Relief Alternatives during Resuscitation: Instructions to Teach Bystanders. A Randomized Control Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Selection of Participants
2.3. Intervention
2.4. Experimental Group: Structured Orders
- “Kneel in front of me”.
- “Interlock your hands, one over the other, and straighten your arms”.
- “When I count to three, you have to place your hand in the middle of the chest and compress “hard and fast” [25] 30 times”.
- “Have you understood?” (If the participant answered “NO” to this question, the order would be repeated again without any changes).
- “1, 2, 3, now!”
- “Put your hand on the forehead”.
- “Put the other hand on the chin and lift”.
- “Cover the nose and blow two times when your partner reaches 30”.
2.5. Control Group: Structured Orders
2.6. Analysis Parameters
2.7. Measurements
2.8. Analysis
2.9. Ethical Considerations
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hawkes, C.; Booth, S.; Ji, C.; Brace-McDonnell, S.J.; Whittington, A.; Mapstone, J.; Cooke, M.W.; Deakin, C.D.; Gale, C.P.; Fothergill, R.; et al. Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation 2017, 110, 133–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasselqvist-Ax, I.; Riva, G.; Herlitz, J.; Rosenqvist, M.; Hollenberg, J.; Nordberg, P.; Ringh, M.; Jonsson, M.; Axelsson, C.; Lindqvist, J.; et al. Early Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2015, 372, 2307–2315. [Google Scholar] [CrossRef] [Green Version]
- Zideman, D.A.; De Buck, E.D.J.; Singletary, E.M.; Cassan, P.; Chalkias, A.F.; Evans, T.R.; Hafner, C.M.; Handley, A.J.; Meyran, D.; Schunder-Tatzber, S.; et al. European Resuscitation Council Guidelines for Resuscitation 2015 First aid. Resuscitation 2015, 95, 278–287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pek, J.H.; de Korne, D.F.; Hannawa, A.F.; Leong, B.S.H.; Ng, Y.Y.; Arulanandam, S.; Tham, L.P.; Ong, M.E.H.; Ong, G.Y.-K. Dispatcher-assisted cardiopulmonary resuscitation for paediatric out-of-hospital cardiac arrest: A structured evaluation of communication issues using the SACCIA® safe communication typology. Resuscitation 2019, 139, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Yamada, N.; Fuerch, J.; Halamek, L. Impact of Standardized Communication Techniques on Errors during Simulated Neonatal Resuscitation. Am. J. Perinatol. 2015, 33, 385–392. [Google Scholar] [PubMed]
