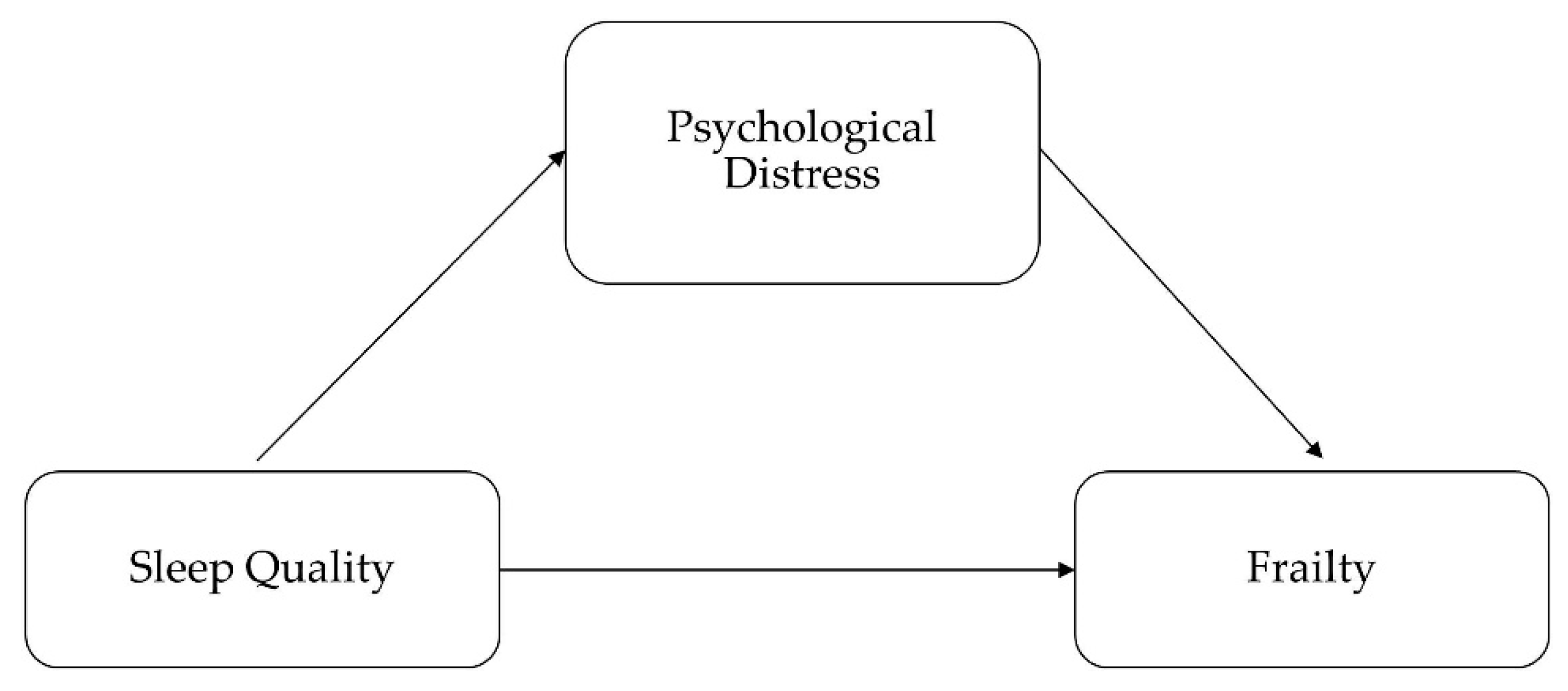
Associations of Sleep Quality and Frailty among the Older Adults with Chronic Disease in China: The Mediation Effect of Psychological Distress
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Frailty Status Measurements
2.3. Sleep Quality
2.4. Psychological Distress
2.5. Statistic Analysis
2.6. Ethical Consideration
3. Results
3.1. Effects of Sleep Quality on Psychological Distress
3.2. Effects of Sleep Quality and Psychological Distress on Frailty
3.3. Mediation Effects of Psychological Distress on Frailty
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Measures | Cut-Off Points for Frailty | |
|---|---|---|
| Weakness | Male | |
| Grip Strength (Kg) | BMI | |
| <29 | ≤24 | |
| <30 | 24.1–26 | |
| <30 | 26.1–28 | |
| <32 | >28 | |
| Female | ||
| Grip Strength (Kg) | BMI | |
| <17 | ≤23 | |
| <17.3 | 23.1–26 | |
| <18 | 26.1–29 | |
| <21 | >29 | |
| Slowness | Male | |
| Time to walk 4.6 m (seconds) | Height (cm) | |
| ≥7 | ≤173 | |
| ≥6 | >173 | |
| Female | ||
| Time to walk 4.6 m (seconds) | Height (cm) | |
| ≥7 | ≤159 | |
| ≥6 | >159 | |
| Low physical Activity | Male | |
| Total Kcals (per week) | - | |
| <383 | - | |
| Female | ||
| Total Kcals (per week) | - | |
| <270 | - | |
References
- Villacampa-Fernandez, P.; Navarro-Pardo, E.; Tarin, J.J.; Cano, A. Frailty and multimorbidity: Two related yet different concepts. Maturitas 2017, 95, 31–35. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- Santos-Eggimann, B.; Sirven, N. Screening for frailty: Older populations and older individuals. Public Health Rev. 2016, 37, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buckinx, F.; Rolland, Y.; Reginster, J.Y.; Ricour, C.; Petermans, J.; Bruyere, O. Burden of frailty in the elderly population: Perspectives for a public health challenge. Arch. Public Health 2015, 73, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sahle, B.W.; Chen, W.; Melaku, Y.A.; Akombi, B.J.; Rawal, L.B.; Renzaho, A.M.N. Association of psychosocial factors with risk of chronic diseases: A nationwide longitudinal study. Am. J. Prev. Med. 2020, 58, E39–E50. [Google Scholar] [CrossRef] [PubMed]
- Renne, I.; Gobbens, R.J.J. Effects of frailty and chronic diseases on quality of life in Dutch community-dwelling older adults: A cross-sectional study. Clin. Interv. Aging 2018, 13, 325–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amaral, C.D.; Amaral, T.L.M.; Monteiro, G.T.R.; De Vasconcellos, M.T.L.; Portela, M.C. Factors associated with low handgrip strength in older people: Data of the study of chronic diseases (Edoc-I). BMC Public Health 2020, 20, 395. [Google Scholar]
- Merchant, R.A.; Chen, M.Z.; Tan, L.W.L.; Lim, Y.D.; Ho, H.K.; Van Dam, R.M. Singapore healthy older people everyday (HOPE) study: Prevalence of frailty and associated factors in older adults. J. Am. Med. Dir. Assoc. 2017, 18, 734.e9–734.e14. [Google Scholar] [CrossRef]
- Adabag, S.; Vo, T.N.; Langsetmo, L.; Schousboe, J.T.; Cawthon, P.M.; Stone, K.L.; Shikany, J.M.; Taylor, B.C.; Ensrud, K.E. Frailty as a risk factor for cardiovascular versus noncardiovascular mortality in older men: Results from the mros sleep (outcomes of sleep disorders in older men) study. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2018, 7, 1785. [Google Scholar] [CrossRef]
