Individual Circadian Preference, Shift Work, and Risk of Medication Errors: A Cross-Sectional Web Survey among Italian Midwives
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Instruments and Procedures
- demography, actual working schedule, and working experience information;
- the Morningness–Eveningness Questionnaire (MEQ), consisting of 19 questions about personal daily sleep-wake habits and the times of day of preference of certain activities, with assigned points from 0 to 5, giving a possible overall score ranging from 16 to 86. Five categories can be identified: definitely E-type (16–30), moderately E-type (31–41), neither type or I-type (42–58), moderately M-type (59–69), and definitely M-type (70–86). For ease of interpretation, we considered moderately E-type as E-type (16–41 points) and moderately M-type as M-type (59–86 points). Thus, we had three final subgroups: E-types, I-types, and M-types.
- a perception of risk of medication errors survey, based on the “seven rights” (7R) rule of medication administration (right medication, right client, right dose, right time, right route, right reason, and right documentation) [33]. As for risk evaluation, we chose “near misses”, i.e., accidents that do not cause the patient harm [34], since they represent the majority of medication errors [14]. The perception of risk of medication errors was evaluated on the basis of the following questions:
- -
- Based on the 7R rule, during the last shift, how many times did you (or any of your colleagues) run the risk of making a medication error?
- -
- Why medication error was about to occur?
2.3. Statistical Analysis
3. Results
3.1. Participants
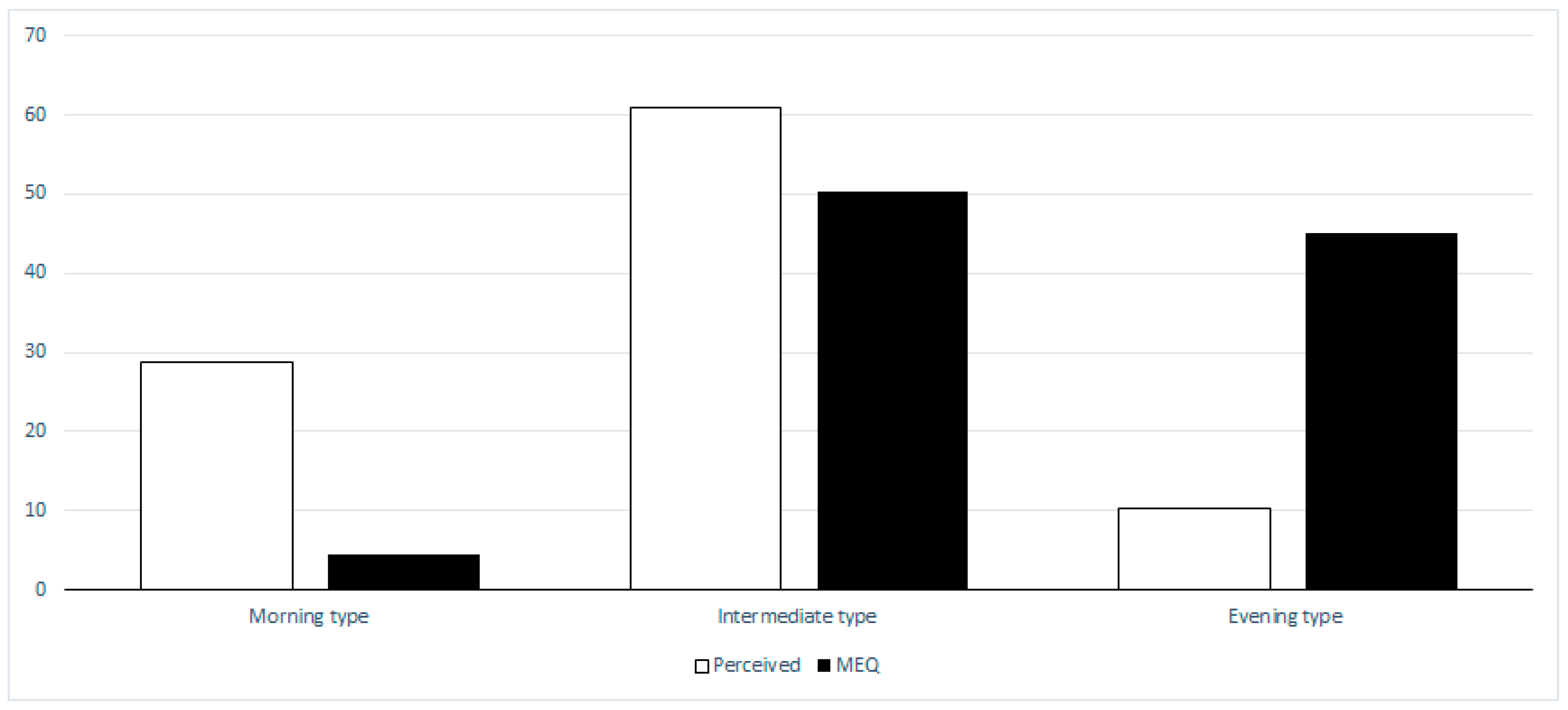
3.2. Chronotype
3.3. Perception of Risk of Medication Errors
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Manfredini, R.; Salmi, R.; Malagoni, A.M.; Manfredini, F. Circadian rhythm effects on cardiovascular and other stress-related events. In George Fink (Editor-in-Chief) Encyclopedia of Stress, 2nd ed.; Academic Press: Oxford, UK, 2007; Volume 1, pp. 500–505. [Google Scholar]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar] [PubMed]
