; Wang, J.; Heymsfield, S.B.; Pierson, R.N., Jr.; Kotler, D.P. Effects of whey protein and resistance exercise on body cell mass, muscle strength, and quality of life in women with HIV. AIDS 2001, 15, 2431–2440. [Google Scholar] [CrossRef] [PubMed]
- Baigis, J.; Korniewicz, D.M.; Chase, G.; Butz, A.; Jacobson, D.; Wu, A.W. Effectiveness of a home-based exercise intervention for HIV-infected adults: A randomized trial. J. Assoc. Nurses AIDS Care 2002, 13, 33–45. [Google Scholar] [CrossRef]
- Martin, K.; Naclerio, F.; Karsten, B.; Vera, J.H. Physical activity and quality of life in people living with HIV. AIDS Care 2019, 31, 589–598. [Google Scholar] [CrossRef]
- Peleias, M.; Tempski, P.; Paro, H.B.; Perotta, B.; Mayer, F.B.; Enns, S.C.; Gannam, S.; Pereira, M.A.D.; Silveira, P.S.; Santos, I.S.; et al. Leisure time physical activity and quality of life in medical students: Results from a multicentre study. BMJ Open Sport Exerc. Med. 2017, 3, e000213. [Google Scholar] [CrossRef]
- Worthington, C.; Krentz, H.B. Socio-economic factors and health-related quality of life in adults living with HIV. Int. J. STD AIDS 2005, 16, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Millar, B.M.; Starks, T.J.; Gurung, S.; Parsons, J.T. The impact of comorbidities, depression, and substance use problems on quality of life among older adults living with HIV. AIDS Behav. 2017, 21, 1684–1690. [Google Scholar] [CrossRef] [PubMed]


| Parameter | Non-Exercise | Exercise | CTE | STE |
|---|---|---|---|---|
| n = 166 | n = 288 | n = 141 | n = 147 | |
| Female, n (%) | 21 (12.7) | 13 (4.5) * | 5 (3.5) | 8 (5.4) |
| Male, n (%) | 143 (86.1) | 275 (95.5) * | 136 (96.5) | 139 (94.6) |
| Other, n (%) | 2 (1.2) | 0 (0) | - | - |
| Age (yrs.) | 46 (12) | 43 (13) * | 43 (13) | 43 (13) |
| Height (cm) | 178 (10.8) | 180 (10) | 180 (9) | 180 (11) |
| Weight (kg) | 75 (17.8) | 78 (12) | 78 (13) | 78 (12) |
| BMI (kg/m2) | 23.3 (5) | 23.7 (3.8) | 23.6 (3.9) | 23.7 (3.8) |
| Residential area | ||||
| <100,000 citizens, n (%) | 31 (18.7) | 58 (20.1) | 31 (22) | 27 (18.4) |
| 100,000–500,000 citizens, n (%) | 24 (14.5) | 42 (14.6) | 22 (15.6) | 20 (13.6) |
| >500,000 citizens, n (%) | 111 (66.9) | 188 (65.3) | 88 (62.4) | 100 (68) |
| Years with HIV (yrs.) | 8 (10) | 7 (11) | 7 (11) | 8 (11) |
| Year of diagnosis > 1990 | 151 (90.9) | 266 (92.4) | 133 (94.3) | 133 (90.5) |
| Year of diagnosis ≤ 1990 | 15 (9.1) | 22 (7.6) | 8 (5.7) | 14 (9.5) |
| Years with ART (yrs.) | 6 (9) | 5 (10) | 5 (10) | 5 (10) |
| CD4 cell count (cell·µL−1) | 600 (330.3) | 640 (255.5) | 619 (229.5) | 650 (336.5) |
| Cardiovascular disease, n (%) | 32 (19.3) | 40 (13.9) | 17 (12.1) | 23 (15.6) |
| Metabolic disease, n (%) | 52 (31.3) | 49 (17) * | 25 (17.7) | 24 (16.3) |
| Psychological disorder, n (%) | 61 (36.7) | 85 (29.5) | 40 (28.4) | 45 (30.6) |
| HRQOL | Value | Estimate (±SE) | Standardized | t | p | R2 | Partial R2 |
|---|---|---|---|---|---|---|---|
| Multiple regression—all exercisers | |||||||
