A Systematic Review of the Psychosocial Adjustment of Children and Adolescents with Facial Palsy: The Impact of Moebius Syndrome
Abstract
:1. Introduction
Aims and Objectives
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.2.1. Types of Studies
2.2.2. Types of Participants
2.2.3. Types of Intervention
2.2.4. Types of Outcome Measure
2.3. Information Sources
2.4. Search
2.5. Study Selection
2.6. Data Collection Process
2.7. Data Items
2.8. Quality Assessment
3. Results
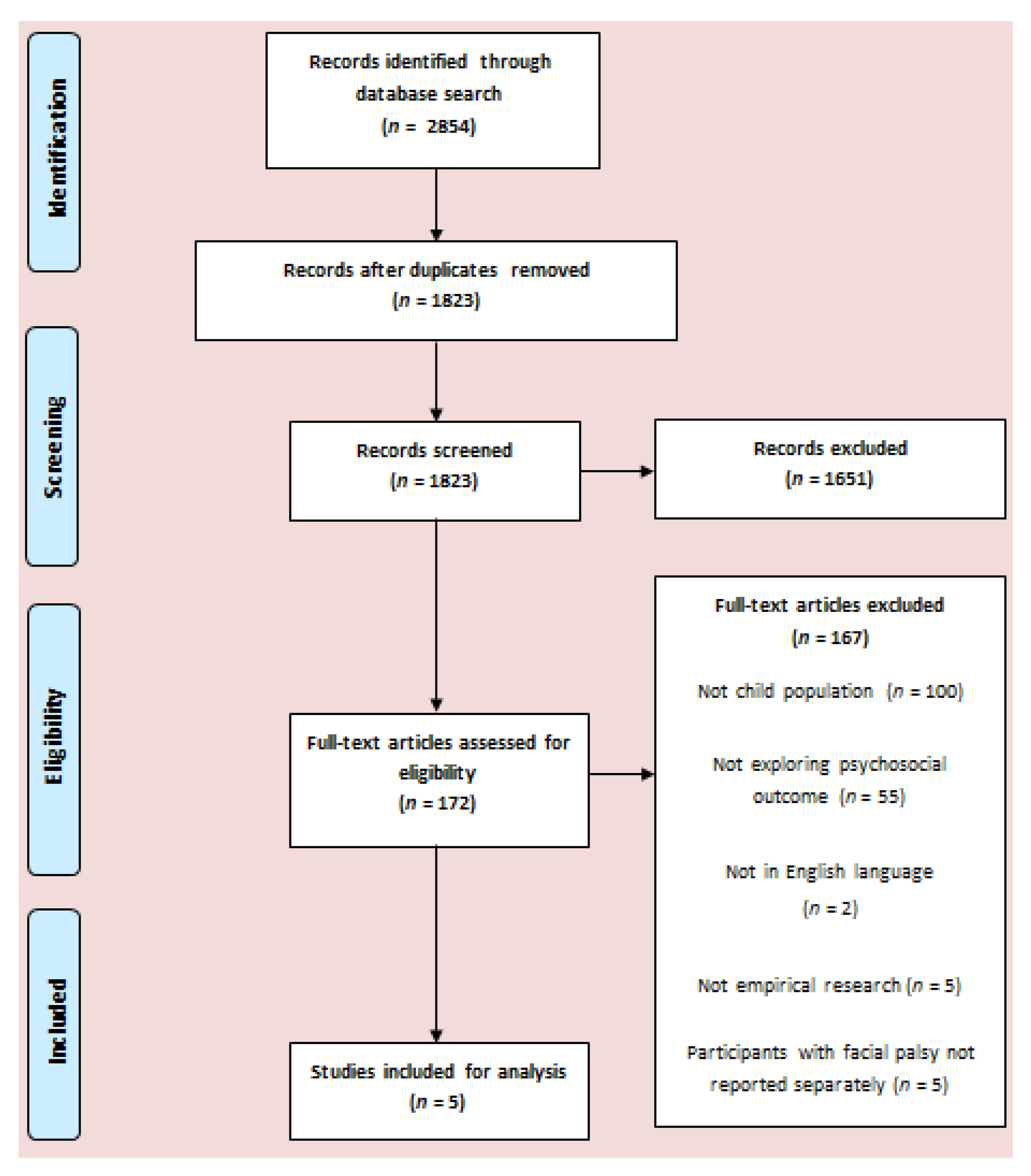
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias
3.4. Behaviour
3.5. Social Difficulties
3.6. Quality of Life
3.7. Anxiety
3.8. Depression
3.9. Personality
4. Discussion
4.1. Clinical Implications
4.2. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Shargorodsky, J.; Lin, H.W.; Gopen, Q. Facial nerve palsy in the pediatric population. Clin. Pediatr. 2010, 49, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Falco, N.A.; Eriksson, E. Facial nerve palsy in the newborn: Incidence and outcome. Plast. Reconstr. Surg. 1990, 85, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Picciolini, O.; Porro, M.; Cattaneo, E.; Castelletti, S.; Masera, G.; Mosca, F.; Bedeschi, M.F. Moebius syndrome: Clinical features, diagnosis, management and early intervention. Ital. J. Pediatr. 2016, 42, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jenke, A.C.; Stoek, L.M.; Zilbauer, M.; Wirth, S.; Borusiak, P. Facial palsy: Etiology, outcome and management in children. Eur. J. Peadiatr. Neuv. 2011, 15, 209–213. [Google Scholar] [CrossRef]
- Horstmann, G. What Do Facial Expression Convey: Feeling States, Behavioral Intentions, or Action Requests. Emotion 2003, 3, 150–166. [Google Scholar] [CrossRef]
- Lundy, B.L. Father–and mother–infant face-to-face interactions: Differences in mind-related comments and infant attachment? Infant. Behav. Dev. 2003, 26, 200–212. [Google Scholar] [CrossRef]
- Thompson, A.; Kent, G. Adjusting to disfigurement: Processes involved in dealing with being visibly different. Clin. Psychol. Rev. 2001, 21, 663–682. [Google Scholar] [CrossRef]
- Bogart, K.R.; Matsumoto, D. Living with Moebius syndrome: Adjustment, social competence, and satisfaction with life. Cleft Palate-Cran. J. 2010, 47, 134–142. [Google Scholar] [CrossRef]
- Masnari, O.; Landolt, M.A.; Roessler, J.; Weingaertner, S.K.; Neuhaus, K.; Meuli, M.; Schiestl, C. Self-and parent-perceived stigmatisation in children and adolescents with congenital or acquired facial differences. J. Plast. Reconstr. Aes. 2012, 65, 1664–1670. [Google Scholar] [CrossRef]
- Rumsey, N.; Harcourt, D. Visible difference amongst children and adolescents: Issues and interventions. Dev. Neurorehabil. 2007, 10, 113–123. [Google Scholar] [CrossRef]
- Bogart, K.R. People are all about appearances: A focus group of teenagers with Moebius syndrome. J. Health Psychol. 2015, 20, 1579–1588. [Google Scholar] [CrossRef] [Green Version]
- Hotton, M.; Hamlet, C.; Kilcoyne, S.; Johnson, D.; Norris, J.H.; Huggons, E.; Shore, D.; Dalton, L. The Psychosocial Impact of Facial Palsy: A Systematic Review. Br. J. Health Psychol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Int. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- National Institutes of Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [National Heart, Blood, and Lung Institute]. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 2 June 2020).