- Ashkenazi, I.E.; Reinberg, A.E.; Motohashi, Y. Interindividual differences in the flexibility of human temporal organization: Pertinence to jetlag and shiftwork. Chronobiol. Int. 1997, 14, 99–113. [Google Scholar] [CrossRef] [PubMed]
- Randler, C.; Engelke, J. Gender differences in chronotype diminish with age: A meta-analysis based on morningness/chronotype questionnaires. Chronobiol. Int. 2019, 36, 888–905. [Google Scholar] [CrossRef] [PubMed]
- Fabbian, F.; Zucchi, B.; De Giorgi, A.; Tiseo, R.; Boari, B.; Salmi, R.; Cappadona, R.; Gianesini, G.; Bassi, E.; Signiani, F.; et al. Chronotype, gender and general health. Chronobiol. Int. 2016, 33, 863–882. [Google Scholar] [CrossRef] [PubMed]
- Ki, J.; Ryu, J.; Baek, J.; Huh, I.; Choi-Kwon, S. Association between Health Problems and Turnover Intention in Shift Work Nurses: Health Problem Clustering. Int. J. Environ. Res. Public Health 2020, 17, 4532. [Google Scholar] [CrossRef]
- Nowack, K.; Van Der Meer, E. The synchrony effect revisited: Chronotype, time of day and cognitive performance in a semantic analogy task. Chronobiol. Int. 2018, 35, 1647–1662. [Google Scholar] [CrossRef]
- López-Soto, P.J.; Fabbian, F.; Cappadona, R.; Zucchi, B.; Manfredini, F.; Garcia-Arcos, A.; Carmona-Torres, J.M.; Manfredini, R.; Rodriguez-Borrego, M.A. Chronotype, nursing activity, and gender: A systematic review. J. Adv. Nurs. 2019, 75, 734–748. [Google Scholar] [CrossRef]
- Sack, R.L.; Auckley, D.; Auger, R.R.; Carskadon, M.A.; Wright, K.P., Jr.; Vitiello, M.V.; Zhdanova, I.V. Circadian rhythm sleep disorders: Part II, advanced sleep phase disorder, delayed sleep phase disorder, free-running disorder, and irregular sleep-wake rhythm. An American Academy of Sleep Medicine review. Sleep 2007, 30, 1484–1501. [Google Scholar] [CrossRef] [Green Version]
- European Foundation for the Improvement of Living and Working Conditions. Available online: https://www.eurofound.europa.eu/publications/report/2009/working-time-in-the-european-union-italy (accessed on 21 March 2020).