- Avgerinou, C.; Gardner, B.; Kharicha, K.; Frost, R.; Liljas, A.; Elaswarapu, R.; Manthorpe, J.; Drennan, V.M.; Goodman, C.; Iliffe, S.; et al. Health promotion for mild frailty based on behaviour change: Perceptions of older people and service providers. Health Soc. Care Community 2019, 27, 1333–1343. [Google Scholar] [CrossRef] [Green Version]
- Ng, T.P.; Feng, L.; Nyunt, M.S.Z.; Feng, L.; Niti, M.; Tan, B.Y.; Chan, G.; Khoo, S.A.; Chan, S.M.; Yap, P.; et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: A randomized controlled trial. Am. J. Med. 2015, 128, 1225–1236.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Xu, X.J.; Lian, T.Y.; Huang, L.F.; Zeng, J.M.; Liang, D.M.; Yin, M.J.; Huang, J.X.; Xiu, L.C.; Yu, Z.W.; et al. Development of frailty subtypes and their associated risk factors among the community-dwelling elderly population. Aging-US 2020, 12, 1128–1140. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, T.-J.; Su, S.-C.; Chen, C.-W.; Kang, Y.-W.; Hu, M.-H.; Hsu, L.-L.; Wu, S.-Y.; Chen, L.; Chang, H.-Y.; Chuang, S.-Y.; et al. Individualized home-based exercise and nutrition interventions improve frailty in older adults: A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wai, J.L.T.; Yu, D.S.F. The relationship between sleep-wake disturbances and frailty among older adults: A systematic review. J. Adv. Nurs. 2020, 76, 96–108. [Google Scholar] [CrossRef] [PubMed]
- Baniak, L.M.; Yang, K.; Choi, J.; Chasens, E.R. Long sleep duration is associated with increased frailty risk in older community-dwelling adults. J. Aging Health 2020, 32, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.M.; Chen, H.G.; Song, M.; Xu, S.J.; Yu, L.L.; Wang, L.; Wang, R.; Shi, L.; He, J.; Huang, Y.Q.; et al. Prevalence of insomnia and its risk factors in older individuals: A community-based study in four cities of Hebei Province, China. Sleep Med. 2016, 19, 116–122. [Google Scholar] [CrossRef]
- Wang, P.; Song, L.; Wang, K.L.; Han, X.L.; Cong, L.; Wang, Y.X.; Zhang, L.; Yan, Z.R.; Tang, S.; Du, Y.F. Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: A population-based study. Aging Clin. Exp. Res. 2020, 32, 125–131. [Google Scholar] [CrossRef] [Green Version]
- Sun, X.H.; Ma, T.; Yao, S.; Chen, Z.K.; Xu, W.D.; Jiang, X.Y.; Wang, X.F. Associations of sleep quality and sleep duration with frailty and pre-frailty in an elderly population Rugao longevity and ageing study. BMC Geriatr. 2020, 20, 9. [Google Scholar] [CrossRef]
- Jiang, J.J.; Li, Y.Q.; Mao, Z.X.; Wang, F.; Huo, W.Q.; Liu, R.H.; Zhang, H.Q.; Tian, Z.Y.; Liu, X.T.; Zhang, X.; et al. Abnormal night sleep duration and poor sleep quality are independently and combinedly associated with elevated depressive symptoms in Chinese rural adults: Henan rural cohort. Sleep Med. 2020, 70, 71–78. [Google Scholar] [CrossRef]