- Briegel, W.; Hofmann, C.; Schwab, K.O. Moebius sequence: Behaviour problems of preschool children and parental stress. Genet. Couns. 2007, 18, 267. [Google Scholar] [PubMed]
- Briegel, W.; Hofmann, C.; Schwab, K.O. Behaviour problems of patients with Moebius sequence and parental stress. J. Paediatr. Child. Health 2010, 46, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Strobel, L.; Renner, G. Quality of life and adjustment in children and adolescents with Moebius syndrome: Evidence for specific impairments in social functioning. Res. Dev. Disabil. 2016, 53, 178–188. [Google Scholar] [CrossRef]
- Briegel, W.; Heinzel-Gutenbrunner, M.; Beate, Y. Psychological adjustment of young subjects with Möbius sequence and their primary caregivers’ strain and life satisfaction: First longitudinal data. Res. Dev. Disabil. 2019, 85, 42–49. [Google Scholar] [CrossRef]
- Achenbach, T.M.; Edelbrock, C.S. Manual for the Child Behavior Checklist and Revised Child Behaviour Profile; University of Vermont Department of Psychiatry: Burlington, NJ, USA, 1983. [Google Scholar]
- Klasen, H.; Woerner, W.; Rothenberger, A.; Goodman, R. German version of the Strength and Difficulties Questionnaire (SDQ-German)—Overview and evaluation of initial validation and normative results. Prax. Kinderpsychol. Kinderpsychiatr. 2003, 52, 491–502. [Google Scholar]
- Briegel, W. Self-perception of children and adolescents with Möbius sequence. Res. Dev. Disabil. 2012, 33, 54–59. [Google Scholar] [CrossRef]
- Wieczerkowski, W.; Nickel, H.; Janowski, A.; Fittkau, B.; Rauer, W. Angstfragebogen für Schüler: (AFS); Handanweisung für die Durchführung, Auswertung und Interpretation; Hogrefe-Verlag: Göttingen, Germany, 1998. [Google Scholar]
- Stiensmeier-Pelster, J.; Schürmann, M.; Duda, K. Depressions-Inventar für Kinder und Jugendliche (DIKJ); Hogrefe-Verlag: Göttingen, Germany, 2000. [Google Scholar]
- Ravens-Sieberer, U.; Bullinger, M. Assessing health-related quality of life in chronically ill children with the German KINDL: First psychometric and content analytical results. Qual. Life Res. 1998, 7, 399–407. [Google Scholar] [CrossRef]
- Seitz, W.; Rausche, A. Persönlichkeitsfragebogen für Kinder Zwischen 9 und 14 Jahren: PFK 9-14; Hogrefe-Verlag: Göttingen, Germany, 2004. [Google Scholar]
- Krause, M.P.; Petermann, F.; Petermann, F. Soziale Orientierungen von Eltern Behinderter Kinder (SOEBEK); Hogrefe Verlag für Psychologie; Hogrefe-Verlag: Göttingen, Germany, 1997. [Google Scholar]
- Bogart, K.R. The role of disability self-concept in adaptation to congenital or acquired disability. Rehabil. Psychol. 2014, 59, 107–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wood, A.; Rychlowska, M.; Korb, S.; Niedenthal, P. Fashioning the face: Sensorimotor simulation contributes to facial expression recognition. Trends Cogn. Sci. 2016, 20, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Movérare, T.; Lohmander, A.; Hultcrantz, M.; Sjögreen, L. Peripheral facial palsy: Speech, communication and oral motor function. Eur. Ann. Otorhinolary 2017, 134, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Gillberg, C.; Steffenburg, S. Autistic behaviour in Moebius syndrome. Acta Paediatr. 1989, 78, 314–316. [Google Scholar] [CrossRef] [PubMed]
- Briegel, W.; Schimek, M.; Kamp-Becker, I. Moebius sequence and autism spectrum disorders—Less frequently associated than formerly thought. Res. Dev. Disabil. 2010, 31, 1462–1466. [Google Scholar] [CrossRef]