| MHSS | Intercept | 50.46 (±0.97) | 52.05 | 0.000 | |||
| Minutes (slope) | 4.86 (±1.89) | 0.12 | 2.57 | 0.011 | 0.344 | 0.023 | |
| Psych. Disorder | −14.00 (±1.17) | −0.58 | −12.00 | 0.000 | |||
| MHSS | Intercept | 50.72 (±0.97) | 52.45 | 0.000 | |||
| MMW (slope) | 0.66 (±0.30) | 0.11 | 2.22 | 0.027 | 0.340 | 0.017 | |
| Psych. Disorder | −13.92 (±1.17) | −0.57 | −11.91 | 0.000 | |||
| PHSS | Intercept | 55.32 (±0.84) | 66.00 | 0.000 | |||
| Minutes (slope) | 2.91 (±1.65) | 0.09 | 1.77 | 0.079 | 0.338 | 0.011 | |
| Psych. Disorder | −11.93 (±1.00) | −0.58 | −11.92 | 0.000 | |||
| PHSS | Intercept | 55.13 (±0.83) | 66.22 | 0.000 | |||
| MMW (slope) | 0.54 (±0.26) | 0.10 | 2.08 | 0.038 | 0.341 | 0.015 | |
| Psych. Disorder | −11.89 (±1.00) | −0.58 | −11.90 | 0.000 | |||
| VAS | Intercept | 81–64 (±1.74) | 46.97 | 0.000 | |||
| Minutes (slope) | 6.79 (±3.40) | 0.10 | 2.00 | 0.047 | 0.263 | 0.014 | |
| Psych. Disorder | −20.27 (±2.07) | −0.50 | −9.78 | 0.000 | |||
| VAS | Intercept | 81.57 (±1.73) | 47.11 | 0.000 | |||
| MMW (slope) | 1.10 (±0.53) | 0.11 | 2.06 | 0.040 | 0.263 | 0.015 | |
| Psych. Disorder | −20.16 (±2.07) | −0.50 | −9.73 | 0.000 | |||
| Simple regression—exercisers with a psychological disorder | |||||||
| MHSS | Intercept | 35.04 (±1.92) | 18.25 | 0.000 | |||
| Minutes (slope) | 9.72 (±3.80) | 0.28 | 2.56 | 0.012 | 0.08 | ||
| MHSS | Intercept | 35.44 (±1.94) | 18.27 | 0.000 | |||
| MMW (slope) | 1.44 (±0.63) | 0.25 | 2.28 | 0.026 | 0.06 | ||
| PHSS | Intercept | 42.39 (±1.94) | 21.81 | 0.000 | |||
| Minutes (slope) | 6.56 (±4.05) | 0.18 | 1.62 | 0.11 | 0.03 | ||
| PHSS | Intercept | 41.80 (±1.91) | 21.91 | 0.000 | |||
| MMW (slope) | 1.32 (±0.65) | 0.22 | 2.03 | 0.045 | 0.05 | ||
| VAS | Intercept | 56.29 (±3.90) | 14.27 | 0.000 | |||
| Minutes (slope) | 23.75 (±8.47) | 0.30 | 2.80 | 0.006 | 0.09 | ||
| VAS | Intercept | 55.30 (±3.89) | 14.20 | 0.000 | |||
| MMW (slope) | 4.34 (±1.38) | 0.34 | 3.15 | 0.002 | 0.11 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zech, P.; Schuch, F.; Pérez-Chaparro, C.; Kangas, M.; Rapp, M.; Heissel, A. Exercise, Comorbidities, and Health-Related Quality of Life in People Living with HIV: The HIBES Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 5138. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145138
Zech P, Schuch F, Pérez-Chaparro C, Kangas M, Rapp M, Heissel A. Exercise, Comorbidities, and Health-Related Quality of Life in People Living with HIV: The HIBES Cohort Study. International Journal of Environmental Research and Public Health. 2020; 17(14):5138. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145138
Chicago/Turabian StyleZech, Philipp, Felipe Schuch, Camilo Pérez-Chaparro, Maria Kangas, Michael Rapp, and Andreas Heissel. 2020. "Exercise, Comorbidities, and Health-Related Quality of Life in People Living with HIV: The HIBES Cohort Study" International Journal of Environmental Research and Public Health 17, no. 14: 5138. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145138