- Zhou, L.; Zhang, H.Q.; Luo, Z.C.; Liu, X.T.; Yang, L.Y.; Hua, H.Y.; Wang, Y.; Wang, C.J.; Wang, F. Abnormal night sleep duration and inappropriate sleep initiation time are associated with elevated anxiety symptoms in Chinese rural adults: The henan rural cohort. Psychiatry Res. 2020, 291, 113232. [Google Scholar] [CrossRef]
- Meerlo, P.; Havekes, R.; Steiger, A. Chronically restricted or disrupted sleep as a causal factor in the development of depression. In Sleep, Neuronal Plasticity and Brain Function; Meerlo, P., Benca, R.M., Abel, T., Eds.; Springer Berlin Heidelberg: Berlin/Heidelberg, Germany, 2015; pp. 459–481. [Google Scholar]
- De Sousa, D.E.; De Carli, M.N.; Fernandes, R.C.; Trindade, D.B.; Laviano, A.; Pichard, C.; Pimentel, G.D. Are depression and anxiety disorders associated with adductor pollicis muscle thickness, sleep duration, and protein intake in cancer patients? Exp. Gerontol. 2020, 130, 5. [Google Scholar] [CrossRef] [PubMed]
- Biddle, D.J.; Kelly, P.J.; Hermens, D.F.; Glozier, N. The association of insomnia with future mental illness: Is it just residual symptoms? Sleep Health 2018, 4, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Kay, D.B.; Dombrovski, A.Y.; Buysse, D.J.; Reynolds, C.F.; Begley, A.; Szanto, K. Insomnia is associated with suicide attempt in middle-aged and older adults with depression. Int. Psychogeriatr. 2016, 28, 613–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, P.J.; Roose, S.P.; O’Boyle, K.R.; Ciarleglio, A.; Maas, B.; Igwe, K.C.; Chung, S.; Gomez, S.; Naqvi, M.; Brickman, A.M.; et al. Frailty and its correlates in adults with late life depression. Am. J. Geriatr. Psychiatr. 2020, 28, 145–154. [Google Scholar] [CrossRef]
- Bickford, D.; Morin, R.T.; Woodworth, C.; Verduzco, E.; Khan, M.; Burns, E.; Nelson, J.C.; Mackin, R.S. The relationship of frailty and disability with suicidal ideation in late life depression. Aging Ment. Health 2019. [Google Scholar] [CrossRef]
- Mccrae, C.S.; Mcnamara, J.P.H.; Rowe, M.A.; Dzierzewski, J.M.; Dirk, J.; Marsiske, M.; Craggs, J.G. Sleep and affect in older adults: Using multilevel modeling to examine daily associations. J. Sleep Res. 2008, 17, 42–53. [Google Scholar] [CrossRef] [Green Version]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Ward, R.E.; Orkaby, A.R.; Chen, J.Y.; Hshieh, T.T.; Driver, J.A.; Gaziano, J.M.; Djousse, L. Association between diet quality and frailty prevalence in the physicians’ health study. J. Am. Geriatr. Soc. 2020, 68, 770–776. [Google Scholar] [CrossRef]
- Ningning, Q.; Keji, L. Study on the reliability and validity of international physical activity questionnaire (Chinese Version, IPAQ). Chin. J. Epidemiol. 2004, 25, 265–268. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The pittsburgh sleep quality index-a new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Del Brutto, O.H.; Mera, R.M.; Sedler, M.J.; Zambrano, M.; Nieves, J.L.; Cagino, K.; Fanning, K.D.; Milla-Martinez, M.F.; Castillo, P.R. The effect of age in the association between frailty and poor sleep? quality: A population-based study in community-dwellers (the atahualpa project). J. Am. Med Dir. Assoc. 2016, 17, 269–271. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.Q.; Pan, B.C.; Sun, W.; Wu, H.; Wang, L. Anxiety symptoms among Chinese nurses and the associated factors: A cross sectional study. BMC Psychiatry 2012, 12, 141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kessler, R.; Barker, P.; Colpe, L.; Epstein, J.; Zaslavsky, A. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Anderson, T.M.; Sunderland, M.; Andrews, G.; Titov, N.; Dear, B.F.; Sachdev, P.S. The 10-item Kessler psychological distress scale (K10) as a screening instrument in older individuals. Am. J. Geriatr. Psychiatry 2013, 21, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.C.; Jiang-Jiang, H.E.; Ling-Zhong, X.U. First application of Kessler 10 scale to measuring mental health status of the aged in China. Chin. J. Clin. Psychol. 2009, 17, 761–763. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, S.; Park, S.H.; Heo, Y.W.; Chang, B.S.; Lee, C.K.; Yeom, J.S. The significance of frailty in the relationship between socioeconomic status and health-related quality of life in the Korean community-dwelling elderly population: Mediation analysis with bootstrapping. Qual. Life Res. 2017, 26, 3323–3330. [Google Scholar] [CrossRef]
- Jiao, J.; Wang, Y.; Zhu, C.; Li, F.; Zhu, M.; Wen, X.; Jin, J.; Wang, H.; Lv, D.; Zhao, S.; et al. Prevalence and associated factors for frailty among elder patients in China: A multicentre cross-sectional study. BMC Geriatr. 2020, 20, 100. [Google Scholar] [CrossRef]
- Ye, B.; Chen, H.; Huang, L.M.; Ruan, Y.; Qi, S.G.; Guo, Y.F.; Huang, Z.Z.; Sun, S.Y.; Chen, X.Q.; Shi, Y.; et al. Changes in frailty among community- dwelling chinese older adults and its predictors: Evidence from a two-year longitudinal study. BMC Geriatr. 2020, 20, 130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, B.; Ma, Y.; Wang, C.; Jiang, M.; Geng, C.; Chang, X.; Ma, B.; Han, L. Prevalence and risk factors for frailty among community-dwelling older people in china: A systematic review and meta-analysis. J. Nutr. Health Aging 2019, 23, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Tuna, F.; Ustundag, A.; Can, H.B.; Tuna, H. Rapid geriatric assessment, physical activity, and sleep quality in adults aged more than 65 years: A preliminary study. J. Nutr. Health Aging 2019, 23, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Campanini, M.Z.; Mesas, A.E.; Carnicero-Carreno, J.A.; Rodriguez-Artalejo, F.; Lopez-Garcia, E. Duration and quality of sleep and risk of physical function impairment and disability in older adults: Results from the enrica and elsa cohorts. Aging Dis. 2019, 10, 557–569. [Google Scholar] [CrossRef] [Green Version]
- Kang, I.; Kim, S.; Kim, B.S.; Yoo, J.; Kim, M.; Won, C.W. Sleep latency in men and sleep duration in women can be frailty markers in community-dwelling older adults: The Korean Frailty and Aging Cohort Study (KFACS). J. Nutr. Health Aging 2019, 23, 63–67. [Google Scholar] [CrossRef]
- Moreno-Tamayo, K.; Manrique-Espinoza, B.; Rosas-Carrasco, O.; Perez-Moreno, A.; Salinas-Rodriguez, A. Sleep complaints are associated with frailty in Mexican older adults in a rural setting. Geriatr. Gerontol. Int. 2017, 17, 2573–2578. [Google Scholar] [CrossRef]
