Attitudes of the Public to Receiving Medical Care during Emergencies through Remote Physician–Patient Communications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Procedures
2.3. Instrument
2.4. Statistical Methods
2.5. Ethical Aspects
3. Results
3.1. Descriptive Analysis
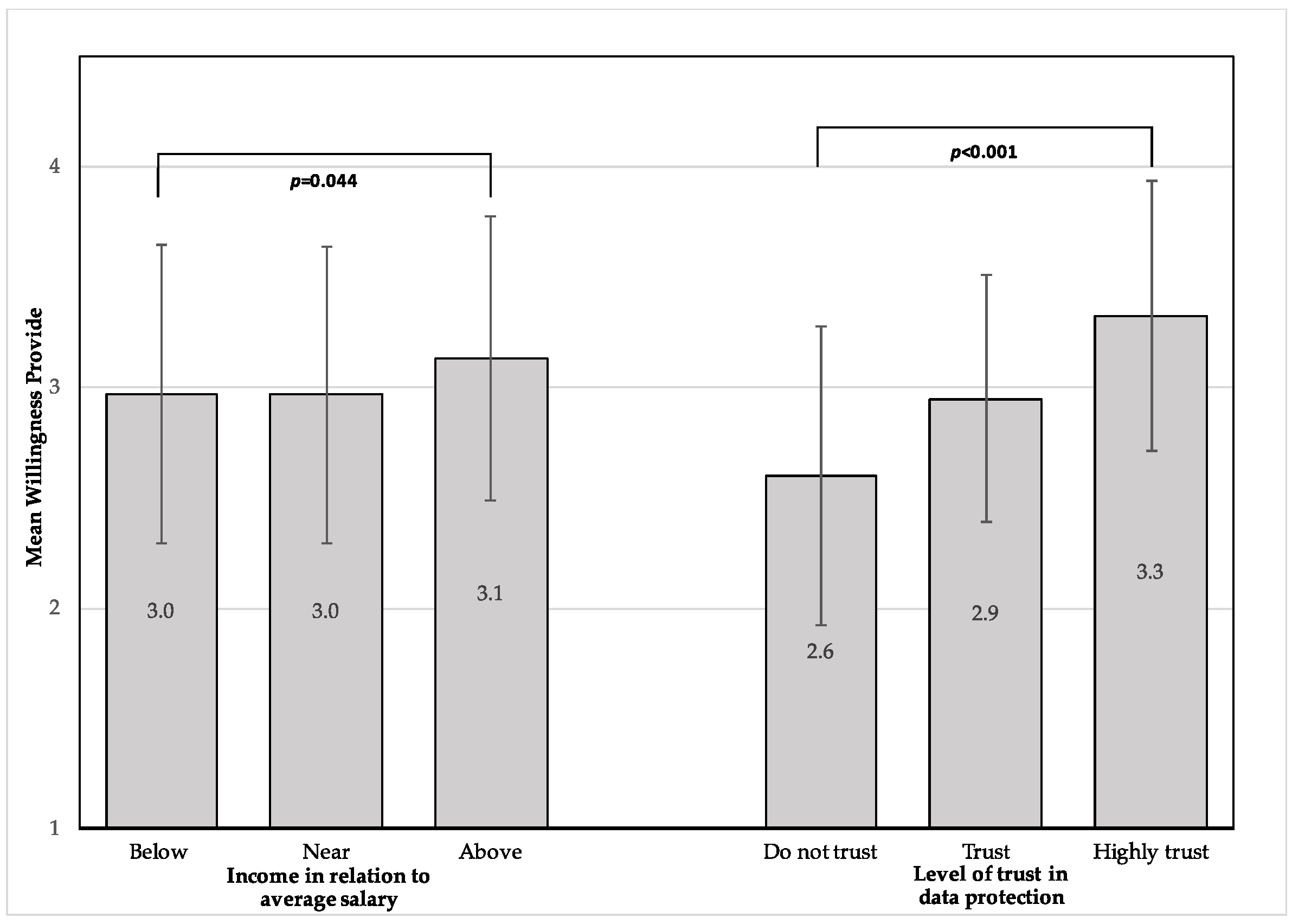
3.2. Differences in Mean Willingness to Receive and Provide Medical Services/Information
3.3. Correlations between Willingness to Receive or Provide Medical Services/Information and Other Variables
3.4. Linear Regression Model
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Moon, S.; Sridhar, D.; Pate, M.A.; Jha, A.K.; Clinton, C.; Delaunay, S.; Edwin, V.; Fallah, M.; Fidler, D.P.; Garrett, L.; et al. Will Ebola change the game? Ten essential reforms before the next pandemic. The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Lancet 2015, 386, 2204–2221. [Google Scholar] [CrossRef] [Green Version]
- Deng, S.Q.; Peng, H.J. Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China. J. Clin. Med. 2020, 9, 575. [Google Scholar] [CrossRef] [Green Version]
- Guarner, J. Three Emerging Coronaviruses in Two Decades. Am. J. Clin. Pathol. 2020, 153, 420–421. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Disease (COVID-19) Situation Report—105. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200504-covid-19-sitrep-105.pdf?sfvrsn=4cdda8af_2 (accessed on 5 May 2020).