- Yamada, N.K.; Halamek, L.P. On the Need for Precise, Concise Communication during Resuscitation: A Proposed Solution. J. Pediatrics 2015, 166, 184–187. [Google Scholar] [CrossRef]
- Wu, Z.; Panczyk, M.; Spaite, D.W.; Hu, C.; Fukushima, H.; Langlais, B.; Sutter, J.; Bobrow, B.J. Telephone cardiopulmonary resuscitation is independently associated with improved survival and improved functional outcome after out-of-hospital cardiac arrest. Resuscitation 2018, 122, 135–140. [Google Scholar] [CrossRef]
- Soar, J.; Maconochie, I.; Wyckoff, M.H.; Olasveengen, T.M.; Singletary, E.M.; Greif, R.; Aickin, R.; Bhanji, F.; Donnino, M.W.; Mancini, M.E.; et al. 2019 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation 2019, 140. [Google Scholar] [CrossRef] [Green Version]
- Ro, Y.S.; Shin, S.D.; Song, K.J.; Hong, K.J.; Ahn, K.O.; Kim, D.K.; Kwak, Y.H. Effects of Dispatcher-assisted Cardiopulmonary Resuscitation on Survival Outcomes in Infants, Children, and Adolescents with Out-of-hospital Cardiac Arrests. Resuscitation 2016, 108, 20–26. [Google Scholar] [CrossRef]
- Goto, Y.; Maeda, T.; Goto, Y. Impact of Dispatcher-Assisted Bystander Cardiopulmonary Resuscitation on Neurological Outcomes in Children with Out-of-Hospital Cardiac Arrests: A Prospective, Nationwide, Population-Based Cohort Study. J. Am. Heart Assoc. 2014, 3, e000499. [Google Scholar] [CrossRef] [Green Version]
- Bohm, K.; Vaillancourt, C.; Charette, M.L.; Dunford, J.; Castrén, M. In patients with out-of-hospital cardiac arrest, does the provision of dispatch cardiopulmonary resuscitation instructions as opposed to no instructions improve outcome: A systematic review of the literature. Resuscitation 2011, 82, 1490–1495. [Google Scholar] [CrossRef] [PubMed]
- Olasveengen, T.M.; Mancini, M.E.; Vaillancourt, C.; Brooks, S.C.; Castren, M.; Chung, S.P.; Couper, K.; Dainty, K.N.; Escalante, R.; Gazmuri, R.J.; et al. Emergency Care: Dispatcher Instruction in CPR: Systematic Review. Available online: https://costr.ilcor.org/document/emergency-care-dispatcherinstruction-in-cpr (accessed on 25 February 2019).