- Bernert, R.A.; Joiner, T.E., Jr.; Cukrowicz, K.C.; Schmidt, N.B.; Krakow, B. Suicidality and sleep disturbances. Sleep 2005, 28, 1135–1141. [Google Scholar] [CrossRef] [Green Version]
- Schnittger, R.I.B.; Walsh, C.D.; Casey, A.M.; Wherton, J.P.; McHugh, J.E.; Lawlor, B.A. Psychological distress as a key component of psychosocial functioning in community-dwelling older people. Aging Ment. Health 2012, 16, 199–207. [Google Scholar] [CrossRef]
- Seaton, V.A.; Narcisse, M.R.; Subica, A.M.; Long, C.R.; Matthews, E.E.; McElfish, P.A. Sleep quality partially mediates the association between type 2 diabetes and psychological distress in native hawaiian and pacific islander adults in the united states: Analysis of the 2014 national health interview survey. Asian Am. J. Psychol. 2019, 10, 258–267. [Google Scholar] [CrossRef]
- De Rooij, A.; Van Der Leeden, M.; Roorda, L.D.; Rinkema, M.; Beuving, W.; Dekker, J. Factors associated with sleep quality in patients with chronic widespread pain attending multidisciplinary treatment. Pain Pract. 2020, 20, 471–479. [Google Scholar] [CrossRef]
- Grov, E.K.; Fosså, S.D.; Dahl, A.A. Insomnia in elderly cancer survivors—A population-based controlled study of associations with lifestyle, morbidity, and psychosocial factors. Results from the Health Survey of North-Trøndelag County (HUNT-2). Support. Care Cancer 2011, 19, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Wong, P.S.; Hasan, S.S.; Kairuz, T. The relationship between sleep quality, inappropriate medication use and frailty among older adults in aged care homes in Malaysia. PLoS ONE 2019, 14, e0224122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgan, K.; Hartescu, I. Sleep duration and all-cause mortality: Links to physical activity and prefrailty in a 27-year follow up of older adults in the UK. Sleep Med. 2019, 54, 231–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging 2018, 13, 757–772. [Google Scholar] [CrossRef] [Green Version]
- Derbre, F.; Gratas-Delamarche, A.; Gomez-Cabrera, M.C.; Vina, J. Inactivity-induced oxidative stress: A central role in age-related sarcopenia? Eur. J. Sport Sci. 2014, 14, S98–S108. [Google Scholar] [CrossRef]
- Norheim, K.B.; Jonsson, G.; Omdal, R. Biological mechanisms of chronic fatigue. Rheumatology 2011, 50, 1009–1018. [Google Scholar] [CrossRef] [Green Version]
- Patel, R.S.; Ghasemzadeh, N.; Eapen, D.J.; Sher, S.; Arshad, S.; Ko, Y.A.; Veledar, E.; Samady, H.; Zafari, A.M.; Sperling, L.; et al. Novel biomarker of oxidative stress is associated with risk of death in patients with coronary artery disease. Circulation 2016, 133, 361–369. [Google Scholar] [CrossRef]
| Characteristics | All N (%) | Robust | Pre-Frailty | Frailty | p-Value |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Total | 2346 (100) | 342 (15) | 1504 (64) | 500 (21) | |
| Gender | 0.090 | ||||
| Male | 820 (35) | 109 (32) | 550 (37) | 161 (32) | |
| Female | 1526 (65) | 233 (68) | 954 (63) | 339 (68) | |
| Age (years) | <0.001 | ||||
| Mean ± SD | 70.15 (6.05) | 68.19 (5.03) | 70.08 (6.00) | 71.70 (6.41) | |