- Choi, S.J.; Song, P.; Suh, S.; Joo, E.Y.; Lee, S.I. Insomnia symptoms and mood disturbances in shift workers with different chronotypes and working schedules. J. Clin. Neurol. 2020, 16, 108–115. [Google Scholar] [CrossRef]
- Ritonja, J.; Tranmer, J.; Aronson, K.J. The relationship between night work, chronotype, and cardiometabolic risk in female hospital employees. Chronobiol. Int. 2019, 36, 616–628. [Google Scholar] [CrossRef]
- Brum, M.C.B.; Dantas Filho, F.F.; Schnorr, C.C.; Bertoletti, O.A.; Bottega, G.B.; da Costa Rodrigues, T. Night shift work, short sleep and obesity. Diabetol. Metab. Syndr. 2020, 12, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aseeri, M.; Banasser, G.; Baduhduh, O.; Baksh, S.; Ghalibi, N. Evaluation of medication error incident reports at a tertiary care hospital. Pharmacy (Basel) 2020, 8, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. World Alliance for Patient Safety: WHO Draft Guidelines for Adverse Event Reporting and Learning Systems: From Information to Action; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Härkänen, M.; Vehviläinen-Julkunen, K.; Murrells, T.; Paananen, J.; Franklin, B.D.; Rafferty, A.M. The contribution of staffing to medication administration errors: A text mining analysis of incident report data. J. Nurs. Scholarsh. 2020, 52, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Drake, C.L.; Roehrs, T.; Richardson, G.; Walsh, J.K.; Roth, T. Shift work sleep disorder: Prevalence and consequences beyond that of symptomatic day workers. Sleep 2004, 27, 1453–1462. [Google Scholar] [CrossRef] [PubMed]
- Rosa, D.; Terzoni, S.; Dellafiore, F.; Destrebecq, A. Systematic review of shift work and nurses’ health. Occup. Med. (Lond.) 2019, 69, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Di Muzio, M.; Reda, F.; Diella, G.; Di Simone, E.; Novelli, L.; D’Atri, A.; Giannini, A.; De Gennaro, L. Not only a Problem of Fatigue and Sleepiness: Changes in Psychomotor Performance in Italian Nurses across 8-h Rapidly Rotating Shifts. J. Clin. Med. 2019, 8, 47. [Google Scholar] [CrossRef] [Green Version]
- Di Muzio, M.; Dionisi, S.; Di Simone, E.; Cianfrocca, C.; Di Muzio, F.; Fabbian, F.; Barbiero, G.; Tartaglini, D.; Giannetta, N. Can nurses’ shift work jeopardize the patient safety? A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 4507–4519. [Google Scholar]
- Barclay, N.L.; Myachykov, A. Sustained wakefulness and visual attention: Moderation by chronotype. Exp. Brain. Res. 2017, 235, 57–68. [Google Scholar] [CrossRef] [Green Version]
- Weaver, A.L.; Stutzman, S.E.; Supnet, C.; Olson, D.M. Sleep quality, but not quantity, is associated with self-perceived minor error rates among emergency department nurses. Int. Emerg. Nurs. 2016, 25, 48–52. [Google Scholar] [CrossRef]
- Reske, M.; Rosenberg, J.; Plapp, S.; Kellermann, T.; Shah, N.J. fMRI identifies chronotype-specific brain activation associated with attention to motion--why we need to know when subjects go to bed. Euroimage 2015, 111, 602–610. [Google Scholar] [CrossRef]
- Weaver, M.D.; Vetter, C.; Rajaratnam, S.M.W.; O’Brien, C.S.; Qadri, S.; Benca, R.M.; Rogers, A.E.; Leary, E.B.; Walsh, J.K.; Czeisler, C.A.; et al. Sleep disorders, depression and anxiety are associated with adverse safety outcomes in healthcare workers: A prospective cohort study. J. Sleep. Res. 2018, 27, e12722. [Google Scholar] [CrossRef] [Green Version]
- Rydz, E.; Hall, A.L.; Peters, C.E. Prevalence and recent trends in exposure to night shiftwork in Canada. Ann. Work Expo. Health 2020, 64, 270–281. [Google Scholar] [CrossRef]
- Matheson, A.; O’Brien, L.; Reid, J.A. Women’s experience of shiftwork in nursing whilst caring for children: A juggling act. J. Clin. Nurs. 2019, 28, 3817–3826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verma, A.; Kishore, J.; Gusain, S. A comparative study of shift work effects and injuries among nurses working in rotating night and day shifts in a tertiary care hospital of North India. Iran J. Nurs. Midwifery Res. 2018, 23, 51–56. [Google Scholar] [CrossRef]