- Lyons, P.; Bandura, R.P. Case-based modeling for learning: Socially constructed skill development. Educ.+ Train. 2018, 60, 139–154. [Google Scholar] [CrossRef]
- Domjan, M. Principios de Aprendizaje y Conducta; Paraninfo: Madrid, Spain, 2007; ISBN 9788497325844. [Google Scholar]
- Lauridsen, K.G.; Watanabe, I.; Løfgren, B.; Cheng, A.; Duval-Arnould, J.; Hunt, E.A.; Good, G.L.; Niles, D.; Berg, R.A.; Nishisaki, A.; et al. Standardising communication to improve in-hospital cardiopulmonary resuscitation. Resuscitation 2020, 147, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Hunt, E.A.; Cruz-Eng, H.; Bradshaw, J.H.; Hodge, M.; Bortner, T.; Mulvey, C.L.; McMillan, K.N.; Galvan, H.; Duval-Arnould, J.M.; Jones, K.; et al. A novel approach to life support training using “action-linked phrases”. Resuscitation 2015, 86, 1–5. [Google Scholar] [CrossRef]
- Research Methods Knowledge Base. Available online: http://anatomyfacts.com/Research/ResearchMethodsKnowledgeBase.pdf (accessed on 25 February 2019).
- Salazar, L.F.; Crosby, R.A.; DiClemente, R.J. Research Methods in Health Promotion; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Experimental Research Designs. Available online: https://psycnet.apa.org/record/2015-10205-005 (accessed on 25 February 2019).
- Allen, M. The SAGE Encyclopedia of Communication Research Methods; Sage Publications: Southend Oaks, CA, USA, 2017. [Google Scholar]
- Trochim, W.M.K.; Donnelly, J.P. Research Methods Knowledge Base, 3rd ed.; Atomic Dog: New York, NY, USA, 2020. [Google Scholar]
- Painter, I.; Chavez, D.E.; Ike, B.R.; Yip, M.P.; Tu, S.P.; Bradley, S.M.; Rea, T.D.; Meischke, H. Changes to DA-CPR instructions: Can we reduce time to first compression and improve quality of bystander CPR? Resuscitation 2014, 85, 1169–1173. [Google Scholar] [CrossRef]
- Chen, K.-Y.; Ko, Y.-C.; Hsieh, M.-J.; Chiang, W.-C.; Ma, M.H.-M. Interventions to improve the quality of bystander cardiopulmonary resuscitation: A systematic review. PLoS ONE 2019, 14, e0211792. [Google Scholar] [CrossRef]