| Education | <0.001 | ||||
| Illiteracy | 963 (41) | 117 (34) | 627 (42) | 219 (44) | |
| Junior school | 948 (40) | 136 (40) | 600 (40) | 212 (42) | |
| Senior school+ | 435 (19) | 89 (26) | 277 (18) | 69 (14) | |
| Occupation | <0.001 | ||||
| Unemployed | 1026 (44) | 99 (29) | 632 (42) | 295 (59) | |
| Farmers | 1320 (56) | 243 (71) | 872 (58) | 205 (41) | |
| Marital Status | 0.209 | ||||
| Married | 1737 (74) | 266 (78) | 1108 (74) | 363 (73) | |
| Other | 609 (26) | 76 (22) | 396 (26) | 137 (27) | |
| Household income/year | <0.001 | ||||
| <7 K | 787 (33) | 65 (19) | 513 (34) | 209 (42) | |
| 7–15 K | 657 (28) | 114 (33) | 404 (27) | 139 (28) | |
| >15 K | 902 (39) | 163 (48) | 587 (39) | 152 (30) | |
| Activity | <0.001 | ||||
| Moderate | 1166 (49) | 134 (39) | 697 (46) | 335(67) | |
| Vigorous | 1180 (51) | 208(61) | 807 (54) | 165 (33) | |
| Drinking | <0.001 | ||||
| None | 1708 (72) | 247 (72) | 1067 (71) | 394 (79) | |
| Ever | 178 (8) | 24 (7) | 122 (8) | 32 (6) | |
| Current | 460 (20) | 71 (21) | 315 (21) | 74 (15) | |
| Smoking | 0.506 | ||||
| None | 1652 (70) | 249 (73) | 1048 (70) | 355(71) | |
| Ever | 262 (11) | 41 (12) | 170 (11) | 51 (10) | |
| Current | 432 (19) | 52 (15) | 286 (19) | 94 (19) | |
| BMI | 0.671 | ||||
| Mean ± SD | 24.72 (4.05) | 24.62 (3.46) | 24.78 (4.08) | 24.63 (4.31) | |
| Self-reported Health Status | <0.001 | ||||
| Poor | 786 (33) | 53 (15) | 455 (30) | 278 (56) | |
| Medium | 740 (32) | 109 (32) | 499 (33) | 132 (26) | |
| Good | 820 (35) | 180 (53) | 550 (37) | 90 (18) | |
| Variables | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Frailty | Psychological Distress | Frailty | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sleep quality | - | - | - | - | - | - |
| PSQI < 7 (ref.) | - | - | - | - | - | - |
| PSQI ≥ 7 | 1.84 *** | (1.53, 2.23) | 3.48 *** | (2.89, 4.18) | 1.44 *** | (1.19, 1.76) |
| Psychological distress | - | - | - | - | - | |
| No (ref.) | - | - | - | - | - | - |
| Mild | - | - | - | - | 1.63 *** | (1.29, 2.05) |
| Moderate | - | 2.34 *** | (1.81, 3.02) | |||
| Severe | - | - | - | - | 4.43 *** | (3.15, 6.22) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fu, P.; Zhou, C.; Meng, Q. Associations of Sleep Quality and Frailty among the Older Adults with Chronic Disease in China: The Mediation Effect of Psychological Distress. Int. J. Environ. Res. Public Health 2020, 17, 5240. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145240
Fu P, Zhou C, Meng Q. Associations of Sleep Quality and Frailty among the Older Adults with Chronic Disease in China: The Mediation Effect of Psychological Distress. International Journal of Environmental Research and Public Health. 2020; 17(14):5240. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145240
Chicago/Turabian StyleFu, Peipei, Chengchao Zhou, and Qingyue Meng. 2020. "Associations of Sleep Quality and Frailty among the Older Adults with Chronic Disease in China: The Mediation Effect of Psychological Distress" International Journal of Environmental Research and Public Health 17, no. 14: 5240. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17145240