- Ferguson, N.M.; Cummings, D.A.T.; Cauchemez, S.; Fraser, C.; Riley, S.; Meeyai, A.; Iamsirithaworn, S.; Burke, D.S. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature 2005, 437, 209–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, S.Y.; Kang, J.-M.; Ha, Y.E.; Park, G.E.; Lee, J.Y.; Ko, J.-H.; Lee, J.Y.; Kim, J.M.; Kang, C.-I.; Jo, I.J.; et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: An epidemiological outbreak study. Lancet 2016, 388, 994–1001. [Google Scholar] [CrossRef]
- Levin, P.J.; Gebbie, E.N.; Qureshi, K. Can the health-care system meet the challenge of pandemic flu? Planning, ethical, and workforce considerations. Public Health Rep. 2007, 122, 573–578. [Google Scholar] [CrossRef]
- Zhang, J.; Zhou, L.; Yang, Y.; Peng, W.; Wang, W.; Chen, X. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir. Med. 2020, 8, e11–e12. [Google Scholar] [CrossRef] [Green Version]
- Bostick, N.A.; Levine, M.A.; Sade, R.M. Ethical obligations of physicians participating in public health quarantine and isolation measures. Public Health Rep. 2008, 123, 3–8. [Google Scholar] [CrossRef] [Green Version]
- Rhoads, S.J.; Bush, E.; Haselow, D.; Vyas, K.S.; Wheeler, J.G.; Faulkner, A.; Lowery, C. Mobilizing a Statewide Network to Provide Ebola Education and Support. Telemed. J. e-Health 2016, 22, 153–158. [Google Scholar] [CrossRef] [PubMed]
- North, F.; Varkey, P.; Bartel, G.A.; Cox, D.L.; Jensen, P.L.; Stroebel, R.J. Can an office practice telephonic response meet the needs of a pandemic? Telemed. J. e-Health 2010, 16, 1012–1016. [Google Scholar] [CrossRef] [PubMed]
- Latifi, R.; Tilley, E.H. Telemedicine for disaster management: Can it transform chaos into an organized, structured care from the distance? Am. J. Disaster Med. 2014, 9, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Telemedicine Glossary. Available online: https://thesource.americantelemed.org/resources/telemedicine-glossary (accessed on 24 February 2020).
- Telehealth. Available online: https://www.who.int/sustainable-development/health-sector/strategies/telehealth/en/ (accessed on 24 February 2020).