- Helfert, S.; Warschburger, P. The face of appearance-related social pressure: Gender, age and body mass variations in peer and parental pressure during adolescence. Child. Adolesc. Psychiatry Ment. Health 2013, 7, 16. [Google Scholar] [CrossRef] [Green Version]
- Morgan, S.; Davies, S.; Palmer, S.; Plaster, M. Sex, drugs, and rock ‘n’roll: Caring for adolescents and young adults with cancer. J. Clin. Oncol. 2010, 28, 4825–4830. [Google Scholar] [CrossRef]
- Blakemore, S.J. Development of the social brain in adolescence. J. R. Soc. Med. 2012, 105, 111–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyerson, M.D. Resiliency and success in adults with Moebius syndrome. Cleft Palate-Cran. J. 2001, 38, 231–235. [Google Scholar] [CrossRef]
- Bogart, K.R. Socioemotional functioning with facial paralysis: Is there a congenital or acquired advantage? Health Psychol. 2019, 39, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Bogart, K.R.; Tickle-Degnen, L.; Joffe, M.S. Social interaction experiences of adults with Moebius syndrome: A focus group. J. Health Psychol. 2012, 17, 1212–1222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartels, M.; Hendriks, A.; Mauri, M.; Krapohl, E.; Whipp, A.; Bolhuis, K.; Roetman, P. Childhood aggression and the co-occurrence of behavioural and emotional problems: Results across ages 3–16 years from multiple raters in six cohorts in the EU-ACTION project. Eur. Child. Adolesc. Psychiatry 2018, 27, 1105–1121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renault, F.; Quijano-Roy, S. Congenital and acquired facial palsies. In Neuromuscular Disorders of Infancy, Childhood, and Adolescence; Darras, B.T., Jones, H.R., Ryan, M.M., De Vivo, D.C., Eds.; Academic Press: Cambridge, MA, USA, 2015; pp. 225–242. [Google Scholar]
- Guajardo, N.R.; Snyder, G.; Petersen, R. Relationships among parenting practices, parental stress, child behaviour, and children’s social-cognitive development. Infant. Child. Dev. 2009, 18, 37–60. [Google Scholar] [CrossRef]
- Hastings, R.P. Parental stress and behaviour problems of children with developmental disability. J. Intell. Dev. Disabil. 2002, 27, 149–160. [Google Scholar] [CrossRef]
- Michael, J.; Bogart, K.; Tylén, K.; Krueger, J.; Bech, M.; Østergaard, J.R.; Fusaroli, R. Training in compensatory strategies enhances rapport in interactions involving people with Möbius syndrome. Front. Neurol. 2015, 6, 213. [Google Scholar] [CrossRef] [Green Version]
- Hotton, M.; Kilcoyne, S.; Holden, C.; Dalton, L.; Norris, J.H.; Johnson, D. Addressing the physical and psychosocial needs of young people with facial palsy: Facilitation of a single session group intervention. J. Plast. Reconstr. Aes. Surg. 2019, 72, 1219–1243. [Google Scholar] [CrossRef]
- Hsu, P.; Ma, A.; Wilson, M.; Williams, G.; Curotta, J.; Munns, C.F.; Mehr, S. CHARGE syndrome: A review. J. Paediatr. Child. Health 2014, 50, 504–511. [Google Scholar] [CrossRef]
- Hartshorne, T.S.; Stratton, K.K.; Brown, D.; Madhavan-Brown, S.; Schmittel, M.C. Behavior in CHARGE syndrome. Am. J. Med. Genet. C 2017, 175, 431–438. [Google Scholar] [CrossRef] [Green Version]
- Berger, Z.E.; Dalton, L.J. Coping with a cleft: Psychosocial adjustment of adolescents with a cleft lip and palate and their parents. Cleft Palate-Cran. J. 2009, 46, 435–443. [Google Scholar] [CrossRef]