- Khastar, H.; Mirrezaie, S.M.; Chashmi, N.A.; Jahanfar, S. Sleep improvement effect on sexual life quality among rotating female shift workers: A randomized controlled trial. J. Sex. Med. 2020, 17, 1467–1475. [Google Scholar] [CrossRef] [PubMed]
- Querstret, D.; O’Brien, K.; Skene, D.J.; Maben, J. Improving fatigue risk management in healthcare: A systematic scoping review of sleep-related/fatigue-management interventions for nurses and midwives. Int. J. Nurs. Stud. 2019, 106, 103513. [Google Scholar] [CrossRef]
- Arbour, M.; Tanner, T.; Hensley, J.; Beardsley, J.; Wika, J.; Garvan, C. Factors that contribute to excessive sleepiness in midwives practicing in the United States. J. Midwifery Women Health 2019, 64, 179–185. [Google Scholar] [CrossRef]
- McCarthy, E.; Mazza, D. Cost and effectiveness of using Facebook advertising to recruit young women for research: PREFER (Contraceptive Preferences Study) Experience. J. Med. Internet Res. 2019, 21, e15869. [Google Scholar] [CrossRef] [PubMed]
- Shaver, L.G.; Khawer, A.; Yi, Y.; Aubrey-Bassler, K.; Etchegary, H.; Roebothan, B.; Asghari, S.; Wang, P.P. Using Facebook advertising to recruit representative samples: Feasibility assessment of a cross-sectional survey. J. Med. Internet. Res. 2019, 21, e14021. [Google Scholar] [CrossRef] [Green Version]
- Smeulers, M.; Verweij, L.; Maaskant, J.M.; de Boer, M.; Krediet, C.T.; Nieveen van Dijkum, E.J.; Vermeulen, H. Quality indicators for safe medication preparation and administration: A systematic review. PLoS ONE 2015, 10, e0122695. [Google Scholar] [CrossRef] [Green Version]
- Kessels-Habraken, M.; Van der Schaaf, T.; De Jonge, J.; Rutte, C. Defining near misses: Towards a sharpened definition based on empirical data about error handling processes. Soc. Sci. Med. 2010, 70, 1301–1308. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.Q.; Jiang, X.M.; Zheng, Q.X.; Zheng, J.; He, H.G.; Pan, Y.Q.; Liu, G.H. Factors associated with workplace fatigue among midwives in southern China: A multi-centre cross-sectional study. J. Nurs. Manag. 2020. [Google Scholar] [CrossRef]
- Suclupe, S.; Martinez-Zapata, M.J.; Mancebo, J.; Font-Vaquer, A.; Castillo-Masa, A.M.; Viñolas, I.; Morán, I.; Robleda, G. Medication errors in prescription and administration in critically ill patients. J. Adv. Nurs. 2020, 76, 1192–1200. [Google Scholar] [CrossRef]
- Cappadona, R.; Di Simone, E.; De Giorgi, A.; Zucchi, B.; Fabbian, F.; Manfredini, R. Biological rhythms, health, and gender-specific differences. Ital. J. Gender-Specific. Med. 2020, in press. [Google Scholar]
- Santhi, N.; Lazar, A.S.; McCabe, P.J.; Lo, J.C.; Groeger, J.A.; Dijk, D.J. Sex differences in the circadian regulation of sleep and waking cognition in humans. Proc. Natl. Acad. Sci. USA 2016, 113, E2730–E2739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gowen, R.; Filipowicz, A.; Ingram, K.K. Chronotype mediates gender differences in risk propensity and risk-taking. PLoS ONE 2019, 14, e0216619. [Google Scholar] [CrossRef] [PubMed]
- Correa, A.; Molina, E.; Sanabria, D. Effects of chronotype and time of day on the vigilance decrement during simulated driving. Accid. Anal. Prev. 2014, 67, 113–118. [Google Scholar] [CrossRef]
- Khan, W.A.A.; Conduit, R.; Kennedy, G.A.; Jackson, M.L. The relationship between shift-work, sleep, and mental health among paramedics in Australia. Sleep Health 2020, 6, 330–337. [Google Scholar] [CrossRef]
- Levandoski, R.; Sasso, E.; Hidalgo, M.P. Chronotype: A review of the advances, limits and applicability of the main instruments used in the literature to assess human phenotype. Trends Psychiatry Psychother. 2013, 35, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Sheikhtaheri, A. Near misses and their importance for improving patient safety. Iran. J. Public. Health 2014, 43, 853–854. [Google Scholar]