- Donelan, K.; Barreto, E.A.; Sossong, S.; Michael, C.; Estrada, J.J.; Cohen, A.B.; Wozniak, J.; Schwamm, L.H. Patient and clinician experiences with telehealth for patient follow-up care. Am. J. Manag. Care 2019, 25, 40–44. [Google Scholar]
- Konttila, J.; Siira, H.; Kyngäs, H.; Lahtinen, M.; Elo, S.; Kääriäinen, M.; Kaakinen, P.; Oikarinen, A.; Yamakawa, M.; Fukui, S.; et al. Healthcare professionals’ competence in digitalisation: A systematic review. J. Clin. Nurs. 2019, 28, 745–761. [Google Scholar] [CrossRef]
- Emerson, J.F.; Welch, M.; Rossman, W.E.; Carek, S.; Ludden, T.; Templin, M.; Moore, C.G.; Tapp, H.; Dulin, M.; McWilliams, A. A Multidisciplinary Intervention Utilizing Virtual Communication Tools to Reduce Health Disparities: A Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2015, 13, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holt, G.R. Making difficult ethical decisions in patient care during natural disasters and other mass casualty events. Otolaryngol. Head Neck Surg. 2008, 139, 181–186. [Google Scholar] [CrossRef]
- Klein, K.R.; Pepe, P.E.; Burkle, F.M., Jr.; Nagel, N.E.; Swienton, R.E. Evolving need for alternative triage management in public health emergencies: A Hurricane Katrina case study. Disaster Med. Public Health Prep. 2008, 2, s40–s44. [Google Scholar] [CrossRef]
- Garshnek, V.; Burkle, F.M., Jr. Telecommunications systems in support of disaster medicine: Applications of basic information pathways. Ann. Emerg. Med. 1999, 34, 213–218. [Google Scholar] [CrossRef]
- Uscher-Pines, L.; Fischer, S.; Chari, R. The Promise of Direct-to-Consumer Telehealth for Disaster Response and Recovery. Prehosp. Disaster Med. 2016, 31, 454–456. [Google Scholar] [CrossRef]
- Kellermann, A.L.; Isakov, A.P.; Parker, R.; Handrigan, M.T.; Foldy, S. Web-Based self-triage of influenza-like illness during the 2009 H1N1 influenza pandemic. Ann. Emerg. Med. 2010, 56, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Rademacher, N.J.; Cole, G.; Psoter, K.J.; Kelen, G.; Fan, J.W.Z.; Gordon, D.; Razzak, J. Use of Telemedicine to Screen Patients in the Emergency Department: Matched Cohort Study Evaluating Efficiency and Patient Safety of Telemedicine. JMIR Med. Inform. 2019, 7, e11233. [Google Scholar] [CrossRef] [PubMed]
- Tolia, V.; Castillo, E.; Guss, D. EDTITRATE (Emergency Department Telemedicine Initiative to Rapidly Accommodate in Times of Emergency). J. Telemed. Telecare 2017, 23, 484–488. [Google Scholar] [CrossRef] [PubMed]
- Buxton Bridges, C.; Katz, J.M.; Seto, W.H.; Chan, P.K.; Tsang, D.; Ho, W.; Mak, K.H.; Lim, W.; Tam, J.S.; Clarke, M.; et al. Risk of influenza A (H5N1) infection among health care workers exposed to patients with influenza A (H5N1), Hong Kong. J. Infect. Dis. 2000, 181, 344–348. [Google Scholar] [CrossRef]
- Balicer, R.D.; Omer, S.B.; Barnett, D.J.; Everly, G.S., Jr. Local public health workers’ perceptions toward responding to an influenza pandemic. BMC Public Health 2006, 6, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uscher-Pines, L.; Fischer, S.; Tong, I.; Mehrotra, A.; Malsberger, R.; Ray, K. Virtual First Responders: The Role of Direct-To-Consumer Telemedicine in Caring for People Impacted by Natural Disasters. J. Gen. Intern. Med. 2018, 33, 1242–1244. [Google Scholar] [CrossRef] [Green Version]
- Gesser-Edelsburg, A.; Cohen, R.; Diamant, A. Experts’ Views on the Gaps in Public Health Emergency Preparedness in Israel: A Qualitative Case Study. Disaster Med. Public Health Prep. 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S.-H.; Kraus, J.; Wu, H.-R.; Chen, W.-L.; Chiang, M.-F.; Lu, L.-H.; Chang, C.-E.; Chiu, W.-T. The effectiveness of video-telemedicine for screening of patients requesting emergency air medical transport (EAMT). J. Trauma 2007, 62, 504–511. [Google Scholar] [CrossRef]