- Murray, L.; Arteche, A.; Bingley, C.; Hentges, F.; Bishop, D.V.; Dalton, L.; Cleft Lip and Palate Study Team. The effect of cleft lip on socio-emotional functioning in school-aged children. J. Child. Psychol. Psychiatry 2010, 51, 94–103. [Google Scholar] [CrossRef]
| Subheading | Search Terms |
|---|---|
| Population | Facial palsy-facial paralys *, facial pals *, facial pares *, hemi-facial paralys *, hemi-facial pals *, hemi-facial pares *, Bell * Pals *, Ramsay Hunt, Mo?bius |
| Outcome | Psychosocial- psychology, psychiatry, psych *, mental disorders, anxiety, anxious, depress *, distress *, mood, emotion *, confidence, self-concept, self-perception, self-esteem, self-image, self-worth, body image, appearance |
| Outcome Measure | Construct Measured | Subscales | Parent-or Self-Report |
|---|---|---|---|
| AFS | Anxiety | Test Anxiety Manifest Anxiety Dislike of School Social Desirability | Self-report |
| CBCL | Behaviour | Social Withdrawal Somatic Complaints Anxiety/Depression Social Problems Thought Problems Attention Problems Delinquent Behaviour Aggressive Behaviour | Parent-report |
| DIKJ | Depression | N/A | Self-report |
| KINDL | Quality of Life | Physical Wellbeing Emotional Wellbeing Self-Esteem Family Friends School | Parent- and self-report |
| PFK 9–14 | Personality | General Anxiety Belief in Own Opinions Decisions and Plans Self-Perception of Impulsivity Tendency to Overestimate One’s own Capabilities Feeling of Inferiority | Self-report |
| SDQ-Deu | Psychosocial Adjustment | Emotional Problems Conduct Problems Hyperactivity/Inattention Peer Problems Prosocial Behaviour | Parent-and self-report |
| Authors | Country | Sample Size n (n Female) | Age in Years M (SD) | Diagnosis | Comorbidities | Design and Setting | Measures | Main Finding(s) |
|---|---|---|---|---|---|---|---|---|
| Briegel, Hofmann, and Schwab (2007) | Germany | 13 (6) | 3.83 (Range = 2.08– 5.92) |
Moebius syndrome:
|
| Cross-sectional; recruitment from the German Moebius Foundation | CBCL (parent-report) | 16.7% (n = 2) scored in clinical range on at least one scale Boys scored higher (more problems) than girls on: Aggressive Behaviour, Total Problems, Oppositional Defiant Problems and Anxiety Problems |
| Briegel, Hofmann, and Schwab (2010) | Germany | 31 (19) | Median = 10.58 (Range = 4.58 – 17.00) |
Moebius syndrome:
|
| Cross-sectional; recruitment from the German Moebius Foundation | CBCL (parent-report) | 32.2% (n = 10) scored in clinical range on at least one scale No significant differences between genders on any scale Social Problems more common among older children |
| Briegel (2012) | Germany | 17 (8) | 11.59 (1.87) |
Moebius syndrome:
|
| Cross-sectional; recruitment from the German Moebius Foundation | AFS | Lower Test Anxiety and Manifest Anxiety than normative data |
| DIKJ | Lower Total Depression than normative data | |||||||
| SDQ- Deu | 52.9% (n = 9) scored in the abnormal range on at least one scale Social Problems significantly increased with age | |||||||
| Strobel and Renner (2016) | Germany | 26 (11) | 11.30 (4.50) |
Moebius syndrome:
|
| Cross-sectional; recruitment from the German Moebius Syndrome Foundation | KINDL | Significantly greater difficulties with Friends compared to normative data (parent- and self-report) Significantly greater difficulties with Friends and Emotional Well-Being with increased age |