- García del Águila, J.; López-Messa, J.; Rosell-Ortiz, F.; de Elías Hernández, R.; Martínez del Valle, M.; Sánchez-Santos, L.; López-Herce, J.; Cerdà-Vila, M.; Roza-Alonso, C.L.; Bernardez-Otero, M. Recomendaciones para el soporte telefónico a la reanimación por testigos desde los centros de coordinación de urgencias y emergencias. Med. Intensiva 2015, 39, 298–302. [Google Scholar] [CrossRef]
- Trethewey, S.P.; Vyas, H.; Evans, S.; Hall, M.; Melody, T.; Perkins, G.D.; Couper, K. The impact of resuscitation guideline terminology on quality of dispatcher-assisted cardiopulmonary resuscitation: A randomised controlled manikin study. Resuscitation 2019, 142, 91–96. [Google Scholar] [CrossRef]
- Fontes, S.; García-Gallego, C.; Quintanilla, L.; Rodríguez, R.; Rubio, P.; Sarriá, E. Fundamentos de investigación en psicología. In Diseños y Estrategias; UNED: Madrid, Spain, 2010. [Google Scholar]
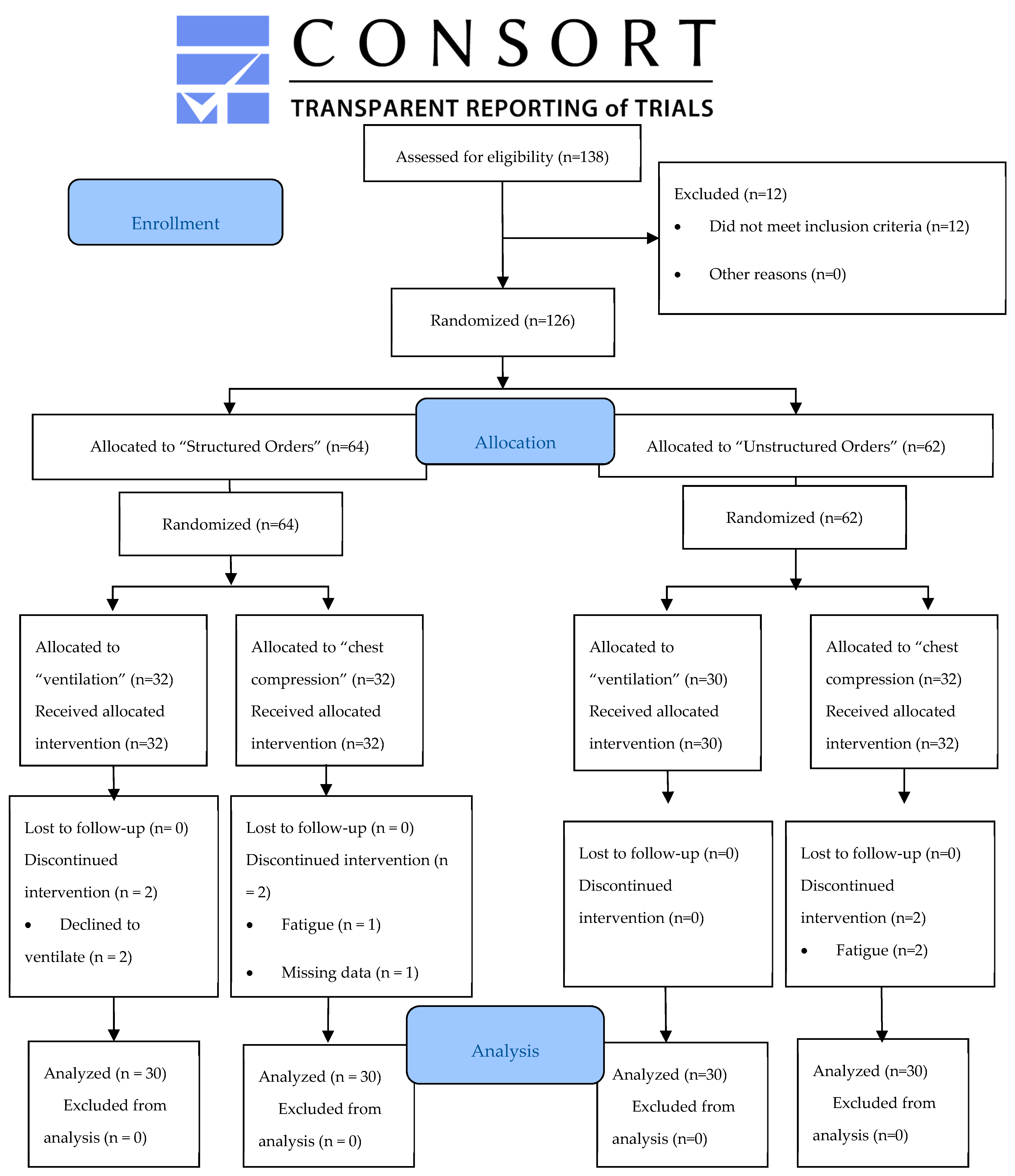
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340. [Google Scholar] [CrossRef]
- Ortiz, F.R.; Roig, F.E.; Navalpotro Pascual, J.M.; Iglesias Vázquez, J.A.; Sucunza, A.E.; Cordero Torres, J.A.; Cobos, E.; del Valle, M.M.; Rozalen, I.C.; martín Sánchez, E.; et al. Out-of-Hospital Spanish Cardiac Arrest Registry (OHSCAR). Results of the first year. Resuscitation 2015, 96, 100. [Google Scholar] [CrossRef]
- Williams, A.M.; Hodges, N.J. Practice, instruction and skill acquisition in soccer: Challenging tradition. J. Sports Sci. 2005, 23, 637–650. [Google Scholar] [CrossRef] [PubMed]
- D’Innocenzo, G.; Gonzalez, C.C.; Williams, A.M.; Bishop, D.T. Looking to Learn: The Effects of Visual Guidance on Observational Learning of the Golf Swing. PLoS ONE 2016, 11, e0155442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez, S.A.; Sutton, R.M.; Berg, M.D.; Nishisaki, A.; Maltese, M.; Meaney, P.A.; Niles, D.E.; Leffelman, J.; Berg, R.A.; Nadkarni, V.M. Simplified dispatcher instructions improve bystander chest compression quality during simulated pediatric resuscitation. Resuscitation 2014, 85, 119–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, S.; Kan, T.; Guo, Z.; Chen, C.; Gui, L. Assessing the quality of CPR performed by a single lifeguard, two lifeguards and a lifeguard with a bystander after water rescue: A quasi-experimental trial. Emerg. Med. J. 2020. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, T.; Sato, K.; Fujita, T.; Okajima, M.; Takamura, M. Attitudes to Bystander Cardiopulmonary Resuscitation in Japan in 2010. Circ. J. 2012, 76, 1130–1135. [Google Scholar] [CrossRef] [Green Version]