- Happell, B.; Reid-Searl, K.; Dwyer, T.; Caperchione, C.M.; Gaskin, C.J.; Burke, K.J. How nurses cope with occupational stress outside their workplaces. Collegian 2013, 20, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Lamont, S.; Brunero, S.; Perry, L.; Duffield, C.; Sibbritt, D.; Gallagher, R.; Nicholls, R. ‘Mental health day’ sickness absence amongst nurses and midwives: Workplace, workforce, psychosocial and health characteristics. J. Adv. Nurs. 2017, 73, 1172–1181. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, R.; Cappadona, R.; Fabbian, F. Nurses, shift work, and diabetes: Should late chronotype be considered as a risk factor? BMJ 2019, 364, 1178. [Google Scholar] [CrossRef] [PubMed]
- Zion, N.; Shochat, T. Let them sleep: The effects of a scheduled nap during the night shift on sleepiness and cognition in hospital nurses. J. Adv. Nurs. 2019, 75, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Di Simone, E.; Giannetta, N.; Auddino, F.; Cicotto, A.; Grilli, D.; Di Muzio, M. Medication errors in the emergency department: Knowledge, attitude, behavior and training needs of nurses. Indian J. Crit. Care Med. 2018, 22, 46–352. [Google Scholar]

| Main Health Issues | Chronotype | Main Findings |
|---|---|---|
| General and cardiovascular health | Evening-type | Unhealthy diet ↓ Physical activity ↑ Smoking Metabolic syndrome Diabetes mellitus |
| Psychological & psychopathological issues | Evening-type | ↑ Common mental disorders ↑ Depression symptoms ↑ Anxiety symptoms Nightmares Risk-taking behaviour |
| Morning-type | ↑ Health-related quality of life | |
| Sleep & sleep-related issues | Evening-type | Later bedtime and wake-up ↓ Sleep duration ↓ Sleep quality ↓ Sleep quantity ↓ Sleep efficiency |
| Number of Participants (n) | 401 |
|---|---|
| Female (n (%)) | 396 (98.8) |
| Mean age (years) | 38.5 ± 10.1 |
| age 23–30 years (n (%)) | 102 (25.5) |
| age 31–35 years (n (%)) | 81 (20.0) |
| age 36–40 years (n (%)) | 79 (19.8) |
| age 41–45 years (n (%)) | 37 (9.2) |
| age 46–50 years (n (%)) | 37 (9.2) |
| age 51–55 years (n (%)) | 30 (7.5) |
| age 56–60 years (n (%)) | 35 (8.8) |
| University degree (n (%)) | 32 (8) |
| High school degree (n (%)) | 369 (92) |
| Shift work schedule (n (%)) | 293 (73) |
| Mean working experience (years) | 11.7 ± 8.9 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cappadona, R.; Di Simone, E.; De Giorgi, A.; Boari, B.; Di Muzio, M.; Greco, P.; Manfredini, R.; Rodríguez-Borrego, M.A.; Fabbian, F.; López-Soto, P.J. Individual Circadian Preference, Shift Work, and Risk of Medication Errors: A Cross-Sectional Web Survey among Italian Midwives. Int. J. Environ. Res. Public Health 2020, 17, 5810. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17165810
Cappadona R, Di Simone E, De Giorgi A, Boari B, Di Muzio M, Greco P, Manfredini R, Rodríguez-Borrego MA, Fabbian F, López-Soto PJ. Individual Circadian Preference, Shift Work, and Risk of Medication Errors: A Cross-Sectional Web Survey among Italian Midwives. International Journal of Environmental Research and Public Health. 2020; 17(16):5810. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17165810
Chicago/Turabian StyleCappadona, Rosaria, Emanuele Di Simone, Alfredo De Giorgi, Benedetta Boari, Marco Di Muzio, Pantaleo Greco, Roberto Manfredini, María Aurora Rodríguez-Borrego, Fabio Fabbian, and Pablo Jesús López-Soto. 2020. "Individual Circadian Preference, Shift Work, and Risk of Medication Errors: A Cross-Sectional Web Survey among Italian Midwives" International Journal of Environmental Research and Public Health 17, no. 16: 5810. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17165810