| SDQ- |Deu | Significantly higher Total Difficulties (parent-report) and Peer Problems (parent- and self-report) than normative data | |||||||
| Briegel, Heinzel-Guttenbrunner, and Beate (2019) | Germany | 26 (14) | 15.20 (3.48) |
Moebius syndrome:
|
| Cohort; four-year follow-up to participants in study described by Briegel et al. (2010); German Moebius Syndrome Foundation | CBCL (parent report) | Significantly higher scores (more problems) than the general population on all scales apart from Externalising problems 55% (n = 11) scored in clinical range on at least one scale No significant changes between scores at T1 (Briegel et al. 2010) and T2 (Briegel et al. 2019) |
| Study | |||||
|---|---|---|---|---|---|
| Briegel et al. (2007) [15] | Briegel et al. (2010) [16] | Briegel (2012) [21] | Strobel and Renner (2016) [17] | Briegel et al. (2019) [18] | |
| 1. Was the research question or objective in this paper clearly stated? | Yes | Yes | Yes | Yes | Yes |
| 2. Was the study population clearly specified and defined? | Yes | Yes | Yes | Yes | Yes |
| 3. Was the participation rate of eligible persons at least 50%? | Yes | Yes | NR | Yes | Yes |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? | Yes | Yes | Yes | Yes | Yes |
| 5. Was a sample size justification, power description, or variance and effect estimates provided? | Yes | No | No | Yes | No |
| 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? | No | No | No | No | No |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | Yes | Yes | Yes | Yes | Yes |
| 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? | No | No | No | No | No |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | Yes | Yes | Yes | Yes | Yes |
| 10. Was the exposure(s) assessed more than once over time? | No | No | No | No | Yes |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | NR | NR | NR | Yes | NR |
| 12. Were the outcome assessors blinded to the exposure status of participants? | NR | NR | NR | NR | NR |
| 13. Was loss to follow-up after baseline 20% or less? | NA | NA | NA | NA | Yes |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | No | No | No | No | No |
| Overall Score (0–14) | 7 | 6 | 5 | 8 | 8 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hotton, M.; Huggons, E.; Hamlet, C.; Bogart, K.; Johnson, D.; Norris, J.H.; Kilcoyne, S.; Dalton, L. A Systematic Review of the Psychosocial Adjustment of Children and Adolescents with Facial Palsy: The Impact of Moebius Syndrome. Int. J. Environ. Res. Public Health 2020, 17, 5528. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17155528
Hotton M, Huggons E, Hamlet C, Bogart K, Johnson D, Norris JH, Kilcoyne S, Dalton L. A Systematic Review of the Psychosocial Adjustment of Children and Adolescents with Facial Palsy: The Impact of Moebius Syndrome. International Journal of Environmental Research and Public Health. 2020; 17(15):5528. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17155528
Chicago/Turabian StyleHotton, Matthew, Esme Huggons, Claire Hamlet, Kathleen Bogart, David Johnson, Jonathan H. Norris, Sarah Kilcoyne, and Louise Dalton. 2020. "A Systematic Review of the Psychosocial Adjustment of Children and Adolescents with Facial Palsy: The Impact of Moebius Syndrome" International Journal of Environmental Research and Public Health 17, no. 15: 5528. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17155528