- Chang, M.P.; Gent, L.M.; Sweet, M.; Potts, J.; Ahtone, J.; Idris, A.H. A novel educational outreach approach to teach Hands-Only Cardiopulmonary Resuscitation to the public. Resuscitation 2017, 116, 22–26. [Google Scholar] [CrossRef]
- Olasveengen, T.M.; de Caen, A.R.; Mancini, M.E.; Maconochie, I.K.; Aickin, R.; Atkins, D.L.; Berg, R.A.; Bingham, R.M.; Brooks, S.C.; Castrén, M.; et al. 2017 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations Summary. Circulation 2017, 136, e424–e440. [Google Scholar] [CrossRef] [Green Version]
- González-Salvado, V.; Rodríguez-Ruiz, E.; Abelairas-Gómez, C.; Ruano-Raviña, A.; Peña-Gil, C.; González-Juanatey, J.R.; Rodríguez-Núñez, A. Training adult laypeople in basic life support. A systematic review. Revista Española de Cardiología (Engl. Ed.) 2020, 73, 53–68. [Google Scholar] [CrossRef]
- Beskind, D.L.; Stolz, U.; Thiede, R.; Hoyer, R.; Robertson, W.; Brown, J.; Ludgate, M.; Tiutan, T.; Shane, R.; McMorrow, D.; et al. Viewing an ultra-brief chest compression only video improves some measures of bystander CPR performance and responsiveness at a mass gathering event. Resuscitation 2017, 118, 96–100. [Google Scholar] [CrossRef]
- Benoit, J.L.; Vogele, J.; Hart, K.W.; Lindsell, C.J.; McMullan, J.T. Passive ultra-brief video training improves performance of compression-only cardiopulmonary resuscitation. Resuscitation 2017, 115, 116–119. [Google Scholar] [CrossRef]

| Demographic Variables | Unstructured Orders Group (n = 60) | Structured Orders Group (n = 60) | p-Value |
|---|---|---|---|
| Age (years)—mean (SD) | 21 (5.07) | 21 (3.78) | 0.669 |
| Sex (% female) | 36 (60) | 36 (60) | 0.574 |
| Height (m)—mean (SD) | 1.72 (0.09) | 1.70 (0.09) | 0.31 |
| Weight (kg)—mean (SD) | 67.3 (13.46) | 64.3 (11.68) | 0.209 |
| BMI (kg/m2)—mean (SD) | 22.7 (3.20) | 22.1 (2.77) | 0.236 |