- Brebner, E.M.; Brebner, J.A.; Ruddick-Bracken, H.; Wootton, R.; Ferguson, J.; Palombo, A.; Pedley, D.; Rowlands, A.; Fraser, S. Evaluation of an accident and emergency teleconsultation service for north-east Scotland. J. Telemed. Telecare 2004, 10, 16–20. [Google Scholar] [CrossRef]
- Mohr, N.M.; Young, T.; Harland, K.K.; Skow, B.; Wittrock, A.; Bell, A.; Ward, M.M. Emergency Department Telemedicine Shortens Rural Time-To-Provider and Emergency Department Transfer Times. Telemed. J. e-Health 2018, 24, 582–593. [Google Scholar] [CrossRef]
- Clarfield, A.M.; Manor, O.; Nun, G.B.; Shvarts, S.; Azzam, Z.S.; Afek, A.; Basis, F.; Israeli, A. Health and health care in Israel: An introduction. Lancet 2017, 389, 2503–2513. [Google Scholar] [CrossRef]
- Musharraf, M.; Khan, F.; Veitch, B. Validating Human Behavior Representation Model of General Personnel During Offshore Emergency Situations. Fire Technol. 2019, 55, 643–665. [Google Scholar] [CrossRef]
- Vigorito, C.; Faggiano, P.; Mureddu, G.F. COVID-19 pandemic: What consequences for cardiac rehabilitation? Monaldi Arch. Chest Dis. 2020, 90, 205–206. [Google Scholar] [CrossRef] [PubMed]
- McKay, D.; Yang, H.; Elhai, J.; Asmundson, G. Anxiety Regarding Contracting COVID-19 Related to Interoceptive Anxiety Sensations: The Moderating Role of Disgust Propensity and Sensitivity. J. Anxiety Disord. 2020, 73, 102233. [Google Scholar] [CrossRef]
- Edwards, L.; Thomas, C.; Gregory, A.; Yardley, L.; O’Cathain, A.; Montgomery, A.A.; Salisbury, C. Are people with chronic diseases interested in using telehealth? A cross-sectional postal survey. J. Med. Internet Res. 2014, 16, e123. [Google Scholar] [CrossRef] [Green Version]
- Valikodath, N.G.; Leveque, T.K.; Wang, S.Y.; Lee, P.P.; Newman-Casey, P.A.; Hansen, S.O.; Woodward, M.A. Patient Attitudes Toward Telemedicine for Diabetic Retinopathy. Telemed. J. e-Health 2017, 23, 205–212. [Google Scholar] [CrossRef] [Green Version]
- Van Veen, T.; Binz, S.; Muminovic, M.; Chaudhry, K.; Rose, K.; Calo, S.; Rammal, J.A.; France, J.; Miller, J.B. Potential of Mobile Health Technology to Reduce Health Disparities in Underserved Communities. West. J. Emerg. Med. 2019, 20, 799–802. [Google Scholar] [CrossRef]
- Polinski, J.M.; Barker, T.; Gagliano, N.; Sussman, A.; Brennan, T.A.; Shrank, W.H. Patients’ Satisfaction with and Preference for Telehealth Visits. J. Gen. Intern. Med. 2016, 31, 269–275. [Google Scholar] [CrossRef] [Green Version]
- Martinez, K.A.; Rood, M.; Jhangiani, N.; Kou, L.; Rose, S.; Boissy, A.; Rothberg, M.B. Patterns of Use and Correlates of Patient Satisfaction with a Large Nationwide Direct to Consumer Telemedicine Service. J. Gen. Intern. Med. 2018, 33, 1768–1773. [Google Scholar] [CrossRef] [Green Version]
- Orlando, J.F.; Beard, M.; Kumar, S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS ONE 2019, 14, e0221848. [Google Scholar] [CrossRef] [Green Version]
- Velsen, L.V.; Tabak, M.; Hermens, H. Measuring patient trust in telemedicine services: Development of a survey instrument and its validation for an anticoagulation web-service. Int. J. Med. Inform. 2017, 97, 52–58. [Google Scholar] [CrossRef]
- Van Velsen, L.; Wildevuur, S.; Flierman, I.; Van Schooten, B.; Tabak, M.; Hermens, H. Trust in telemedicine portals for rehabilitation care: An exploratory focus group study with patients and healthcare professionals. BMC Med. Inform. Decis. Mak. 2016, 16, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilkowska, W.; Ziefle, M. Privacy and data security in E-Health: Requirements from the user’s perspective. Health Inform. J. 2012, 18, 191–201. [Google Scholar] [CrossRef]
- Kontos, E.; Blake, K.D.; Chou, W.Y.; Prestin, A. Predictors of eHealth usage: Insights on the digital divide from the Health Information National Trends Survey 2012. J. Med. Internet Res. 2014, 16, e172. [Google Scholar] [CrossRef]
- Green, B.B.; Anderson, M.L.; Ralston, J.D.; Catz, S.; Fishman, P.A.; Cook, A.J. Patient ability and willingness to participate in a web-based intervention to improve hypertension control. J. Med. Internet Res. 2011, 13, e1. [Google Scholar] [CrossRef] [PubMed]
- Berner, J.S.; Rennemark, M.; Jogréus, C.; Berglund, J. Factors associated with change in Internet usage of Swedish older adults (2004–2010). Health Inform. J. 2013, 19, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Buliński, L.; Błachnio, A. Health in old age, and patients’ approaches to telemedicine in Poland. Ann. Agric. Environ. Med. 2017, 24, 322–328. [Google Scholar] [CrossRef]
- Wolf, M.S.; Serper, M.; Opsasnick, L.; O’Conor, R.M.; Curtis, L.M.; Benavente, J.Y.; Wismer, G.; Batio, S.; Eifler, M.; Zheng, P.; et al. Awareness, Attitudes, and Actions Related to COVID-19 Among Adults With Chronic Conditions at the Onset of the U.S. Outbreak: A Cross-Sectional Survey. Ann. Intern. Med. 2020. [Google Scholar] [CrossRef] [Green Version]

| Characteristics | n (%) | |
|---|---|---|
| Age | <40 | 299 (59.0) |
| Gender | Male | 274 (54.0) |
| Living area | Jerusalem | 71 (14.0) |
| Tel Aviv-Gush Dan-Sharon | 185 (36.5) | |
| Haifa and North | 182 (35.9) | |
| South and Lowlands | 69 (13.6) | |
| Religion | Jewish | 410 (80.9) |
| Non-Jewish | 97 (19.1) | |
| Religiosity | Secular | 256 (50.5) |
| Traditional | 151 (29.8) | |
| Religious | 100 (19.7) | |
| Marital status | In partnership | 347 (68.4) |
| Children <18 living at home | No children | 232 (45.8) |
| One child | 90 (17.8) | |
| ≥2 children | 185 (36.5) | |
| Adult offspring at home | No children | 233 (46.0) |
| One child | 109 (21.5) | |
| ≥2 children | 165 (32.5) | |
| Education | Below tertiary education | 247 (48.7) |
| Tertiary education | 260 (51.3) | |
| Salary | Below average | 212 (41.8) |
| Near average | 133 (26.2) | |
| Above average | 162 (32.0) |
| Variable | Unstandardized Coefficients | Standardized Coefficient | |||
|---|---|---|---|---|---|
| B | Standard Error | B | t | p | |
| (Constant) | 2.324 | 0.126 | 18.462 | <0.001 | |
| Trust of data protection | 0.263 | 0.037 | 0.347 | 7.162 | <0.001 |
| Education | 0.119 | 0.057 | 0.100 | 2.077 | 0.038 |
| Activity on social media | 0.076 | 0.037 | 0.098 | 2.032 | 0.043 |
| Variable | Unstandardized Coefficients | Standardized Coefficient | |||
|---|---|---|---|---|---|
| B | Standard Error | B | t | p | |
| (Constant) | 2.273 | 0.095 | 23.899 | <0.001 | |
| Trust of data protection | 0.319 | 0.039 | 0.389 | 8.161 | <0.001 |
| Education | 0.149 | 0.061 | 0.117 | 2.452 | 0.015 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamlin, M.; Steingrimsson, S.; Cohen, I.; Bero, V.; Bar-Tl, A.; Adini, B. Attitudes of the Public to Receiving Medical Care during Emergencies through Remote Physician–Patient Communications. Int. J. Environ. Res. Public Health 2020, 17, 5236. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145236
Hamlin M, Steingrimsson S, Cohen I, Bero V, Bar-Tl A, Adini B. Attitudes of the Public to Receiving Medical Care during Emergencies through Remote Physician–Patient Communications. International Journal of Environmental Research and Public Health. 2020; 17(14):5236. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145236
Chicago/Turabian StyleHamlin, Matilda, Steinn Steingrimsson, Itzhak Cohen, Victor Bero, Avishay Bar-Tl, and Bruria Adini. 2020. "Attitudes of the Public to Receiving Medical Care during Emergencies through Remote Physician–Patient Communications" International Journal of Environmental Research and Public Health 17, no. 14: 5236. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145236