| Variables of Study | Unstructured Orders | Structured Orders | t-Test/Mann–Whitney U | p-Value |
|---|---|---|---|---|
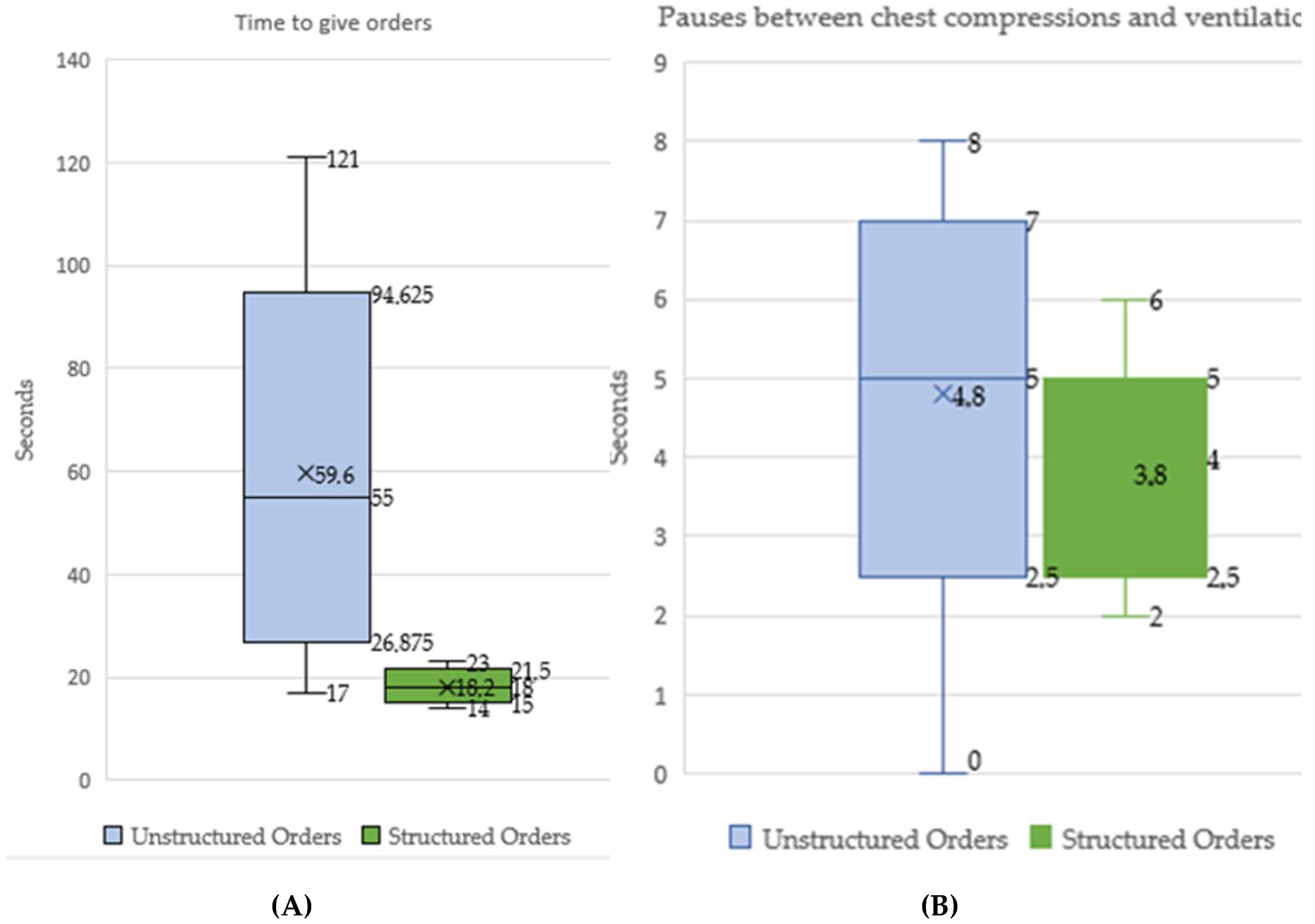
| Time needed to give orders (seconds)—mean (SD) | 55.3 (26.09) | 17.9 (2.34) | t = 7.813 | <0.001 |
| Pauses between chest compressions and ventilations (seconds)—median (IQR) | 5 (5, 6) | 4 (3, 4) | U = 152 | <0.001 |
| Depth (mm)—mean (SD) | 42.2 (12.04) | 51.1 (7.94) | t = 3.38 | 0.001 |
| Rate (comp/min)—median (IQR) | 121 (113, 132) | 121 (110, 130) | U = 443.5 | 0.923 |
| Overall score (0–100)—mean (SD) | 45.03 (22.5) | 73 (14.5) | t = 5.73 | <0.001 |
| Ventilation score (0−100) a—median (IQR) | 65 (34, 81.5) | 67 (49, 83) | U = 370.5 | 0.437 |
| Chest compression score (0–100)—median (IQR) | 53 (37.25, 61) | 78.5 (61.5, 87.25) | U = 171 | <0.001 |
| Hands position—median (IQR) | 100 (100, 100) | 100 (100, 100) | U = 437.5 | 0.784 |
| % Effective ventilation (500–600 mL) a—median (IQR) | 40 (0, 60.42) | 20 (5, 50) | U = 394.5 | 0.682 |
| % Chest recoil—median (IQR) | 58.3 (27.46, 84.33) | 86.32 (62.36, 98.87) | U = 263.5 | 0.006 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pujalte-Jesús, M.J.; Leal-Costa, C.; Ruzafa-Martínez, M.; Ramos-Morcillo, A.J.; Díaz Agea, J.L. Relief Alternatives during Resuscitation: Instructions to Teach Bystanders. A Randomized Control Trial. Int. J. Environ. Res. Public Health 2020, 17, 5495. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17155495
Pujalte-Jesús MJ, Leal-Costa C, Ruzafa-Martínez M, Ramos-Morcillo AJ, Díaz Agea JL. Relief Alternatives during Resuscitation: Instructions to Teach Bystanders. A Randomized Control Trial. International Journal of Environmental Research and Public Health. 2020; 17(15):5495. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17155495
Chicago/Turabian StylePujalte-Jesús, María José, César Leal-Costa, María Ruzafa-Martínez, Antonio Jesús Ramos-Morcillo, and José Luis Díaz Agea. 2020. "Relief Alternatives during Resuscitation: Instructions to Teach Bystanders. A Randomized Control Trial" International Journal of Environmental Research and Public Health 17, no. 15: 5495. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17155495








